Abstract
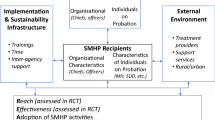
Police experience a documented, elevated need for mental health (MH) care due to the significant chronic stressors and acute traumatic experiences that characterize police work. Yet, many barriers prevent officers from accessing and engaging fully in MH treatment. The purpose of this study is to understand the idiosyncratic officer-perceived barriers and facilitators to MH service utilization to generate strategies for increasing the accessibility of MH resources. Heeding the call for more qualitative work in this line of inquiry, we used thematic analysis of in-depth, semi-structured interviews with a sample of 48 U.S. police officers to examine how officers came to initiate MH services, why they chose to engage or not engage such resources, and what organizational and supervisory factors promoted service utilization. Officers’ narratives show that police leadership should strive to (1) alleviate fear of negative professional consequences by addressing structural stigma, (2) improve agency culture and social norms around mental health care by focusing on prevention and resilience, and (3) emphasize the development of relevant and trustworthy MH care. To address structural barriers, officers described the urgent need for police leadership to clarify and make transparent organizational MH policies and processes, systematize departmental MH responses, and leverage mandated counseling. Additionally, officers perceived the need for a cultural shift emphasizing comprehensive, incentivized, preventative MH services. Finally, officers’ concerns regarding the quality of MH care encompassed the need for confidential, trustworthy services grounded in the realities of police work. Implications for research and practice are discussed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The significant chronic stressors and acute traumatic experiences characterizing police work are well-documented (Anshel 2000; Velazquez and Hernandez 2019; Violanti and Aron 1995) and are known to have adverse effects on officers, their agencies, and the public with which they interact. For example, police populations are more likely to experience a broad range of adverse mental health consequences such as higher incidences of depression, anxiety, post-traumatic stress disorder (PTSD), substance abuse, interpersonal stressors, and emotional exhaustion (Larson et al. 2007; van Gelderen et al. 2011). All of these negative effects of stress on officers’ bodies and relationships may explain the consistent finding that police officers are at higher risk for physical health problems and early death than the general population (Violanti et al. 2013). At the agency level, the strains of police work have been shown to negatively shape officers’ job performance and job satisfaction (Dowler 2005; Martinussen et al. 2007; Shane 2010), and it has been estimated that the negative effects of stress on physical and mental health create lost productivity costing at least $4489 per officer annually (Fox et al. 2012). More generally, there is strong evidence that enduring chronic stress can lead to neuroendocrine and structural deficits that can impair decision-making capacity, especially in high-risk situations (Starcke et al. 2008, 2011)—a potentially critical consideration for how officers resolve risky interactions with members of the public. Similarly, chronic stress may lead to hypervigilance or avoidance that can influence the quality of officers’ interactions with the public, for example, by heightening attitudinal endorsements of use of force (Kop et al. 1999). Thus, the need for intervention is great, and it is critical to understand how police leadership can promote the occupational health of officers by increasing engagement with mental health resources that can help improve officers’ well-being.
With the growing recognition of the benefits to occupational health that are derived from supporting police officers’ well-being through access to mental health services (Patterson et al. 2012), the U.S. has seen policy changes and greater funding for such resources (Waters and Ussery 2007). For example, officer wellness was highlighted by President Obama’s Task Force on 21st Century Policing as one of the pillars of police reform (President’s Task Force on 21st Century Policing 2015), and the International Association of Chiefs of Police (IACP), the main professional organization for police leaders, has compiled and made accessible considerations documents and model policies on employee mental health and wellness (IACP Law Enforcement Policy Center 2020). Today, police agencies attempt to meet the mental health needs of their officers by hiring staff psychologists, expanding Employee Assistance Programs, providing confidential access to a hotline (e.g., COP-2-COP), developing educational workshops on mental health, arranging critical incident debriefings, and establishing peer support groups (Finn 2000; Patterson et al. 2012).
Although police leaders are taking the need for mental health care seriously, many barriers appear to prevent officers from accessing and engaging fully in treatment. Quantitative research suggests that police officers’ service utilization does not necessarily match the need for treatment (Delprino and Bahn 1988; Patterson 2001; Waters and Ussery 2007). The bulk of the academic literature on police officers’ barriers to service utilization has emphasized the negative impact of self and social stigma on engagement with mental health services (Corrigan et al. 2006; Haugen et al. 2017; Wheeler et al. 2018), as well as logistical concerns with the accessibility to resources (Karaffa and Tochkov 2013). For example, several studies show the prevalence of self-stigma in police officer populations negatively impacts treatment seeking (Haugen et al. 2017; Karaffa and Koch 2016; Wheeler et al. 2018). Further, even if an officer has not internalized stigmatized views of mental health treatment, wider societal levels of mental health stigma may influence officers’ treatment utilization (Corrigan et al. 2006). Beyond navigating stigma, officers may also experience logistical barriers to care, such as not knowing where to get help and scheduling issues that keep some officers from using mental health supports (Delprino and Bahn 1988; Haugen et al. 2017).
Research on treatment-seeking behaviors among the general public has recently begun to focus on structural stigma (Pugh et al. 2015), which includes the “societal-level conditions, cultural norms, and institutional policies that constrain the opportunities, resources, and well-being for stigmatized populations” (Hatzenbuehler and Link 2014, p. 2). In the context of police work, structural stigma encompasses agency culture and system-level processes and policies that may impact an officer’s willingness to seek mental health treatment (e.g., requiring officers to disclose to supervisors a need for mental health treatment in order to access such services). Structural stigma has not been examined among U.S. law enforcement officers; however, international research has found evidence for structural mental health stigma in law enforcement organizations. For example, in a study with German police officers, Krick and Felfe (2020), found that coworkers’ favorable attitudes and social norms toward a mental health intervention significantly influenced its effectiveness and was marginally associated with lowered psychological strain for the officers. Structural stigma was also found among Canadian public safety personnel (PSP; Ricciardelli et al. 2020). Specifically, in thematically analyzed open-ended comments by over 800 Canadian PSPs, system-level processes emerged as a prominent factor both in deciding to seek care and in how individuals who sought treatment were perceived by coworkers in their agency. Many PSPs expressed concerns that taking leave to address mental health issues would be “leaving the team short,” pointing to both stigma in the department culture and system-level funding constraints. Surprisingly, PSPs also endorsed the fear of being perceived by their coworkers as “taking advantage of the diagnosis” if they were to take a mental health leave. Further, PSPs indicated concerns that they may receive negative performance evaluations for endorsing mental health concerns, which created another structural barrier to seeking and continuing mental health treatments. Another Canadian qualitative study with 20 Royal Canadian Mounted Police officers similarly found that system-level processes, including fear of negative repercussions on career trajectories, presented barriers to treatment seeking. Moreover, officers identified several organizational processes that would help facilitate engagement with treatment, such as consistency in the policies and processes guiding mental health responses (Burns and Buchanan 2020). Specifically, eight of 20 officers endorsed organizational processes as a hinderance to accessing care, and 19 of 20 officers felt that addressing organizational barriers to improving access to psychological services was critical.
Study Rationale
While previous research has examined barriers to accessing and engaging in mental health treatment and the general effectiveness of mental health interventions, there are several limitations to this line of inquiry. Even though a range of barriers to police officers’ service utilization have been identified, most studies have taken a piece-meal approach to understanding the association between specific barriers on levels of treatment seeking. Moreover, studies in this area typically do not consider how the various pathways by which officers may enter treatment (i.e., care-seeking profiles) may coincide with unique barriers for officer mental health service utilization. To our knowledge, no study has attempted to untangle the mutual influences of the range of known barriers and considered how officers weigh them in deciding to seek treatment and, importantly, how agencies can develop resources that comprehensively and systematically address perceived barriers.
One reason for this gap in the existing literature is the overwhelming reliance on quantitative methods, which are unable to shed light on the influences of complex nested layers of psychological and organizational factors that interact with one another when officers consider accessing mental health treatments. Specifically, there has been a lack of consideration for how officers come to initiate mental health treatments, why they choose to engage or not engage with them, and what organizational and supervisory factors may promote service utilization. For example, studies examining police officers’ experiences with mental health treatments generally do not account for the process by which officers enter care, but care-seeking profiles may have important implications for how to effectively engage officers in the offered resources. While officer’s attitudes of the value of mental health care (Karaffa and Tochkov 2013) and levels of self-stigma (Corrigan et al. 2006) may influence the likelihood of accessing treatment, the expansion of mandated post-crisis counseling (Malcolm et al. 2005) preempts the assumption that officers entering the therapeutic environment actually perceive its value or will be open to engaging meaningfully with the provider. Similarly, a study by Amaranto et al. (2003) highlights the need for qualitative research in order to understand the underlying mechanisms that may facilitate service utilization. Amaranto et al. (2003) examined the relationship between the development of educational workshops on mental health topics with calls to a newly created, anonymous hotline (staffed by retired police officers) among officers in the Newark Police Department. Over the course of 16 months, while the educational workshops were conducted, there was a significant increase in the number of calls to the hotline indicating increased utilization of the mental health resource. However, it was unclear why officers’ willingness to engage with this service improved. Two hypothesized mechanisms for the increased utilization were (1) a greater knowledge of mental health resources and (2) a reduction in mental health treatment stigma. Without nuanced information on what aspects of the program facilitated engagement with mental health resources, critical information about how police agencies can improve the occupational health of their employees is lost.
Finally, it is also notable that much of the research on the promotion of mental health service utilization for police officers was performed in international contexts, particularly in the United Kingdom, Germany, Scandinavia, and Canada (Bullock and Garland 2018; Hansson and Markström 2014; Krick and Felfe 2020; Ricciardelli et al. 2020). It cannot be assumed that the mechanisms underlying treatment seeking are similar in the U.S., where there has generally been a lesser emphasis on and investment in police officers’ psychological well-being until recently (IACP Law Enforcement Policy Center 2020; President’s Task Force on 21st Century Policing 2015; Spence et al. 2019). It is critical for U.S. police leadership to understand the nuances of officer-perceived barriers to service utilization in order to effectively facilitate officers’ engagement with such services and prevent the adverse consequences of trauma and stress.
Overall, the lack of research on the processes and nuances of officers’ treatment-seeking behaviors has prompted calls for research using qualitative methodologies to contextualize participants’ experiences with mental health interventions (Patterson et al. 2012). No U.S.-based studies have used qualitative methods to allow law enforcement officers to comprehensively identify their subjective concerns about seeking mental health treatment while also considering the idiosyncratic nested environments and experiences that may drive their decision-making process. The current study leverages in-depth qualitative interviews with a sample of police officers from across the United States (N = 48) to gain a nuanced understanding of how police officers perceive the barriers to mental health service utilization. However, unlike much existing work on officers’ barriers to treatment, which has not explicitly addressed how such barriers may be ameliorated by police leadership, we also examine the factors that facilitated officers’ service utilization by paying particular attention to officer-generated comments about specific aspects of their organization that increased access and engagement with mental health services. To that end, with the goal of providing police agencies with actionable steps for improving officers’ occupational health by increasing access and engagement with mental health services, we focus on one main research question: “In what ways can officers’ descriptions of the barriers and facilitators to mental health service utilization enhance strategies for developing accessible mental health services?”.
Methods
The qualitative data were collected as part of a study on police officers’ professional experiences more broadly. Participants in this study (N = 48)Footnote 1 included active and recently retired (within 5 years) U.S. police officers coming from a diverse set of organizational, professional, and personal backgrounds and operating in rural, suburban, and urban jurisdictions. Interview participants were recruited using network-based sampling strategies leveraging four distinct starting points (Heckathorn 1997), including social media outlets with a verified police membership, national officer associations, police department blogs, and police survivor networks. All recruitment materials referred interested officers to a study website prompting them to submit an electronic recruitment questionnaire assessing their personal and professional backgrounds. Officers’ median age was 38 (range 24–68) and median length of service was 12 years (range 3–28). Overall, female officers (n = 14) and officers who identified as persons of color (n = 21) were overrepresented relative to their percentages in the U.S. law enforcement population (Reaves 2015).Footnote 2 About half of officers held the ranks of police officer, deputy, or trooper (n = 23); 15 participants served in criminal investigations (31%), and 10 held supervisory ranks (21%). Table 1 displays the overall characteristics of the sample.
Ethics approval was granted by a research‐focused university before the commencement of the study. The data were collected by the first author in early 2019 via in-depth, semi-structured interviews held primarily by phone (average length: 2:14 h). One officer elected to be interviewed in person. No notable differences were noted between interview types. All participants gave informed consent and agreed to be audio-recorded, and participants were offered a $40 gift card in appreciation of their time. Recordings were transcribed for analysis by undergraduate research assistants (RAs). Following each interview, the researcher recorded detailed summary notes reflecting on interview content and considering themes across interviews.
Our analytic approach was guided by an essentialist/realist perspective that assumes a direct relationship between meaning and experience (Potter and Wetherell 1987), thereby privileging the participants’ perceptions and interpretations of service utilization decision-making. Overall, the analytic process involved two steps. First, the entire data corpus was examined using a master code for “Orientations toward Treatment Seeking.” A team of coders, consisting primarily of doctoral psychology students, applied this code to any text highlighting attitudes and behaviors related to seeking professional help for mental health concerns, regardless of valuation. For examples, statements could include the recognition of need for psychological support, outright rejection of psychological treatment, stigma toward mental health treatment, confidence in mental health professionals, actual or intended engagement in formal treatment or programs, and the processes by which officers arrived in a care setting, among others. “Chunking” the data in this way served to (1) provide flexibility to broadly capture all types of influences on treatment seeking without being constrained by the findings of prior research in the area and (2) allow for nuanced subcategories of barriers and facilitators to service utilization to emerge directly from officers’ narratives. The coders were trained in the proper application of the master code over several training cycles in which the same sample of transcripts was independently coded. The first author then checked inter-coder agreement for each transcript, identified discrepancies, and provided written and verbal feedback to coders to clarify disagreements on the application of the codes. After discrepancies in the application of codes had been reconciled, the data were divided among the graduate RAs and independently coded. Coding was completed in MAXQDA (VERBI Software 2018). The first author reviewed all coded transcripts to confirm consistency, and discrepancies were resolved through team consensus using an iterative process and regular research team meetings (Hill et al. 2005).
Next, the authors used the framework for thematic analysis (Braun and Clarke 2006) to examine the data for emergent themes. As the goal of our analysis was to provide a rich thematic analysis that captured the meanings from all participants’ narratives, we examined each of the 189 segments coded for “Orientations toward Treatment Seeking” to identify themes. The data examined in this study primarily derives from two sources: (1) general appraisals of officers’ stress management strategies, history of engaging in counseling services and intent to do so,Footnote 3 and (2) descriptions of high-stress events that officers had experienced (e.g., a line of duty death), how they managed each, and how their agency supported them in doing so.Footnote 4 Each coded segment was annotated with a preliminary subcategory identifying officers’ general willingness to seek treatment as well as the officer-perceived barrier or facilitator to service utilization. All subcategories were examined for patterns by clustering them into broader conceptual themes, which were refined until all subcategories were adequately captured and represented.
Findings
Officers’ narratives highlight several considerations for police leaders working to support their employees’ occupational health by facilitating engagement with mental health services. Specifically, officers’ concerns point to a multi-pronged organizational strategy to address officers’ concerns related to seeking mental health care by (1) alleviating fear of negative professional consequences by addressing structural stigma, (2) improving agency culture and social norms around mental health care by focusing on prevention and resilience, and (3) emphasizing the development of relevant and trustworthy care. Each theme and its constituent categories are provided in Table 2.
Prior to presenting the main findings of this study, it is helpful to contextualize them by considering the ways by which officers accessed mental health resources (see Table 3 for full details). Perhaps surprisingly, half of the officers (n = 24) indicated involvement with mental health or peer support services.Footnote 5 Moreover, two-thirds of the officers who entered counseling did so voluntarily; the rest were mandated to attend a mental health service following a critical incident. Notably, of the eight officers that entered mandated counseling, half continued their treatment on a voluntary basis because they found some value to the services that were provided. The majority of officers who voluntarily entered counseling primarily did so for non-professional reasons (n = 9; e.g., marriage counseling), though six officers specified work-related reasons that were causing significant distress (e.g., dealing with a tough case or line-of-duty death). One of these officers entered counseling upon becoming suicidal. Finally, only one officer engaged mental health services for preventative reasons outside of a personal or work-related crisis.
Interestingly, the majority of the 24 officers who had not accessed any form of counseling at the time of the interview stated that they would be willing to access such services should they feel the need (n = 15), at times specifying circumstances under which they may access such services (e.g., only if suicidal). Five officers were undecided about their willingness to engage in mental health counseling—primarily because they were weighing the value of treatment with concerns about structural and social stigma. Only four officers stated they would not access mental health services under any circumstances, citing concerns such as stigma or not seeing the value in counseling.
Considering the documented cultural prohibition against mental health service utilization and general trends indicating that mental health services are typically underutilized among law enforcement, the trends in officers’ care-seeking attitudes and behaviors may point to a surprising willingness to engage with mental health services and may be instructive for improving the accessibility of services. We now elaborate the main findings of the study, which are supported with direct quotations from participants. Participants are designated by the abbreviation “Ofc.” (i.e., officer) and the number of their interview.
Alleviate Fear of Negative Professional Consequences by Addressing Structural Stigma
Consistent with international research on treatment-seeking behaviors among law enforcement, we found that officers perceive significant structural stigma related to accessing mental health services. In fact, among our participants, structural stigma was the most critical barrier to treatment seeking, discussed by 31 of 48 participants. Officers generally felt that mental health service utilization could result in meaningful negative professional repercussions, and many assumed that seeking mental health care would inevitably compromise their career opportunities and financial stability: “There’s always the concerns of…what can the job find out” (Ofc. 3). Officers felt “a diagnosis like PTSD or something like that…could ruin your career” (Ofc. 40). Specifically, “…if the bosses find out, they’re going to pull you [off the street] and put you on light duty… you’re going to lose your gun. And then, you lose your job…” (Ofc. 20). Accessing mental health services meant “there goes your career, you know, your credibility—all of it” (Ofc. 3). Some officers were also concerned that having to disclose previous counseling could prevent them from being hired by another agency: “If I take a psych exam and tell them that I received counseling for whatever related to the job, I worry that I wouldn’t be able to get a job somewhere else” (Ofc. 16). Officers’ narratives revealed three main organizational efforts for improving service utilization: (1) clarifying and making transparent mental health policies and processes, (2) systematizing departmental mental health responses, and (3) leveraging mandated counseling.
Clarify and Make Transparent Mental Health Policies and Processes
While most officers expected negative professional repercussions should they seek mental health treatment, they also voiced a lack of clarity about their agencies’ processes for addressing officers’ mental health concerns and generally felt that the procedures by which their leadership addressed officers’ mental health needs were unsystematic, unpredictable and opaque:
I’m not a hundred percent sure what the rules and laws are…but even if you went to see, like, some sort doctor to talk about stuff, they could… potentially take your guns away and, you know, try to put at a disadvantage at work—you know, money-wise and losing overtime and all that. So, I just keep to myself. (Ofc. 26)
Another officer stated that “if you land in counseling way too many times—I’m not sure how it works, but I don’t know if they’ll take my gun away or whatever” (Ofc. 1). It is critical that police leadership make transparent (and easily accessible) the mental health policies that would impact an officer in need of services; or, if formal policies are unwritten, they should be developed to carefully address areas of potential concerns. Officers should understand the circumstances under which they may be placed on modified assignments, for what length of time, and by what process they would be fully reinstated. Financial consequences of seeking mental health services should be explicitly addressed to provide clarity in regard to eligibility for overtime while on modified duty. Moreover, in addition to developing mental health policies, agencies should also address in writing what steps are taken to protect the confidentiality of officers’ using such services. For example, an important concern related to accessing confidential mental health resources was officers’ perception that their agencies would “know you’re going [to counseling] because they’re paying for that through the insurance” (Ofc. 14). Transparent policies should clearly outline the steps that are taken to maintain officers’ confidentiality around treatment seeking when utilizing medical insurance, as well as limits to confidentiality.
Systematize Departmental Mental Health Responses
Many supervisors, of course, were perceived to make a concerted effort to remain vigilant of the needs of the officers under their command, allow time for officers to process serious events, and attempt to provide needed resources informally. For example, after a challenging infant death, one sergeant “pulled us both and didn’t make us work—you know, ‘go ahead and fill out your paperwork’. Do your thing. Take it easy” (Ofc. 23). In another case, when an officer became depressed following the murder of his academy classmate and attempted to resign from his position, the chief of police instead offered to place him on paid administrative leave to attend counseling, emphasizing, too, that doing so would not be “viewed negatively” (Ofc. 31).
However, because mental health responses are often not written in policy, particularly in smaller police agencies, many officers describe departmental responses to serious incidents that are comprised of a haphazard process by which individual supervisors are charged with initiating a mental health response based on their subjective sense of whether such a response was warranted. Yet, in an environment where supervisors are operating under the same cultural mental health stigma as line officers (and may additionally be navigating fiscal pressures), they may not always be effective at making such decisions. Too often leadership approaches to addressing potentially traumatic events were described as little more than informal check-ins: “my department never did debriefs on anything other than just an informal, like… ‘oh, how’s everybody doing? Ok? Good’” (Ofc. 41).
Officers who have just gone through life-threatening or deeply emotional events described completing shifts or reporting back to work the following shift without being given the time or resources to process the events they had experienced. Ofc. 3 told of the aftermath of a coworker being shot, officers went “…back up to the streets the next day” because supervisors “kind of…let us pick and choose” whether to work as normal. She felt strongly that her agency “should have” initiated a formal mental health response.
Additionally, when police leadership did not acknowledge or provide a formal response to serious events, individual officers, by extension, often did not feel comfortable discussing the incident amongst each other, particularly if there was a concern that such discussion may elicit social stigma. For example, in one agency, after two officers were shot during a routine call for an activated burglar alarm, leadership did not proactively address the situation in any way, leaving officers without an open forum to leverage the social support of their peers and process the events that left one of their coworkers permanently disabled:
I remember sitting there at roll call and we’re all just like looking at each other. Like, we didn’t know what to do; we didn’t know what to say. We did nothing. And, the captain came down and did roll call and he’s like ‘okay, go ahead, go.’ Like, that was it. (Ofc. 22)
On the other hand, when leadership proactively addressed serious events, for example by holding a debrief, they preempted the paralyzing effects of perceived social stigma by opening conversations that helped officers to “[find] out you’re not alone, that everybody else is having the same problem, or the same regrets, or the same feelings about it” (Ofc. 41).
To ensure that officers are provided with consistent and appropriate supports to process the unique burdens of police work, agencies should systematize their mental health responses. For example, formal policies should outline the types of incidents that will elicit mandated counseling or outreach by peer support. Moreover, agency responses in the aftermath of serious events should not be limited to formal mental health services. Policies should also outline guidelines for paid time off to engage with counseling services or attend the funeral of coworkers. Systematizing incidents that will elicit a mental health response by the agency and developing consistent operational procedures after serious incidents would ensure that agencies will never be without a “plan in place to get [officers] help” (Ofc. 41).
Leverage Mandated Counseling
Because of the high level of mental health stigma that characterizes police agencies and prevents officers from openly engaging in mental health services, it is important to structure access to such services in a way that facilitates officers’ involvement. As several officers stated, “[v]ery few officers are going to independently go to see a therapist—they just don’t” (Ofc. 23). Officers specified that they “[ha]ve never voluntarily gone to counseling” (Ofc. 40) and that they have refused accessing voluntary services even though they “probably should have” (Ofc. 37). Even when agencies made explicit the availability of services, officers did not always see them as accessible: “they were like, ‘if anybody needs additional help or support, you can contact us.’ And honestly, I don’t know anybody that did” (Ofc. 40). For this reason, beyond simply informing officers of the resources available to them, several participants stated that agencies should leverage mandated counseling to force officers to engage with mental health services, particularly in the aftermath of critical incidents. Some officers specified that they should have personally been forced to engage with services: “I wish they’d made me go talk to somebody. I really do” (Ofc. 3), while others felt that mandated counseling should be used as a general strategy to ensure proactive care for officers who will inevitably experience high-stress, potentially traumatizing events: “we should all be mandated to get help somehow” (Ofc. 44).
The primary reason why mandated counseling was seen as effective was because it allowed officers to bypass the potential stigma of seeking out services: “you don’t want to look like there’s something wrong with you…[b]ut if it’s something that’s forced on you, then you have to do it” (Ofc. 48). Mandated counseling provided officers cover from the potential negative consequences of engaging in mental health services because, within the hierarchical environment of a police agency, such an order is non-negotiable: “Anytime [we were] involved a threshold incident, it was mandatory. And so, [I] didn’t worry about any stigma there” (Ofc. 29). The officer went on to say “You want to remove stigma? Make them all mandatory.”
Improve Agency Culture and Social Norms Around Mental Health by Focusing on Prevention and Resilience
Officers generally perceived agency cultures and social norms that made it extremely difficult to acknowledge and proactively address the mental health challenges of police work, which reflects continuing high levels of self- and social mental health stigma. Almost half of the officers (n = 22) voiced self-stigma that has prevented them from seeking counseling. To these officers, seeking mental health care implied a personal weakness or an inability to perform police work effectively. Officers with such views eschewed treatment because “you don’t want to show weakness” (Ofc. 32), “you’re weak if you talk about [traumatic events]. You’re weak if you let it get to you” (Ofc. 28), or because they believed that “I don’t need that. I’m strong” (Ofc. 24). In some cases, they may still seek treatment but may do “it in secret. I didn’t even tell my husband I had done it” (Ofc. 15).
Relatedly, many officers that internalized stigma also had an abiding concern that social stigma from coworkers could negatively affect their professional experiences should they seek mental health treatment (n = 21). Officers voiced a deep apprehension that they would be seen as untrustworthy or unreliable due to perceived mental health struggles. Concerns about safety may lead coworkers to avoid working with certain individuals because of the perception that “they’re not strong enough to handle this; they can’t do the job” (Ofc. 20). Such concerns prevented some officers from seeking psychological counseling under all circumstances: “I’ve never talked to anybody about it…I never would, because I would think that might make me seem unstable” (Ofc. 7), or even from discussing troubling aspects of their work: “there’s a negative stigma attached. You know, if you have a bad day, you…usually don’t even tell anybody” (Ofc. 32). Moreover, even if mental health services were offered, for example, after a critical incident, officers did not always perceive them as accessible. One officer, for example, did not take advantage of offered services “because my colleagues were there” (Ofc. 38).
In spite of an acknowledgement of wide-spread mental health stigma, officers overwhelmingly felt that efforts must be taken to change “the perceptions and the culture within police departments…it’s okay to talk about feelings, it’s okay to be upset about cases, about incidents, about calls. It’s okay to not be okay” (Ofc. 23). In fact, several officers specifically noted the desire to change the culture around officers’ mental health as their primary motivation for participating in this study. Participants generally felt that police officers “need to have… more conversations about, you know, our mental health and our mental wellness” (Ofc. 10), and voiced hope that “the good old cowboy days of ‘suck it up and move on’ hopefully are done. We now need to move into the twenty-first century and…get people assistance and help so that it doesn’t fester and became a bigger issue” (Ofc. 29).
One way in which police agencies can proactively show that they prioritize the mental health of their officers while concurrently addressing existing mental health stigma is by building an organizational culture that openly emphasizes officers’ well-being, resilience, and proactive mental health care without fear of negative consequences. Some officers felt that it was not a general lack of willingness or concern among police leadership to address mental health concerns that preempted the changes that were required; however, that due to poor communication, officers may simply not be aware that the topic of mental health is important to their agency: “I think that [mental health] is a very important topic for supervisors… I don’t think officers realize that” (Ofc. 23). Police leadership can begin to improve the culture and social norms around mental health by (1) emphasizing preventative mental health services, (2) expanding mental health resources to address non-work-related stressors, and (3) improving the accessibility of mental health care by systematically addressing logistical barriers and incentivizing service utilization.
Emphasize Preventative Mental Health Services
A third of participants (n = 16) were ambivalent about the value of mental health care within the policing environment. For example, a couple of officers described a general sense of “just not having a lot of faith in the field [of psychology]” (Ofc. 41) or having a “bias already that [counseling] doesn’t work for me” (Ofc. 46). However, more often, counseling was seen only as a “last resort,” once an officer was in serious distress or after becoming suicidal: “It took all the way up to the point of me getting in that suicidal range before I finally sought help” (Ofc. 46). In other cases, while officers were willing to engage with the therapeutic process, they became disillusioned by the inability of treatment to change the stressors of police work and decided to disengage from therapy. For example, after voluntarily meeting with a counselor in the aftermath of his coworker’s felonious line of duty death, one officer came to wonder “…what is [the therapist] going to do after? She can’t make me forget about the event” (Ofc. 1), at which point he discontinued from therapy.
Police leadership (and clinical practitioners) can challenge such beliefs by re-emphasizing the value of mental health counseling in terms of the prevention of negative mental health consequences and as a strategy for resilience and improved coping with the strains for police work, rather than simply to address significant psychological distress while in crisis. Notably, out of the 16 officers that entered counseling on a voluntary basis, only one (Ofc. 8) did so outside of a personal or professional crisis with the primary goal of preventing future adverse mental health consequences. One concrete way to begin to shift beliefs about the value of preventative mental health care is by systematically restructuring mental health services to include preventative care and incentivizing the use of such resources.
Expand Mental Health Resources to Address Non-Work-Related Stressors
The officers who voluntarily sought counseling typically came to engage such resources because of personal stressors, such as the death of a loved one or a divorce. Often, counseling engaged for personal reasons subsequently also became an outlet for processing work-related stressors. As such, comprehensive preventative services addressing non-work-related matters may be an important tool for facilitating broader engagement with therapeutic services. For example, one officer “started talking to a church counselor first, and then I realized there were definitely some PTSD issues inside me” (Ofc. 24), which later facilitated engagement with the police counselor. Several officers “got into counseling because my marriage fell apart” (Ofc. 20). The ability to access a variety of counseling services allowed officers to circumvent potential stigma they may encounter for engaging in services specifically related to work-related mental health concerns. In fact, some officers strategically leveraged personal stressors to access counseling for work-related reasons. In the aftermath of a shooting, Ofc. 25 “used [his failing marriage] as a good excuse to go and talk to somebody and started seeing a psychologist.” Officers in agencies that offer a range of mental health resources generally view their agencies as very supportive and perceive the available services as more accessible: “you know, alcoholism, addiction, marital issues, anger issues, depression, like whatever – [the Employee Assistance Program] is there. So, in that way, our department does a very good job of supporting their officers” (Ofc. 33).
Systematically Address Logistical Barriers and Incentivize Service Utilization
When resources were available and perceived as accessible, some officers nonetheless encountered logistical barriers to service utilization. In our study, seven officers specified logistical barriers preventing them from accessing resources even when they felt comfortable doing so. Logistical barriers encompassed a lack of knowledge about the resources available to officers or the perceived challenge of finding a provider who could be assumed to be trustworthy and knowledgeable of the realities of police work. First, officers were overwhelmed by having to find providers they felt they would maintain their confidentiality. When Ofc. 41 wanted to access counseling after he was involved in a shooting, his agency leadership encouraged him to do so, but he wondered: “…well, where do I start? Who do I trust?” Second, unusual and erratic work schedules created challenges to scheduling or keeping appointments: “we have a mindfulness class and it teaches you how to destress…I haven’t been able to take it because it hasn’t worked with my schedule” (Ofc. 10). Services can be made more accessible when agencies allow service utilization “on city time [during work hours]” (Ofc. 27). Another officer reiterated how helpful it was when his agency facilitated service utilization during work hours by emphasizing his agency’s push to help officers engage with counseling services: “Go do what you need to do. You can do it on the clock; you can do it however you want to do it. Go get help” (Ofc. 33).
However, a critical logistical barrier pertained to the financial burden of counseling that prevented officers from engaging in such services. Some officers experienced extensive challenges to navigating the reimbursement process of their mental health treatment, especially when workers compensation is involved: “Instead of just paying for the bill, they wanted me to go through workers comp who denied the claim…So, it really made everything more complicated, added a ton more stress, and I’m still dealing with workers comp two years later” (Ofc. 41). More typically, officers felt that due to structural mental health stigma, they were unable to use their medical insurance to access mental health care as they feared that doing so could expose their mental health needs to their agency: “They know you’re going because they’re paying for that through the insurance” (Ofc. 14). As such, officers may try to protect their confidentiality by paying for care through personal financial resources instead: “I’d rather go through private counseling because it’s just best for me. It’s an extra layer of protection because it’s an outside entity” (Ofc. 38). If officers are not taking advantage of their insurance coverage due to structural mental health stigma, it may be particularly important to proactively offset the financial burden of mental health treatment in the aftermath of critical incidents, for example, by mandating and providing counseling services. One officer suggested agencies should “give me a few days [off] while paid, so I don’t have to worry about the finances. Pay me for my time to go to the counselor” (Ofc. 44).
However, beyond simply addressing officers’ direst mental health needs, agencies should also consider providing incentives to preventative health care. Officers mentioned several innovative ways in which police leadership facilitated their engagement with preventative mental health care services, for example, by offering a number of free counseling sessions per year, or by providing over-time or flex-time for engaging in counseling services: “So, we have six visits…And they don’t really even care who goes, but it’s available” (Ofc. 8). Another officer drew a parallel to her agency’s incentive schemes that compensated officers for getting preventative physical check-ups, which she felt should similarly be applied to proactively addressing mental health concerns: “if you go to a counseling appointment X amount of times or whatever, give me a day off, give me two days off, something like that” (Ofc. 44). In other cases, because “cops love overtime” (Ofc. 35), agencies strategically compensated officers with overtime payments for engaging in mental health services related to specific incidents. In Ofc. 35′s case, “going back and talking about the call…kind of helped me out.”
By creating incentives to engage with preventative mental health services, police agencies can facilitate initial access to such services, provide an opportunity to highlight the value of such care in building officers’ coping strategies and resilience, and increase officers’ comfort level for engaging with service providers in the case of an adverse event.
Emphasize Relevant and Trustworthy Mental Health Care
Officers’ engagement with treatment presented an invaluable opportunity for signaling the value of mental health services and encouraging future utilization. For example, officers who entered mandated counseling at times decided to continue treatment on a voluntary basis as they perceived the benefits of mental health care. This was the case for four of the eight officers who were mandated counseling. Two factors were critical to officer-perceived quality of services, including (1) the felt trustworthiness and confidentiality of mental health resources and (2) mental health service providers that were knowledgeable and grounded in the realities of police work.
Maximize the Perceived Trustworthiness and Confidentiality of Mental Health Resources
Many officers perceived that providers closely linked to their agency are not trustworthy (e.g., “we’ve got peer support groups that you can’t trust. We have a staff psychologist that you can’t trust”) and that providers may breach officers’ confidentiality because they are seen to “have an obligation to the county” (Ofc. 44), not the officer. Similarly, particularly in small agencies, engagement with peer support may feel stigmatizing to officers who prefer to “reach out to another cop that’s not affiliated with my agency” (Ofc. 44). To alleviate concerns of social and structural stigma when engaging in mental health resources, agencies should place priority on developing a network of service providers that are perceived by officers to be trustworthy and confidential. Officers generally felt more comfortable engaging in services unaffiliated with their agency: “It’s an outside agency that they contract with, and you can do it completely confidentially” (Ofc. 27). In some cases, officers gladly engaged with services that were accessed remotely: “my city uses a service…where you can speak with, you know, a doctor over an app on your phone. And, so, I did that, and it was like nobody knew” (Ofc. 15). Moreover, as outlined above, agencies should develop clear written mental health policies that outline the processes by which officers’ confidentiality is protected should they seek treatment.
Ensure Service Providers Are Knowledgeable About the Realities of Police Work
To increase the likelihood that officers continued to engage in services on a voluntary basis, mental health care providers also had to be knowledgeable about and grounded in the realities of police work. Officers voiced a particular concern that they would be unable to connect with counselors without a deep understanding of the stressors of police work. One officer described the necessity of counselors to have specialized knowledge because “we’re not very open to outsiders,” and there would be a concern about “[t]alking about certain things to people who maybe don’t understand what we do, and maybe, would take something the wrong way” (Ofc. 37). In fact, counselors who were ignorant of the realities of police work could unintentionally cause harm to officers within the therapeutic setting. One officer relayed the counseling experience of his coworker who talked about a violent incident he had experienced when “he noticed the doctor started the deep breathing exercises, because she was getting worked up over just hearing about it from him…so then he’s worried about her…he’s now like taking care of her” (Ofc. 41). In another case, an officer attended a mandated counseling session after the suicide of her coworker: “These people like came in and they didn’t have a clue…don’t send people in that don’t know…Do not send them in and expect them to understand me” (Ofc. 15).
Discussion/Conclusion
There are many benefits to addressing the mental health needs of law enforcement, not just to individual officers but also to police agencies and the public. For example, mental health treatment access and engagement has been shown to alleviate turnover, burnout, the number of medical retirements, and instances of disciplinary issues for officers (Christopher et al. 2016; Finn 2000), and interventions focusing on relaxation and mindfulness have been shown to have positive effects on mood and stress levels (Arnetz et al. 2009). Moreover, early intervention is preferable to reduce costs of treatment and speed the recovery of officers in crisis (as cited in Kureczka 1996). Through an in-depth examination of the narratives of U.S. police officers, the current study took a comprehensive perspective on police officers’ care-seeking attitudes and behaviors in relation to their perceived psychosocial and organizational barriers to service utilization in order to develop actionable recommendations for police leadership seeking to promote officers’ occupational health.
The way by which police officers arrive in a therapeutic setting can provide meaningful context that can guide service providers endeavoring to engage officers entering the therapeutic environment. It is likely that officers who are mandated to treatment present in counseling with different barriers than those who voluntarily seek treatment. For example, officers in mandated treatment may value mental health care less or experience higher self- or social stigma, which could influence their level of engagement in treatment and, as a result, the effectiveness of the treatment. A surprising finding of our study concerns the unexpected overall willingness of officers to engage mental health services, reflecting the tremendous work that has been done by police leaders and peer support teams to change departmental cultures about mental health, and reduce self-and social stigma associated with mental health service utilization. However, even with strides in reducing self- and social stigma, officers point to structural stigma as a persistent barrier to service utilization.
While there is some overlap in how structural stigma is expressed in U.S. and Canadian contexts, there are also notable distinctions, highlighting the prominent influence of social, political, and organizational contexts on officers’ care-seeking experiences. Structural stigma among Canadian PSPs primarily regarded concerns about being perceived by coworkers as “playing the system” when taking leave to address mental health concerns (Ricciardelli et al. 2020). It is notable that not a single U.S. officer made statements to that effect. Instead, U.S. officers voiced concerns that their treatment information might be shared and used against them, with inevitable adverse collateral consequences on their career trajectories. They also cited haphazard, inconsistent organizational practices as reasons for confusion about departmental mental health policies and the implications of service utilization on their finances and career opportunities. While the predominating organizational recommendations presented by Burns and Buchanan (2020) focused on the need to address stigmatizing departmental cultures (i.e., encouraging officers to checking in on each other’s mental health and leveraging senior members of the department as role models for accessing and utilizing care), there is some overlap with the findings of our study. Specifically, Royal Canadian Mounted Police officers emphasized the critical need for improving the organizational processes influencing access to care, particularly those related to systematizing policies for initiating Critical Incident Stress Debriefings and mandatory psychological check-ins. Overall, our findings taken together with prior work (e.g., Burns and Buchanan 2020; Krick and Felfe 2020; Ricciardelli et al. 2020) highlight that system-level factors, such as agency culture, coworker norms, and organizational policies and processes related to utilizing mental health treatment can influence not only access to but also continued engagement in treatment.
Regardless of the pathways to treatment, officers overwhelmingly endorsed structural stigma as a considerable barrier to accessing and remaining engaged with mental health services. Yet, surprisingly, organizational interventions designed to reduce mental health stigma tend to focus on factors such as self-stigma rather than structural stigma (Haugen et al. 2017). As such, police organizations may be missing an important opportunity to facilitate service utilization by directly addressing officers’ system-level concerns. To address system-level stigma, priority should be placed on developing detailed written policies guiding agency’s mental health responses to ensure consistent and adequate responses to officers’ needs even in agencies characterized by high levels of stigma. Critically, agencies should consider instituting systematic departmental responses following not only traditional critical incidents (e.g., officer-involved shooting) but also other emotionally ladened events (e.g., infant death). Moreover, greater clarity on the potential career implications of treatment seeking could help alleviate officers’ unfounded concerns related to service utilization. For example, based on officers’ narratives, it is unclear how many agencies transparently communicate policies on officer mental health service utilization. The potentially poor communication of agencies’ mental health policies may also be reflected in a recent national report on police policies, which neglected to even include mental health policies as a category (Brooks 2020). Transparent communication of policies could go a long way in promoting positive departmental norms about accessing and engaging in mental health treatment. In general, interventions designed to reduce stigma and increase service utilization do not appear to address the development and clarification of departmental policies and procedures.
While the majority of officers entered treatment voluntarily, there was a consensus among officers who generally endorsed the need for mandated treatment as a strategy for circumventing the stigma of service utilization. Academic scholars have similarly called for the implementation of mandatory counseling, noting that barriers to treatment seeking could be ameliorated by doing so (e.g., Carlan and Nored 2008; Papazoglou and Tuttle 2018). Yet, there is very little research to inform evidence-based practices for the implementation of mandatory counseling within police agencies. It is possible, for example, that the implementation of mandatory services could impede rapport building between counselors and officers, or have unintended adverse consequences for officers’ perceptions of their organizational environments. Systematic empirical research in the area could help inform recommendations for clinical and organizational practices that facilitate the implementation of mandatory mental health services.
While recent policy reports have emphasized the need for addressing officers’ well-being and mental health (President’s Task Force on 21st Century Policing 2015), few concrete recommendations have been made to address structural stigma systematically. In fact, while the federal report in 2015 issued a vague directive to continue supporting research into the efficacy of an annual mental health check for officers, no specific recommendations for addressing mental health stigma and improving service utilization were highlighted. Since then, however, the Law Enforcement Mental Health and Wellness Act has been signed into law (2018), which has brought more awareness and allocated more resources to this important issue. Most recently, a report to Congress recommended (1) the development of a strategic national campaign to destigmatize mental health and wellness concerns among law enforcement, as well as (2) the need to identify culturally competent clinicians in community settings and embed them within departments to help improve service utilization (Spence et al. 2019).
Encouragingly, the IACP has attempted to provide some additional guidance on policies and procedures that can assist officers in navigating mental health challenges. For example, a recent publication of the IACP has recognized the need to address mental health stigma and, moreover, acknowledges the necessity for an organizational culture in which “ mental health is a key aspect of overall employee wellness, with the focus on mental health couched in positive, as opposed to punitive, terms” and where police leadership “exhibit unconditional support for the use of mental health services” (IACP Law Enforcement Policy Center 2020, p. 3). However, while the IACP generally states the need for preventative services, the overall focus of officer mental health still emphasizes crisis services and suicide prevention. Our findings related to the prominence of personal stressors as the primary reason for entering the therapeutic environment highlight the need for preventative services and broad shift toward agency cultures and social norms that support preventative services for a variety of psychological needs (e.g., marital issues, chronic stress on the job, and trauma from critical incidents). Such proactive preventative efforts have to be initiated by police leadership (Cohen et al. 2019) and could serve to mitigate the risk for crisis-level mental health concerns that are difficult, expensive, and time-consuming to treat (Amaranto et al. 2003; Arnetz et al. 2009; Levenson 2007).
In addition to concerns about structural stigma, many officers expressed concerns about the quality of mental health services, specifically, clinicians’ understanding of police culture and the nature of the job, trustworthiness of the clinician, and need for adequate confidentiality. Cultural competency and evidence-based treatment are two pillars of training for clinical psychologists (Bhui et al. 2007). Clinicians anecdotally describe the intricacies of working with police officers and there are practical manuals that address cultural competency in working with police officers (e.g., Rudofossi et al. 2020), but there appears to be scant research on evidence-based principles for treating police officers that comprehensively addresses police culture (Arnetz et al. 2009; Lees et al. 2019), particularly outside of the context of extreme stress and trauma (Papazoglou and Tuttle 2018). Of note, all of the officers supported the use of critical incident debriefings. Although there is evidence to suggest that mandated debriefings may have iatrogenic effects when they are used in response to traumatic incidents among civilian populations (e.g., debriefings following natural disasters or mass shootings), findings on the impact of debriefings for police officers and other first-responders are mixed (Devilly et al. 2006; Harris et al. 2002; Regehr 2001). One consideration for future research in this line of inquiry may be to consider how debriefings may function differently within the unique context of police work, where such interventions may serve to lower stigma by acknowledging that something stressful occurred (i.e., validation of distress) and by opening doors to social support from peers.
This study took an exploratory approach to uncover nuanced details on police officers’ decisions about accessing and continuing mental health treatment by examining officers’ self-generated concerns and recommendations for addressing the barriers to mental health service utilization. However, our findings should be considered in light of several limitations. First, our sample size is relatively small. Moreover, there are currently very few resources available for facilitating recruitment from the national pool of officers. As such, the network-based recruitment strategy may have resulted in a sample that was particularly interested in mental health care, had higher levels of previous service utilization, or had experienced particularly high levels of stressful or traumatic events that prompted them to participate in our study. However, if such a shift occurred, we do not believe it was detrimental to the study, and may in fact have led to the emergence of additional meaningful themes that impact officers’ treatment-seeking behaviors. Second, as with any qualitative study, our findings are not intended to be generalizable. However, the wide sampling strategy used resulted in participants representing a range of organizational contexts, jurisdictional characteristics, and officer demographics, which may have served to maximize the transferability of the findings across settings. Finally, we collected the data in this study in 2019. It is possible that recent controversies, particularly calls to “defund the police,” may have amplified some of the pressures described by officers in this study. Future research should consider how such sociopolitical tensions may influence both officers’ perceptions about treatment-seeking barriers as well as the feasibility of organizational changes and investments, particularly as fiscal pressures increase.
Overall, officers generated several strategies for facilitating service utilization to which police leadership can be responsive. Police leaders should address structural barriers by clarifying and systematizing organizational mental health policies, processes, and responses and implementing mandated counseling as a tool for bypassing officers’ concerns around stigma. Additionally, police leaders should move toward a culture emphasizing comprehensive, incentivized, preventative mental health services by consistently communicating the value of mental health care in terms of prevention and by providing training, resources, and programming emphasizing officers’ wellness and resilience. Finally, police leaders need to ensure the quality of accessible mental health care by developing a network of confidential services that are perceived as trustworthy and grounded in the realities of police work.
Notes
The principal investigator originally aimed for a sample of approximately 35 participants, exceeding the recommended sample size of Creswell (2007) based on the study’s design. The goal of participant selection in qualitative research is to achieve saturation (i.e., informational redundance) by gathering sufficient depth of information to fully understand the range of perceptions and experiences that describe the issue under examination (Fossey et al. 2002; Gaskell 2000). As such, we allowed for some flexibility related to a subjective sense of whether new information about the constructs under examination was discussed by participants, which ultimately increased the sample to 48.
Within our general sampling framework, we prioritized demographic diversity among the sample in an effort to be responsive to the increasing diversity of the U.S. police force (Hyland and Davis 2019) and collect sufficient data to understand the experiences of groups typically underrepresented in law enforcement.
Officers were asked broadly how they process the stressors of police work (i.e., “What do you think helps you deal with the impact of your job?”) and then, specifically, if they have received mental health counseling (i.e., “Have you ever gone to counseling to deal with the challenges of this job?”). If they had not accessed counseling, they were asked if they had concerns about doing so (i.e., “Would you have any concerns about going to counseling if you felt that you wanted to?”) and were prompted to elaborate on their answer (e.g., “Tell me more about why you’d be concerned to seek counseling?”).
When discussing high-stress events, the participant gave a general description of the event and, broadly, what their agency’s response was to the incident. As appropriate, the interviewer asked if and who they spoke to about the event, including medical or mental health care providers (i.e., “Did you talk to anyone about what happened? What about medical or mental health care providers?”). As needed, the interviewer followed up to inquire whether counseling services would have been helpful and if they would have had any concerns about accessing them.
We consider the possibility that our recruitment strategy may have resulted in a sample particularly engaged or concerned with mental health in our discussion section.
References
Amaranto E, Steinberg J, Castellano C, Mitchell R (2003) Police stress interventions. Brief Treat Crisis Interv 3(1):47–53
Anshel MH (2000) A conceptual model and implications for coping with stressful events in police work. Crim Justice Behav 27(3):375–400. https://doi.org/10.1177/0093854800027003006
Arnetz BB, Nevedal DC, Lumley MA, Backman L, Lublin A (2009) Trauma resilience training for police: psychophysiological and performance effects. J Police Crim Psychol 24(1):1–9. https://doi.org/10.1007/s11896-008-9030-y
Bhui K, Warfa N, Edonya P, McKenzie K, Bhugra D (2007) Cultural competence in mental health care: a review of model evaluations. BMC Health Serv Res 7(1):15
Braun V, Clarke V (2006) Using thematic analysis in psychology. Qual Res Psychol 3(2):77–101. https://doi.org/10.1191/1478088706qp063oa
Brooks C (2020) Local police departments: policies and procedures, 2016. U.S, Department of Justice, Office of Justice Programs, Bureau of Justice Statistics
Bullock K, Garland J (2018) Police officers, mental (ill-)health and spoiled identity. Criminol Crim Just 18(2):173–189. https://doi.org/10.1177/1748895817695856
Burns C, Buchanan M (2020) Factors that influence the decision to seek help in a police population. Int J Environ Res Public Health 17(18):6891. https://doi.org/10.3390/ijerph17186891
Carlan PE, Nored LS (2008) An examination of officer stress: should police departments implement mandatory counseling? J Police Crim Psychol 23(1):8–15. https://doi.org/10.1007/s11896-008-9015-x
Christopher MS, Goerling RJ, Rogers BS, Hunsinger M, Baron G, Bergman A, Zava DT (2016) A pilot study evaluating the effectiveness of a mindfulness-based intervention on cortisol awakening response and health outcomes among law enforcement officers. J Police Crim Psychol 31:15–28
Cohen IM, McCormick AV, Rich B (2019) Creating a culture of police officer wellness. Policing: J Policy Pract 13(2):213–229. https://doi.org/10.1093/police/paz001
Corrigan PW, Watson AC, Barr L (2006) The self–stigma of mental illness: implications for self–esteem and self–efficacy. J Soc Clin Psychol 25(8):875–884. https://doi.org/10.1521/jscp.2006.25.8.875
Creswell JW (2007) Qualitative inquiry and research design: choosing among five approaches, 2nd ed. Sage Publications, Inc.
Delprino RP, Bahn C (1988) National survey of the extent and nature of psychological services in police departments. Prof Psychol Res Pract 19(4):421–425. https://doi.org/10.1037/0735-7028.19.4.421
Devilly G, Gist R, Cotton P (2006) Ready! Fire! Aim! The status of psychological debriefing and therapeutic interventions: in the work place and after disasters. Rev Gen Psychol 10(4):318–345
Dowler K (2005) Job satisfaction, burnout, and perception of unfair treatment: the relationship between race and police work. Police Q 8(4):476–489. https://doi.org/10.1177/1098611104269787
Finn P (2000) On-the-job-stress in policing: reducing it and preventing Ii. National Institute of Justice Journal 18–24
Fossey E, Harvey C, McDermott F, Davidson L (2002) Understanding and evaluating qualitative research. Aust N Z J Psychiatry 36(6):717–732
Fox J, Desai MM, Britten K, Lucas G, Luneau R, Rosenthal MS (2012) Mental-health conditions, barriers to care, and productivity loss among officers in an urban police department. Conn Med 76(9):525–531
Gaskell G (2000) Individual and group interviewing. In M. W. Bauer & G. Gaskell (Eds.), Qualitative researching with test, image and sound: A practical handbook (pp. 38–56). Sage
Hansson L, Markström U (2014) The effectiveness of an anti-stigma intervention in a basic police officer training programme: a controlled study. BMC Psychiatry 14(1). https://doi.org/10.1186/1471-244X-14-55
Harris MB, Baloğlu M, Stacks JR (2002) Mental health of trauma-exposed firefighters and critical incident stress debriefing. J Loss Trauma 7(3):223–238
Hatzenbuehler ML, Link BG (2014) Introduction to the special issue on structural stigma and health. Soc Sci Med 103:1–6. https://doi.org/10.1016/j.socscimed.2013.12.017
Haugen PT, McCrillis AM, Smid GE, Nijdam MJ (2017) Mental health stigma and barriers to mental health care for first responders: a systematic review and meta-analysis. J Psychiatr Res 94:218–229. https://doi.org/10.1016/j.jpsychires.2017.08.001
Heckathorn DD (1997) Respondent-driven sampling: a new approach to the study of hidden populations. Soc Probl 44(2):174–199
Hill CE, Knox S, Thompson BJ, Williams EN, Hess SA, Ladany N (2005) Consensual qualitative research: an update. J Couns Psychol 52(2):196–205. https://doi.org/10.1037/0022-0167.52.2.196
Hyland SS, Davis E (2019) Local police departments personnel, 2016 (NCJ 2522835). U.S, Department of Justice, Office of Justice Programs, Bureau of Justice Statistics
IACP Law Enforcement Policy Center (2020) Employee mental health and wellness. Law Enforcement Policy Center, International Association of Chiefs of Police. https://www.theiacp.org/resources/policy-center-resource/employee-mental-health-and-wellness
Karaffa KM, Koch JM (2016) Stigma, pluralistic ignorance, and attitudes toward seeking mental health services among police officers. Crim Justice Behav 43(6):759–777. https://doi.org/10.1177/0093854815613103
Karaffa KM, Tochkov K (2013) Attitudes toward seeking mental health treatment among law enforcement officers. Applied Psychology in Criminal Justice 9(2):75–99
Kop N, Euwema M, Schaufeli W (1999) Burnout, job stress and violent behaviour among Dutch police officers. Work Stress 13(4):326–340. https://doi.org/10.1080/02678379950019789
Krick A, Felfe J (2020) Who benefits from mindfulness? The moderating role of personality and social norms for the effectiveness on psychological and physiological outcomes among police officers. J Occup Health Psychol 25(2):99–112. https://doi.org/10.1037/ocp0000159
Kureczka A (1996) Critical incident stress in law enforcement. FBI Law Enforcement Bulletin 65:10–16
Larson SL, Eyerman J, Foster MS, Gfroerer JC (2007) Worker substance use and workplace policies and programs (DHHS Publication No. SMA 07–4273; Analytic Series A-29). Substance Abuse and Mental Health Services Administration, Office of Applied Studies
Lees T, Elliott JL, Gunning S, Newton PJ, Rai T, Lal S (2019) A systematic review of the current evidence regarding interventions for anxiety, PTSD, sleepiness and fatigue in the law enforcement workplace. Ind Health 2018–0088
Levenson RL (2007) Prevention of traumatic stress in law enforcement personnel: a cursory look at the roles of peer support and critical incident stress management. Forensic Exam 16–19
Malcolm AS, Seaton J, Perera A, Sheehan DC, Van Hasselt VB (2005) Critical incident stress debriefing and law enforcement: an evaluative review. Brief Treat Crisis Interv 5(3):261–278
Martinussen M, Richardsen AM, Burke RJ (2007) Job demands, job resources, and burnout among police officers. J Crim Just 35(3):239–249. https://doi.org/10.1016/j.jcrimjus.2007.03.001
Papazoglou K, Tuttle BM (2018) Fighting police trauma: practical approaches to addressing psychological needs of officers. SAGE Open 8(3):215824401879479. https://doi.org/10.1177/2158244018794794
Patterson GT (2001) Reconceptualizing traumatic incidents experienced by law enforcement personnel. The Australasian Journal of Disaster and Trauma Studies 2:1
Patterson GT, Chung IW, Swan PG (2012) The effects of stress management interventions. Campbell Systematic Reviews 7
Potter J, Wetherell M (1987) Discourse and social psychology: beyond attitudes and behaviour. SAGE
President’s Task Force on 21st Century Policing (2015) Final report of the president’s task force on 21st century policing (p. 116). Office of Community Oriented Policing Services
Pugh T, Hatzenbuehler M, Link B (2015) Structural stigma and mental illness [Commissioned Paper for Committee on the Science of Changing Behavioral Health Social Norms, Mailman School of Public, Columbia University]
Reaves BA (2015) Local police departments, 2013: personnel, policies, and practices. U.S. Department of Justice. http://www.bjs.gov/content/pub/pdf/1pd13ppp.pdf
Regehr C (2001) Crisis debriefing groups for emergency responders: reviewing the evidence. Brief Treat Crisis Interv 1(2):87–100
Ricciardelli R, Carleton RN, Mooney T, Cramm H (2020) “Playing the system”: structural factors potentiating mental health stigma, challenging awareness, and creating barriers to care for Canadian public safety personnel. Health: An Interdisciplinary Journal for the Social Study of Health, Illness and Medicine 24(3):259–278. https://doi.org/10.1177/1363459318800167
Rudofossi D, Lund DA, Benner AW (2020) Working with traumatized police-officer patients: a clinician’s guide to complex PTSD syndromes in public safety professionals. Routledge
Shane JM (2010) Organizational stressors and police performance. J Crim Just 38:807–818. https://doi.org/10.1016/j.jcrimjus.2010.05.008
Spence DL, Fox M, Moore GC, Estill S, Comrie NEA (2019) Law enforcement mental health and wellness act: report to congress. U.S, Department of Justice
Starcke K, Polzer C, Wolf OT, Brand M (2011) Does stress alter everyday moral decision-making? Psychoneuroendocrinology 36(2):210–219. https://doi.org/10.1016/j.psyneuen.2010.07.010
Starcke K, Wolf OT, Markowitsch HJ, Brand M (2008) Anticipatory stress influences decision making under explicit risk conditions. Behav Neurosci 122(6):1352–1360. https://doi.org/10.1037/a0013281
van Gelderen BR, Bakker AB, Konijn EA, Demerouti E (2011) Daily suppression of discrete emotions during the work of police service workers and criminal investigation officers. Anxiety Stress Coping 24(5):515–537. https://doi.org/10.1080/10615806.2011.560665
Velazquez E, Hernandez M (2019) Effects of police officer exposure to traumatic experiences and recognizing the stigma associated with police officer mental health: a state-of-the-art review. Policing: Int J 42(4):711–724. https://doi.org/10.1108/PIJPSM-09-2018-0147
VERBI Software (2018) MAXQDA 2018. Verbi Software
Violanti JM, Aron F (1995) Police stressors: variations in perception among police personnel. J Crim Just 23(3):287–294. https://doi.org/10.1016/0047-2352(95)00012-F
Violanti JM, Hartley TA, Gu JK, Fekedulegn D, Andrew ME, Burchfiel CM (2013) Life expectancy in police officers: a comparison with the US general population. Int J Emerg Ment Health 15(4):217–228
Waters JA, Ussery W (2007) Police stress: History, contributing factors, symptoms, and interventions. Policing: Int J Police Strat Manag 30(2), 169–188. https://doi.org/10.1108/13639510710753199
Wheeler C, Fisher A, Jamiel A, Lynn TJ, Hill WT (2018) Stigmatizing attitudes toward police officers seeking psychological services. J Police Crim Psychol. https://doi.org/10.1007/s11896-018-9293-x
Acknowledgements
We wish to extend our deepest appreciation to the research participants of this study.
Funding
This study was funded by internal grants to the first author from the University of Virginia (no grant number applicable).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Verbal informed consent was obtained from all individual participants included in the study.
Consent for publication
Participants gave verbal informed consent regarding publishing their deidentified data.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hofer, M.S., Savell, S.M. “There Was No Plan in Place to Get Us Help”: Strategies for Improving Mental Health Service Utilization Among Law Enforcement. J Police Crim Psych 36, 543–557 (2021). https://doi.org/10.1007/s11896-021-09451-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11896-021-09451-0