Abstract
Purpose of review
Small bowel motility disorders constitute a relatively small but important segment of clinical gastroenterology. Presenting features encompass a broad range of symptom manifestations and severity: from chronic functional-type complaints to life-threatening nutritional impairment. Diagnostic assessment of patients with suspected intestinal motility disorders is often hampered by the complexity of measuring intestinal contractile activity in humans. In this review, we describe and critically comment the main current and forthcoming methodologies.
Recent findings
Beyond conventional small bowel manometry, radiological methods, and intestinal transit tests that have been available for several decades, now we focus on novel methodologies such as high-resolution manometry, magnetic resonance methodology, and endoluminal capsule image analysis.
Summary
Gradual introduction of new approaches to diagnostic investigation of patients with suspected intestinal motility disorders should facilitate a less invasive and more accurate characterization of disturbed motor function. Enhanced understanding of the pathophysiological basis of clinical conditions should allow better application of therapeutic approaches that are also highlighted in this review.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In health, normal intestinal motility is a critically important function that facilitates digestion and absorption of nutrients. Without normal intestinal motility, nutrition is severely compromised and life cannot be sustained without the aid of artificial feeding methods. And yet, this essential function takes place virtually unperceived by normal individuals and it is largely governed by autonomous control mechanisms. In this review, we will describe normal intestinal motility, its regulation and disturbances of motility that determine various clinical manifestations in disease and current diagnostic methods to assess intestinal motility. We will place special emphasis on new technologies that are now being gradually introduced to assess small bowel dysmotility in clinical practice.
Normal Intestinal Motility
Digestion and absorption of nutrients occur during controlled progression of chyme throughout the bowel. When food is emptied from the stomach into the small bowel, coordinated contractions and relaxations of the intestine, named peristalsis, mix and spread chyme over the mucosal surface, allowing absorption of nutrients and water. When digestion ends, small bowel motility changes to a cyclical pattern called the migrating motor complex (MMC). The most prominent phase of the MMC (phase III) is characterized by strong repetitive contractions of the small bowel that migrate distally and produce the so-called “house-keeping” effect cleansing the bowel of digestion residues and preventing small intestinal bacterial overgrowth [1•]. It has also recently been confirmed that the phase III of the MMC coincides with hunger peaks in healthy subjects [2].
Intestinal motility is locally controlled and coordinated by the enteric nervous system (ENS). The neuronal circuits the ENS form two plexus (submucosal and myenteric) embedded between the muscular layers of the bowel wall. An extrinsically denervated bowel with an intact ENS can maintain its motor function since the ENS automatism operates independently of the central nervous system. However, extrinsic efferents and afferents from the autonomic nervous system regulate intestinal motility and sensations through the vagal nerve (parasympathetic) and the splachnic nerves (sympathetic). Thus, intestinal motility is a physiological function governed by neural control stratified along the brain-gut axis. Dysfunction at any level of the axis may potentially disrupt normal motor activity.
Intestinal Dysmotility
Intestinal motility may be pathologically disrupted and impaired by either myopathic or neuropathic conditions. While myopathies are local processes affecting the smooth muscle of the bowel wall, neuropathies can originate in the ENS but also involve the autonomic and central nervous systems. A list of the main myopathic and neuropathic disorders causing severe intestinal dysmotility can be found in Table 1.
Severe impairment of intestinal motility, either of neuropathic or myopathic nature, can generate pseudo-occlusive episodes with a radiologically apparent dilated bowel in the absence of mechanical obstruction [3]. In this clinical setting, it is relatively simple to diagnose an intestinal motility disorder and further testing may even be unnecessary. Nevertheless, most intestinal motility disorders affect patients with chronic gastrointestinal symptoms seemingly functional and without a dilated bowel. In this case, diagnosis becomes much more challenging [4].
Conventional Intestinal Manometry
Intestinal manometry was developed and begun to be clinically applied several decades ago [5, 6]. It may be performed with a water-perfused manometric catheter orally introduced up to the mid small bowel under fluoroscopic and/or endoscopic guidance. The standard manometric catheter incorporates six manometric ports spanned at 10-cm intervals that are positioned from the proximal duodenum to the mid-jejunum with fluoroscopic assistance, as required. These ports register the amplitude and duration of phasic pressure waves produced by the intestinal contractions. Recordings are usually performed for 3 h fasting and 2 h after ingestion of a solid-liquid meal (450 Kcal). Some variations on the protocol procedure have been introduced by various specialized groups. Some use longer recordings, including ambulatory or overnight recordings, taking advantage of electronic pressure sensors and Holter type equipment. These solid-state systems with long observation periods capture MMC’s with higher probability than the 3-h test.
The criteria for reading and interpreting manometric tracings have been developed from observation of normal patterns in healthy volunteers compared to aberrant patterns observed in patients with clinical manifestations of intestinal dysmotility. This empiric approach has led to the development of certain criteria that are conventionally applied to the clinical diagnosis. Three abnormal patterns have been described, as listed in Table 2. Although the criteria employed to classify manometric recordings as either normal or abnormal have not been subjected to rigorous testing, the abnormal patterns are sufficiently stereotyped as to be recognizable by readers sufficiently acquainted with the technique. Conventional manometry appears to have high specificity in detecting pathologic motor disturbances but relatively low sensitivity. Consequently, this test is most useful when applied to symptomatic patients with major motor disturbances.
The most controversial of the above abnormal patterns is the myopathic manometric pattern characterized by very low amplitude pressure waves configuring apparently normal fasting MMC’s and normal responses to a meal. Subsequent observations have shown that this pattern does not necessarily correspond with a myopathic condition (although it may) but rather reflects a dilated small bowel with non-occluding contractions that fail to fully activate the pressure-sensitive ports of the manometry probe. Therefore, it represents more of a hypocontractile pattern than a diagnostic representation of bowel myopathy. Indeed, in advanced neuropathy with dilated loops, the same pattern may be observed.
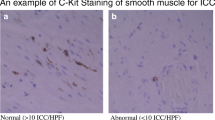
The results of a recent study comparing manometric patterns with full-thickness biopsy histopathology suggest that intestinal manometry may constitute a useful clinical tool to preselect patients with severe intestinal dysmotility for subsequent laparoscopic procurement of full-thickness small bowel tissue [7]. In our study, about three fourth of patients with definite abnormal intestinal manometry also showed aberrant intestinal histopathology and/or immunohistopathology compatible with intrinsic neuromuscular disease. Although the manometric pattern was not found to correlate tightly with any specific histopathological findings, the results suggest that intestinal manometry can detect neuromuscular abnormalities at an earlier stage compared to histopathological and immunohistological methods.
A previous study suggested that chronic intestinal pseudo-obstruction was more likely to be associated with a stereotyped manometric pattern than patients with severe functional gastrointestinal disorders [4]. However, our observations do not support this contention since we found no differences in manometric pattern abnormalities between these two groups. In our view, intestinal manometry is a potentially valuable diagnostic method that despite its relative invasiveness, technical complexity, and elevated cost helps to establish the presence of intestinal dysmotility in patients with severe and longstanding abdominal symptoms of uncertain origin.
Transit Tests
Transit tests can be used to indirectly estimate intestinal motility. Normal small bowel transit time is highly variable, and only extreme values can be considered abnormal. These tests are relatively inexpensive and widely available; therefore, small bowel motility evaluation is frequently performed using these tests.
The most used transit tests are based on ingestion of an unabsorbable carbohydrate, generally lactulose, which produces a peak in breath hydrogen when fermented by intestinal bacteria. Although these tests are clinically interpreted as a surrogate for small bowel transit times, they actually measure oro-cecal transit time and therefore accelerated or delayed gastric emptying time markedly bias the results [8]. Moreover, transit data may also be biased by the fact that lactulose itself may accelerate intestinal transit [9] and that the hydrogen peak may begin when the carbohydrate reaches the terminal ileum, as demonstrated by a recent study using simultaneous MRI [10].
Lactulose breath tests are also used to diagnose small intestinal bacterial overgrowth (SIBO), a common complication of intestinal dysmotility, when the peak in breath hydrogen is detected early after ingestion. However, accelerated intestinal transit may cause an early peak and be confused with SIBO as shown by simultaneous breath and scintigraphy testing [11]. Therefore, a positive breath test for SIBO must be cautiously interpreted if the patient has a fast small bowel transit [12], especially in patients with previous gastrointestinal surgery [13].
Scintigraphy tends to be more reliable than breath tests for the measurement of small bowel transit in humans. It is generally used in research settings and as part of a whole gut study [8]. Small bowel transit is measured as the time between gastric emptying of the radio-labeled meal and 10 or 50% arrival to the colon. Studies in healthy subjects have shown a wide inter- and intrasubject variability, so only extreme values are diagnostic. Scintigraphic data obtained in patients with various small bowel motility disorders has generally produced a quantitative measure of impaired small bowel transit. This technique has also been used to document acceleration of transit induced by prokinetics [14, 15].
The Smartpill is a small capsule which can measure gastric emptying and intestinal transit times based on the different intraluminal pH of these segments. This test has shown to be equivalent to scintigraphy for small bowel transit evaluation. Normal ranges have recently been determined in a large multicenter study [16]. Using this technique, it has been shown that slow colonic transit delays small bowel transit [17].
Radiopaque markers (ROM) have mainly been used to measure colonic transit in patients with constipation. However, they have also been applied to assess small bowel transit time by obtaining repetitive fluoroscopic images for 8 h after ingestion of the ROMs [18,19,20]. The main drawback of this procedure is the difficulty to assure the position of the ROMs in the small bowel or colon. However, with this technique, it has been shown that untreated celiac disease patients have delayed small bowel transit times, which concurs with the fact that intestinal micro-inflammation inhibits intestinal motility [21].
MRI is another imaging technique that has been employed to accurately measure small bowel transit time. Two strategies have been used: detection of the arrival of the head of a meal to the cecum or by tracking the movement of luminal marker pills [10, 22].
In the colon, transit time corresponds well with the expected symptom: slow transit in constipation and accelerated in diarrhea. This is not true for the small bowel. For example, a study evaluating small bowel transit time with radiopaque markers in a large group of patients with severe unexplained digestive symptoms found that, in patients with diarrhea, a delayed transit (defined as longer than the 95th percentile in healthy subjects) was much more frequent than an accelerated transit [23]. In fact, intestinal transit time is normal in most patients with functional GI disorders [24, 25].
As we pointed out earlier, the current gold standard technique for the evaluation of small bowel is intestinal manometry. However, since motility testing with manometry is complex and not widely available, intestinal dysmotility is frequently only presumed and indirect transit tests tend to be used to corroborate the clinical diagnosis, despite the fact that these tests have repeatedly shown to only be of value in cases of extremely delayed intestinal transit. The overall situation for intestinal motility evaluation has been obscure until recent developments have come forward. These new tools are described in the following sections.
High-Resolution Manometry
As opposed to conventional manometric catheters, high-resolution catheters have closely placed sensors that are much more sensitive to detect the frequency and direction of intestinal contractile activity, be it peristaltic, stationary, or retroperistaltic. High-resolution manometry was initially applied to other segments of the digestive tract, especially in the esophagus, with huge repercussion on the field [26]. In the colon, the use of long 72 sensor catheters has shown to detect previously unidentified cyclic motility patterns. These patterns correspond to repetitive propagating pressure events of the colonic smooth muscle that markedly increase after meals in the distal colon of healthy subjects and are diminished or even absent in patients with slow transit constipation [27•].
Application to the small bowel has not been intensively investigated, but the potential of this technique is exciting. Studies performed more than 15 years ago with high-resolution water-perfused catheters in the duodenum showed that phase III activity in the duodenum combines both antegrade and retrograde peristaltic waves [28]. Unfortunately, most of the information available so far on the use of intestinal high-resolution manometry is observational and unpublished. It comes from a small group of neurogastroenterology units around the world that are beginning to apply this method. The future use of new fiber-optic manometric catheters could greatly improve our understanding of small bowel motility [29].
Endoluminal Image Analysis
Computerized analysis of the images obtained by the endoscopic capsule has shown to reliably detect intestinal dysmotility. As compared to the current gold standard technique, intestinal manometry, the capsule obtains objective measurements of intestinal motility in a non-invasive manner. Tools to measure and quantify contractile events (luminal occlusions and radial wrinkles), non-contractile patterns (open tunnel and smooth wall patterns), type of content (secretions, chyme), and motion of wall and content have been developed using machine-learning techniques [30,31,32,33,34]. Each of these features can be found inside or outside the normal range compared to healthy subjects, although final discrimination between normal and abnormal motility is performed using computerized classifiers which use combinations of features.
This advanced methodology was first validated in a group of 36 patients with severe gut motor disorders. Patients presented either intestinal pseudo-obstruction or chronic abdominal symptoms with reduced feeding tolerance and inability to maintain normal body weight. All patients underwent intestinal manometry and 19 fulfilled manometric criteria of intestinal dysmotility. In this subgroup, endoluminal image analysis was abnormal in all but one case. Compared to healthy subjects, patients had less contractile activity, more intestinal quiescence, and greater retention of luminal content. Interestingly, in the 17 patients in whom conventional intestinal manometry failed to fulfill the established criteria of dysmotility, endoluminal imaging was abnormal in 65% of cases [35].
These encouraging results prompted subsequent studies in patients with functional bowel disorders. Even though disturbed small bowel motility is presumed to constitute an important pathophysiological mechanism in this category of patients, intestinal manometry is probably not sensitive enough to detect the more subtle motor abnormalities.
We evaluated a group of 80 patients with functional bowel disorders with the endoluminal image analysis technique and identified abnormal intestinal motility in about one third of patients with functional bowel disorders, the majority with irritable bowel syndrome. Patients with abnormal motility were either hypo- or hyperdynamic compared to healthy subjects. Patients with hypodynamic intestinal motility had similar abnormalities as those found in patients with severe motor disorders: low number of intestinal contractions and more static sequences albeit in a milder degree and without retention of secretions or overall delay of small bowel transit time [36]. A subsequent study using a newer version of the capsule evaluated a larger group of patients (205) with functional bowel disorders, and the results confirmed that one third of patients with functional bowel disorders have demonstrable intestinal dysmotility. The computerized analysis of the endoscopic images in this second study was based on the detection of sequences of motility events. In healthy subjects, most of the recording time corresponded to sequences of contractile activity with only about one third of the time exhibiting non-static content sequences. Contractile activity was consistently stimulated when subjects ingested the test meal and the effect of the meal gradually declined throughout the postprandial period as the capsule advanced towards the end of the small bowel. By contrast, patients with a hypodynamic pattern had less contractile activity and a blunted postprandial response but without an overall delay in transit or retention of secretions. Static and tunnel images were also much increased, especially in the last two thirds of recording time. On the other hand, patients with hyperdynamic behavior displayed an increased postprandial response and high-motion sequences. This latter group of patients also showed more rapid transit times and decreased pooling of intestinal content [37•].
Recently, a new tool to facilitate visualization of intestinal motility events recorded by endoluminal image analysis has been developed which has been named the motility color bar. It is constructed by using a one-pixel wide strip from each of the consecutive capsule images. With this tool, the oscillations in the caliber of the intestinal lumen and time periods with content or absence of movement are easily displayed in just one image (Fig. 1) [38, 39].
Examples of intestinal motility patterns visualized by endoluminal image analysis. The motility color bars are constructed by concatenating one-pixel wide diametric strips from consecutive images. a Occlusive contractile activity, b non-occlusive contractile activity, c static sequence with a closed intestinal lumen, d static sequence with an open intestinal lumen. Figure adapted with permission from Drozdzal M, Seguí S, Radeva P, Malagelada C, Azpiroz F, Vitrià J. Motility bar: A new tool for motility analysis of endoluminal videos. Comput Biol Med. 2015;65:320–30
Studies using endoluminal image analysis have been performed in other diseases affecting the small bowel and with suspected intestinal dysmotility that had not been previously investigated using conventional intestinal manometry. For instance, we have prospectively evaluated a group of patients with primary immunodeficiency and chronic digestive symptoms. Preliminary data shows that intestinal hypomotility is detected in about 40% of these patients and often is associated to mucosal abnormalities such as diffuse lymphoid hyperplasia that is undetectable by other imaging techniques. This demonstrates that the capsule can be used to determine the presence of structural and functional abnormalities of the small bowel in just one non-invasive test [40].
Similarly, we have also recently evaluated a group of patients with cystic fibrosis, in whom small bowel hypomotility was detected by endoluminal image analysis in 75% of cases. As compared to healthy subjects, patients with cystic fibrosis exhibited less intestinal contractions and greater luminal retention of turbid secretions [41].
Radiological Imaging Techniques
Computerized analysis of CT and MRI images of the abdomen are increasingly being applied to measure intestinal function. Specifically, measurement of the volume and morphology of intra-abdominal content has shown that the mechanisms of abdominal distention are quite different in patients with severe gut motility disorders compared to those with functional bloating. In patients with severe intestinal dysmotility, such as advanced intestinal neuropathy and enteric dysmotility, there is ineffective peristalsis which results in pooling of intestinal content (debris, fluid, and gas) associated with intestinal distension (Fig. 2). The degree of abdominal distension in such patients is directly related to intestinal volume expansion [42]. By contrast, in functional bowel disorders with abdominal distension, gut content (gas and/or fluid) is modestly increased, but through the mechanism of visceral hypersensitivity and other altered neural control mechanisms, an aberrant viscero-somatic response develops: Patients elevate their costal rack and hyperinflate their lungs while, paradoxically, contracting the diaphragm (forcing its decent) and relaxing their oblique abdominal muscles. As a result, there is a “reshaping” of abdominal geometry that redistributes its contents with protrusion of the anterior abdominal wall with minimal or no increase in total intra-abdominal volume [43, 44].
Applicability of MRI technology to assessment of intestinal motor activity. The abdominal MRI images displayed are an example of morphovolumetric analysis of the small bowel. The small bowel is first identified and filtered in each MRI image (left) to obtain a three-dimensional reconstruction where intestinal volume is measured (right). Dynamic data may be obtained by sequential imaging
MRI technology is also being applied to the measurement of intestinal diameter and content, as surrogate indicators of motor function. MRI quantification of small bowel water content has shown that patients with diarrhea subtype IBS have a reduced intraluminal water content compared to healthy subjects, reflecting spasm or constriction of the intestine [45]. Interestingly, reduction of small bowel content can also be induced by experimentally inducing acute stress via parenteral CRH administration or cold water hand immersion [46]. Contrarily, patients with functional constipation appear to have increased small bowel water content, which has been interpreted as an indicator of overall decreased intestinal tone [47].
In addition to static imaging, dynamic imaging can also be obtained using MRI by taking successive images over a period of time. In most instances, short sequences have been obtained during a breath-hold, which represents a significant technical limitation. However, prolonged sequences during free breathing have been recently obtained and analyzed by applying a computer program that automatically compensates diaphragmatic movement. The motility of small bowel segments during these sequences can be quantified using software-assisted methods [48, 49].
Many MRI units are currently adding a short cine-MRI sequence to standard small bowel imaging [50]. Thus, motility analysis has been initially applied to studies requested for evaluation of structural diseases, such as Crohn’s disease. Using dynamic-MRI methodology, several research groups have shown that intestinal segments affected by inflammation and/or stricture display reduced motility [51,52,53,54]. This technology has also been recently applied to patients with chronic intestinal pseudo-obstruction, in whom software-assisted analysis of cine-MRI images is able to detect the reduced intestinal contractility characteristic of this condition [55, 56•, 57].
Management of Small Bowel Motility Disorders
Therapeutic interventions to correct intestinal motility disturbances are limited, and for many approaches, only experimental evidence of efficacy is available. Main current and future potential options are summarized.
Pharmacological Agents
Drugs to stimulate and regularize intestinal propulsive activity (also referred to as prokinetics) belong to various classes that differ in their mechanism and preferential site of action in the gut.
The somatostatin analogue octreotide (usually administered subcutaneously as a 50–100 mcg dose in the evening) induces phase III activity in the small bowel [58, 59]. It is especially useful in the management of primary and secondary (i.e., scleroderma) forms of chronic intestinal pseudo-obstruction [60].
Metoclopramide and domperidone are dopamine-2 receptor antagonists, which have a predominant prokinetic effect on gastric motility and, to a smaller extent, on the small bowel. They are generally restricted to short-term therapies because of their significant side effects. Cholinergic agonists, mainly neostigmine and pyridostigmine, have an indication for acute bowel atony, but are also of limited use because of their side effects and likelihood of tachyphylaxis.
A number of serotonin 5HT-4 agonists have been developed as prokinetics, but unfortunately have shown to be arrhythmogenic and have been withdrawn (tegaserod) or are of very limited use (cisapride, only available with restrictions in the USA). Prucalopride is a potent 5HT-4 receptor agonist which has been approved for the treatment of constipation, but actually has whole-gut prokinetic properties [15]. In a randomized-controlled study in patients with chronic intestinal pseudo-obstruction, prucalopride significantly improved their symptoms, especially bloating and pain [61]. It is generally well tolerated and orally administered which facilitates ambulatory therapy.
Motilin agonists, such as erythromycin, induce gastric phases III which progress to the small bowel during fasting [59, 62]. Hence, it is particularly useful to accelerate gastric evacuation of retained debris in gastroparesis. However, a study comparing the effect before and after a meal has shown that in the postprandial period, erythromycin actually inhibits intestinal motility [63]. Camicinal is a new motilin agonist that has shown to accelerate gastric emptying, but did not have significant effects on small bowel or colonic transit time in a recent small study in healthy volunteers [64]. Clinical experience with camicinal is lacking.
Another new category of prokinetics agents are ghrelin agonists. Ghrelin induces gastric contractions and phase III activity in the intestine but has very short half-life [65, 66]. Synthetic peptides have been developed and shown to decrease postoperative ileus in animals [67]. The recently developed drug relamorelin is a synthetic ghrelin agonist that has been shown to increase antral contractions and to stimulate propagated contractions in the colon [68, 69]. There is still no clinical experience with this class of prokinetics.
Neurostimulation
Electrical stimulation of vagal efferents has the potential to activate cholinergic myenteric neurons in animal models [70]. Implantable devices have been developed for the treatment of refractory epilepsy and treatment resistant depression. Recently, a transcutaneous vagus nerve stimulator has been developed and has shown to stimulate gastroduodenal motility, but no clinical data with this device is available yet [71]. Sacral nerve stimulation has shown some efficacy in reducing symptoms of diarrhea-predominant and mixed IBS. However, it has no detectable effect on small intestinal transit patterns [72, 73].
Transplantation and Palliative Surgery
Severe intestinal dysmotility can lead to intestinal failure, which has recently been defined as “the reduction of gut function below the minimum necessary for the absorption of macronutrients and/or water and electrolytes, such that intravenous supplementation is required to maintain health and/or growth” [74]. In these extreme cases, patients should be placed on home parenteral nutrition (HPN). Intestinal transplantation is a last resource therapeutic option for patients unsuitable for HPN or when the underlying intestinal disease implies a high mortality rate [75••]. Whether intestinal transplantation should be offered to young patients unwilling to accept HPN should be evaluated on a careful case-by-case basis because long-term outcomes after transplantation remain unfavorable [76, 77].
In selected cases with marked intestinal atony and dilatation, a number of surgical techniques directed to prevent stasis and intraluminal pooling are available. Especially in children, these techniques have been able to partially reverse intestinal failure. They are generally called autologous intestinal reconstruction techniques and include tapering enteroplasty, the LILT and the STEP procedures [74]. In adults, experience with these palliative surgical approaches is very limited. However, insertion of venting catheters in the dilated upper small bowel to decompress it or ileostomy to facilitate emptying may be employed in selected cases.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance ••Of major importance
• Deloose E, Janssen P, Depoortere I, Tack J, et al. Nat Rev Gastroenterol Hepatol. 2012;9(5):271–85. A current and comprehensive review of the intestinal migrating motor complex
Deloose E, Vos R, Janssen P, Van den Bergh O, Van Oudenhove L, Depoortere I, et al. The motilin receptor agonist erythromycin stimulates hunger and food intake through a cholinergic pathway. Am J Clin Nutr. 2016;103(3):730–7.
Di Nardo G, Di Lorenzo C, Lauro A, Stanghellini V, Thapar N, Karunaratne TB, et al. Chronic intestinal pseudo-obstruction in children and adults: diagnosis and therapeutic options. Neurogastroenterol Motil. 2016;
Cogliandro RF, Antonucci A, De Giorgio R, Barbara G, Cremon C, Cogliandro L, et al. Patient-reported outcomes and gut dysmotility in functional gastrointestinal disorders. Neurogastroenterol Motil. 2011;23(12):1084–91.
Malagelada JR, Stanghellini V. Manometric evaluation of functional upper gut symptoms. Gastroenterology. 1985;88(5 Pt 1):1223–31.
Stanghellini V, Camilleri M, Malagelada JR. Chronic idiopathic intestinal pseudo-obstruction: clinical and intestinal manometric findings. Gut. 1987;28(1):5–12.
Accarino Garaventa AM, De Giorgio R, Cogliandro R, Malagelada C, Gori A, Malagelada JR, et al. Diagnosis of enteric dysmotility: are manometric disturbances predicable of hystopathological findings? Neurogastroenterol Motil. 2012;24:100.
Rao SS, Camilleri M, Hasler WL, Maurer AH, Parkman HP, Saad R, et al. Evaluation of gastrointestinal transit in clinical practice: position paper of the American and European Neurogastroenterology and Motility Societies. Neurogastroenterol Motil. 2011;23(1):8–23.
Miller MA, Parkman HP, Urbain JL, Brown KL, Donahue DJ, Knight LC, et al. Comparison of scintigraphy and lactulose breath hydrogen test for assessment of orocecal transit: lactulose accelerates small bowel transit. Dig Dis Sci. 1997;42(1):10–8.
Savarino E, Savarino V, Fox M, Di Leo G, Furnari M, Marabotto E, et al. Measurement of oro-caecal transit time by magnetic resonance imaging. Eur Radiol. 2015;25(6):1579–87.
Yu D, Cheeseman F, Vanner S. Combined oro-caecal scintigraphy and lactulose hydrogen breath testing demonstrate that breath testing detects oro-caecal transit, not small intestinal bacterial overgrowth in patients with IBS. Gut. 2011;60(3):334–40.
Roland BC, Ciarleglio MM, Clarke JO, Semler JR, Tomakin E, Mullin GE, et al. Small intestinal transit time is delayed in small intestinal bacterial overgrowth. J Clin Gastroenterol. 2015;49(7):571–6.
Lin EC, Massey BT. Scintigraphy demonstrates high rate of false-positive results from glucose breath tests for small bowel bacterial overgrowth. Clin Gastroenterol Hepatol. 2016;14(2):203–8.
Camilleri M, Brown M, Malagelada J. Impaired transit of chyme in chronic intestinal pseudo-obstruction. Correction by cisapride1986. 619–26 p.
Bouras EP, Camilleri M, Burton DD, Thomforde G, McKinzie S, Zinsmeister AR. Prucalopride accelerates gastrointestinal and colonic transit in patients with constipation without a rectal evacuation disorder. Gastroenterology. 2001;120(2):354–60.
Wang YT, Mohammed SD, Farmer AD, Wang D, Zarate N, Hobson AR, et al. Regional gastrointestinal transit and pH studied in 215 healthy volunteers using the wireless motility capsule: influence of age, gender, study country and testing protocol. Aliment Pharmacol Ther. 2015;42(6):761–72.
Rao SS, Kuo B, McCallum RW, Chey WD, DiBaise JK, Hasler WL, et al. Investigation of colonic and whole-gut transit with wireless motility capsule and radiopaque markers in constipation. Clin Gastroenterol Hepatol. 2009;7(5):537–44.
Sadik R, Abrahamsson H, Stotzer PO. Gender differences in gut transit shown with a newly developed radiological procedure. Scand J Gastroenterol. 2003;38(1):36–42.
Strid H, Simrén M, Störsrud S, Stotzer PO, Sadik R. Effect of heavy exercise on gastrointestinal transit in endurance athletes. Scand J Gastroenterol. 2011;46(6):673–7.
Kalaitzakis E, Sadik R, Holst JJ, Ohman L, Björnsson E. Gut transit is associated with gastrointestinal symptoms and gut hormone profile in patients with cirrhosis. Clin Gastroenterol Hepatol. 2009;7(3):346–52.
Sadik R, Abrahamsson H, Kilander A, Stotzer PO. Gut transit in celiac disease: delay of small bowel transit and acceleration after dietary treatment. Am J Gastroenterol. 2004;99(12):2429–36.
Chaddock G, Lam C, Hoad CL, Costigan C, Cox EF, Placidi E, et al. Novel MRI tests of orocecal transit time and whole gut transit time: studies in normal subjects. Neurogastroenterol Motil. 2014;26(2):205–14.
Sadik R, Stotzer PO, Simrén M, Abrahamsson H. Gastrointestinal transit abnormalities are frequently detected in patients with unexplained GI symptoms at a tertiary centre. Neurogastroenterol Motil. 2008;20(3):197–205.
Camilleri M, McKinzie S, Busciglio I, Low PA, Sweetser S, Burton D, et al. Prospective study of motor, sensory, psychologic, and autonomic functions in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2008;6(7):772–81.
Bonapace ES, Maurer AH, Davidoff S, Krevsky B, Fisher RS, Parkman HP. Whole gut transit scintigraphy in the clinical evaluation of patients with upper and lower gastrointestinal symptoms. Am J Gastroenterol. 2000;95(10):2838–47.
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160–74.
• Dinning PG, Wiklendt L, Maslen L, Patton V, Lewis H, Arkwright JW, et al. Colonic motor abnormalities in slow transit constipation defined by high resolution, fibre-optic manometry. Neurogastroenterol Motil. 2015;27(3):379–88. Applicability of high-resolution manometry to enhance the yield of intestinal motility measurement
Castedal M, Abrahamsson H. High-resolution analysis of the duodenal interdigestive phase III in humans. Neurogastroenterol Motil. 2001;13(5):473–81.
Lindberg G. High-resolution manometry changes our views of gastrointestinal motility. Neurogastroenterol Motil. 2013;25(10):780–2.
Segui S, Drozdzal M, Pascual G, Radeva P, Malagelada C, Azpiroz F, et al. Generic feature learning for wireless capsule endoscopy analysis. Comput Biol Med. 2016;79:163–72.
Segui S, Drozdzal M, Zaytseva E, Malagelada C, Azpiroz F, Radeva P, et al. Detection of wrinkle frames in endoluminal videos using betweenness centrality measures for images. IEEE J Biomed Health Inform. 2014;18(6):1831–8.
Seguí S, Drozdzal M, Vilariño F, Malagelada C, Azpiroz F, Radeva P, et al. Categorization and segmentation of intestinal content frames for wireless capsule endoscopy. IEEE Trans Inf Technol Biomed. 2012;16(6):1341–52.
Drozdzal M, Seguí S, Malagelada C, Azpiroz F, Vitrià J, Radeva P. Interactive labeling of WCE images. Pattern Recognition and Image Analysis. 2011:143–50.
Segui S, Igual L, Radeva P, Malagelada C, Azpiroz F, Vitria J. Industrial and medical applications of pattern recognition—a semi-supervised learning method for motility disease diagnostic. Lect Notes Comput Sci. 2007;4789:773–82.
Malagelada C, de Iorio F, Azpiroz F, Accarino A, Segul S, Radeva P, et al. New insight into intestinal motor function via noninvasive endoluminal image analysis. Gastroenterology. 2008;135(4):1155–62.
Malagelada C, Seguí S, Mendez S, Drozdzal M, Vitria J, Radeva P, et al. Functional gut disorders or disordered gut function? Small bowel dysmotility evidenced by an original technique. Neurogastroenterology & Motility. 2012.
• Malagelada C, Drozdzal M, Seguí S, Mendez S, Vitrià J, Radeva P, et al. Classification of functional bowel disorders by objective physiological criteria based on endoluminal image analysis. Am J Physiol Gastrointest Liver Physiol. 2015;309(6):G413–9. Intestinal dysmotility in patients with functional bowel disorders can be objectively detected with a new non-invasive methodology
Drozdzal M, Seguí S, Radeva P, Malagelada C, Azpiroz F, Vitrià J. Motility bar: a new tool for motility analysis of endoluminal videos. Comput Biol Med. 2015;65:320–30.
Drozdzal M, Seguí S, Vitrià J, Malagelada C, Azpiroz F, Radeva P. Adaptable image cuts for motility inspection using WCE. Comput Med Imaging Graph. 2013;37(1):72–80.
Sihuay D, Malagelada C, Molero X, Drozdzal M, Soriano SM, Nieto A, et al. Structural and functional abnormalities of the small bowel in patients with common variable immunodeficiency. Gastroenterology. 2015;148(4):S667.
Malagelada C, Sihuay D, Bendezú A, Montenegro A, Molero X, Nieto A, et al. External and internal gut imaging for morpho-functional evaluation of the gut. United European Gastroenterology Journal. 2016;4(5_suppl):A157–720.
Barba E, Quiroga S, Accarino A, Lahoya EM, Malagelada C, Burri E, et al. Mechanisms of abdominal distension in severe intestinal dysmotility: abdomino-thoracic response to gut retention. Neurogastroenterol Motil. 2013;25(6):e389–94.
Villoria A, Azpiroz F, Burri E, Cisternas D, Soldevilla A, Malagelada JR. Abdomino-phrenic dyssynergia in patients with abdominal bloating and distension. Am J Gastroenterol. 2011;106(5):815–9.
Barba E, Burri E, Accarino A, Cisternas D, Quiroga S, Monclus E, et al. Abdominothoracic mechanisms of functional abdominal distension and correction by biofeedback. Gastroenterology. 2015;148(4):732–9.
Marciani L, Cox EF, Hoad CL, Pritchard S, Totman JJ, Foley S, et al. Postprandial changes in small bowel water content in healthy subjects and patients with irritable bowel syndrome. Gastroenterology. 2010;138(2):469–77. 77.e1.
Pritchard SE, Garsed KC, Hoad CL, Lingaya M, Banwait R, Thongborisute W, et al. Effect of experimental stress on the small bowel and colon in healthy humans. Neurogastroenterol Motil. 2015;27(4):542–9.
Lam C, Chaddock G, Marciani Laurea L, Costigan C, Cox E, Hoad C, et al. Distinct abnormalities of small bowel and regional colonic volumes in subtypes of irritable bowel syndrome revealed by MRI. Am J Gastroenterol. 2017;112(2):346–55.
Bickelhaupt S, Froehlich JM, Cattin R, Raible S, Bouquet H, Bill U, et al. Software-assisted quantitative analysis of small bowel motility compared to manual measurements. Clin Radiol. 2014;69(4):363–71.
Menys A, Hamy V, Makanyanga J, Hoad C, Gowland P, Odille F, et al. Dual registration of abdominal motion for motility assessment in free-breathing data sets acquired using dynamic MRI. Phys Med Biol. 2014;59(16):4603–19.
Khalaf A, Hoad CL, Spiller RC, Gowland PA, Moran GW, Marciani L. Magnetic resonance imaging biomarkers of gastrointestinal motor function and fluid distribution. World J Gastrointest Pathophysiol. 2015;6(4):140–9.
Akerman A, Mansson S, Fork FT, Leander P, Ekberg O, Taylor S, et al. Computational postprocessing quantification of small bowel motility using magnetic resonance images in clinical practice: an initial experience. J Magn Reson Imaging. 2016;44(2):277–87.
Hahnemann ML, Nensa F, Kinner S, Kohler J, Gerken G, Umutlu L, et al. Quantitative assessment of small bowel motility in patients with Crohn’s disease using dynamic MRI. Neurogastroenterol Motil. 2015;27(6):841–8.
Bickelhaupt S, Pazahr S, Chuck N, Blume I, Froehlich JM, Cattin R, et al. Crohn’s disease: small bowel motility impairment correlates with inflammatory-related markers C-reactive protein and calprotectin. Neurogastroenterol Motil. 2013;
Menys A, Atkinson D, Odille F, Ahmed A, Novelli M, Rodriguez-Justo M, et al. Quantified terminal ileal motility during MR enterography as a potential biomarker of Crohn’s disease activity: a preliminary study. Eur Radiol. 2012;22(11):2494–501.
Fuyuki A, Ohkubo H, Higurashi T, Iida H, Inoh Y, Inamori M, et al. Clinical importance of cine-MRI assessment of small bowel motility in patients with chronic intestinal pseudo-obstruction: a retrospective study of 33 patients. J Gastroenterol. 2016.
• Menys A, Butt S, Emmanuel A, Plumb AA, Fikree A, Knowles C, et al. Comparative quantitative assessment of global small bowel motility using magnetic resonance imaging in chronic intestinal pseudo-obstruction and healthy controls. Neurogastroenterol Motil. 2016;28(3):376–83. Non-invasive detection of intestinal dysmotility in patients with chronic intestinal pseudo-obstruction by dynamic MRI.
Ohkubo H, Kessoku T, Fuyuki A, Iida H, Inamori M, Fujii T, et al. Assessment of small bowel motility in patients with chronic intestinal pseudo-obstruction using cine-MRI. Am J Gastroenterol. 2013;108(7):1130–9.
Ambartsumyan L, Flores A, Nurko S, Rodriguez L. Utility of Octreotide in advancing enteral feeds in children with chronic intestinal pseudo-obstruction. Paediatr Drugs. 2016;18(5):387–92.
Tack J, Deloose E, Ang D, Scarpellini E, Vanuytsel T, Van Oudenhove L, et al. Motilin-induced gastric contractions signal hunger in man. Gut. 2016;65(2):214–24.
Soudah HC, Hasler WL, Owyang C. Effect of octreotide on intestinal motility and bacterial overgrowth in scleroderma. N Engl J Med. 1991;325(21):1461–7.
Emmanuel A, Cools M, Vandeplassche L, Kerstens R. Prucalopride improves bowel function and colonic transit time in patients with chronic constipation: an integrated analysis. Am J Gastroenterol. 2014;109(6):887–94.
Cucchiara S, Minella R, Scoppa A, Emiliano M, Calabrese F, Az-Zeqeh N, et al. Antroduodenal motor effects of intravenous erythromycin in children with abnormalities of gastrointestinal motility. J Pediatr Gastroenterol Nutr. 1997;24(4):411–8.
Medhus AW, Bondi J, Gaustad P, Husebye E. Low-dose intravenous erythromycin: effects on postprandial and fasting motility of the small bowel. Aliment Pharmacol Ther. 2000;14(2):233–40.
Hobson R, Farmer AD, Dewit OE, O’Donnell M, Hacquoil K, Robertson D, et al. The effects of camicinal, a novel motilin agonist, on gastro-esophageal function in healthy humans-a randomized placebo controlled trial. Neurogastroenterol Motil. 2015;27(11):1629–37.
Swartz EM, Browning KN, Travagli RA, Holmes GM. Ghrelin increases vagally mediated gastric activity by central sites of action. Neurogastroenterol Motil. 2014;26(2):272–82.
Tack J, Depoortere I, Bisschops R, Delporte C, Coulie B, Meulemans A, et al. Influence of ghrelin on interdigestive gastrointestinal motility in humans. Gut. 2006;55(3):327–33.
Venkova K, Fraser G, Hoveyda HR, Greenwood-Van MB. Prokinetic effects of a new ghrelin receptor agonist TZP-101 in a rat model of postoperative ileus. Dig Dis Sci. 2007;52(9):2241–8.
Acosta A, Camilleri M, Busciglio I, Boldingh A, Nelson AD, Burton D. Short-term effects of Relamorelin on descending colon motility in chronic constipation: a randomized. Controlled Trial Dig Dis Sci. 2016;61(3):852–60.
Nelson AD, Camilleri M, Acosta A, Busciglio I, Linker Nord S, Boldingh A, et al. Effects of ghrelin receptor agonist, relamorelin, on gastric motor functions and satiation in healthy volunteers. Neurogastroenterol Motil. 2016;28(11):1705–13.
Matteoli G, Gomez-Pinilla PJ, Nemethova A, Di Giovangiulio M, Cailotto C, van Bree SH, et al. A distinct vagal anti-inflammatory pathway modulates intestinal muscularis resident macrophages independent of the spleen. Gut. 2014;63(6):938–48.
Frokjaer JB, Bergmann S, Brock C, Madzak A, Farmer AD, Ellrich J, et al. Modulation of vagal tone enhances gastroduodenal motility and reduces somatic pain sensitivity. Neurogastroenterol Motil. 2016;28(4):592–8.
Fassov JL, Lundby L, Laurberg S, Buntzen S, Krogh K. A randomized, controlled, crossover study of sacral nerve stimulation for irritable bowel syndrome. Ann Surg. 2014;260(1):31–6.
Fassov J, Lundby L, Worsoe J, Buntzen S, Laurberg S, Krogh K. A randomised, controlled study of small intestinal motility in patients treated with sacral nerve stimulation for irritable bowel syndrome. BMC Gastroenterol. 2014;14:111.
Pironi L, Arends J, Bozzetti F, Cuerda C, Gillanders L, Jeppesen PB, et al. ESPEN guidelines on chronic intestinal failure in adults. Clin Nutr. 2016;35(2):247–307.
•• Pironi L, Joly F, Forbes A, Colomb V, Lyszkowska M, Baxter J, et al. Long-term follow-up of patients on home parenteral nutrition in Europe: implications for intestinal transplantation. Gut. 2011;60(1):17–25. This study confirms that home parenteral nutrition (HPN) is the treatment of choice for intestinal failure and suggests that only patients with HPN-associated liver failure or invasive desmoids should be referred for a life-saving intestinal transplant
Lacaille F, Irtan S, Dupic L, Talbotec C, Lesage F, Colomb V, et al. Twenty-eight years of intestinal transplantation in Paris: experience of the oldest European center. Transpl Int. 2017;30(2):178–86.
Brandt CF, Hvistendahl M, Naimi RM, Tribler S, Staun M, Brobech P, et al. Home parenteral nutrition in adult patients with chronic intestinal failure: the evolution over 4 decades in a tertiary referral center. JPEN J Parenter Enteral Nutr. 2016;
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Juan R. Malagelada has patents issued to Given Imaging Ltd. (US 8611621 B2, US 8422755 B2, US 20130188845 A1).
Carolina Malagelada reports grants from Given Imaging and patents issued to Given Imaging Ltd. (US8611621 B2, US8422755 B2, WO2013114361,WO2015170321 A1).
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Small Intestine
Rights and permissions
About this article
Cite this article
Malagelada, C., Malagelada, J.R. Small Bowel Motility. Curr Gastroenterol Rep 19, 26 (2017). https://doi.org/10.1007/s11894-017-0565-x
Published:
DOI: https://doi.org/10.1007/s11894-017-0565-x