Abstract
There is growing evidence for the role of several natural products as either useful agents or adjuncts in the management of functional GI disorders (FGIDs). In this review, we examine the medical evidence for three such compounds: chili, a culinary spice; curcumin, another spice and active derivative of a root bark; and prebiotics, which are nondigestible food products. Chili may affect the pathogenesis of abdominal pain especially in functional dyspepsia and cause other symptoms. It may have a therapeutic role in FGIDs through desensitization of transient receptor potential vanilloid-1 receptor. Curcumin, the active ingredient of turmeric rhizome, has been shown in several preclinical studies and uncontrolled clinical trials as having effects on gut inflammation, gut permeability and the brain–gut axis, especially in FGIDs. Prebiotics, the non-digestible food ingredients in dietary fiber, may serve as nutrients and selectively stimulate the growth and/or activity of certain colonic bacteria. The net effect of this change on colonic microbiota may lead to the production of acidic metabolites and other compounds that help to reduce the production of toxins and suppress the growth of harmful or disease-causing enteric pathogens. Although some clinical benefit in IBS has been shown, high dose intake of prebiotics may cause more bloating from bacterial fermentation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Between 70 and 84 % of irritable bowel syndrome (IBS) patients report aggravation of symptoms after food ingestion, and 62 % of them either limit or exclude foods from their diet [1, 2]. Food intolerance is associated with more severe IBS symptoms and this reduces the quality of life [1]. A recent study also demonstrated that high fermentable carbohydrate content or fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) were associated with more bloating, abdominal pain and unsatisfied stool form among IBS patients but not in healthy volunteers [3].
On the other hand, dietary fiber, which is described as nondigestible carbohydrates, are essential for promoting normal bowel movements, and a subgroup of nondigestible carbohydrate- prebiotics has been shown to promote health benefit through modulation of gut microbiota. In addition, chili and curcumin, which are spices commonly consumed by populations in several parts of the world, not only serve as flavor enhancers in daily food but have also long been recognized for medicinal benefits on gastrointestinal health. They have been included in folk or home remedies for treatment of abdominal pain and bloating since ancient times. In this review, we will focus on the evidence of the effects of two common spices (chili pepper and curcumin) and a subgroup of nondigestible carbohydrate-prebiotics on gastrointestinal function in health and functional gastrointestinal disorders (FGID).
Chili Pepper and Capsaicin Receptors
Chili is a common ingredient in Asian and Latin American food. The average daily chili consumption by Asians is 2.5–8 g/person which is 10–300 times higher than by Europeans and Americans [4, 5]. Capsaicin is an active component of chili that triggers a painful and burning sensation in the human gut via transient receptor potential vanilloid-1 (TRPV1) receptors which are expressed throughout the digestive tract mucosa with variable distribution in each organ [6, 7•]. Studies in visceral hypersensitivity conditions, including non-erosive reflux disease, rectal hypersensitivity, fecal urgency and inflammatory gut mucosa including symptomatic esophagitis, have revealed more TRPV1-immunoreactive fibers or TRPV1 mRNA and protein expression than in healthy controls [8, 9]. TRPV1 receptors can also be activated by heat, acid pH, ethanol, and mechanical distension [7], and stimulate the release of several peptides, including substance P and calcitonin gene-related peptide [10]. Interestingly, repeated exposure to capsaicin can desensitize this receptor, and this not only causes the receptor to become refractory but the whole nerve fiber that subserves the receptor may also become refractory to other nociceptive and mechanical stimuli [11]. Thus, this effect provides a broader modification of painful and burning symptoms during food ingestion than the effects of specific capsaicin antagonists which inhibit only a specific group of receptors. Therefore, using chili, a natural capsaicin agonist, for providing relief to patients with chronic gastrointestinal symptoms may provide a broader effect than synthetic/specific capsaicin receptor antagonists in modifying the gut symptoms. In addition, capsaicin receptor antagonist(s) are still in development and may cause severe side effects particularly hyperthermia [12].
Effects of Capsaicin on Esophageal Sensation and Motor Function
Studies in healthy volunteers have reported that single dose intra-esophageal capsaicin infusion induced heartburn in a dose-dependent manner [13–15]. After repeated exposure, the desensitizing properties of capsaicin occurred rapidly and caused a significant decrease in heartburn intensity [16]. Desensitization to chemical stimuli may result from dephosphorylation of TRPV1 by calcium-induced calcineurin activation [17]. The recovery time from desensitization is dependent on the stimulus intensity and interstimulus interval [18].
Regarding esophageal motor function, an animal study demonstrated the role of capsaicin-sensitive neurons in esophageal myenteric plexus on controlling peristalsis [19]. In healthy volunteers, single-dose esophageal capsaicin infusion significantly increased the amplitude of distension-induced secondary peristalsis compared with placebo, and a desensitization effect on distension-induced secondary peristalsis as well as heartburn sensation were also demonstrated after repeated capsaicin infusion at the esophagus for two consecutive sessions with at least a 1-h time interval [13, 16]. A previous study also demonstrated comparable distension thresholds for secondary peristalsis as a consequence of hydrochloric acid (0.1 N) or 0.84 mg capsaicin esophageal infusion [13]. A histological study of the lower esophageal sphincter tissue in humans observed no evidence for capsaicin-sensitive axon collateral reflexes [20]. However, manometric studies on the effects of capsaicin on the lower esophageal sphincter in healthy volunteers have demonstrated conflicting results [21, 22].
Effects of Capsaicin on Gastric Sensation and Motor Function
In healthy volunteers study using the barostat technique, a single-dose capsaicin (red pepper sauce) infusion into the proximal stomach during a fasting period decreased proximal gastric tone, increased proximal stomach compliance and also increased proximal gastric distension sensitivity compared to placebo [23]. Gastric electrical activity study showed a significant increase in tachygastric activity and significantly delayed liquid gastric emptying after single-dose intraesophageal capsaicin infusion compared to placebo [21]. Regarding gastric sensation, the ingestion of capsaicin capsules induced gastric sensations of pressure, heartburn, and warmth in healthy volunteers [24]. Gastric mucosal protection of capsaicin has been demonstrated in an animal model by the release of neurotransmitters including calcitonin gene-related peptide and nitric oxide through stimulation of TRPV1 receptors. In rat and dog models, capsaicin induced calcitonin gene-related peptide release and inhibited gastric secretion [25, 26]. It was also found to induce the release of a vasodilator, nitric oxide, which may be beneficial for gastric mucosal blood perfusion [26]. Gastroprotective effects of capsaicin in human studies are limited and have not been demonstrated in a randomized trial.
Clinical Studies of Capsaicin on Gastro-esophageal Reflux Disease and Dyspepsia
Clinical studies on the efficacy of chili or capsaicin receptor antagonists on heartburn symptoms in gastro-esoesophageal reflux disease and dyspepsia are limited. Studies in Asian countries with high chili consumption rates have demonstrated a low prevalence of heartburn symptoms in GERD [27, 28]. A small randomized cross-over study comparing chest pain, heartburn, epigastric burning, and epigastric pain symptoms induced by intraesophageal capsaicin perfusion or normal saline perfusion among 17 healthy volunteers and 31 GERD patients (10 non-erosive reflux disease, 11 erosive esophagitis and 10 Barrett's esophagus) reported significantly higher esophageal and gastric symptoms in the GERD group compared to the control group. Thirty minutes after saline or capsaicin infusion, an acid perfusion test of HCl was performed. The results showed that symptoms in response to acid perfusion in both healthy volunteers and GERD patients reduced after capsaicin infusion, especially in the Barrett's esophagus group [14]. A study from our center in NERD patients showed that a single-dose chili ingestion increased postprandial acid refluxes which were associated with increased food retention in the stomach during the first hour after ingestion compared to placebo [29]. A subsequent study confirmed these observations and showed that the chili-induced food retention resulted from exaggerated gastric accommodation which was observed only in NERD patients but not in healthy volunteers [30]. This suggests that an abnormal TRPV1 pathway may mediate gastric accommodation and this may play a role in the pathophysiology of postprandial gastroesophageal reflux. In a preliminary cross-over study that compared the therapeutic effects of chili and placebo administered in gelatin capsules to 8 NERD patients, we also showed desensitization effects after red chili capsule (2.1 mg capsaicin/day) ingestion for 6 weeks. After 6 weeks, the red chili significantly decreased total reflux symptom scores, heartburn symptom scores, and food regurgitation symptom scores when compared to placebo [31].
The effects of capsaicin on patients with esophageal motility disorders have been reported. In a randomized cross-over study of 12 mild reflux esophagitis patients with severe ineffective esophageal motility, single-dose intraesophageal capsaicin infusion increased the amplitude of esophageal contractions when compared to placebo. However, the peristalsis velocity and the lower esophageal sphincter basal tone remained unchanged [32]. Also, a study in patients with Barrett’s esophagus showed no demonstrable effects on esophageal motility [33]. The effects of chronic capsaicin ingestion on esophageal motility have not been reported.
Gut hypersensitivity to capsaicin has been demonstrated in functional dyspepsia (FD) patients. Randomized double-blind controlled trials in FD patients have revealed that capsaicin ingestion induced more nausea, flutter-like sensations in the stomach, warmth and abdominal pain than placebo. This effect was not different between FD subtypes and most patients reported that these symptoms were similar to what they had experienced before the study [34•]. In a recent study on the effects of spicy meals on gastrointestinal symptoms in FD patients, a greater proportion of FD patients reported that spicy meals induced more abdominal burning symptoms in their daily life in relation to healthy controls. However, in this study, epigastric pain syndrome-subtype patients had a greater prevalence of spicy meal-induced abdominal burning symptoms compared to postprandial distress syndrome-subtype patients [35]. There is limited information regarding the effect of chronic capsaicin ingestion in FD. A randomized double-blind controlled study in 30 functional dyspepsia patients without GERD or IBS using 2.5 g red pepper powder capsules (capsaicin 1.75 mg) ingestion for 5 weeks demonstrated that red pepper significantly improved overall symptoms of epigastric pain, fullness, and nausea but not epigastric burning, bloating, and belching compared to placebo. These symptom improvements were significantly observed after chili ingestion for 3 weeks. Seven of 15 patients who received chili reported abdominal pain and/or discomfort during the first week, but these side effects improved after a few days [36].
Effects of Capsaicin on Intestinal Sensation and Motor Function
In healthy volunteers, a small intestinal capsaicin infusion induced abdominal pain, cramping, pressure, and nausea, and 3-day capsaicin ingestion increased rectal sensitivity to urgency [24, 37]. Along the small intestine, the duodenum was more sensitive to capsaicin and induced more intense symptoms compared to the distal part [24]. Desensitization after chronic capsaicin ingestion in healthy humans can also be demonstrated by capsaicin administration and balloon distension of the duodenum [11]. Regarding colonic motility, capsaicin-induced giant migrating contractions and defecation have been shown in an animal study [38], although another study reported no effect of capsaicin on colonic transit in IBS-diarrhea and healthy humans [39, 40].
Clinical Studies of Capsaicin on IBS
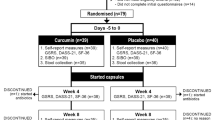
An increase in TRPV1-expressing nerve fibers were seen in the rectal mucosa of patients with rectal hypersensitivity [9] and significantly increased TRPV1-immunoreactive nerve fibers were seen in sigmoid mucosa of IBS patients when compared to controls [41]. Some studies have revealed that IBS patients had gut hypersensitivity to capsaicin, and that their reported symptoms included more severe abdominal burning and pain after ingestion of spicy meals than healthy volunteers [39]. Acute chili ingestion in IBS patients increased abdominal burning, pain, and discomfort as well as increased rectal sensitivity compared to placebo [39, 42]. Desensitization effects of capsaicin ingestion in IBS patients were demonstrated in two randomized controlled trials [43, 44]. The first study revealed that 6-week red pepper ingestion (capsaicin 2 mg/day), not placebo, significantly decreased abdominal pain and bloating compared to the baseline [44]. The second study by Aniwan et al. reported that 6-week ingestion of 2.1 g. chili/day in gelatin and enteric-coated capsules in 16 IBS-diarrhea patients significantly reduced spicy meal-induced abdominal burning symptoms compared to placebo. In addition, chronic chili ingestion significantly increased rectal sensory thresholds in response to balloon distention without significant effects on rectal compliance [43]. The effects of single-dose chili administration on gastrointestinal sensation and motility are shown in Table 1. Table 2 shows studies demonstrated desensitization effects of repeated chili administration in GERD and FGIDs.
In conclusion, there has been increasing evidence to support the role of capsaicin in the pathogenesis of abdominal pain and burning symptoms in functional GI disorders. The therapeutic role of chili pepper as a natural capsaicin for the desensitization of capsaicin receptors in patients with functional dyspepsia, IBS and GERD is evolving.
Curcumin
Curcumin, the active ingredient of turmeric (Curcumin longa) rhizome, has been used in Asia as a herbal remedy for a variety of diseases. Like chili, turmeric is commonly used in Asian cuisine to add yellow color, as a flavor, and as a preservative. Some promising effects of curcumin have been observed including the treatment of chronic inflammatory conditions such as arthritis, uveitis, and inflammatory bowel disease, leading to improved metabolic parameters involving atherosclerosis and diabetes. In some cases, it has been found to aid in cancer prevention and treatment [45, 46]. The effects of turmeric on the gastrointestinal tract have been widely described in folk medicine including the treatment of abdominal pain and flatulence and in appetite promotion without considerable side effects. Although the molecular mechanisms of action have been studied, clinical trials on gastrointestinal conditions are limited.
Mechanisms of the Action of Curcumin on the Gastrointestinal Tract
Anti-inflammatory Effect and the Effect on Gut Permeability
Gut inflammation has been recognized in the pathogenesis of FGIDs. Curcumin has been shown in preclinical studies to modulate several inflammatory mediators. The activity of proinflammatory enzymes, including cyclooxygenase-2, 5-lipoxygenase, inducible nitric oxide synthase (iNOS) enzymes, tumor necrosis factor-alpha, interleukin (IL) -1, -2, -6, -8 and -12 have been shown to be inhibited by curcumin. It can also downregulate the expression of various cell surface adhesion molecules that have been linked with inflammation [47–49]. Recent studies have demonstrated the effects of curcumin in animal models of colitis through the suppression of Toll-like receptor (TLR) 4, nuclear factor-kappa B (NFkB), and signal transducers and activators of the transcription 3 signaling pathway [50–52]. In an animal colitis model, there was no significant difference in IL 27, TLR4, and NFkB protein expression inhibition between curcumin and sulfasalazine-treated groups, whereas curcumin significantly decreased the disease activity index faster than sulfasalazine [51]. In addition, an in vitro study demonstrated protective effects of curcumin on oxidative stress-induced intestinal barrier disruption in human intestinal epithelial cells by heme oxygenase 1 induction [53]. Since disruption of epithelial tight junctions followed by the loss of barrier function and low-grade mucosal inflammation has been described in the pathogenesis of FGIDs, particularly IBS, this might support the therapeutic role of curcumin in these patients.
Antibacterial Effect
Curcumin inhibits most metronidazole-resistant H. pylori growth in vitro with MIC values between 5 and 50 μg/mL irrespective of the genetic strains, and was also highly effective in the eradication of H. pylori from infected mice [54, 55]. The mechanism of H.pylori growth inhibition of curcumin may differ from antibiotics. Curcumin inhibits the assembly dynamics of FtsZ (a bacterial protofilament), which polymerizes to form a Z ring that orchestrates bacterial cell division [56] and inhibits the shikimate pathway that is necessary for the synthesis of aromatic amino acids in bacteria [57]. The effect of curcumin on gut microbiota has not been explored. Just one small study in healthy volunteers has reported that ingesting rice with turmeric significantly increased breath-hydrogen concentrations compared to rice without turmeric. This may suggest that curcumin increases carbohydrate fermentation by colonic bacteria [58].
Effect on the Brain–Gut Axis
In animal studies, curcumin significantly modulated HPA activity, up-regulated serotonin (5-HT1A) mRNA and brain-derived neurotrophic factor protein levels in the hippocampus which represented a possible antidepressive effect which might be beneficial to FGIDs patients [59–61]. In regard to visceral pain perception, curcumin has been shown to have antinociceptive effects in animal models. Chronic curcumin ingestion was able to attenuate intraperitoneal acetic acid-induced visceral pain [62]. The antinociceptive mechanism was demonstrated by antagonizing TRPV1 receptors, [63•] and this may be involved in the endogenous analgesic opioid system [62].
Effect on Gastrointestinal Motility
The effect of curcumin on human gastrointestinal motility has not been clearly demonstrated, but it has antispasmodic effects in animal models. In a chemically induced colitis animal, 21-day curcumin administration significantly reduced spontaneous intestinal contractions as well as contractions in response to atropine compared to placebo, and was independent of an anti-inflammatory effect [64]. Antispasmodic mechanisms appeared as a non-competitive inhibitor through cholinergic, histaminergic, and serotoninergic receptors and showed an antispasmodic effect on potassium-induced contractions in calcium channels [65]. Effects of curcumin on gastric function were demonstrated in diabetic gastroparesis rats [66]. In this study, chronic curcumin administration significantly accelerated gastric emptying and increased ghrelin levels in a dose-dependent manner. Asummary of curcumin effects on the pathogenesis of FGIDs is shown in Table 3.
Clinical Studies of Curcumin in Functional Gastrointestinal Disorders
Studies on curcumin efficacy in FGIDs patients are limited to uncontrolled and case series studies. An uncontrolled study showed a significant improvement in dyspeptic symptoms and a reduction of serologic signs of gastric inflammation at 2 months after a 7-day treatment by non-antibiotic therapy comprised of curcumin, lactoferrin, N-acetylcysteine, and pantoprazole despite the persistence of H.pylori infection [67].
Clinical trials of patients with major depression have shown that curcumin has antidepressant effects similar to fluoxetine [68, 69]. Although depression is prevalent among FGIDs patients, more studies are needed to elucidate the antidepressant benefits of curcumin in FGIDs.
Poor oral bioavailability is one major concern with the use of curcumin [70]. A study showed that crude turmeric, a precursor of curcumin, provided better bioavailability and had better effects on pro-inflammatory gene transcription than curcumin [71]. Structural modification, modulation of the route and medium of curcumin administration, and the blocking of metabolic pathways by concomitant administration with other agents to overcome its poor bioavailability is still being developed [72].
Regarding its safety profiles, curcumin is considerably safe with minimal side effects, which include diarrhea and nausea as well as increased serum alkaline phosphatase and lactate dehydrogenase levels [45]. Curcumin dosages of up to 8 g/day have been taken for 3 months without serious adverse events in clinical trials [73]. Nevertheless, more studies are required to evaluate its long-term toxicity.
Prebiotics
A prebiotic is defined as “a nondigestible food ingredient that beneficially affects the host by selectively stimulating the growth and/or activity of one or a limited number of bacteria in the colon, thusly improving host health” [74]. Although dietary fiber from fruits and vegetables are nondigestible, not all have prebiotic effects. Leeks, asparagus, chicory, garlic, artichoke, onions, wheat, bananas, oats, and soy beans contain inulin, fructo-oligosaccharides, and galacto-oligosaccharides as their major substrates and are considered prebiotics [74, 75]. They have been shown to stimulate growth of certain colonic microbiota that might benefit the host [74].
Product of Bacterial Fermentation and Effects on Host
Nondigestible carbohydrates that reach the colon are fermented to short chain fatty acids (SCFA), mainly acetate, propionate and butyrate. A number of other metabolites such as lactate, pyruvate, ethanol, and succinate as well as hydrogen, carbon dioxide, and methane gases are also produced. Of these, SCFA is considered to be beneficial to human health. It is rapidly absorbed and metabolized in muscles, kidneys, the heart and brain and serves as a tissue energy substrate [76]. Butyrate is one SCFA that is largely metabolized by colonic epithelial cells and mainly contributes to colonic tissue energy and growth of the colonic epithelium. It promotes normal colonic epithelial cell differentiation and proliferation [77]. Recent studies have demonstrated that butyrate may also play a role in gut immune homeostasis by facilitated extrathymic generation of regulatory T cells, which is the key in limiting inflammatory responses in the intestine [78, 79]. Almost all carbohydrates that reach the colon are fermented and provide substrates for colonic microbiota; however, stimulation of growth by these carbohydrates is nonspecific and they also stimulate some bacteria genera that ferment proteins and amino. The end product of these proteolyic bacteria are branch chain fatty acids, ammonia, amines and phenolic compounds which may be toxic to the host [80].
Prebiotics are non-digestible carbohydrates that selectively stimulate the growth of “specific bacteria” which prefer using saccharides as a primary substrate [81]. Lactobacillus and bifidobacterium are two colonic bacteria genera that have been widely established for the target of prebiotics. These two genera do not contain any known pathogens. They produce acetic acid and lactic acid as the major end-metabolites. An acidic luminal environment helps to reduce peptide degradation and the formation of amino acid end-product toxic compounds by other groups of bacteria and suppresses the growth of enteric pathogens. Their growth also leads to an increase in bacterial mass which consequently increases fecal mass to promote normal bowel movements. In addition, a genera Bifidobacterium is a dominant colonic bacteria in exclusive breast-feeding which may play a significant role in the immune defense mechanism in newborns [82, 83].
Clinical Studies of Prebiotics on Functional GI Disorders
Among FGIDs, there is significant evidence of the effects of gut microbiota in IBS pathogenesis. Alterations of gut microbiota composition and metabolites could contribute to IBS by increasing gut permeability, activating the mucosal immune response, increasing visceral sensitivity and altering intestinal motility [84]. Previous studies based on the analysis of fecal samples have demonstrated a decreased proportion of the genera Bifidobacterium and Lactobacillus in IBS patients in comparison to healthy subjects. However, there is still a lack of consensus regarding microbiota composition changes among IBS subtypes [85] and limited evidence to sufficiently report the prebiotic effect in IBS patients. A recent randomized controlled study that included 60 constipation, diarrhea and alternating subtype IBS patients to receive either trans-galactooligosaccharide 3.5 g/day, 7 g/day or placebo for 4 weeks in cross-over fashion showed that prebiotics significantly improved symptoms and increased fecal Bifidobacterium spp. and Eubacterium rectal/Clostridium coccoides proportion but decreased the proportion of the C. perfringens–hystolyticum subgroup and Bactriodes/Prevotella spp. A higher dose improved stool consistency, subjective global assessment and anxiety score but increased bloating symptoms and flatulence compared to a lower dose [86] (see Table 4). A randomized controlled study comparing 5 g short-chain fructo-oligosaccharides with placebo over 6 weeks in 105 patients with mild functional bowel disorders fulfilling the Rome II criteria of IBS, functional abdominal bloating, functional constipation or functional diarrhea showed that fructo-oligosaccharides improved symptoms, improved disease-related quality of life and the performance of daily activities compared to placebo [85]. Two other randomized controlled studies did not show prebiotic benefits in IBS patients [87, 88]. High-dose fructo-oligosaccharide (20 g/day) showed a trend to increase flatulence than placebo in the first 4–6 weeks of treatment [88]. This suggests that high doses of prebiotics should not be recommended for patients with IBS as this may cause more fermentation and bloating and could possibly worsen IBS symptoms. Natural foods such as wheat, bananas, oats, and soy beans contain prebiotics but at only trace levels [74, 75], while many other foods such as yogurt, cereal and bread are fortified with prebiotics, such as inulin, fructo-oligofructose, and galacto-oligosaccharides. Several prebiotic studies used extracted active ingredients from these food products rather than using natural food to avoid side effects from high nondigestible carbohydrate fermentation. Table 4 summarizes the clinical trials of prebiotics in IBS.
In contrast, a recent randomized controlled study showed that a low intake of FODMAPs improved overall gastrointestinal symptoms compared to a normal Australian diet which contains higher FODMAPs in IBS patients [3]. However, the low FODMAPs diet was shown to be associated with a significantly lower total fecal bacterial load by 47 % compared with a normal diet. It lowered an absolute abundance of the butyrate-producing bacteria, the prebiotic bacteria, Bifidobacterium spp and the mucus-associated bacterium, A. muciniphila which may play a role in gut barrier function. No alteration in fecal SCFA concentration or colonic transit time was shown in either group [89•]. Thus, the risk-benefit of the low FODMAPs in IBS must be elucidated because it caused a significant difference in gut microbiota with putative health benefits.
Due to the advancement of molecular biologic technology on gut microbiota, more bacteria species can be identified and a distinction between physiologic and pathologic changes in the intestinal microbiome can be made [90, 91]. Many other possible un-identified bacteria apart from Bifidobacterium and Lactobacillus could be affected when using new microbiological study techniques. In addition, it has not been clearly shown whether the colonic microbiota diversity or proportion of certain colonic bacteria may play a role in bowel function in both health and disease. Therefore, more future research is needed as previous reports may have limitations on microbiological studies on identifying the variety of gut microbiota species. This knowledge would help healthcare professionals recognize more substrates or food items that would have better prebiotic effects to improve health.
Conclusions
In summary, there has been increasing scientific evidence on GI health benefits of some food ingredients that have been previously acknowledged in traditional medicine. Chili pepper, a natural capsaicin, demonstrates the effect on TRPV1 receptor desensitization which may modify abdominal burning and pain sensation aggravated by mechanical and chemical stimulation in FGIDs including functional dyspepsia and IBS as well as GERD. Curcumin demonstrates anti-inflammatory effects and may benefit the brain–gut axis. The beneficial effects of prebiotics in FGIDs are still controversial. Low FODMAP diets, which potentially contain less prebiotic effects, significantly improved overall gastrointestinal symptoms in IBS but caused marked changes in fecal microbiota. In contrast, a higher FODMAPs intake was associated with specific stimulation of a particular gut microbiota with colonic health benefits but can produce more intestinal gas and gas symptoms. Current knowledge on the roles of gut microbiota on human health and disease is continuing with advanced techniques for gut microbiota studies. This may help identify dietary ingredients which have prebiotic effects with good fermentation profiles as well as major health benefits in gut microbiota composition modulation. Thus, more controlled trials on these common foods or ingredients in patients with functional GI disorders are encouraged.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Bohn L, Storsrud S, Tornblom H, Bengtsson U, Simren M. Self-reported food-related gastrointestinal symptoms in IBS are common and associated with more severe symptoms and reduced quality of life. Am J Gastroenterol. 2013;108(5):634–41.
Monsbakken KW, Vandvik PO, Farup PG. Perceived food intolerance in subjects with irritable bowel syndrome-- etiology, prevalence and consequences. Eur J Clin Nutr. 2006;60(5):667–72.
Halmos EP, Power VA, Shepherd SJ, Gibson PR, Muir JG. A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology. 2014;146(1):67–75.
Ferrucci LM, Daniel CR, Kapur K, Chadha P, Shetty H, Graubard BI, et al. Measurement of spices and seasonings in India: opportunities for cancer epidemiology and prevention. Asian Pac J Cancer Prev. 2010;11(6):1621–9.
Govindarajan VS, Sathyanarayana MN. Capsicum--production, technology, chemistry, and quality. Part V. Impact on physiology, pharmacology, nutrition, and metabolism; structure, pungency, pain, and desensitization sequences. Crit Rev Food Sci Nutr. 1991;29(6):435–74.
Domotor A, Peidl Z, Vincze A, Hunyady B, Szolcsanyi J, Kereskay L, et al. Immunohistochemical distribution of vanilloid receptor, calcitonin-gene related peptide and substance P in gastrointestinal mucosa of patients with different gastrointestinal disorders. Inflammopharmacology. 2005;13(1-3):161–77.
Holzer P. Transient receptor potential (TRP) channels as drug targets for diseases of the digestive system. Pharmacol Ther. 2011;131(1):142–70. A recent extensive review on TRP channels in GI tract and their therapeutic potential.
Guarino MP, Cheng L, Ma J, Harnett K, Biancani P, Altomare A, et al. Increased TRPV1 gene expression in esophageal mucosa of patients with non-erosive and erosive reflux disease. Neurogastroenterol Motil. 2010;22(7):746–51.
Chan CL, Facer P, Davis JB, Smith GD, Egerton J, Bountra C, et al. Sensory fibres expressing capsaicin receptor TRPV1 in patients with rectal hypersensitivity and faecal urgency. Lancet. 2003;361(9355):385–91.
Matsumoto K, Hosoya T, Tashima K, Namiki T, Murayama T, Horie S. Distribution of transient receptor potential vanilloid 1 channel-expressing nerve fibers in mouse rectal and colonic enteric nervous system: relationship to peptidergic and nitrergic neurons. Neuroscience. 2011;172:518–34.
Fuhrer M, Hammer J. Effect of repeated, long term capsaicin ingestion on intestinal chemo- and mechanosensation in healthy volunteers. Neurogastroenterol Motil. 2009;21(5):521–7.
Voight EA, Kort ME. Transient receptor potential vanilloid-1 antagonists: a survey of recent patent literature. Expert Opin Ther Pat. 2010;20(9):1107–22.
Chen CL, Yi CH, Liu TT. Comparable effects of capsaicin-containing red pepper sauce and hydrochloric acid on secondary peristalsis in humans. J Gastroenterol Hepatol. 2013;28(11):1712–6.
Herrera-Lopez JA, Mejia-Rivas MA, Vargas-Vorackova F, Valdovinos-Diaz MA. Capsaicin induction of esophageal symptoms in different phenotypes of gastroesophageal reflux disease. Rev Gastroenterol Mex. 2010;75(4):396–404.
Kindt S, Vos R, Blondeau K, Tack J. Influence of intra-oesophageal capsaicin instillation on heartburn induction and oesophageal sensitivity in man. Neurogastroenterol Motil. 2009;21(10):1032–9.
Liu TT, Yi CH, Lei WY, Hung XS, Yu HC, Chen CL. Influence of repeated infusion of capsaicin-contained red pepper sauce on esophageal secondary peristalsis in humans. Neurogastroenterol Motil. 2014;26(10):1487–93.
Touska F, Marsakova L, Teisinger J, Vlachova V. A "cute" desensitization of TRPV1. Curr Pharm Biotechnol. 2011;12(1):122–9.
Liu B, Zhang C, Qin F. Functional recovery from desensitization of vanilloid receptor TRPV1 requires resynthesis of phosphatidylinositol 4,5-bisphosphate. J Neurosci. 2005;25(19):4835–43.
Shima T, Shiina T, Naitou K, Nakamori H, Shimizu Y. Functional roles of capsaicin-sensitive intrinsic neural circuit in the regulation of esophageal peristalsis in rats: in vivo studies using a novel method. Am J Physiol Gastrointest Liver Physiol. 2014;306(9):G811–8.
Smid SD, Blackshaw LA. Neuromuscular function of the human lower oesophageal sphincter in reflux disease and Barrett's oesophagus. Gut. 2000;46(6):756–61.
Gonzalez R, Dunkel R, Koletzko B, Schusdziarra V, Allescher HD. Effect of capsaicin-containing red pepper sauce suspension on upper gastrointestinal motility in healthy volunteers. Dig Dis Sci. 1998;43(6):1165–71.
Chen CL, Liu TT, Yi CH, Orr WC. Effects of capsaicin-containing red pepper sauce suspension on esophageal secondary peristalsis in humans. Neurogastroenterol Motil. 2010;22(11):1177–82.
Lee KJ, Vos R, Tack J. Effects of capsaicin on the sensorimotor function of the proximal stomach in humans. Aliment Pharmacol Ther. 2004;19(4):415–25.
Hammer J, Vogelsang H. Characterization of sensations induced by capsaicin in the upper gastrointestinal tract. Neurogastroenterol Motil. 2007;19(4):279–87.
Tache Y, Pappas T, Lauffenburger M, Goto Y, Walsh JH, Debas H. Calcitonin gene-related peptide: potent peripheral inhibitor of gastric acid secretion in rats and dogs. Gastroenterology. 1984;87(2):344–9.
Raimura M, Tashima K, Matsumoto K, Tobe S, Chino A, Namiki T, et al. Neuronal nitric oxide synthase-derived nitric oxide is involved in gastric mucosal hyperemic response to capsaicin in rats. Pharmacology. 2013;92(1-2):60–70.
Patcharatrakul T, Gonlachanvit S. Gastroesophageal reflux symptoms in typical and atypical GERD: roles of gastroesophageal acid refluxes and esophageal motility. J Gastroenterol Hepatol. 2014;29(2):284–90.
He J, Ma X, Zhao Y, Wang R, Yan X, Yan H, et al. A population-based survey of the epidemiology of symptom-defined gastroesophageal reflux disease: the Systematic Investigation of Gastrointestinal Diseases in China. BMC Gastroenterol. 2010;10:94.
Geratikornsupuk N, Chaiwatanarat T, Gonlachanvit S. Effects of capsaicin containing chili on gastroesophageal acid refluxes (GER) and gastric emptying (GE) in patients with gastroesophageal reflux symptoms. J Gastroenterol Hepatol. 2008;23:A5.
Kriengkirakul C, Vasavid P, Gonlachanvit S. Chili induces epigastrium burning symptom in non-erosive reflux disease (NERD) with no effect on gastric accommodation (GA). J Gastroenterol Hepatol. 2010;25:A14.
Jutaghokiat S, Imraporn B, Gonlachanvit S. Chili improves gastroesophageal reflux symptoms in patients with Non Erosive Gastroesophageal Reflux Disease (NERD). Gastroenterology. 2009;136(5):A92.
Grossi L, Cappello G, Marzio L. Effect of an acute intraluminal administration of capsaicin on oesophageal motor pattern in GORD patients with ineffective oesophageal motility. Neurogastroenterol Motil. 2006;18(8):632–6.
Kiraly A, Suto G, Czimmer J, Horvath OP, Mozsik G. Failure of capsaicin-containing red pepper sauce suspension to induce esophageal motility response in patients with Barrett's esophagus. J Physiol Paris. 2001;95(1-6):197–200.
Fuhrer M, Vogelsang H, Hammer J. A placebo-controlled trial of an oral capsaicin load in patients with functional dyspepsia. Neurogastroenterol Motil. 2011;23(10):918–e397. This study demonstrated visceral hypersensitivity to capsaicin in functional dyspepsia.
Patcharatrakul T, Singhagowinta P, Kullavanijaya P, Gonlachanvit S. Gastrointestinal (GI) symptoms induced by spicy, sour, and fatty food ingestion in Functional Dyspepsia (FD): a difference between Epigastric Pain Syndrome (EPS) and Postprandial Distress Syndrome (PDS). Gastroenterology. 2013;144(5):S549–50.
Bortolotti M, Coccia G, Grossi G, Miglioli M. The treatment of functional dyspepsia with red pepper. Aliment Pharmacol Ther. 2002;16(6):1075–82.
Gonlachanvit S, Fongkam P, Wittayalertpanya S, Kullavanijaya P. Red chili induces rectal hypersensitivity in healthy humans: possible role of 5HT-3 receptors on capsaicin-sensitive visceral nociceptive pathways. Aliment Pharmacol Ther. 2007;26(4):617–25.
Hayashi K, Shibata C, Nagao M, Sato M, Kakyo M, Kinouchi M, et al. Intracolonic capsaicin stimulates colonic motility and defecation in conscious dogs. Surgery. 2010;147(6):789–97.
Gonlachanvit S, Mahayosnond A, Kullavanijaya P. Effects of chili on postprandial gastrointestinal symptoms in diarrhoea predominant irritable bowel syndrome: evidence for capsaicin-sensitive visceral nociception hypersensitivity. Neurogastroenterol Motil. 2009;21(1):23–32.
Agarwal MK, Bhatia SJ, Desai SA, Bhure U, Melgiri S. Effect of red chillies on small bowel and colonic transit and rectal sensitivity in men with irritable bowel syndrome. Indian J Gastroenterol. 2002;21(5):179–82.
Akbar A, Yiangou Y, Facer P, Walters JR, Anand P, Ghosh S. Increased capsaicin receptor TRPV1-expressing sensory fibres in irritable bowel syndrome and their correlation with abdominal pain. Gut. 2008;57(7):923–9.
Schmulson MJ, Valdovinos MA, Milke P, Zubiran S. Chili pepper and rectal hypera gesia in irritable bowel syndrome. Am J Gastroenterol. 2003;98(5):1214–5.
Aniwan S, Gonlachanvit S. Effects of chili treatment on gastrointestinal and rectal sensation in diarrhea-predominant irritable bowel syndrome: a randomized, double-blinded, crossover study. J Neurogastroenterol Motil. 2014;20(3):400–6. This study demonstrated desensitization effect of 6-week chili ingestion on upper and lower GI symptoms in IBS-D patients.
Bortolotti M, Porta S. Effect of red pepper on symptoms of irritable bowel syndrome: preliminary study. Dig Dis Sci. 2011;56(11):3288–95.
Gupta SC, Patchva S, Aggarwal BB. Therapeutic roles of curcumin: lessons learned from clinical trials. AAPS J. 2013;15(1):195–218.
Kumar S, Ahuja V, Sankar MJ, Kumar A, Moss AC. Curcumin for maintenance of remission in ulcerative colitis. Cochrane Database Syst Rev. 2012;10, CD008424.
Thong-Ngam D, Choochuai S, Patumraj S, Chayanupatkul M, Klaikeaw N. Curcumin prevents indomethacin-induced gastropathy in rats. World J Gastroenterol. 2012;18(13):1479–84.
Gupta SC, Tyagi AK, Deshmukh-Taskar P, Hinojosa M, Prasad S, Aggarwal BB. Downregulation of tumor necrosis factor and other proinflammatory biomarkers by polyphenols. Arch Biochem Biophys. 2014;559:91–9.
Aggarwal BB, Gupta SC, Sung B. Curcumin: an orally bioavailable blocker of TNF and other pro-inflammatory biomarkers. Br J Pharmacol. 2013;169(8):1672–92.
Liu L, Liu YL, Liu GX, Chen X, Yang K, Yang YX, et al. Curcumin ameliorates dextran sulfate sodium-induced experimental colitis by blocking STAT3 signaling pathway. Int Immunopharmacol. 2013;17(2):314–20.
Zeng Z, Zhan L, Liao H, Chen L, Lv X. Curcumin improves TNBS-induced colitis in rats by inhibiting IL-27 expression via the TLR4/NF-kappaB signaling pathway. Planta Med. 2013;79(2):102–9.
Ali T, Shakir F, Morton J. Curcumin and inflammatory bowel disease: biological mechanisms and clinical implication. Digestion. 2012;85(4):249–55.
Wang N, Wang G, Hao J, Ma J, Wang Y, Jiang X, et al. Curcumin ameliorates hydrogen peroxide-induced epithelial barrier disruption by upregulating heme oxygenase-1 expression in human intestinal epithelial cells. Dig Dis Sci. 2012;57(7):1792–801.
De R, Kundu P, Swarnakar S, Ramamurthy T, Chowdhury A, Nair GB, et al. Antimicrobial activity of curcumin against Helicobacter pylori isolates from India and during infections in mice. Antimicrob Agents Chemother. 2009;53(4):1592–7.
Foryst-Ludwig A, Neumann M, Schneider-Brachert W, Naumann M. Curcumin blocks NF-kappaB and the motogenic response in Helicobacter pylori-infected epithelial cells. Biochem Biophys Res Commun. 2004;316(4):1065–72.
Rai D, Singh JK, Roy N, Panda D. Curcumin inhibits FtsZ assembly: an attractive mechanism for its antibacterial activity. Biochem J. 2008;410(1):147–55.
Han C, Wang L, Yu K, Chen L, Hu L, Chen K, et al. Biochemical characterization and inhibitor discovery of shikimate dehydrogenase from Helicobacter pylori. FEBS J. 2006;273(20):4682–92.
Shimouchi A, Nose K, Takaoka M, Hayashi H, Kondo T. Effect of dietary turmeric on breath hydrogen. Dig Dis Sci. 2009;54(8):1725–9.
Yu Y, Wu S, Li J, Wang R, Xie X, Yu X, et al. The effect of curcumin on the brain-gut axis in rat model of irritable bowel syndrome: involvement of 5-HT-dependent signaling. Metab Brain Dis. 2015;31(1):47–55.
Hurley LL, Akinfiresoye L, Nwulia E, Kamiya A, Kulkarni AA, Tizabi Y. Antidepressant-like effects of curcumin in WKY rat model of depression is associated with an increase in hippocampal BDNF. Behav Brain Res. 2013;239:27–30.
Rinwa P, Kumar A, Garg S. Suppression of neuroinflammatory and apoptotic signaling cascade by curcumin alone and in combination with piperine in rat model of olfactory bulbectomy induced depression. PLoS One. 2013;8(4), e61052.
Tajik H, Tamaddonfard E, Hamzeh-Gooshchi N. The effect of curcumin (active substance of turmeric) on the acetic acid-induced visceral nociception in rats. Pak J Biol Sci. 2008;11(2):312–4.
Zhi L, Dong L, Kong D, Sun B, Sun Q, Grundy D, et al. Curcumin acts via transient receptor potential vanilloid-1 receptors to inhibit gut nociception and reverses visceral hyperalgesia. Neurogastroenterol Motil. 2013;25(6):e429–40. An animal study which demonstrated a mechanism of intestinal anti-nociception of curcumin via TRPV-1 receptors.
Aldini R, Budriesi R, Roda G, Micucci M, Ioan P, D'Errico-Grigioni A, et al. Curcuma longa extract exerts a myorelaxant effect on the ileum and colon in a mouse experimental colitis model, independent of the anti-inflammatory effect. PLoS One. 2012;7(9), e44650.
Gilani AH, Shah AJ, Ghayur MN, Majeed K. Pharmacological basis for the use of turmeric in gastrointestinal and respiratory disorders. Life Sci. 2005;76(26):3089–105.
Xu L, Li Z, Guo F. Curcumin improves expression of ghrelin through attenuating oxidative stress in gastric tissues of streptozotocin-induced diabetic gastroparesis rats. Eur J Pharmacol. 2013;718(1-3):219–25.
Di Mario F, Cavallaro LG, Nouvenne A, Stefani N, Cavestro GM, Iori V, et al. A curcumin-based 1-week triple therapy for eradication of Helicobacter pylori infection: something to learn from failure? Helicobacter. 2007;12(3):238–43.
Lopresti AL, Maes M, Maker GL, Hood SD, Drummond PD. Curcumin for the treatment of major depression: a randomised, double-blind, placebo controlled study. J Affect Disord. 2014;167:368–75.
Sanmukhani J, Satodia V, Trivedi J, Patel T, Tiwari D, Panchal B, et al. Efficacy and safety of curcumin in major depressive disorder: a randomized controlled trial. Phytother Res. 2014;28(4):579–85.
Anand P, Kunnumakkara AB, Newman RA, Aggarwal BB. Bioavailability of curcumin: problems and promises. Mol Pharm. 2007;4(6):807–18.
Martin RC, Aiyer HS, Malik D, Li Y. Effect on pro-inflammatory and antioxidant genes and bioavailable distribution of whole turmeric vs curcumin: Similar root but different effects. Food Chem Toxicol. 2012;50(2):227–31.
Prasad S, Tyagi AK, Aggarwal BB. Recent developments in delivery, bioavailability, absorption and metabolism of curcumin: the golden pigment from golden spice. Cancer Res Treat. 2014;46(1):2–18.
Sharma RA, Euden SA, Platton SL, Cooke DN, Shafayat A, Hewitt HR, et al. Phase I clinical trial of oral curcumin: biomarkers of systemic activity and compliance. Clin Cancer Res. 2004;10(20):6847–54.
Roberfroid M, Gibson GR, Hoyles L, McCartney AL, Rastall R, Rowland I, et al. Prebiotic effects: metabolic and health benefits. Br J Nutr. 2010;104 Suppl 2:S1–63.
Macfarlane S, Macfarlane GT, Cummings JH. Review article: prebiotics in the gastrointestinal tract. Aliment Pharmacol Ther. 2006;24(5):701–14.
Macfarlane GT, Macfarlane S. Fermentation in the human large intestine: its physiologic consequences and the potential contribution of prebiotics. J Clin Gastroenterol. 2011;45(Suppl):S120–7.
Leonel AJ, Alvarez-Leite JI. Butyrate: implications for intestinal function. Curr Opin Clin Nutr Metab Care. 2012;15(5):474–9.
Arpaia N, Campbell C, Fan X, Dikiy S, van der Veeken J, DeRoos P, et al. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature. 2013;504(7480):451–5.
Furusawa Y, Obata Y, Fukuda S, Endo TA, Nakato G, Takahashi D, et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature. 2013;504(7480):446–50.
Nyangale EP, Mottram DS, Gibson GR. Gut microbial activity, implications for health and disease: the potential role of metabolite analysis. J Proteome Res. 2012;11(12):5573–85.
De Peter V, Falony G, Windey K, Hamer HM, De Vuyst L, Verbeke K. The prebiotic, oligofructose-enriched inulin modulates the faecal metabolite profile: an in vitro analysis. Mol Nutr Food Res. 2010;54(12):1791–801.
Walker WA, Iyengar RS. Breast milk, microbiota, and intestinal immune homeostasis. Pediatr Res. 2015;77(1-2):220–8.
Cederlund A, Kai-Larsen Y, Printz G, Yoshio H, Alvelius G, Lagercrantz H, et al. Lactose in human breast milk an inducer of innate immunity with implications for a role in intestinal homeostasis. PLoS One. 2013;8(1), e53876.
Ohman L, Simren M. Intestinal microbiota and its role in irritable bowel syndrome (IBS). Curr Gastroenterol Rep. 2013;15(5):323.
Paineau D, Payen F, Panserieu S, Coulombier G, Sobaszek A, Lartigau I, et al. The effects of regular consumption of short-chain fructo-oligosaccharides on digestive comfort of subjects with minor functional bowel disorders. Br J Nutr. 2008;99(2):311–8.
Silk DB, Davis A, Vulevic J, Tzortzis G, Gibson GR. Clinical trial: the effects of a trans-galactooligosaccharide prebiotic on faecal microbiota and symptoms in irritable bowel syndrome. Aliment Pharmacol Ther. 2009;29(5):508–18.
Hunter JO, Tuffnell Q, Lee AJ. Controlled trial of oligofructose in the management of irritable bowel syndrome. J Nutr. 1999;129(7 Suppl):1451S–3.
Olesen M, Gudmand-Hoyer E. Efficacy, safety, and tolerability of fructooligosaccharides in the treatment of irritable bowel syndrome. Am J Clin Nutr. 2000;72(6):1570–5.
Halmos EP, Christophersen CT, Bird AR, Shepherd SJ, Gibson PR, Muir JG. Diets that differ in their FODMAP content alter the colonic luminal microenvironment. Gut. 2015;64(1):93–100. A randomized cross-over study demonstrated that a 21-day low FODMAP intake had effects on gut microbiota composition.
Ding T, Schloss PD. Dynamics and associations of microbial community types across the human body. Nature. 2014;509(7500):357–60.
Backhed F, Fraser CM, Ringel Y, Sanders ME, Sartor RB, Sherman PM, et al. Defining a healthy human gut microbiome: current concepts, future directions, and clinical applications. Cell Host Microbe. 2012;12(5):611–22.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
TP and SG declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
With regard to the authors’ research cited in this paper, all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. In addition, all applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Additional information
This article is part of the Topical Collection on Neurogastroenterology and Motility Disorders of the Gastrointestinal Tract
Rights and permissions
About this article
Cite this article
Patcharatrakul, T., Gonlachanvit, S. Chili Peppers, Curcumins, and Prebiotics in Gastrointestinal Health and Disease. Curr Gastroenterol Rep 18, 19 (2016). https://doi.org/10.1007/s11894-016-0494-0
Published:
DOI: https://doi.org/10.1007/s11894-016-0494-0