Abstract
Purpose of Review
Formalized chronic care management has the potential to improve the quality and cost-effectiveness of complex diabetes management in adults, but has historically not been sustainably supported by health care systems. This review discusses the application of the chronic care model in the care of complex diabetes and its translation in the current reimbursement structure designed by Centers for Medicare and Medicaid Services (CMS).
Recent Findings
Following the introduction of Wagner’s Chronic Care Model (CCM) in the late 1990s, evidence gathered over the past 2 decades has supported the shift in focus of health care systems from acute to chronic disease management and proactive care. Acknowledging evidence and potential for improved cost-effectiveness, in 2015, Medicare began reimbursing for chronic care management services (CCMS) for patients with multiple chronic conditions. The CCMS billing codes allow a program to be reimbursed for up to 90 min per month spent by clinical staff performing interim care within a comprehensive care plan. Recent data from local and global programs support the application of formalized CCM in diabetes management.
Summary
Although reimbursement models for CCM have been designed for use in primary care, the challenges of the reimbursement model has opened the door for specialty areas focused on multimorbidity care such as diabetes care to explore this approach. With the broader availability of remote glucose monitoring and telemedicine, a strategy that combines goal-oriented care and telehealth solutions appears to be most effective in diabetes CCM care. Despite widespread acceptance of the chronic care model of care, there remain significant barriers to its incorporation into standard practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Recent statistics indicate that 14% of adults in the USA have diabetes, a prevalence that has risen every year since the mid-1990s. In several sub-cohorts the prevalence is higher, with > 15% of non-Hispanic Black and Hispanic adults and an estimated 28% of individuals over 65 years of age affected by diabetes [1]. This has translated to a 26% increase in the economic costs of the disease since 2012, recently estimated to be $327 billion, with care for people with diagnosed diabetes accounting for one in four health care dollars in the USA. Of importance, about 25% of this cost is due to lost productivity due to complications leading to disability and premature death [2]. Despite the sobering rise in diabetes-related costs, disease control has not clearly improved, with only 19–34% of individuals estimated to be successfully treated based on a recent analysis of US claims and survey data [3]. Health systems around the world are recognizing that current models are inadequate to support the prevention and management of costly complications. It is clear that new approaches to diabetes care focused on preventing micro and macrovascular disease throughout the lifetime of individuals with diabetes are necessary. Moreover, as diabetes advances and therapies become more complex, quality care becomes less feasible in usual care models [4•].
This overview describes the incorporation of established principles of chronic care delivery into diabetes specialty care in order to deliver high quality, sustainable, and scalable services for individuals with complex diabetes. As discussed below, the chronic care model (CCM) is a conceptual framework designed to deliver patient-centered chronic disease management services. [5] In 2015, the Center for Medicaid and Medicare Services (CMS) began reimbursing programs that followed a highly defined rubric of services and structure designed to follow the CCM. [6] For the set of services and corresponding billing codes, CMS adopted the commonly used term Chronic Care Management services (CCMS), which describes care coordination work done outside of the regular office visit for patients with several documented chronic illnesses. For this review, the patient group with complex diabetes includes those who require high-touch interdisciplinary care and ongoing support for self-management due to one or more factors (e.g., sub-optimally controlled and/or frequent hypoglycemia on multiple daily doses of insulin or diabetes in the setting of major or multiple comorbid illnesses).
The main goal of this paper is to address the readiness of diabetes specialty care programs for CCMS or similar structures for management of complex diabetes, and to provide guidance based on the early experience with our program.
The Chronic Care Model and Diabetes
The care model described by Wagner et al., emerged in the 1990s as a way to restructure and organize primary care to better tend to patients with chronic diseases. It is a care design focusing on six modifiable components of health care delivery: organizational/system support, clinical information systems, delivery system design, decision support, self-management support, and community resources. While the first four components in the model address practice strategies, the final two are specifically patient centered. In recent years, two other elements have been suggested, namely enhanced health care professional case management support and facilitated family support. Importantly, care redesign strategies that implement these components have been found to reduce healthcare costs [7•]. Moreover, these components fit naturally into the care of patients with complex diabetes (Table 1).
In diabetes care, there is a large body of evidence supporting the use of the interdisciplinary care team for diabetes care delivery when applied to self-management education, glucose-lowering therapies, and comprehensive lifelong complication prevention. An analysis from data compiled from large health surveys performed in the USA suggests that the increased incorporation of interdisciplinary care has reduced complication rates [8]. Team-oriented interventions have been shown to have the greatest impact on glycemic control [9]. As a result, international societies and health care delivery organizations promote team-based interdisciplinary diabetes care that is tailored to the patient as the best approach to achieve long-term control of the disease [10,11,12,13,14].
Beyond evidence for the team-based model, there is evidence, however limited, suggesting that the CCM model when applied to diabetes produces cost-effective outcomes. An early study illustrated the model across several chronic illnesses, showing savings from reduced hospital admissions, emergency room visits, and physician consultations [15]. Subsequent studies applying CCM showed similar results, and a meta-analysis published in 2005 indicated that implementing at least one element of the chronic care model improved clinical outcomes and processes of care in a host of chronic diseases including asthma, CHF, depression, and diabetes [16]. In a more recent systematic review, 77 high-quality studies were evaluated, which included 24 studies focused on diabetes including six randomized trials. The outcomes evaluated included improvement in healthcare practices or outcomes. The authors found that all but two of the studies demonstrated improved healthcare practice or outcomes with the most common CCM elements used being self-management support and delivery system design [7•]. In another systematic review, 16 studies were included that reported outcomes of CCM for diabetes in primary care settings. The impact on glycemic control (HbA1c) was highly variable, ranging from no significant change to − 1.5% in one study. Of note, the authors found that overall CCM appeared effective in diabetes care delivered in primary care and that studies that incorporated more than one CCM element demonstrated the best outcomes [17].
Challenges of Current Care Models
Unfortunately, in most health systems, and in particular those in the USA, the standard health care delivery system does not provide adequate financial incentives nor infrastructural support for patient-centered team-based care. Importantly, the necessary time spent delivering virtual care (e.g., by phone or electronic communication) between usual visits is not reimbursed.
Complex diabetes management is similar to other high-acuity chronic illnesses: it is oriented around achieving clinical targets; requires interim follow-up for safety and medication titration; and due to common challenges of cost and access, necessitates substantial administrative support for the patient. In state-of-the-art clinical diabetes programs, these domains are tackled 24 h a day, 7 days per week, and in a patient-tailored manner. Recent publications highlight two key barriers that limit the ability of providers and health systems to deliver this level of patient-centered care to patients with complex diabetes. The first is the lack of recognition, through reimbursement, of time required to deliver quality interim care. In a careful analysis of time spent outside of in-person clinical visits on administrative work required to deliver high-quality care, one center reported 28 h per week spent by the non-provider care team on non-billable interim care. The authors estimated this non-billable care by non-providers would cost nearly $100,000 per year to support the patient panel of one provider [4•]. This discrepancy between financial support and actual cost to support patients leads to insufficient administrative staffing of most diabetes clinical programs, placing the challenge of maintaining high care standards entirely on clinicians.
The second major barrier is burnout, both for the patient and the provider. Burnout is a psychological term that refers to long-term exhaustion and diminished interest in self-care for a patient, and work, for the provider. Burnout is multifactorial in etiology and how it manifests. Patients with unaddressed burnout and distress have worse outcomes [18]. Measurement and action upon burnout in the clinical setting is required to deliver comprehensive care. Provider burnout follows from these barriers due to the increase in administrative burden felt at the same time as more patients experience distress and poor outcomes; as a result, caring for diabetes feels like a Sisyphean fate, leaving many clinicians and patients unsatisfied. Importantly, physician burnout leads to poor clinical outcomes, placing additional weight on the interdisciplinary care team [19].
Is Care Redesign in Diabetes Cost Effective?
Redesigning health systems on both large and small scales is difficult and often takes years to realize outcomes (ref: care redesign challenge), during which time other factors can derail efforts. As a result, it is often unclear if taking the risk of change is likely to yield significant benefit. Recent literature sheds some light on this question in diabetes. For example, risk stratification in order to allocate services appears to be effective in diabetes care on a large scale [20]. In a recent report, the RAMP-DM program in China was demonstrated to improve outcomes in a group of 26,718 enrollees over 5 years. The RAMP-DM program functioned essentially as a CCM for diabetes, existing in addition to usual primary care, whereby individuals with diabetes were enrolled after an initial intake assessment and then directed toward specific interventions that were assigned based on both cardiovascular risk and HbA1c. The participants were then assigned a case manager to connect them to appropriate interventions and education provided by a team of multidisciplinary health care professionals, including nurses and allied health professionals. Depending on risk level, some RAMP-DM participants would have an annual full-risk factor screening and intake assessment, and others would have the full assessment every 2–3 years with an annual blood test and follow-up by their primary care doctors. Remarkably, there were significantly lower cumulative incidences of individuals with any complications (15.34 vs. 28.65%, P < 0.001) and all-cause mortality (7.96 vs. 21.35%, P < 0.001) in the RAMP-DM group compared with the usual-care group. Investigators also found that RAMP-DM was cost-effective when added to usual primary care [21]. Despite a mean program cost of just 157 US dollars (range 66–209) per participant over 5 years, the costs of health service utilization among participants in RAMP-DM group was 7451 USD less than that of the usual-care group, resulting in a net savings of 7294 USD per individual.
In general, quality improvement programs in diabetes that involve restructuring of services, mostly to tailor to patient needs or to risk stratify, are effective in improving glucose control. Nuckols et al. performed a systematic review of the economic impact of quality improvement programs to improve glycemic control in patients with diabetes. Among a heterogeneous group of 46 studies reviewed, the 19 RCTs demonstrated an overall mean reduction of glycated hemoglobin (HbA1c) of 0.26% versus the usual care. In the 8 RCTs lasting ≤ 3 years, cost-effectiveness analyses suggested that the improved glycemic control came with a relatively small net incremental cost of $116 (95% CI $612 to $843) per patient annually [22••]. In the nine studies that used modeling to simulate the longer term outcomes (≥ 20 years), the median incremental cost-effectiveness ratios (ICER) were less than $50,000 per quality-adjusted life year gained. In general, interventions that cost < $50,000 to $100,000 per quality-adjusted life year gained are considered to represent a good value [23]. In summary, these results indicate that quality improvement interventions in diabetes that employ patient tracking, treatment team redesign, individualized management risk stratification, and education are likely to be cost-effective over time.
Translation of CCMS to Diabetes Specialty Care: Our Experience
To establish CCMS and meet billing requirements, programs must be able to demonstrate the elements required under CMS rules for CCMS (Table 1). Like all clinical programs billing CMS, CCMS programs are subject to audits and will be potentially fined for not meeting pre-specified criteria that allow the use of specialized billing codes (Table 2). For this reason, hospital systems are careful to allow the establishment of CCMS programs. In our experience, this required several meetings with hospital financial leadership to prove our program’s alignment with the requirements. It also required conversations with primary care leadership as the CCMS reimbursement model was designed for use in these settings and monthly billing codes can be used only once per patient by the same institution. Due to the many challenges of not only meeting the CMS requirements but also the unclear feasibility of scaling CCMS programs to large populations, primary care sites within our system have not successfully implemented their use. This allowed the diabetes program to explore CCMS for complex diabetes.
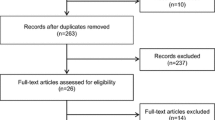
In 2015, we began designing and pilot-testing a diabetes management program called the Setting Targets Achieving Results in Diabetes (STAR-DM) program with the goal of creating a CCMS program. As previously described [24], the STAR-DM program is offered to patients who have been referred to the diabetes program within the last year and have failed to meet clinical targets despite standard specialty care. Patients are identified in two ways: (1) automatically through an internal quality metric that identifies newly referred patients with an HbA1c > 8% who do not achieve an HbA1c lowering of at least 0.5% within 1 year and (2) by individual provider referral. The program provides intensive management in collaboration with the primary diabetologist and care team for 6 months after which time they are transitioned back to the care team. An interdisciplinary assessment and management plan is designed with the patient to achieve individualized primary and secondary goals. The primary goal is most often (95% of patients) achieving an individualized HbA1c target, but patients with their providers may also choose clearance for elective surgery or reducing hypoglycemia. Following an initial intake visit, interim contact incudes weekly/bi-weekly contact via telephone, secure messaging system through the electronic health record, or videoconference. While data from the pilot is still under analysis, recent data show that 73% of patients (N = 104) enrolled in the program achieved their primary goal and of these the mean HbA1c reduction is 1.8%; nearly all achieve some improvement in patient reported outcomes (e.g., diabetes distress).
It is too early to assess cost-effectiveness of our CCMS program, although initial estimates and given the clinical impact thus far suggest it will be. Based on a 60-patient pilot, considering all incremental costs incurred and revenue generated by the program’s clinical staff (including professional continuous glucose monitoring (CGM) and usual face-to-face visits), and modeling a generous 80% reimbursement, we calculated that the program had the potential to yield a surplus by the end of 2 years that would allow for expansion. The “real world” cost assessment, however, considered other factors, including that reimbursement outside of Medicare is still low and the population included just 43% Medicare beneficiaries. At this time, our CCMS reimbursement is being applied mainly to the administrative support of the program and patient care coordination rather than the clinical effort of other staff (Fig. 1). When CCMS reimbursement extends beyond Medicare in the future, we would be able to fund part of the provider staff effort. After hospital approval, we launched the program and began using CCMS billing codes in April 2018.
The diabetes CCM structure. Key members of the chronic care model function to support the patient with diabetes to achieve self-identified clinical goals. Communication is multidirectional (arrows) but tailored to patients’ individual needs. Models can be designed to deliver high-intensity management over short periods (e.g., 6 months), or can be designed to be part of the longitudinal comprehensive care plan. In this model, the patient is supported by an interdisciplinary team that maintains communication through a diabetes nurse practitioner. The NP directs the day-to-day management of the patient as well as consultations and is overseen by the medical director. The weekly team meetings are run by the navigator who goes through the patient roster with key members of the team and tracks interventions. The purpose of the team meeting is to establish the care plan for the following week after receiving input from all disciplines. The navigator also enrolls patients and assists patients with administrative or scheduling challenges. Psych psychiatry/other behavioral health, SW social work, Ophthal ophthalmology, VNA visiting nurse association
CCM Requirements
CMS imposes various stipulations on CCMS. Among the more burdensome are the requirement for patient consent (in the event insurance coverage lapses), specific documentation (Table 2), and the limitation of only one provider using the code per patient per month. These requirements can be challenging in overburdened clinical practices and must be addressed using documentation templates and the clinic administrative support team. Requiring patient consent demands that a sufficient form or electronic avenue be created that is then subject to internal processes of approval. This type of consent (e.g., HIPAA consent, agreement to pay charges that are not reimbursed) is typical in most clinical areas but CCMS requires its own form. The limitation of one provider per month per patient has led hospital systems to create methods to clearly identify patients who are enrolled in CCMS programs so that other co-existing programs (e.g., in primary care) will identify a potential billing conflict in patients enrolled in multiple programs. Unfortunately, this limitation, if not changed in future iterations, will likely inhibit the development of CCMS programs. Indeed, without interdisciplinary cooperation, CCMS billing could easily become a high-burden low-yield investment. Finally, little is known about coverage outside of Medicare for these services which may likely cause providers to shy away.
Implementation of CCMS in diabetes also requires coordination not only with respect to clinical management of patients but also on the part of the diabetes care team. The STAR-DM program has been restructured to meet CCMS requirements and now includes several key players including a medical director, nurse practitioner team manager, nurse educator, patient navigator, and practice assistant (Fig. 1). There is collaboration with other hospital-level chronic care programs which ultimately assist in management. Weekly team meetings and case discussions occur in addition to management of a data set which is used in decision-making around care design and forward movement of our program.
Biometric Data Capture for CCM
Recording glucose data is the cornerstone for diabetes management and is the most important way to optimize interim care to meet clinical targets. With evolving technologies, there are multiple options in capturing this data which come with both advantages and pitfalls. From the latest CGM device to the newest integrated insulin pump, diabetes programs and patients alike are faced with the ongoing challenge of maintaining expertise in new technologies and determining how best to integrate them into the workflow of the busy clinic environment.
Capturing quality glucose data using remote monitoring takes time and effort on the part of patients and for some patients this might require technical support; this can add to treatment burden. Glucose data sharing solutions, for example, often depend on the patient's ability to maneuver a smartphone and conduct basic troubleshooting.
With traditional glucose meters the challenge continues to be accessing the patients’ data in the clinic. Web-based downloading software is constantly changing and it takes time for clinic staff to maintain knowledge of the platforms and integrate new ones into clinic workflow.
CGM has changed diabetes practice and is becoming the standard of care for patients who require insulin therapy. Detailed education is required for both patients and providers to see the full benefits of this technology and to avoid the many pitfalls. Even outside of routine office visits, most platforms require patients to create an online account to initiate data sharing. Calibration, whether in the form of finger sticks or a “sensor warm-up” period has been an ongoing barrier in CGM technology and in some cases can influence accuracy. Very recent developments have begun to address this, such as with the Dexcom G6® and the Abbott Freestyle Libre®. The ability to seamlessly integrate these technologies into clinic work flows and interim diabetes care is an essential component for the success of CCM in complex diabetes.
Challenges to Be Addressed for Diabetes CCM to Become Standard Practice
There remain several barriers to the widespread incorporation of CCM and CCMS into diabetes specialty care. Necessary changes are within reach and can be addressed by the following additions:
-
1)
Expanded coverage beyond Medicare. While some commercial insurers are reimbursing for CCMS billing codes, Medicare is the only payer that acknowledges coverage as part of their services at this time. It is unclear to what extent this will continue or expand. Given the impact of both type 1 and type 2 diabetes across the lifespan including youth, CCMS must be covered by Medicaid and private payers in order to have a population level impact on diabetes outcomes.
-
2)
Refined criteria for patients who are likely to benefit from CCM. We have learned in our practice that intensive services such as those delivered through CCMS do not have equal effectiveness among individuals. While one patient’s failure to succeed within the CCM is often due in large part to specific details of program design (e.g., schedule flexibility, cultural and language concordance, availability of behavioral health services), in our experience it is equally as likely for unmeasured patient factors to create barriers. Such factors include personal priorities [25], personality [26], and psychosocial factors such as diabetes distress [27]. As we take on the challenge of addressing global metabolic disease by designing new methods to improve diabetes outcomes, understanding the relative impact of such factors is an important area of research.
-
3)
Expanded coverage, and reduced cost, of glucose monitoring devices and systems. This area also includes streamlining the technology to allow clinics to more easily incorporate new devices into their workflow for patient education and device downloading.
-
4)
Increased training of diabetes-focused clinicians in general medicine and across the spectrum of disciplines [28]. Expansion of the workforce around general diabetes to provide lower cost, earlier interventions to uncomplicated diabetes is likely required to allow institutions to refine their programs to address complicated diabetes through CCM or similar methodologies.
-
5)
Engage the community in uncomplicated diabetes and diabetes prevention. The scalability of advanced diabetes care remains an unmet need in most countries. Most forms of diabetes become more complicated over time, exhausting available resources in local communities, states, countries, and beyond. Bold methodologies are required to shift disease complexity across populations away from advanced end-organ disease and toward prevention and control. In one telling example from San Diego, California, the rate of acute MI was reduced by 22% in following a population-level multi-tiered campaign for lifestyle modification [29]. An enhanced role of community and government in disease and complication prevention is likely required so that CCM can be applied to more patients who are likely to benefit.
Conclusion
There is an urgent need to shift the care paradigm in complex diabetes away from quantity of in-person care toward quality of patient-tailored care. The CCMS model designed by CMS takes a positive, though small, step toward addressing the issues of unrecognized time spent on interim care and the resulting clinician burnout. New diabetes-tailored CCM approaches would also increase focus on addressing diabetes distress and reducing patient burden [30]. While we are still learning about reimbursement for CCMS, this is the first mechanism care teams can adopt to produce revenue from the hours spent managing chronic diseases in between office visits. High-value comprehensive care planning to vulnerable patient populations represents the direction of future healthcare.
As accountable care organizations and risk-based models become a major part of the reimbursement landscape, integrated models such as CCM that provide high value, efficient, and comprehensive care to a patient population with multiple needs represent the future direction of healthcare. Although CCM was designed for use in primary care, it has a role in comprehensive care of the patient with complex diabetes. Moreover, an integrated care model is cost-efficient because it reduces costly provider visits by tailoring care to objectively measured care needs and maximizing use of telemedicine and telehealth.
Despite the clear need, quality-based reimbursement is in early stages for diabetes management. It is important to evaluate sustainability and scalability over time. The future of diabetes care would be well served by an investment in CCM from organized healthcare payers and delivery systems for select diabetes populations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mendola N, Chen T-C, Gu Q, Prevalence of total, diagnosed, and undiagnosed diabetes among adults: United States, 2013–2016. In: U.D.o.H.a.H. Services. Data Brief; 2018.
American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917–28.
Dwyer-Lindgren L, Mackenbach JP, van Lenthe FJ, Flaxman AD, Mokdad AH. Diagnosed and undiagnosed diabetes prevalence by county in the U.S., 1999-2012. Diabetes Care. 2016;39(9):1556–62.
• Huynh P, Toulouse A, Hirsch IB. One-year time analysis in an academic diabetes clinic: quantifying our burden. Endocr Pract. 2018;24(5):489–91. In this analysis the authors sought to document the nonreimbursable time clinicians spend in the care of patients with diabetes being managed in an academic medical center. The findings illuminated the problem of administrative burden on the clinical diabetes care team and made a case for how it is likely impairing quality of care as well as quality of life for the team members.
Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–9.
The Centers for Medicare & Medicaid Services (CMS). Chronic Care Management Services (2016, December). 2018. Available at https://www.cms.gov/About-CMS/Agency-Information/OMH/Downloads/CCM-Toolkit-Updated-Combined-508.pdf. Accessed 8 Sept 2018.
• Davy C, et al. Effectiveness of chronic care models: opportunities for improving healthcare practice and health outcomes: a systematic review. BMC Health Serv Res. 2015;15:194. This is a systematic review of studies reporting outcomes of chronic care model in the care of diseases in Primary Care including diabetes. Approximately a third of the programs were diabetes-focused. All but two of the 77 studies reported improved healthcare practice or patient health outcomes, but as expected the heterogeneity across the studies did not allow a determination of the ideal program design.
Gregg EW, Li Y, Wang J, Rios Burrows N, Ali MK, Rolka D, et al. Changes in diabetes-related complications in the United States, 1990-2010. N Engl J Med. 2014;370(16):1514–23.
Shojania KG, Ranji SR, McDonald KM, Grimshaw JM, Sundaram V, Rushakoff RJ, et al. Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. JAMA. 2006;296(4):427–40.
Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, et al. 2017 National Standards for diabetes self-management education and support. Diabetes Care. 2017;40(10):1409–19.
American Diabetes Assocation. 10. Microvascular complications and foot care: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S105–18.
American Diabetes Assocation. 9. Cardiovascular disease and risk management: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S86–S104.
American Diabetes Assocation. 8. Pharmacologic approaches to glycemic treatment: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S73–85.
American Diabetes Assocation. 4. Lifestyle management: standards of medical Care in Diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S38–50.
Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, part 2. JAMA. 2002;288(15):1909–14.
Tsai AC, Morton SC, Mangione CM, Keeler EB. A meta-analysis of interventions to improve care for chronic illnesses. Am J Manag Care. 2005;11(8):478–88.
Stellefson M, Dipnarine K, Stopka C. The chronic care model and diabetes management in US primary care settings: a systematic review. Prev Chronic Dis. 2013;10:E26.
Aikens JE. Prospective associations between emotional distress and poor outcomes in type 2 diabetes. Diabetes Care. 2012;35(12):2472–8.
Panagioti M, Geraghty K, Johnson J, Zhou A, Panagopoulou E, Chew-Graham C, et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern Med. 2018;178:1317–30.
Wan EYF, Fung CSC, Jiao FF, Yu EYT, Chin WY, Fong DYT, et al. Five-year effectiveness of the multidisciplinary risk assessment and management programme-diabetes mellitus (RAMP-DM) on diabetes-related complications and health service uses-a population-based and propensity-matched cohort study. Diabetes Care. 2018;41(1):49–59.
Jiao FF, Fung CSC, Wan EYF, Chan AKC, McGhee SM, Kwok RLP, et al. Five-year cost-effectiveness of the multidisciplinary risk assessment and management programme-diabetes mellitus (RAMP-DM). Diabetes Care. 2018;41(2):250–7.
•• Nuckols TK, et al. Economic evaluation of quality improvement interventions designed to improve glycemic control in diabetes: a systematic review and weighted regression analysis. Diabetes Care. 2018;41(5):985–93. In this metanalysis and cost-analysis of studies of diabetes care redesign, among a heterogeneous group of 46 studies reviewed, the 19 RCTs demonstrated an overall mean reduction of glycated hemoglobin (HbA1c) of 0.26% versus usual care. In the 8 RCTs lasting ≤ 3 years, cost-effectiveness analyses suggested that the improved glycemic control came with a relatively small incremental cost.
Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness--the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371(9):796–7.
Rein R, Del Valle KL, McDonnell ME, Hudson M, Potler H. Self-reported health status in patients with poor glycemic control in endocrinology, 735-P. Presented at the American Diabetes Association scientific sessions. 2017.
Serrano V, Spencer-Bonilla G, Boehmer KR, Montori VM. Minimally disruptive medicine for patients with diabetes. Curr Diab Rep. 2017;17(11):104.
Nefs G, Speight J, Pouwer F, Pop V, Bot M, Denollet J. Type D personality, suboptimal health behaviors and emotional distress in adults with diabetes: results from diabetes MILES-The Netherlands. Diabetes Res Clin Pract. 2015;108(1):94–105.
Fisher L, Hessler D, Polonsky WH, Masharani U, Guzman S, Bowyer V, et al. T1-REDEEM: a randomized controlled trial to reduce diabetes distress among adults with type 1 diabetes. In: Diabetes care, vol. 41; 2018. p. 1862–9.
Sadhu AR, Healy AM, Patil SP, Cummings DM, Shubrook JH, Tanenberg RJ. The time is now: diabetes fellowships in the United States. Curr Diab Rep. 2017;17(11):108.
Fremont A, Kim AY, Bailey K, Hanley HR, Thorne C, Dudl RJ, et al. One in five fewer heart attacks: impact, savings, and sustainability in San Diego county collaborative. Health Aff (Millwood). 2018;37(9):1457–65.
Boehmer KR, Abu Dabrh AM, Gionfriddo MR, Erwin P, Montori VM. Does the chronic care model meet the emerging needs of people living with multimorbidity? A systematic review and thematic synthesis. PLoS One. 2018;13(2):e0190852.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Kayla L. Del Valle and Marie E. McDonnell declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Health Care Delivery Systems and Implementation in Diabetes
Rights and permissions
About this article
Cite this article
Del Valle, K.L., McDonnell, M.E. Chronic Care Management Services for Complex Diabetes Management: a Practical Overview. Curr Diab Rep 18, 135 (2018). https://doi.org/10.1007/s11892-018-1118-x
Published:
DOI: https://doi.org/10.1007/s11892-018-1118-x