Abstract
Purpose of Review
Population care approaches for diabetes have the potential to improve the quality of care and decrease diabetes-related mortality and morbidity. Population care strategies are particularly relevant as accountable care organizations (ACOs), patient-centered medical homes (PCMH), and integrated delivery systems are increasingly focused on managing chronic disease care at the health system level. This review outlines the key elements of population care approaches for diabetes in the current health care environment.
Recent Findings
Population care approaches proactively identify diabetes patients through disease registries and electronic health record data and utilize multidisciplinary care teams, personalized provider feedback, and decision support tools to target and care for patients at risk for poor outcomes. Existing evidence suggests that these strategies can improve care outcomes and potentially ameliorate existing race/ethnic disparities in health care. However, such strategies may be less effective for patients who are disengaged from the health care system.
Summary
As population care for diabetes continues to evolve, future initiatives should consider ways to tailor population care to meet individual patient needs, while leveraging improvements in clinical information systems and care integration to optimally manage and prevent diabetes in the future.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is a chronic health condition affecting more than 29 million people in the USA [1]. In addition to its negative effects on patients’ health and quality of life, diabetes is also costly to individual patients, their families, and society at large [2,3,4,5,6,7]. Optimal management of diabetes requires a complex and demanding self-management regimen involving the monitoring of symptoms and blood glucose levels, adherence to medication, efforts at smoking cessation when necessary, and often difficult changes in diet and physical activity level [8–9].
Despite recent decreases in the rates of diabetes-related complications [10], the overall number of diabetes cases has increased steadily in the past decades [11]. For example, the CDC has suggested without major changes in health behaviors, one in three Americans will have diabetes by the year 2050 [12]. Diabetes continues to disproportionately affect vulnerable subgroups such as racial and ethnic minorities and those with low income and education attainment [13, 14]. As diabetes continues to affect larger portions of the US and global populations, effective health care approaches that address diabetes at the population level are urgently needed.
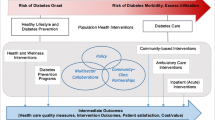
The Chronic Care Model developed by Ed Wagner and colleagues in the 1990s put forth a model of chronic disease care that highlights the role of addressing disease management at the population level [15]. This model emphasizes health care system design strategies that leverage clinical information systems and decision support tools in an effort to optimize population-level disease care, patient self-management, and patient access to community resources. Since the Chronic Care Model was first introduced, health policy initiatives such as accountable care organizations (ACOs), patient-centered medical homes (PCMHs), meaningful use of electronic health records, and Medicare reform have continued to increase the focus on accountability for patient-centered care and outcomes [16,17,18,19,20]. Clinicians, researchers, and health care system leaders face the challenge of creating, maintaining, and improving health care delivery systems that can proactively identify their diabetes populations and provide them with evidence-based patient-centered care. The purpose of this paper is to give an overview of the recent literature and evidence base for current population care management practices and characterize the key components of population health management for diabetes care. In addition, we discuss the role of population-level care in addressing health care disparities and outline a potential research and policy agenda for continuing to improve diabetes population management over time.
Key Components of Diabetes Population Management
Diabetes Population Registries
The starting point for diabetes population management is a comprehensive registry that defines the patients who are in a health care system’s population. In this context, a health care system can be a physician practice, a health plan, an integrated delivery system, or a geographic population at a city, county, state, or national level [21–22]. Registries can be formed using diabetes-related diagnosis, laboratory, and/or prescription data available through both claim databases and electronic health records (EHRs). Early diabetes registries often relied on claim data; however, even as EHR use has become much more widespread [17], the ability to automatically harness individual-level data into registries that can be harnessed for population care may not exist without additional investment and technology. Research suggests that disease registries are a critical component for improving chronic disease care for conditions such as diabetes [23], and that their formation and use are fostered through the use of clinical information systems proposed in the Chronic Care Model framework [24–25]. Once a diabetes registry is formed, it can be used as a foundation for proactive care monitoring and improvement, and to identify and track patients at risk for diabetes complications and related mortality and morbidity. The continued development, maintenance, and expansion of diabetes care registries are an important foundation for population health-level diabetes care moving forward.
Electronic Health Records
While EHR data is not necessary for forming a disease population registry, comprehensive EHR-based data on processes and outcomes of care can significantly improve diabetes registry quality. An EHR allows care data to be linked across care delivery sites (lab, pharmacy, inpatient, outpatient, etc.) to both manage individual care (e.g., individuals overdue for eye exams) and track population-level outcomes (e.g., the proportion of patients with neuropathy) [26]. EHRs can also allow ordering of lab tests and medications at the point of care, provider prompts, and secure messaging between patients and their providers. EHRs also enhance the ability to conduct comparative effectiveness research across a range of diabetes outcomes [27]. Recent research suggests that when clinicians and practices use electronic health records, as opposed to traditional paper-based records, they enhance their ability to provide high-quality diabetes population care [28–29].
Team-Based Diabetes Care
Team-based care that is multidisciplinary, and includes a range of providers across settings, is an important component of population care [26]. A diabetes care team can take many forms but may include primary care physicians, medical assistants (MAs), nurses, health education and behavioral medicine specialists, nutritionists, and endocrinologists. When a diabetes care team has registries and EHR data at its disposal, it can use these tools to proactively identify patients at elevated risk who might not be achieving care goals and outreach to patients to address nutrition, exercise, medication use, and other aspects of self-care that happen at home and within the community. An ideal care team is centered on the patient’s needs and concerns and includes primary care, specialty care, and health education providers [30]. Evidence suggests that when care is provided by a multidisciplinary team in a population context, diabetes complications can be reduced [31]. It is important to note that with team-based care approaches comes an additional need to coordinate care across providers and settings. Population care that uses clinical information tools and data to facilitate care coordination has the potential to maximize efforts and improve health care outcomes [32].
Information on Race/Ethnicity and Preferred Language
When population care management strategies have access to patient-level information on race/ethnicity, and preferred language, they have the potential to identify and address disparities in chronic disease care and outcomes [33••, 34]. One health care system that implemented a population care management program for colorectoral cancer screening that focused on identifying patients overdue for screening and facilitated screening outreach outside of the physician office visit was able to both increase screening rates and reduce disparities [33••]. In another example, one population care management program for hypertension was able to not only increase rates of blood pressure control for the whole population but also decrease the gap in blood pressure control between Blacks/African Americans and Whites by strengthening care teams for hypertension and incorporating culturally tailored communication and self-management tools [35].
Health care providers who deliver care in a patient’s primary language may improve their communication and rapport with patients, which may lead to better outcomes. In one study for example, Spanish-speaking patients who had Spanish-speaking doctors had better adherence to diabetes medications [36]. Access to information about primary language can help health care systems deliver care in the language most appropriate for each patient. When clinical information systems contain the demographic, socioeconomic, and language information necessary for identifying and targeting potentially vulnerable groups, they can be used by care teams to better tailor care in a way that is both language and culturally appropriate [35, 38••], leading to improvements in overall quality and a reduction in disparities.
Decision Support Tools and Feedback
As noted by Wagner and colleagues [15, 23–24], effective models for chronic disease care emphasize decision support tools that can be used to guide evidence-based, guideline-concordant care that is consistent with patient needs and preferences. Registries and EHRs can provide timely information to care teams, and EHRs in particular can be designed to include “best practice alerts” for physicians that flag potential diabetes care concerns and offer evidence-based guidance. Ideally, clinical information systems will include tools that embed evidence-based guidelines directly into practice and further the integration of specialist expertise with primary care [15]. Research suggests that the use of decision support tools as an element of population care, combined with timely feedback to the care team providers on performance of recommended diabetes care practices and patient outcomes, is a key element of effective diabetes population management [22, 37].
Limitations to Current Population Care Approaches and New Directions
Diabetes care processes and outcomes have improved significantly in recent years, during a time when clinical information systems have expanded, and diabetes population care practices, along with key policies and incentives designed to encourage these practices, have grown [38••]. However, there is also evidence that while improvements for the overall population in diabetes complications, morbidity, and mortality have been dramatic, they have been accompanied by potential increases in racial/ethnic disparities in these outcomes [13–14]. A major concern for population care approaches is that while their systematic approach can improve quality of care, their standardization comes with an increased chance that individuals who are not engaged with the health care system may “fall through the cracks” [39]. Population care should be designed in ways that help empower patients to be more engaged with their health care system, address patient-centered outcomes [20], and are in tune with each individual’s barriers and facilitators to receiving optimal care that meets their needs [22, 37]. For example, the Chronic Care Model recommends population care approaches that connect patients with community-based resources that can address disease risk factors outside of the clinical context [15], which can be of particular value for patients who are not regularly accessing the traditional health care system. In addition, mobile applications and other strategies that encourage engagement and sharing of lifestyle and other data between patients and care teams may be important new frontiers for diabetes population care.
Population care for managing chronic conditions has been adopted for a wide range of conditions, including diabetes, congestive heart failure, and hypertension, and implemented across a range of clinical settings within the USA [40]. The US population is aging, and the number of residents who are 65 and older is expected to double by 2050 [41]. As our population ages, the number of patients who have multiple chronic conditions will continue to increase. Approaches to care management are often “siloed” by disease, with different providers responsible for separate clinical areas. Future approaches to population care for diabetes should be well-integrated with care for other chronic conditions a patient may have, reducing the burden on patients and increasing the efficiency of the health care system.
Glasgow and others have suggested that approaches shown to be successful for chronic disease management could be also adopted as an effective approach for preventing diabetes and other chronic diseases [42]. Even as diabetes complication rates decrease, the incidence of diabetes continues to affect significant portions of the population, including younger age groups [10]. Policies such as the recently approved Medicare eligibility for covering Diabetes Prevention Program participation [43] for patients at high risk for developing diabetes are examples of how health care policies can encourage the spread prevention programs at the population level. Leveraging registries of high-risk patients, clinical information systems, feedback, and decision support towards preventing diabetes is an important new frontier in expanding population care principles.
Recommendations for Future Research and Policy
Many research studies have noted that the use of the Chronic Care Model and population-based care strategies are strongly correlated with external incentives and other policy initiatives designed to improve care at the population level [24, 28, 38••, 40, 44]. Our current review of the evidence suggests that population-based approaches to diabetes care have significant potential for continuing to improve diabetes care and outcomes and are well-aligned with current policy initiatives to increase both the accountability and patient centeredness of the US health care system. However, our review of the literature also found that there are a limited number of published evaluations of specific diabetes population care approaches, and those that are published may not have the level of programmatic detail required for dissemination into other settings. Future research in this area should continue to identify, rigorously evaluate, and publish results from high-quality “natural experiments” in diabetes population care management [45].
As we write this review, there are major questions regarding the future of both the Affordable Care Act and Medicare policy, and uncertainty as to what the health care policy landscape holds for chronic disease care in general. However, we believe that issues surrounding the affordability and efficiency of health care will remain top priorities in the coming years, and that the future of diabetes population care initiatives lies on our ability to better understand how to provide the highest value in diabetes care to the largest portion of the population [46]. In addition, it is important that we continue to promote policies and engage in research that helps to ensure that best practices in diabetes population care are implemented and disseminated in ways that ameliorate racial and ethnic disparities in health care outcomes. Research results have a significantly greater potential to directly impact care practices when researchers work closely with patient, clinical, health care system, and policy stakeholders [47–48]. We recommend that those studying how to continue to improve population care for diabetes engage directly with a wide range of stakeholders to help shape the health care policy agenda.
Conclusions
Population care for diabetes that uses effective principles of care management can have a significant impact on diabetes quality and outcomes of care. As population care for diabetes continues to evolve, future research should consider ways to tailor population care to individual patient needs and vulnerable subgroups, while leveraging improvements in information technology and data integration to optimally manage and prevent diabetes in the future.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Centers for Disease Control and Prevention (2011). National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention http://www.cdc.gov/diabetes/pubs/statsreport14.htm. Accessed July 22, 2014.
Fox CS, Coady S, Sorlie PD, D'Agostino Sr RB, Pencina MJ, Vasan RS, et al. Increasing cardiovascular disease burden due to diabetes mellitus: the Framingham Heart Study. Circulation. 2007;115:1544–50.
Franco OH, Steyerberg EW, Hu FB, Mackenbach J, Nusselder W. Associations of diabetes mellitus with total life expectancy and life expectancy with and without cardiovascular disease. ArchInternMed. 2007;167:1145–51.
Rodbard HW, Green AJ, Fox KM, et al. Impact of type 2 diabetes mellitus on prescription medication burden and out-of-pocket healthcare expenses. Diabetes Res Clin Pract. 2010;87(3):360–5.
American Diabetes Association. Economic costs of diabetes in the United States in 2007. Diabetes Care. 2008;31:596–615.
Zhang P, Brown MB, Bilik D, Ackermann RT, Li R, Herman WH. Health utility scores for people with type 2 diabetes in U.S. managed care health plans: results from Translating Research Into Action for Diabetes (TRIAD). Diabetes Care. 2012;35:2250–6.
Dall TM, Zhang Y, Chen YJ, et al. The economic burden of diabetes. Health Aff (Millwood). 2010;29(2):297–303.
American Diabetes Association. Standards of medical care in diabetes 2016. Diabetes Care. 2016;36(Suppl1):S1–2. doi:10.2337/dc16-S001.
Gonder-Frederick LA, Cox DJ, Ritterband LM. Diabetes and behavioral medicine: the second decade. J Consult Clin Psychol. 2002;70:611–25.
Gregg EW, Sattar N, Ali MK. The changing face of diabetes complications. Lancet Diabetes Endocrinol. 2016;4(6):537–47.
Centers for Disease Control. Long Term Trends in Diabetes. https://www.cdc.gov/diabetes/statistics/slides/long_term_trends.pdf. Accessed January 4, 2017.
Centers for Disease Control. Diabetes at a Glance 2016. https://www.cdc.gov/chronicdisease/resources/publications/aag/diabetes.htm. Accessed December 14, 2016.
Agency for Healthcare Research and Quality. 2015 National healthcare quality and disparities report and 5th anniversary update on the national quality strategy. AHRQ Publication No. 16–0015. April 2016.
National Quality Forum. Risk adjustment for socioeconomic status or other sociodemographic factors. Technical report. August 15, 2014.
Wagner Chronic Care Model. http://www.improvingchroniccare.org/index.php?p=1:_Models&s=363. Accessed December 19, 2016.
Schmittdiel JA, Nichols GA, Dyer W, Steiner JF, Karter AJ, Raebel M. Health care system-level approaches to improving performance on Medicare STAR medication adherence metrics for diabetes patients. Med Care. 2015;5394:332–7.
Marcotte L, Seidman J, Trudel K, et al. Achieving meaningful use of health information technology: a guide for physicians to the EHR incentive programs. Arch Intern Med. 2012;172(9):731–6.
Rittenhouse DR, Thom DH, Schmittdiel JA. Developing a policy-relevant research agenda for the patient-centered medical home: a focus on outcomes. J Gen Intern Med. 2010;25(6):593–600.
Rittenhouse DR, Shortell SM, Fisher ES. Primary care and accountable care—two essential elements of delivery-system reform. N Engl J Med. 2009;361(24):2301–3.
Selby JV, Beal AC, Frank L. The Patient-Centered Outcomes Research Institute (PCORI) national priorities for research and initial research agenda. JAMA. 2012;307(15):1583–4.
Schmittdiel J, Bodenheimer T, Solomon NA, Gillies RR, Shortell SM. Brief report: the prevalence and use of chronic disease registries in physician organizations. A national survey. J Gen Intern Med. 2005;20(9):855–8.
Watts, Brook, Renee H. Lawrence, Paul Drawz, Cameron Carter, Amy Hirsch Shumaker, and Elizabeth F. Kern. Development and implementation of team-based panel management tools: filling the gap between patient and population information systems. Population Health Management 19, no. 4 (2016): 232–39. doi:10.1089/pop.2015.0093
Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–9.
Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. The Chronic Care Model part 2. JAMA, October 16, 2002. Vol 288, no. 15.
Li R, Bodenheimer T, Simon J, Gillies RR, Casalino L, Schmittdiel J. Organizational factors affecting the adoption of diabetes care management process in physician organizations. Diabetes Care. 2004;27(10):2312–6.
Neuwirth EE, Schmittdiel J, Tallman K, Bellows J. Panel management population care program adoption and spread: what have we learned? Perm J. 2007;11(3):12–20.
Kuyakov R, Bowen J, Ewen E, West SL, Daoud Y, Fleming N, Masica A. Electronic health record use to classify patients with newly diagnosed versus preexisting type 2 diabetes: infrastructure for comparative effectiveness research and population health management. Popul Health Manag. 2012;15(1):3–11.
Vaghefi I, Hughes JB, Law S, Lortie M, Leaver C, Lapointe L. Understanding the impact of electronic medical record use on practice-based population health management: a mixed-method study. JMIR Med Inform. 2016;4:e10.
Sequist TD, Adams A, Zhang F, Ross-Degnan D, Ayanian JZ. Effect of quality improvement on racial disparities in diabetes care. Arch Intern Med. 2006;166(6):675–81.
Wagner EH. The role of patient care teams in chronic care management. BMJ 2000.
Krishnan S, Nash F, Baker N, Fowler D, Rayman G. Reduction in diabetic amputations over 11 years in a defined U.K. population: benefits of multidisciplinary team work and continuous prospective audit. Diabetes Care. 2008;31(1):99–101.
Rushton S. The population care coordination process. Prof Case Manag. 2015;20(5):230–8. quiz 239-40. doi:10.1097/NCM.0000000000000105.
•• Berkowitz SA, Percac-Lima S, Ashburner JM, Chang Y, Zai AH, He W, Grant RW, Atlas SJ. Building equity improvement into quality improvement: reducing socioeconomic disparities in colorectal cancer screening as part of population health management. J Gen Intern Med. 2015;30(7):942–9. doi:10.1007/s11606-015-3227-4. This study gives a strong example of an intervention to improve population care outreach and reduce disparities and uses a robust evaluation approach to determine its effectiveness.
Tsui EW, Wang G, Zahler A, Simoyan OM, White MV, Mckee M. A multilingual population health management program. J Ambul Care Manage. 2013;36(2):140–6.
Bartolome RE, Chen A, Handler J, Platt ST, Gould B. Population care management and team-based approach to reduce racial disparities among African Americans/blacks with hypertension. Perm J. 2016;20(1):53–9. doi:10.7812/TPP/15-052.
Traylor A, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. Adherence to cardiovascular disease medications: does patient-provider race/ethnicity and language concordance matter? J Gen Intern Med. 2010;25(11):1172–7.
Beaverson, Janice M., and Jaewon Ryu. Quality at Kaiser Permanente: using the population care model. Maryland Medicine : MM : A Publication of MEDCHI, the Maryland State Medical Society 12, no. 2 (2011): 15, 17.
•• Wiley JA, Rittenhouse DR, Shortell SM, Casalino LP, Ramsay PP, Bibi S, Ryan AM, Copeland KR, Alexander JA. Managing chronic illness: physician practices increased the use of care management and medical home processes. Health Aff (Millwood). 2015;34(1):78–86. This important policy paper outlines the increase in population care management processes nationally and ties them to key policy innovations such as pubic reporting and pay for performance.
Buetow S, Getz L, Adams P. Individualized population care: linking personal care to population care in general practice. J Eval Clin Pract. 2008;14(5):761–6. doi:10.1111/j.1365-2753.2007.00938.x.
Casalino L, Gillies RR, Shortell SM, Schmittdiel J, Bodenheimer T, Oswald N, Schauffler H, Wang MC. External incentives, information technology, and organized processes to improve health care quality for patients with chronic diseases. JAMA. 2003;289(4):434–41.
US Census. An aging nation: the older population in the United States. https://www.census.gov/prod/2014pubs/p25–1140.pdf. Accessed January 4, 2017.
Glasgow RE, Orleans CT, Wagner EH, Curry SJ, Solberg LI. Does the chronic care model serve as a template for improving prevention? The Milbank Quarterly. 79(4):579–612.
Centers for Medicare and Medicaid Services. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2016-Fact-sheets-items/2016-07-07.html. Accessed January 5, 2017.
Bojadzievski T and Gabbay RA. Patient-centered medical home and diabetes. Diabetes Care. 34: 1047–1053.
Ackermann RT, Duru K, Albu J, Schmittdiel JA, Soumerai SB, Ali MK, Gregg E. Evaluating diabetes health policies using natural experiments: the natural experiments for translation in diabetes (NEXT-D) study. Am J Prev Med. 2015;48(6):747–54.
Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759–69.
Schmittdiel J, Grumbach K, Selby JV. Health care system-based participatory research: an approach for sustainable translational research and quality improvement. Ann Fam Med. 2010;8(3):256–9.
Schmittdiel JA, Desai J, Schroeder E, Paolino A, Nichols G, Lawrence J, O’Connor P, Ohnsorg K, Newton K, Steiner J. Methods for engaging stakeholders in comparative effectiveness research: a patient-centered approach to improving diabetes care. Healthc(Amst). 2015;3(2):80–8.
Acknowledgements
This work was supported by NIDDK grant numbers 5R18DK104249 and 2P30-DK092924.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Julie Schmittdiel, Anjali Gopalan, Mark Lin, Somalee Banerjee, Christopher Chau, and Alyce Adams declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any new studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Economics and Policy in Diabetes
Rights and permissions
About this article
Cite this article
Schmittdiel, J.A., Gopalan, A., Lin, M.W. et al. Population Health Management for Diabetes: Health Care System-Level Approaches for Improving Quality and Addressing Disparities. Curr Diab Rep 17, 31 (2017). https://doi.org/10.1007/s11892-017-0858-3
Published:
DOI: https://doi.org/10.1007/s11892-017-0858-3