Abstract
Outside pregnancy, HbA1c analysis is used for monitoring, screening for and diagnosing diabetes and prediabetes. During pregnancy, the role for HbA1c analysis is not yet established. Physiological changes lower HbA1c levels, and pregnancy-specific reference ranges may need to be recognised. Other factors that influence HbA1c are also important to consider, particularly since emerging data suggest that, in early pregnancy, HbA1c elevations close to the reference range may both identify women with underlying hyperglycaemia and be associated with adverse pregnancy outcomes. In later pregnancy, HbA1c analysis is less useful than an oral glucose tolerance test (OGTT) at detecting gestational diabetes. Postpartum, HbA1c analysis detects fewer women with abnormal glucose tolerance than an OGTT, but the ease of testing may improve follow-up rates and combining HbA1c analysis with fasting plasma glucose or waist circumference may improve detection rates. This article discusses the relevance of HbA1c testing at different stages of pregnancy.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
HbA1c analysis was recently endorsed as a screening test for unrecognised diabetes in both the general population and in early pregnancy [1–3]. HbA1c analysis is more convenient and more reproducible with less pre-analytical error than measures of blood glucose. We know from pregnancy data in women with pre-existing diabetes, that strict glucose control and HbA1c levels as close to normal as possible improve pregnancy outcomes. However, when considering HbA1c as a screening test in early pregnancy to detect significant glucose elevations in women without known diabetes, there are few data to inform clinicians as to what HbA1c threshold should be used for intervention. As the relationship between measures of glycaemia and adverse pregnancy outcomes is a continuum, any HbA1c threshold recommended for intervention will probably be reached by consensus [4]. In addition to early HbA1c testing, there is interest in exploring the value of measuring HbA1c at other stages during pregnancy and for postpartum follow-up in women with a diagnosis of gestational diabetes (GDM). In this review, we examine the published data and identify the pitfalls and potential uses of HbA1c analysis at each stage of pregnancy and postpartum.
Factors Affecting the Applicability of HbA1c as a Diagnostic Test
The accuracy of HbA1c as a measure of an individual’s level of glycaemia is affected primarily by conditions that affect red blood cell survival time or non-enzymatic glycation of haemoglobin [5]. A reduced red blood cell survival time will lower the HbA1c level and may lead to a false negative result, for example in any haemolytic anaemia, chronic renal failure, severe liver disease and anaemia of chronic disease. HbA1c levels also fall in most women in early pregnancy, which is thought to relate to increased red cell production and a decrease in fasting blood glucose levels [6, 7].
An important factor that influences HbA1c levels is iron deficiency, which becomes more common during pregnancy. Whether there is an associated anaemia and whether iron replacement is underway are also considerations, all of which were reviewed recently [8]. Iron deficiency may prolong red cell survival and increase HbA1c levels [9]. Studies in both non-pregnant and pregnant populations show that iron deficiency can lead to a 1–1.5 % relative rise in HbA1c, or an absolute increase of 1–2 mmol/mol (0.1–0.2 %), which falls after treatment hypothesised to be due to an associated increase in immature red cells [10, 11•]. Within the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2006, healthy women (n = 6666) aged 18 years or older underwent studies of iron parameters, haemoglobin and HbA1c [12]; 13.7 % had iron deficiency and 4.0 % had iron deficiency anaemia. After adjustment for other factors, iron deficiency was associated with a small upward shift in HbA1c at lower levels, so there was a greater odds of having an HbA1c ≥37 mmol/mol (5.5 %), odds ratio (OR) 1.39 (95 % confidence interval (CI) 1.11–1.73), but no greater odds of HbA1c ≥6.5 % (48 mmol/mol), OR 0.79 (0.33–1.85). In pregnancy, iron status may be relevant for some individuals whose HbA1c level is close to a referral threshold.
Congenital variants of the haemoglobin molecule (haemoglobinopathies), which may be relatively common in certain ethnic communities (e.g. African, Mediterranean), affect the HbA1c result, principally due to interference with the laboratory measurement of HbA1c (usually lowering the result). Susceptibility to interference varies between methodologies, and the National Glycohemoglobin Standardization Program (NGSP) provides a summary of the effect of common haemoglobinopathies on measurement of HbA1c levels using various methods [13]. However, any HbA1c result that is not consistent with clinical expectations, or the results of self-monitored capillary blood glucose readings, should alert the medical practitioner to consider a potential problem. Some methodologies for HbA1c measurement (such as boronate affinity chromatography) are less susceptible to the effects of haemoglobinopathies and should be considered in populations with a higher prevalence of haemoglobinopathies or as an additional test when one is suspected. A diagnosis of abnormal haemoglobin should also be confirmed by appropriate investigations. Some recommendations indicate that if a haemoglobin variant is suspected, then HbA1c is not an appropriate diagnostic test and glucose-based criteria should be preferred [14].
Ethnic Variations in HbA1c
There are data reporting different HbA1c ranges between some ethnic groups. In the USA, data suggest that African Americans have higher HbA1c values than Mexicans and non-Hispanic Whites [15]. In groups with similar glucose tolerance by glucose measures, the mean HbA1c levels were 4 mmol/mol (0.4 %) higher in African American and 3 mmol/mol (0.3 %) higher in Asian compared with Caucasian women [16]. Similarly, in the UK, South Asians had an HbA1c measure 2 mmol/mol (0.2 %) higher than white Europeans [17, 18]. It is not known whether these ethnic variations relate to differences in the prevalence of conditions affecting erythrocyte turnover, genetic glycation differences, or differences in glycaemia that are not represented by the fasting and 2-h plasma glucose levels of the oral glucose tolerance test (OGTT). Studies incorporating additional glucose measures and clinical outcomes will answer this in the future. This issue also brings into consideration the presumption that the OGTT is a gold standard for diagnosis, which may not necessarily be the case.
Amongst other caveats, the HbA1c assay also needs to be reliable and consistent across different centres. In a recent Australian study, from whole blood samples sent to more than 200 laboratories, more than 90 % of HbA1c results fell within 6 % of the median and further improvements in comparability of HbA1c measurements may be expected [19].
HbA1c Reference Range in Pregnancy
HbA1c measurement during pregnancy is typically used to monitor control in women with pre-existing diabetes. Recently, HbA1c analysis has been introduced to screen for unrecognised pre-existing diabetes at the first antenatal visit. There is also interest in finding an HbA1c threshold that is useful for intervention, so understanding pregnancy-specific reference ranges is important.
From early in the first trimester, HbA1c levels fall, reaching a nadir in the early second trimester [7] when levels are consistently reported as lower than in non-pregnant controls as summarised in Table 1 [20–26]. It appears that in Caucasian and Japanese women, an HbA1c level above 39 mmol/mol (5.7 %) should be considered elevated in the first and second trimesters of pregnancy. Further data are required in other ethnic groups.
In later pregnancy, reported reference ranges vary (Table 1). This inconsistency may be contributed to by differences in both the iron status between groups and the methodology of excluding women with GDM.
HbA1c and Pregnancy Outcomes
Periconceptual and First Trimester HbA1c Levels
Most data reporting peri-conception and first trimester measurements of HbA1c and pregnancy outcomes come from studies of women with pre-existing diabetes. Based on these data, guidelines recommend that women should aim for glucose levels as close to normal as possible peri-conception [3, 27]. There are only a few reports of pregnancy outcomes in women with prediabetes, or in women without known diabetes, who had an early pregnancy HbA1c measurement.
Women with pre-existing diabetes have increased risks of perinatal loss, which is associated with the degree of HbA1c elevation at conception and through pregnancy [25, 28–32]. Additional factors are likely to contribute to some losses, particularly in women with type 2 diabetes who are more likely to be obese and may have socio-economic factors contributing to poor pregnancy outcomes [33, 34].
A significant proportion of perinatal losses relate to congenital anomalies. A review of studies reporting an association between risk of congenital anomaly and peri-conception HbA1c levels showed a direct relationship between HbA1c level and risk [35]. A linear relationship down to an HbA1c of 45 mmol/mol (6.3 %) has been demonstrated in a more recent large study [36•], with an absolute increase in risk of anomaly of 2 % with every 11 mmol/mol (1 %) increase in HbA1c. The authors noted that this relationship may continue with lower HbA1c levels, but the number of women with an HbA1c below 45 mmol/mol (6.3 %) was too small to assess this. In a study of women without known diabetes who had an HbA1c measured in early pregnancy, those with an HbA1c of 41–46 mmol/mol (5.9–6.4 %) had higher rates of major congenital anomaly compared with women whose HbA1c was lower (relative risk (RR) 2.67; 95 % CI 1.28–5.53), though this finding was not adjusted for other possible factors, such as maternal body mass index (BMI) [37•].
The HbA1c level in early pregnancy is also associated with other pregnancy outcomes. In a study of 1505 women with known diabetes, when analysing birth weight as a continuous measure, increasing peri-conception HbA1c was independently associated with lower birth weight [38•]. The authors suggest that, as hyperglycaemia interferes with trophoblast proliferation and invasion, poor placentation may limit later growth [38•, 39]. This theory may also explain the reported independent association between an elevated HbA1c in early pregnancy and risk of preeclampsia in women with type 1 diabetes [40]. Women without known diabetes who had an early HbA1c of 41–46 mmol/mol (5.9–6.4 %) and who were not subsequently diagnosed with GDM, had increased unadjusted risks of preeclampsia, preterm birth, shoulder dystocia and perinatal loss compared with women with lower HbA1c [37•]. Some of these pregnancy outcomes are likely to be influenced by continuing glucose elevations beyond the first trimester.
Second and Third Trimester HbA1c Levels
Studies in women with pre-existing diabetes demonstrate that higher HbA1c levels in the second and third trimesters relate to pregnancy outcomes such as perinatal death [30, 41], preeclampsia [40, 41], macrosomia [41–44] and preterm birth [41]. In a prospective study of 725 women with type 1 diabetes, women with an HbA1c <42 mmol/mol (6 %) at 26 and 34 weeks were used as the reference group and outcomes of women with higher HbA1c levels were compared [45•]. Women with an HbA1c of 42–46 mmol/mol (6.0–6.4 %) at 26 weeks, had an increased risk of delivering a large for gestational age (LGA) baby, adjusted OR 1.7 (95 % CI 1.0–3.0), and those with an HbA1c of 48–52 mmol/mol (6.5–6.9 %) were at increased risk of preterm birth (OR 2.5; 95 % CI 1.3–4.8), preeclampsia (OR 4.3; 95 % CI 1.7–10.8) and neonatal hypoglycaemia requiring a glucose infusion (OR 2.9; 95 % CI 1.5–5.6). These risks increased further with increasing HbA1c levels. There was a similar relationship with HbA1c and outcomes at 34 weeks gestation. These data support tight glucose control through pregnancy, aiming for an HbA1c as close to the reference range as possible.
In women with known diabetes, there is a complex association between a third trimester HbA1c level and birth weight, as there is an interaction with the peri-conception HbA1c level. The study reporting that high peri-conception HbA1c levels independently predicted lower birth weight also found that an increasing third trimester HbA1c value up to 53 mmol/mol (7 %) was independently associated with higher birth weight. However, there was no association found for third trimester HbA1c values above 53 mmol/mol (7 %) when analysing birth weight as a continuous measure. This suggests that in women with a high early pregnancy HbA1c level, an ‘appropriately grown’ foetus by third trimester ultrasound scan should not necessarily be seen as reassuring.
For women with GDM, a number of centres measure HbA1c at the time of diagnosis and again at 36–37 weeks gestation and use this information to gauge glycaemic control and level of risk. In a small study of women with GDM who all had HbA1c ≤42 mmol/mol (6 %) at diagnosis, women with an HbA1c >34 mmol/mol (5.3 %) either at diagnosis or in late pregnancy, had a twofold increased risk of adverse outcomes (which included pregnancy hypertension, abnormal liquor volume, LGA and neonatal morbidity) [46]. The risk was highest in women with an HbA1c >34 mmol/mol (5.3 %) in late pregnancy. A number of studies have examined the relationship between HbA1c level at diagnosis of GDM and risk of LGA and results are varied, some finding an association [47, 48] and others not [49]. In the metformin in gestational diabetes (MiG) trial, the HbA1c at recruitment (mean (standard deviation (SD)) 40 (6) mmol/mol (5.8 (0.7) %)) was also associated with risk of preeclampsia [48, 50]. Trials have shown that treating women with GDM reduces the risk of LGA and preeclampsia [51, 52], which may explain the variable association between HbA1c at diagnosis and these outcomes. Gestation at diagnosis and adherence to treatment are likely factors, and it may be that a later measure of HbA1c in women with GDM is a better marker of risk.
There are also outcome data relating to HbA1c measurements in the second or early third trimester in women with risk factors for GDM but without an OGTT diagnosis. In women with a positive initial screen for GDM but normal OGTT, maternal BMI and HbA1c at the time of the OGTT predicted birth weight but weight gain and fasting glucose did not [53]. In a UK study, pregnancy outcomes were compared in low risk women who were not screened for GDM (n = 32,198) and in women with risk factors who were screened with an OGTT and HbA1c at 28 weeks (n = 7577). Logistic regression showed that high-risk women with a negative OGTT had higher rates of macrosomia and that a subgroup of them with an HbA1c ≥42 mmol/mol (6 %) (n = 157) also had higher rates of preterm birth (OR 1.63 (1.02–2.61)) and stillbirth (OR 4.87 (1.78–13.29) than the low risk group [54]. Finally, HbA1c was analysed at delivery in a small study of obese women who did not have GDM by The International Association of the Diabetes and Pregnancy Study Groups (IADPSG) criteria. An HbA1c at delivery ≥39 mmol/mol (5.7 %) was associated with increased risk of LGA infants (OR 3.1 [95 % CI 1.2–7.6]) and neonatal hypoglycaemia (6.2 [1.3–29]) compared with similar obese women with a lower HbA1c [55].
HbA1c levels were also analysed in the Hyperglycaemia and Adverse Pregnancy Outcomes (HAPO) study, which examined the relationship between glycaemia measures at 28 weeks and pregnancy outcomes. HbA1c values (mean (SD) 29 (4) mmol/mol, 4.8 (0.4) %), measured in over 21,000 women, were predictive of pregnancy outcomes, although less so than glucose measures [4].
These data raise questions for further research, to determine whether measuring HbA1c at different stages of pregnancy can provide important information to guide clinical practice and improve pregnancy outcomes.
HbA1c as a Screening Test
HbA1c analysis may be appropriate to detect women who enter pregnancy with underlying hyperglycaemia but less useful for detecting women who develop GDM in later pregnancy. Unfortunately, the terminology used to describe different degrees of hyperglycaemia in pregnancy does not readily distinguish between these two different clinical entities, so it can create confusion. In general, GDM has been used as an umbrella term for any degree of hyperglycaemia identified in pregnancy. More recently, the WHO, IADPSG and others have added a term ‘overt diabetes’ or ‘diabetes in pregnancy’ to define women with glucose elevations in pregnancy that meet non-pregnancy definitions for diabetes. An early pregnancy screen for pre-existing diabetes is recommended and, as a result, women with lesser degrees of hyperglycaemia, such as prediabetes, will be identified. Often these women are labelled as having GDM, but they differ from women who develop GDM in the second half of pregnancy. For the purposes of this review, we use the terms ‘early GDM’ to describe women who enter pregnancy with pre-existing glucose elevations below the threshold used to define diabetes and ‘later GDM’ to describe women who develop hyperglycaemia in the second half of pregnancy.
It is not yet clear if in early pregnancy, women meeting IADPSG OGTT criteria for GDM, or women with elevated HbA1c levels below the threshold for diagnosis of ‘diabetes’, benefit from early intervention. The ADA state that GDM should only be diagnosed in the second and third trimesters of pregnancy.
HbA1c in Early Pregnancy: for Unrecognised Pre-existing Diabetes and ‘Early GDM’
When HbA1c was endorsed as a potential screening test, a non-pregnancy threshold was recommended to define diabetes (48 mmol/mol (6.5 %)) in pregnancy [2, 3]. However, do the HbA1c thresholds used for classifying diabetes outside of pregnancy apply given that HbA1c levels drop significantly in early pregnancy? In addition, there is currently no recommended or accepted HbA1c threshold to define ‘early GDM’.
A large observational study examined the performance of an early pregnancy HbA1c [37•]. The optimal HbA1c threshold to detect women who had a diagnosis of diabetes by OGTT (fasting ≥ 7 mmol/L, 126 mg/dl or 2 h ≥ 11.1 mmol/L, 200 mg/dl) before 20 weeks was reported as 41 mmol/mol (5.9 %). This HbA1c threshold detected all cases of diabetes and was highly specific 98.4 % (95 % CI 97–99 %) for ‘early GDM’ by IADPSG OGTT criteria. Applying an HbA1c threshold of 48 mmol/mol (6.5 %) to this cohort missed 47 % of women with undiagnosed diabetes.
There are reports of significant hyperglycaemia in women with early pregnancy HbA1c levels within the threshold used to define prediabetes outside pregnancy. In small studies of women referred for blood sugar monitoring and lifestyle intervention because of an isolated elevated HbA1c, approximately 50 % with an HbA1c ≥39 mmol/mol (5.7 %) [56•], and >90 % with HbA1c ≥41 mmol/mol (5.9 %) [57, 58•], required pharmacotherapy (mostly initiated before 21 weeks gestation) to maintain euglycaemia. However, does this early intervention translate into improved outcomes? Large RCTs are required to provide answers, but emerging data suggests that intervention before 20–24 weeks may improve outcomes, with reported lower rates of preeclampsia [59]. The authors speculated that a larger study might also show a reduction in preterm birth. A preliminary report from a small RCT showed improved glycaemia in later pregnancy with early intervention [60]. It is interesting that preeclampsia, preterm birth, and caesarean section, were the HAPO study outcomes that were still associated with the 28-week HbA1c level after adjustment for glucose measures and the authors speculated that these outcomes might be most influenced by earlier glycaemia [61].
In early pregnancy, there should be no need to perform confirmatory OGTTs in women who are identified to have hyperglycaemia by HbA1c and it may just create a dilemma as to which test to act on. In a multi-ethnic population of women referred to a diabetes in pregnancy clinic, there was a subgroup with an HbA1c ≥41 mmol/mol (5.9 %) but non-diagnostic OGTT. The HbA1c predicted significant hyperglycaemia, as confirmed by subsequent capillary glucose monitoring and the need for medication [58•].
HbA1c in Early Pregnancy: as a Predictor for an OGTT Diagnosis of ‘Later GDM’
In these studies, the focus is not on detecting hyperglycaemia per se but how the HbA1c predicts a diagnostic OGTT in early or later pregnancy. These studies confirm that most women with ‘later GDM’ do not have an elevated HbA1c in early pregnancy [37•, 59, 62], so the 24–28-week OGTT is still required.
For ‘early GDM’, HbA1c levels of 40–42 mmol/mol (5.8–6.0 %) are reported to have a high specificity and positive predictive value for detecting women who meet OGTT criteria for GDM at some stage in pregnancy [37•, 63–65]. These data provide further evidence to suggest there may be a useful HbA1c threshold above which an OGTT is not required.
For ‘later GDM’, early pregnancy HbA1c levels positively correlate with risk [62]. One study found that for every 1.0-point increase in HbA1c measured at 11–14+6 weeks gestation, the odds of GDM by OGTT at 22–33 + 6 weeks was 13.9 (95 % CI 2.6–68.0) [66]. The relationship was attenuated after adjusting for age, race, obesity and GDM history (adj. OR 5.1 (95 % CI 0.8–34.7).
HbA1c in Later Pregnancy: as a Predictor for an OGTT Diagnosis of ‘Later GDM’ and/or as an Adjunct Test for Hyperglycaemia in Women with a Non-diagnostic OGTT
Most women with ‘later GDM’ will have an HbA1c <41 mmol/mol (<5.9 %) at the time of diagnosis [67–69], and there is a significant overlap in HbA1c levels between women with and without GDM [68, 70]. Although HbA1c analysis will not replace the 24–28-week OGTT, could it have a role as an adjunct test in high-risk women with a non-diagnostic OGTT? An HbA1c ≥42 mmol/mol (6.0 %) measured in late pregnancy had a high specificity for GDM by OGTT, 97.2 % [68]. Correspondingly, a small observational study found that women with a non-diagnostic OGTT and an HbA1c ≥41 mmol/mol (5.9 %) had significant glucose elevations, with >70 % referred after 24 weeks requiring pharmacotherapy in addition to dietary intervention [58•]. These women had higher BMI and were more likely of Pacific ethnicity than women diagnosed with GDM by OGTT criteria.
Postpartum HbA1c: for Persistent Hyperglycaemia in Women with Recent GDM
Postpartum follow-up of women with GDM is important, as there is a high rate of progression to type 2 diabetes (RR 7.43; 95 % CI 4.79–11.51) compared with women with no GDM history [71]. Worldwide, the uptake of postpartum screening following gestational diabetes is suboptimal, often less than 50 % [72–75]. HbA1c measurement would be a much more convenient test for postpartum hyperglycaemia and HbA1c testing compared with OGTT doubled postpartum screening rates in one community [76].
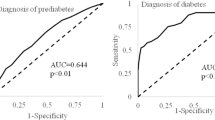
Unfortunately, the reported sensitivity of HbA1c at detecting postpartum hyperglycaemia (diabetes and prediabetes) by OGTT is low. The correlation between HbA1c levels and OGTT is especially poor in the first 6–12 weeks post-delivery and improves with increasing delivery-to-test interval [77, 78]. This may be related to early postpartum changes in red cell turnover and iron status and to the legacy of antenatal treatment for GDM. A meta-analysis of studies published up to 2013, including 1086 women in total, calculated a pooled sensitivity of 0.36 (95 % CI 0.23–0.52) and specificity 0.85 (0.73–0.92) for an HbA1c threshold of 39 mmol/mol (5.7 %) at detecting any degree of postpartum abnormal glucose tolerance by OGTT [79]. A further three studies, including 483 women, report similar results, sensitivity range 0.30–0.57 and specificity range 0.70–0.95 [80, 81•, 82]. The predictive value of HbA1c varies depending both on the prevalence of abnormal glucose tolerance in the given population and the time interval to postpartum testing.
However, data show that a postpartum HbA1c is a marker of risk. For example, women with HbA1c levels ≥39 mmol/mol (5.7 %) vs. those with HbA1c <39 mmol/mol (5.7 %) had more vascular risk factors including a higher BMI and lower HDL cholesterol [74]. Furthermore, an elevated HbA1c test identifies an additional group of women with prediabetes missed by OGTT, and in one study, this additional group had higher LDL cholesterol and where more likely to be Caucasian [73].
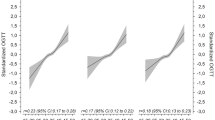
Could HbA1c analysis in combination with other tests replace the cumbersome postpartum OGTT? Studies examining combined screening with fasting plasma glucose (FPG) and HbA1c have conflicting results. In two studies, combined screening did not appreciably improve detection rates above using FPG alone [74, 82]. Whereas two studies report improved detection rates, both concluding that a two-step screening approach would decrease the need for postpartum OGTT by >70 %; HbA1c ≥39 mmol/mol (5.7 %) and FPG ≥5.6 mmol/l (>100 mg/dl) had a sensitivity of 0.9 and specificity of 0.84 [80], and HbA1c ≥37 mmol/mol (5.5 %) and FPG ≥6.1 mmol/l (110 mg/dl) had a sensitivity of 0.82 and specificity of 0.92 [77]. One study examined combined screening using HbA1c ≥39 mmol/mol (5.7 %) and waist circumference >88 cm, which improved detection rates above using HbA1c alone, sensitivity 0.78 vs. 0.48 [83].
It is not known whether combined screening with HbA1c improves screening rates over OGTT alone. RCTs are required to compare the uptake and effectiveness of different screening protocols in diverse ethnic groups. Studies examining serial screening with HbA1c +/− FPG at 3–6-monthly intervals for the first year, compared to a single OGTT at 6 weeks postpartum may also be worth considering. Moreover, all women with a history of GDM should have ongoing healthy lifestyle interventions irrespective of their early postnatal screening result. Subsequent HbA1c monitoring may be enough to determine whether they need more intensive management strategies put into place.
Conclusion
HbA1c analysis in pregnancy is likely to become an increasingly useful tool, as long as pregnancy-specific reference ranges are developed and the various pitfalls are considered (as summarised in Table 2). Further research is required to investigate whether there is an important difference in HbA1c reference range in pregnancy by ethnicity, or whether the differences noted relate to other factors. Emerging data suggest that an HbA1c ≥41 mmol/mol (5.9 %) is a marker of hyperglycaemia in pregnancy irrespective of the OGTT and that it is associated with an increased risk of adverse pregnancy outcome. These findings need confirming by larger studies, and randomised trials are required to assess whether early intervention in women with elevated HbA1c levels in the prediabetes range is of benefit.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Metzger BE, Gabbe SG, Persson B, et al. International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33(3):676–82.
WHO: Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy [http://www.who.int/diabetes/publications/Hyperglycaemia_In_Pregnancy/en/] Accessed on: 10 August 2015.
American Diabetes Association. Classification and diagnosis of diabetes. Diabetes Care. 2015;38 Suppl:S8-S16. doi:10.2337/dc15-S005.
Metzger BE, Lowe LP, Dyer AR, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358(19):1991–2002.
Jiao Y, Okumiya T, Saibara T, et al. Abnormally decreased HbA1c can be assessed with erythrocyte creatine in patients with a shortened erythrocyte age. Diabetes Care. 1998;21(10):1732–5.
Lind T, Billewicz WZ, Brown G. A serial study of changes occurring in the oral glucose tolerance test during pregnancy. J Obstet Gynaecol Br Commonw. 1973;80(12):1033–9.
Worth R, Potter JM, Drury J. Glycosylated haemoglobin in normal pregnancy: a longitudinal study with two independent methods. Diabetologia. 1985;28(2):76–9.
Ahmad J, Rafat D. HbA1c and iron deficiency: a review. Diabetes Metab Syndr. 2013;7(2):118–22.
Coban E, Ozdogan M, Timuragaoglu A. Effect of iron deficiency anemia on the levels of hemoglobin A1c in nondiabetic patients. Acta Haematol. 2004;112(3):126–8.
El-Agouza I, Abu Shahla A, Sirdah M. The effect of iron deficiency anaemia on the levels of haemoglobin subtypes: possible consequences for clinical diagnosis. Clin Lab Haematol. 2002;24(5):285–9.
Rafat D, Rabbani TK, Ahmad J, et al. Influence of iron metabolism indices on HbA1c in non-diabetic pregnant women with and without iron-deficiency anemia: effect of iron supplementation. Diabetes Metab Syndr. 2012;6(2):102–5. This study reports the changes to HbA1c levels in pregnant women associated with iron deficiency and subsequent iron replacement.
Kim C, Bullard KM, Herman WH, et al. Association between iron deficiency and A1C Levels among adults without diabetes in the National Health and Nutrition Examination Survey, 1999-2006. Diabetes Care. 2010;33(4):780–5.
NGSP: HbA1c methods: effects of hemoglobin variants (HbC, HbS, HbE and HbD traits) and elevated fetal hemoglobin (HbF). [http://www.ngsp.org/interf.asp] Accessed on 10 August 2015.
Braatvedt G, Cundy T, Crooke M, et al. Understanding the new HbA1c units for the diagnosis of type 2 diabetes. NZ Med J. 2012;125(1362):70–80.
Ziemer DC, Kolm P, Weintraub WS, et al. Glucose-independent, black-white differences in hemoglobin A1c levels: a cross-sectional analysis of 2 studies. Ann Intern Med. 2010;152(12):770–7.
Herman WH, Ma Y, Uwaifo G, et al. Differences in A1C by race and ethnicity among patients with impaired glucose tolerance in the Diabetes Prevention Program. Diabetes Care. 2007;30(10):2453–7.
Likhari T, Gama R. Glycaemia-independent ethnic differences in HbA(1c) in subjects with impaired glucose tolerance. Diabet Med. 2009;26(10):1068–9.
Mostafa SA, Davies MJ, Webb DR, et al. Independent effect of ethnicity on glycemia in South Asians and white Europeans. Diabetes Care. 2012;35(8):1746–8.
Florkowski C. HbA1c as a diagnostic test for diabetes mellitus—reviewing the evidence. Clin Biochem Rev. 2013;34:75–83.
Versantvoort AR, van Roosmalen J, Radder JK. Course of HbA1c in non-diabetic pregnancy related to birth weight. Neth J Med. 2013;71(1):22–5.
O’Shea P, O’Connor C, Owens L, et al. Trimester-specific reference intervals for IFCC standardised haemoglobin A(1c): new criterion to diagnose gestational diabetes mellitus (GDM)? Ir Med J. 2012;105(5 Suppl):29–31.
Hiramatsu Y, Shimizu I, Omori Y, et al. Determination of reference intervals of glycated albumin and hemoglobin A1c in healthy pregnant Japanese women and analysis of their time courses and influencing factors during pregnancy. Endocr J. 2012;59(2):145–51.
Mosca A, Paleari R, Dalfra MG, et al. Reference intervals for hemoglobin Alc in pregnant women: data from an Italian multicenter study. Clin Chem. 2006;52(6):1138–43.
Radder JK, van Roosmalen J. HbAIC in healthy, pregnant women. Neth J Med. 2005;63(7):256–9.
Nielsen L, Ekbom P, Damm P, et al. HbA1c levels are significantly lower in early and late pregnancy. Diabetes Care. 2004;27(5):1200–1.
O’Kane MJ, Lynch PLM, Moles KW, et al. Determination of a diabetes control and complications trial-aligned HbA1c reference range in pregnancy. Clin Chim Acta. 2001;311(2):157–9.
National Institute for Health and Care Excellence: Diabetes in pregnancy: management of diabetes and its complications from preconception to the postnatal period. [https://www.nice.org.uk/guidance/ng3] Accessed on: 10 August 2015.
Temple R, Aldridge V, Greenwood R, et al. Association between outcomes of pregnancy and glycaemic control in early pregnancy in type 1 diabetes: population based study. BMJ. 2002;325(7375):1275–6.
Dunne FP, Avalos G, Durkan M, et al. ATLANTIC DIP: pregnancy outcome for women with pregestational diabetes along the Irish Atlantic seaboard. Diabetes Care. 2009;32(7):1205–6.
Jensen DM, Korsholm L, Ovesen P, et al. Peri-conceptional A1C and risk of serious adverse pregnancy outcome in 933 women with type 1 diabetes. Diabetes Care. 2009;32(6):1046–8.
Murphy HR, Steel SA, Roland JM, et al. Obstetric and perinatal outcomes in pregnancies complicated by type 1 and type 2 diabetes: influences of glycaemic control, obesity and social disadvantage. Diabet Med. 2011;28(9):1060–7.
Tennant PW, Glinianaia SV, Bilous RW, et al. Pre-existing diabetes, maternal glycated haemoglobin, and the risks of fetal and infant death: a population-based study. Diabetologia. 2014;57(2):285–94.
Cundy T, Gamble G, Neale L, et al. Differing causes of pregnancy loss in type 1 and type 2 diabetes. Diabetes Care. 2007;30(10):2603–7.
Balsells M, Garcia-Patterson A, Gich I, et al. Maternal and fetal outcome in women with type 2 versus type 1 diabetes mellitus: a systematic review and metaanalysis. J Clin Endocrinol Metab. 2009;94(11):4284–91.
Guerin A, Nisenbaum R, Ray JG. Use of maternal GHb concentration to estimate the risk of congenital anomalies in the offspring of women with prepregnancy diabetes. Diabetes Care. 2007;30(7):1920–5.
Bell R, Glinianaia S, Tennant PWG, Bilous R, Rankin J. Peri-conception hyperglycaemia and nephropathy are associated with risk of congenital anomaly in women with pre-existing diabetes: a population-based cohort study. Diabetologia. 2012;55(4):936–947. This study reports useful data for clinicians to accurately give advice about risk of anomaly to women with pre-existing diabetes.
Hughes RC, Moore MP, Gullam JE, et al. An early pregnancy HbA1c >/=5.9% (41 mmol/mol) is optimal for detecting diabetes and identifies women at increased risk of adverse pregnancy outcomes. Diabetes Care. 2014;37(11):2953–9. This study defines a useful pregnancy HbA1c threshold to identify women with pre-existing but undiagnosed diabetes. It also shows that this HbA1c threshold is a marker for adverse pregnancy outcomes such as congenital anomalies, preterm delivery, pre-eclampsia, shoulder dystocia and possibly peri-natal death.
Glinianaia SV, Tennant PW, Bilous RW, et al. HbA(1c) and birthweight in women with pre-conception type 1 and type 2 diabetes: a population-based cohort study. Diabetologia. 2012;55(12):3193–203. This study shows the influence of hyperglycaemia on fetal growth and important interactions between early and later HbA1c measures.
Vambergue A, Fajardy I. Consequences of gestational and pregestational diabetes on placental function and birth weight. World J Diabetes. 2011;2(11):196–203.
Holmes VA, Young IS, Patterson CC, et al. Optimal glycemic control, pre-eclampsia, and gestational hypertension in women with type 1 diabetes in the diabetes and pre-eclampsia intervention trial. Diabetes Care. 2011;34(8):1683–8.
Damm P, Mersebach H, Rastam J, et al. Poor pregnancy outcome in women with type 1 diabetes is predicted by elevated HbA1c and spikes of high glucose values in the third trimester. J Matern Fetal Neonatal Med. 2014;27(2):149–54.
Evers IM, de Valk HW, Mol BW, et al. Macrosomia despite good glycaemic control in type I diabetic pregnancy; results of a nationwide study in The Netherlands. Diabetologia. 2002;45(11):1484–9.
Kerssen A, de Valk HW, Visser GH. Increased second trimester maternal glucose levels are related to extremely large-for-gestational-age infants in women with type 1 diabetes. Diabetes Care. 2007;30(5):1069–74.
Penney GC, Mair G, Pearson DW. The relationship between birth weight and maternal glycated haemoglobin (HbA1c) concentration in pregnancies complicated by type 1 diabetes. Diabet Med. 2003;20(2):162–6.
Maresh MJ, Holmes VA, Patterson CC, et al. Glycemic targets in the second and third trimester of pregnancy for women with type 1 diabetes. Diabetes Care. 2015;38(1):34–42. Useful data to recommend that HbA1c <42 mmol/mol (6.0%) through pregnancy should be the target in women with pre-existing diabetes.
Capula C, Mazza T, Vero R, et al. HbA1c levels in patients with gestational diabetes mellitus: relationship with pre-pregnancy BMI and pregnancy outcome. J Endocrinol Investig. 2013;36(11):1038–45.
Barnes RA, Edghill N, Mackenzie J, et al. Predictors of large and small for gestational age birthweight in offspring of women with gestational diabetes mellitus. Diabet Med. 2013;30(9):1040–6.
Rowan JA, Gao W, Hague WM, et al. Glycemia and its relationship to outcomes in the metformin in gestational diabetes trial. Diabetes Care. 2010;33(1):9–16.
Katon J, Reiber G, Williams MA, et al. Antenatal haemoglobin A1c and risk of large-for-gestational-age infants in a multi-ethnic cohort of women with gestational diabetes. Paediatr Perinat Epidemiol. 2012;26(3):208–17.
Barrett H, Nitert MD, McIntyre HD, et al. Predictors of preeclampsia in women in the Metformin in Gestational Diabetes (Mig) Study. J Diabetes Metab. 2014;5(7):395.
Crowther C, Hiller J, Moss J, et al. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005;352:2477–86.
Landon MB, Spong CY, Thom E, et al. A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med. 2009;361(14):1339–48.
Karcaaltincaba D, Yalvac S, Kandemir O, et al. Glycosylated hemoglobin level in the second trimester predicts birth weight and amniotic fluid volume in non-diabetic pregnancies with abnormal screening test. J Matern Fetal Neonatal Med. 2010;23(10):1193–9.
Nayak AU, Duff CJ, Indusekhar R, et al. Adverse foetal outcomes in women at risk of gestational diabetes with normal OGTT: exploring the role of HbA1c in risk prediction. In: 50th Annual Meeting of the European Association for the Study of Diabetes, EASD 2014: 15-19th Sept 2014; Vienna. Diabetologia. 2014;57(Suppl 1): S447, Abstract 1088.
Ensenauer R, Gmach J, Nehring I, et al. Increased hemoglobin A(1c) in obese pregnant women after exclusion of gestational diabetes. Clin Chem. 2012;58(7):1152–4.
Alunni ML, Roeder HA, Moore TR, et al. First trimester gestational diabetes screening—change in incidence and pharmacotherapy need. Diabetes Res Clin Pract. 2015;109(1):135–40. A retrospective report of first trimester diabetes screening with HbA1c and FPG in a large cohort of women in California.
McGrath NM, Baker C, Simkins A. Increased detection of gestational diabetes mellitus by using HbA screening in the first antenatal blood tests. Diabet Med. 2014;31(10):1277.
Rowan JA, Budden A, Sadler LC. Women with a nondiagnostic 75 g glucose tolerance test but elevated HbA1c in pregnancy: an additional group of women with gestational diabetes. Aust N Z J Obstet Gynaecol. 2014;54(2):177–80. A small study, but it demonstrates that an HbA1c threshold ≥41mmol/mol (5.9%) identifies women with hyperglycaemia in pregnancy and therefore may be considered as an adjunct test for GDM in women with a non-diagnostic OGTT, but where there is high clinical suspicion (eg obese woman with macrosomic fetus).
Rowan JA, Budden A, Ivanova V, et al. Women with an HbA of 41-49 mmol/mol (5.9-6.6%): a higher risk subgroup that may benefit from early pregnancy intervention. Diabet Med. 2015;33(1):25–31.
Osmundson S, Norton M, El-Sayed Y, et al. Early treatment of women with prediabetes in pregnancy: a randomized controlled trial. In: 35th Annual Meeting of the Society for Maternal-Fetal Medicine: The Pregnancy Meeting.: 02-07 Feb 2015; San Diego. Am J Obstet Gynecol. 2015;212(1): S23-S24, abstract 35.
Lowe LP, Metzger BE, Dyer AR, et al. Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study: associations of maternal A1C and glucose with pregnancy outcomes. Diabetes Care. 2012;35(3):574–80.
Fong A, Serra AE, Gabby L, et al. Use of hemoglobin A1c as an early predictor of gestational diabetes mellitus. Am J Obstet Gynecol. 2014;211(6):641 e1–e7.
Balaji V, Madhuri BS, Ashalatha S, et al. A1C in gestational diabetes mellitus in Asian Indian women. Diabetes Care. 2007;30(7):1865–7.
Anaka O, Houlihan C, Beim R, et al. Does first-trimester hemoglobin A1C predict gestational diabetes and fetal outcome? In: 62nd Annual Clinical Meeting of the American College of Obstetricians and Gynecologists: 26-30th April 2014; Chicago. Obstet Gynecol. 2014;123 (Suppl 1): 38S-39S.
Willems D, Moreno YBL, Barglazan D, et al. HbA1c and screening of gestational diabetes. In: EuroMedLab: 21-25th June 2015; Paris. Clin Chem Lab Med. 2015;53(Special Suppl): S664, Abstract T065.
Berggren E, Boggess K, Mathew L, et al. First trimester HbA1c, at clinically normal values, may be an early predictor of third trimester gestational diabetes. In: 35th Annual Meeting of the Society for Maternal-Fetal Medicine: The Pregnancy Meeting.: 02-07 Feb 2015; San Diego. Am J Obstet Gynecol. 2015;212(1): S168-S169, Abstract 312.
Sevket O, Sevket A, Ozel A, et al. The use of HbA1c as an aid in the diagnosis of gestational diabetes mellitus. J Obstet Gynaecol Br Commonw. 2014;34(8):690–2.
Rajput R, Yogesh Y, Rajput M, et al. Utility of HbA1c for diagnosis of gestational diabetes mellitus. Diabetes Res Clin Pract. 2012;98(1):104–7.
Sugiyama T, Saito M, Nishigori H, et al. Comparison of pregnancy outcomes between women with gestational diabetes and overt diabetes first diagnosed in pregnancy: a retrospective multi-institutional study in Japan. Diabetes Res Clin Pract. 2014;103(1):20–5.
Agarwal M, Dhatt G, Punnose J, et al. Gestational diabetes: a reappraisal of HbA1c as a screening test. Acta Obstet Gynecol Scand. 2005;84(12):1159–63.
Bellamy L, Casas JP, Hingorani AD, et al. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373(9677):1773–9.
Keely E. An opportunity not to be missed—how do we improve postpartum screening rates for women with gestational diabetes? Diabetes Metab Res Rev. 2012;28(4):312–6.
Benaiges D, Chillaron JJ, Pedro-Botet J, et al. Role of A1c in the postpartum screening of women with gestational diabetes. Gynecol Endocrinol. 2013;29(7):687–90.
Picon MJ, Murri M, Munoz A, et al. Hemoglobin A1c versus oral glucose tolerance test in postpartum diabetes screening. Diabetes Care. 2012;35(8):1648–53.
Shah BR, Lipscombe LL, Feig DS, et al. Missed opportunities for type 2 diabetes testing following gestational diabetes: a population-based cohort study. Br J Obstet Gynaecol. 2011;118(12):1484–90.
McGrath NM, Coats A, Barach O. Improved post-partum follow-up of patients with gestational diabetes mellitus using HbA1c. Diabet Med. 2013;30(10):1264–5.
Megia A, Naf S, Herranz L, et al. The usefulness of HbA1c in postpartum reclassification of gestational diabetes. Br J Obstet Gynaecol. 2012;119(7):891–4.
Kim C, Herman WH, Cheung NW, et al. Comparison of hemoglobin A1c with fasting plasma glucose and 2-h postchallenge glucose for risk stratification among women with recent gestational diabetes mellitus. Diabetes Care. 2011;34(9):1949–51.
Su X, Zhang Z, Qu X, et al. Hemoglobin A1c for diagnosis of postpartum abnormal glucose tolerance among women with gestational diabetes mellitus: diagnostic meta-analysis. PLoS One. 2014;9(7):e102144.
Noctor E, Crowe C, Carmody LA, et al. ATLANTIC DIP: simplifying the follow-up of women with previous gestational diabetes. Eur J Endocrinol. 2013;169(5):681–7.
Gobl CS, Bozkurt L, Yarragudi R, et al. Is early postpartum HbA1c an appropriate risk predictor after pregnancy with gestational diabetes mellitus? Acta Diabetol. 2014;51(5):715–722. This paper includes an excellent discussion on the usefulness of postpartum HbA1c analysis, suggesting that serial measures of HbA1c are more useful than a single postnatal test.
Claesson R, Ekelund M, Ignell C, et al. Role of HbA1c in post-partum screening of women with gestational diabetes mellitus. J Clin Translational Endocrinol. 2015;2(1):21–5.
Gingras V, Tchernof A, Weisnagel SJ, et al. Use of glycated hemoglobin and waist circumference for diabetic screening in women with a history of gestational diabetes. J Obstet Gynaecol Can. 2013;35(9):810–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ruth C. E. Hughes, Janet Rowan, and Chris M. Florkowski declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article references studies with human subjects performed by Dr. Ruth Hughes and Dr. Janet Rowan. Informed consent was obtained.
Additional information
This article is part of the Topical Collection on Diabetes and Pregnancy
Rights and permissions
About this article
Cite this article
Hughes, R.C.E., Rowan, J. & Florkowski, C.M. Is There a Role for HbA1c in Pregnancy?. Curr Diab Rep 16, 5 (2016). https://doi.org/10.1007/s11892-015-0698-y
Published:
DOI: https://doi.org/10.1007/s11892-015-0698-y