Abstract
Only 21 % of adolescents with type 1 diabetes (T1D) meet glycemic goals set forth by the American Diabetes Association. Adherence to therapy is a particular concern in this population, and the association between poor adherence and worsening glycemic control indicates that there is a critical need to improve adherence to therapy in adolescents with T1D. In this article, we review barriers to adherence in adolescents with T1D and discuss interventions aimed at improving adherence to therapy and glycemic control. Interventions include technology-based applications, family-based therapies, motivational interviewing, and others. Notably, less than 10 % of the interventions reviewed are provider-led, clinic-based interventions, and few have focused on regimen-related aspects of adherence. This article also outlines the importance of provider communication and the role of providers in facilitating adherence behaviors in adolescents with T1D. Finally, we suggest future directions of research to improve adherence to therapy in adolescents with T1D.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Only 21 % of adolescents with type 1 diabetes (T1D) meet American Diabetes Association guidelines for target hemoglobin A1c (a surrogate for disease control) [1••, 2]. As glycemic control is typically at its worst in adolescence, this window is a critical opportunity to improve control and minimize the multiorgan complications (e.g., kidney disease, eye disease, cardiovascular disease, and neuropathy) associated with chronic hyperglycemia [1••, 3]. Adolescence is a period of marked change, including the hormonal and psychosocial changes associated with puberty and emerging young adulthood. While the hormonal changes of adolescence can lead to insulin resistance, there are several other factors (psychosocial, regimen-related, and communication-related) that drive poor glycemic control seen in adolescents. Understanding and targeting the reasons behind the poor control seen in adolescence are requisite steps to improve glycemic control in this population.
The association between glycemic control and adherence to therapy suggests that to improve glycemic control, adherence to therapy must be improved (as adherence increases, A1c decreases, effect size −0.28 with 95 % confidence interval (CI) −0.24 to −0.32) [4]. Adherence can be loosely defined as “the degree to which patients follow the recommendations of their health professionals” [5]. In T1D, these recommendations include checking and logging blood sugars four to six times per day, counting carbohydrates, giving meal, snack, and long-acting insulin, monitoring blood sugar trends, adjusting insulin therapy as needed, attending routine clinic visits, and communicating with providers as necessary between visits [2]. While these specific tasks may change as diabetes technology advances, data suggest that adherence to therapy continues to be a problem even with advanced technologies. For example, research shows that youths with T1D rarely use continuous glucose monitoring (CGM), a technology associated with improved glycemic control and reduction of hypoglycemia when worn regularly [6]. These findings demonstrate that even as diabetes therapies change, poor adherence remains an important problem.
Measuring adherence to therapy in T1D is difficult because adherence is defined by the several recommendations outlined above and individuals may exhibit varying levels of adherence to the different recommendations; fortunately, studies have shown that blood glucose monitoring frequency (BGMF) may be one of the best markers of adherence to therapy [7••]. While other measures of adherence rely primarily on self-report, BGMF provides an objective way to monitor adherence to therapy. Additionally, BGMF has a strong association with change in glycemic control (even when controlling for covariates such as age, ethnicity, gender, and insulin delivery method) [7••, 8]. As would be expected given the poor glycemic control seen in adolescence, data also show that adherence to therapy (measured with BGMF) worsens during adolescence [7••]. This finding reinforces the concept that to improve glycemic control in this age group, adherence to therapy must be improved.
In this article, we review barriers to adherence in adolescents with T1D, discuss interventions to improve adherence behaviors, outline the role of providers in improving adherence, and finally suggest future areas of research to improve adherence to therapy.
Barriers to Adherence in Adolescents with T1D
Many of the barriers to and facilitators of treatment adherence in pediatric diabetes are psychosocial in nature. Family functioning is a well-established factor contributing to adherence in youth with T1D. Parent-child relationships characterized by warmth and support for diabetes management are associated with better adherence to treatment [9–12]. While there is a natural shift in responsibility for diabetes management as children enter adolescence, declines in parental oversight have been associated with worsening adherence [13]. Parental monitoring in particular has emerged as a strong predictor of adolescents’ adherence to their recommended diabetes treatment regimen [9, 10, 14–16]. More recently, studies have examined the influence of fathers on adherence in pediatric diabetes, finding that fathers’ helpfulness and amount of involvement are related to better treatment adherence and quality of life in children [17]. However, the perceptions of involvement are important; parental involvement has been related to better adjustment and adherence when the adolescent enjoyed and needed it [10], whereas involvement that is perceived as intrusive, rather than collaborative, is associated with lower adherence and suboptimal glycemic control [18–20].
Less attention has been given to the role of peers in adherence to diabetes care. For example, one study found that family provided more support for diabetes care, but peers provided more emotional support for diabetes [21]. A more recent review on peer influences in adolescents with diabetes concluded that there is no strong evidence for peer support on adherence in this population [22]. Another study followed adolescents during their transition from high school to college and found that peer support and peer conflict were not significantly associated with glycemic control; however, there were some limitations in patient follow-up during the study [23]. The role of peers during the transition into adulthood and their effect on adherence are still unclear; therefore, additional investigation into their role in this transition period is warranted.
Additional psychosocial barriers to adherence include a high prevalence of mood, anxiety, and eating disorders in adolescents with T1D. While adolescence is a high risk period for depression and other mood disorders in the general population, a recent study examined adolescents 10 years after diagnosis with T1D and found much higher rates of psychiatric morbidity than what was reported in the community [24, 25]. A post hoc analysis also found higher rates of DSM-IV diagnoses in those with poor glycemic control compared to those with good control [25]. Similarly, symptoms of depression, anxiety, and other mood disorders (without formal diagnoses of depression and anxiety) also increase the risk of poor adherence to therapy [26, 27]. Further, eating disorders and disordered eating behavior have been reported at significantly higher rates in adolescents with T1D as compared to the general population, and these have a negative impact on adherence through omission of insulin for weight loss [28]. Eating disorders and disordered eating behavior are seen at higher rates in females with T1D (as compared to males with T1D); however, there is evidence that these behaviors are becoming more common in males with T1D implying that this may be a barrier to adherence in both males and females with T1D [28].
Barriers to care such as problems communicating with providers and cost of care also pose challenges to adherence to therapy. Using the SEARCH cohort of youth with T1D, Valenzuela et al. found that 48 % of families with children with T1D reported that “getting information” was a barrier to care, 43 % reported that communication with health care providers was a barrier, and 48 % reported that cost of care was a barrier [29••]. Communication with health care providers referred to providers listening to patients, spending enough time with patients, and explaining concepts appropriately. Getting information referred to providers discussing questions/concerns and answering patient questions. Nearly half of families with T1D felt that they were unable to effectively communicate with their providers or did not receive the information that they needed, making this a significant barrier to adherence to therapy [29••].
Finally, regimen-associated barriers to adherence also challenge families/adolescent patients. Burdick et al. showed that 65 % of insulin pump-wearing patients miss one or more meal doses of insulin per week and that two missed meal doses of insulin per week increase A1c 0.5 %, a clinically significant amount [30]. The most common reason for not giving a meal bolus of insulin was forgetting to give the insulin, but additional details of this alarming statistic are not known [30]. Specifically, are meals and snacks at certain times of day more easily forgotten, and are blood glucose checks at certain times of day more challenging to remember or act upon? For example, a study using ecological momentary assessment to measure BGM and insulin administration found that morning time was associated with worse adherence [31]. Assessing and intervening on these regimen-associated barriers are important future areas of investigation (see “Future Directions” section below).
Clearly, multiple barriers to adherence in adolescents with T1D exist, including psychosocial, communication, cost, and regimen-associated barriers. To improve adherence in adolescents with T1D, interventions need to target these barriers with the goal of minimizing barriers and improving adherence behaviors.
Interventions to Improve Adherence to Therapy in Youth with T1D
It is not surprising that several interventions have targeted adherence to therapy in pediatric patients with the goal of improving glycemic control given the association between adherence to therapy and glycemic control. Hood et al. conducted a meta-analysis of adherence promoting interventions in pediatric patients with T1D using intervention studies from 1994 to 2009. The analysis examined the ability of the interventions to improve glycemic control (difference in effect size in intervention and control groups when comparing glycemic control before and after the interventions) [32]. This study demonstrated essentially no improvement comparing pre- versus post-intervention in the intervention versus control group (effect size of 0.11 95 % CI −0.01–0.23) [32]. These interventions varied in their approach and included individual and family-based interventions, utilized behavioral family system therapy, problem-solving, coping skills, diabetes video games, blood glucose downloads, telephone case management, and educational interventions. Interestingly, the authors found that interventions that were multicomponent in nature that targeted more than direct behavioral processes had a larger effect (their example was a coping skill intervention by Grey and colleagues that may have improved general coping skills, in addition to diabetes coping skills, with an effect size of 0.49 [33]). No comparisons were made examining gender or other demographic variables with respect to effect size. The small effect of these interventions is concerning in that, as a whole, multiple different types of adherence promoting interventions had very little effect on glycemic control.
One intervention that has recently been gaining more attention is motivational interviewing (MI). In MI the interviewer and patient engage in a collaborative conversation, empowering and motivating the patient to make goals to change behavior [34]. A meta-analysis examining the effects of MI in pediatric chronic care conditions found that across several different chronic diseases, the overall effect size of MI interventions on pediatric health behavior change was small/moderate g = 0.282 (95 % CI 0.242–0.323) [35•]. Interestingly, of the studies analyzed, the largest effect size was found in T1D (g = 0.914). However, of the four T1D studies two had a negative or non-significant effect size, and two had very large effect sizes, suggesting that these results should be interpreted cautiously [35•]. Additionally, an MI intervention targeting providers (see “The Role of Providers” section below) was not effective in improving glycemic control, suggesting that either the intervention itself (web-based modules, and day long training sessions focusing on certain aspects of MI) or the method of implementation may have a limited impact on glycemic control [36]. Powell and colleagues recently published an article reviewing MI in pediatric T1D [37]. They concluded that to be successful, MI needs to be taught and delivered in a uniform way and that MI interventions should focus on components of diabetes care rather than diabetes outcomes alone. While pediatric MI studies have had mixed results thus far, this intervention may hold promise when applied more uniformly and when targeting adherence behaviors, as Powell and colleagues suggest.
Ongoing pilot studies trialing adherence-promoting interventions may offer promising new directions. One study evaluates the effect of positive affect on adherence in T1D—specifically, whether inducing positive affect amongst adolescents increases their motivation to complete diabetes-related tasks. The pilot study found an association between adolescents’ level of positive affect and adherence (measured through the Self-Care inventory, self-reported glucose monitoring, and meter downloads) [38]. High retention in the study suggests that families are engaged by the positive psychology approach, and further/follow-up studies are indicated.
Another pilot study employed a cognitive-behavioral intervention for adolescents to reduce worry/distress that occurred with completing diabetes adherence behaviors around friends. This study was not powered to achieve statistical significance, and no change was seen between levels of worry and distress pre, post, and 1 month after the intervention [39]. However, this study demonstrates another original strategy to improve adherence behaviors in adolescents with T1D. It is difficult to know whether employing this strategy in a larger sample size would demonstrate an improvement in adolescent worry and distress or whether it would improve worry/distress in certain populations of adolescents, thereby improving adherence.
A less-studied component of adherence is the relation between adherence and health care utilization and costs. A 2003 study investigated the effect of Care Ambassadors (CA), non-medically trained research staff that monitored appointments and helped schedule/reschedule appointments, on glycemic control, significant hypoglycemia, and ER visits/hospitalization [40]. The authors found that those in the CA and the CA+ group (which involved a CA plus a psychoeducational intervention) had significantly improved clinic visit attendance compared to those receiving the standard of care (no CA or psychoeducational intervention) (P < 0.001). Additionally, in the CA+ group, there was a decrease in ED visits and rate of hospitalization, an increased likelihood of improving glycemic control amongst “high-risk patients,” and decreased hypoglycemia [40].
Limitations of this study include a homogeneous patient population and no true cost outcome measurement, making it difficult to determine whether a full-time CA who can monitor clinic attendance and perform the psychoeducational intervention is really a cost-saving resource. A follow-up study involving CA failed to show improvement in glycemic control when comparing the intervention groups to the standard of care group [41]. While CA may help facilitate appointments and reduce hypoglycemia and ER visits, their effect on glycemic control is unclear.
Other innovative approaches to improving adherence behaviors in adolescents with T1D include use of technology, specifically cell phones. Eighty-eight percent of American teens aged 13–17 have access to cell phones, and 90 % of teen cell phone users text message [42]. Additionally, research from the Pew Research Center shows that while there are some racial disparities in cell phone ownership, the majority of teens (including White, non-Hispanic black, and Hispanic teens) own cell phones and use text messaging, allowing cell phone/text messaging interventions to reach a broad patient population [42, 43]. Additionally, a report published in April of 2015 found that a majority of adult smart phone users (62 %) used their smart phone to access health-related information in the past year [44]. However, recent text messaging interventions targeting youth with T1D have had mixed results. A pilot study that used text messages to encourage and remind youth about diabetes-related tasks reported stable glycemic control in their intervention group (compared to worsening control in the non-text messaging historical control group) [45]. Another pilot study developed a text message-based system to remind participants to check blood sugars (with email reminders sent to a control group) with notably decreased participation in both the intervention and control groups after the initial month of the study and no change in glycemic control (although no change was expected given small sample size in this pilot study) [46]. While using text messaging to communicate with patients is certainly a new and exciting area, there is doubt about the long-term efficacy of text messaging interventions, given the above data and concerns regarding changing technologies, cell phone use during the summer vs. school year, cell phone use during school hours, caregiver and peer involvement, and lack of novelty over time [47•]. It is likely that text-messaging interventions will be most effective when they incorporate other approaches (e.g., positive psychology, coping skills training).
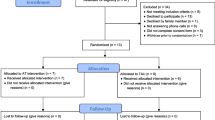
While these are promising new areas of adherence research, it is important to consider not only the effect of the actual interventions studied, but also who provided the intervention in question. Figure 1 depicts the interventions discussed in this section (in addition to other recent interventions) separated by the group that delivered the intervention [33, 36, 38–41, 45, 46, 48–71]. The majority of the interventions are automated (e.g., text message-based intervention) or are provided by research staff, nurses, PhD-trained psychologists, or therapists. While some clinics are very fortunate to have these types of resources, other smaller or more rural clinics would not benefit from these interventions without recruiting additional personnel or further adapting already strained resources. For example, a recent study that surveyed pediatric endocrinologists around the world found that only 40 % of centers studied had a psychologist as a member of the diabetes treatment team [72•]. It is therefore necessary to consider the feasibility of these interventions and consider developing interventions that may be able to target a larger patient population (see “The Role of Providers” and “Future Directions” sections).
Intervention studies (n = 32) in youth with diabetes that have components to improve adherence in the intervention- and/or adherence-based outcome measures, separated by who delivered the intervention. A minority of recent intervention studies with adherence-based components in adolescents with diabetes are performed by providers. A automated [45, 46, 48–53]; R research staff [38, 40, 41, 54–57]; N nurse, diabetes educator, social worker, and dietician [58–65]; P PhD-trained psychologist, graduate student therapist, and therapist [39, 56, 57, 60, 61, 63, 65–67]; PR provider (nurse practitioner or physician) [33, 36, 51, 64]; U unable to determine who provided the intervention [68–71]
The Role of Providers
One area that has been less studied in the adherence field is the role of providers (physicians, nurse practitioners, and physicians assistants), and how providers can impact adherence and, therefore, glycemic control. Of note, other types of providers such as nurses/certified diabetes educators play a large role in providing diabetes care. However, the American Diabetes Association recommends quarterly provider (physician, nurse practitioner, physician assistant) visits for those with poor glycemic control (and at least twice yearly in those meeting glycemic targets) [2]. Given this frequency of visits, interventions that utilize these providers may be an effective way to improve adherence amongst adolescents with T1D.
Notably, less than 10 % of the recent interventions reviewed in this paper aimed at improving adherence or that used adherence as an outcome measure (or with components to improve adherence in the intervention) had a routine clinic visit-based provider component (see Fig. 1). Two of the four studies reviewed in this paper that did utilize providers (1) had a nurse practitioner deliver a behavioral intervention outside of routine office visits (which may not be possible in a busy practice) or (2) asked the nurse practitioner to review blood sugars (part of a telemedicine intervention) [33, 51]. The remaining two studies integrated their intervention into outpatient care delivered by different members of the health care team (including providers) [36, 64]. One of these studies employed guided self-determination (life skills) to improve glycemic control, with no significant improvements in adherence or glycemic control in the intervention versus control groups [64]. The other study (the DEPICTED study) utilized an MI-based intervention to improve glycemic control. There was no difference between the intervention and standard of care arms at 1 year (end of study) in hemoglobin A1c (primary outcome) when compared to baseline nor was there a difference in adherence as measured by the quality of life inventory [36]. It is possible that this type of intervention did not work because of the difficulties in teaching providers MI, in consistently employing the intervention over the year of the study or that this intervention does not work uniformly in all patients with T1D. This study illustrates a type of provider-based intervention that may not be effective in improving patient adherence. It is important that only 4 of the 32 studies reviewed in this paper utilized providers in their intervention, and only 2 of those were targeting clinic visits. Clearly, very few studies in youth with diabetes have investigated what providers can do to impact adherence behaviors during routine office visits.
Provider communication may be an important target for adherence-promoting interventions amongst adolescents with T1D. A 2009 meta-analysis by Zolnierek examining (1) physician communication and its effect on patient adherence and (2) whether communication training amongst physicians improves patient adherence showed the importance of physicians/providers and their effect on patient adherence [5]. Specifically, this study found that the odds of a patient adhering to therapy were much higher when the physician was a “good communicator” (odds ratio 2.16, 95 % CI 1.91–2.35). Interestingly, this relationship was even stronger when the provider was a pediatrician (pediatrician r = 0.25 vs. non-pediatrician r = 0.18). The authors suggest that this may be because unlike adult providers, pediatricians must communicate with both parents and patients and therefore must communicate effectively with two different groups who may require varying levels of detail and explanation. Finally, this meta-analysis also found that the odds of a patient adhering to therapy were higher (1.62) if the physician had received specific training in communication skills [5]. Clearly, patient adherence is closely tied and positively associated with provider communication; therefore, focusing on provider communication specifically within the field of T1D will be very important, as these data suggest that providers have the ability to influence and improve patient adherence to medical therapy.
It is important to note that Zolnierek’s meta-analysis was not specific to diabetes patients and the heterogeneity amongst the studies may make it difficult to broadly apply findings to specific patient populations. However, the overall finding that physician communication is associated with improved patient adherence is very important and warrants investigation in pediatric diabetes patients. This finding is also in line with the recent study by Valenzuela and colleagues, which demonstrated that amongst the SEARCH cohort of youth with T1D, a prominent barrier to care reported by patients and their families was provider communication (43 % of patients/families) [29••]. Taken together, these studies suggest that there is significant room for improvement in provider-patient communication and that improving communication may promote patient adherence. Interestingly, the concept that providers must be able to understand and effectively communicate with their patients may also be gaining national attention. The Association of American Medical Colleges (AAMC) is changing the Medical College Admission Test (which is required for admission to medical school) to include a section on social and behavioral sciences [73]. The AAMC hopes that this will help inform future physicians on social and health care issues that will prepare them to become better physicians. Changing the way providers are trained, and requiring that providers understand the social- and health-related issues of their patients, is an important and necessary step toward improving provider communication and ultimately adherence.
Notably, the need for provider-based interventions, specifically those improving provider communication, is gaining attention within some pediatric settings. In some institutions, providers receive ongoing communication training to facilitate their ability to assist families in their management of chronic disease [74]. While this communication training is not specific to diabetes providers, the approach to improving provider communication has potential to benefit patients with diabetes. Linking these interventions to outcomes in adherence will also be of particular importance.
Thus far, relatively few provider-based interventions aimed at improving adolescent adherence to therapy have been trialed. However, evidence suggests that providers, especially pediatric providers, may be uniquely positioned to improve adherence to therapy in their patients with T1D, making this an important new avenue for research.
Future Directions
Improving glycemic control in adolescents with T1D starts with improving adherence to therapy. Unfortunately, interventions thus far have had very modest effects on glycemic control. The effect of these interventions on adherence is difficult to determine, as studies use different measures to assess adherence, and this range of measures makes it challenging to compare adherence across studies. A minority of studies examined frequency of blood glucose monitoring (an excellent proxy for adherence), and some of these studies relied on patient report of BGMF rather than meter download (which can be unreliable) [7••, 75]. Additionally, it can be challenging to assess which interventions are truly aimed at improving adherence to therapy, as different studies use different terminology for adherence (adherence, compliance, self-management, and self-efficacy are all used synonymously). Moving forward research aimed at improving adherence to therapy should use similar terminology and measures of adherence (BGMF) to allow for clear understanding of the effect of the intervention in question.
Several of the interventions reviewed in this article require resources that may not be available to all patients. Therefore, focus should be given to provider-based interventions to allow providers to influence adherence behaviors in their patients. In addition to improving provider communication, there may be other methods for providers to impact their patients’ adherence to therapy. In a 2001 study, for example, adolescents completed a computerized assessment of health behaviors (focusing on activity and nutrition) prior to office clinic visits and set goals for behavioral change based on problem areas identified in the assessment [76]. Providers were then able to counsel on the health assessment and goals created during routine clinic visits. The study demonstrated that areas targeted by adolescents improved at subsequent clinic visits [76]. Although this study did not involve patients with T1D, time-saving strategies such as this may allow providers to quickly and effectively assess and target barriers to adherence in adolescents with T1D.
Another future direction involves investigating specific regimen-associated barriers to adherence, defined as barriers directly related to adhering to the prescribed diabetes regimen of blood glucose monitoring and administration of meal, snack, and basal insulin (see Table 1). Also, included in this table is provider communication, as patients must be able to effectively communicate with their providers to understand and follow their diabetes regimens. Learning how patients understand and follow provider recommendations, and focusing on the specific barriers that they face, may allow providers to intervene and improve specific aspects of diabetes care during routine quarterly clinic visits. In this way, providers may be able to improve the adherence and, therefore, glycemic control of adolescents with T1D.
An important consideration regarding provider-directed interventions is the pressure that providers are under to see more and more patients. Given limited provider time (15–30 min per patient) and busy pediatric practices, provider-directed interventions will need to demonstrate not only improved patient adherence to therapy and glycemic control but also decreased health care costs. Specifically, examining provider interventions as a function of ED visits and rates of hospitalization to show decreased health care costs both in the short and long term will be a necessary part of this research.
Conclusions
Adherence to therapy in adolescents with T1D is a challenging problem necessitating a multifaceted approach. In addition to the ongoing research in adolescent adherence to therapy in T1D, specific attention needs to be given to the role of providers and their ability to affect change, especially related to regimen-related barriers. As technology becomes more advanced, providers may play an even larger role in promoting adherence. Giving providers the tools to assess and impact their patients’ barriers to adherence holds promise as a strategy that may be universally used by providers to improve adherence and, therefore, glycemic control in youth with T1D.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wood JR, Miller KM, Maahs DM, Beck RW, DiMeglio LA, Libman IM, et al. Most youth with type 1 diabetes in the T1D Exchange Clinic Registry do not meet American Diabetes Association or International Society for Pediatric and Adolescent Diabetes clinical guidelines. Diabetes Care. 2013;36(7):2035–7. doi:10.2337/dc12-1959. This article demonstrates that even before the pediatric glycemic goals of the ADA changed, most youth were not achieving recommended hemoglobin A1c levels.
The American Diabetes Association. Standards of Medical Care in Diabetes-2015. Diabetes Care. 2015;38:S1–93.
The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86. doi:10.1056/nejm199309303291401.
Hood KK, Peterson CM, Rohan JM, Drotar D. Association between adherence and glycemic control in pediatric type 1 diabetes: a meta-analysis. Pediatrics. 2009;124(6):e1171–9. doi:10.1542/peds.2009-0207. PubMed.
Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826–34. doi:10.1097/MLR.0b013e31819a5acc.
Wong JC, Foster NC, Maahs DM, Raghinaru D, Bergenstal RM, Ahmann AJ, et al. Real-time continuous glucose monitoring among participants in the T1D Exchange clinic registry. Diabetes Care. 2014;37(10):2702–9. doi:10.2337/dc14-0303. PubMed.
Rausch JR, Hood KK, Delamater A, Shroff Pendley J, Rohan JM, Reeves G, et al. Changes in treatment adherence and glycemic control during the transition to adolescence in type 1 diabetes. Diabetes Care. 2012;35(6):1219–24. doi:10.2337/dc11-2163. This article finds that blood glucose monitoring frequency can be used as a surrogate for treatment adherence and that declining adherence to therapy leads to worsening glycemic control. Notably, the article also demonstrates that glycemic control should not be used as a surrogate for adherence to therapy.
Helgeson VS, Honcharuk E, Becker D, Escobar O, Siminerio L. A focus on blood glucose monitoring: relation to glycemic control and determinants of frequency. Pediatr Diabetes. 2011;12(1):25–30. doi:10.1111/j.1399-5448.2010.00663.x.
Palmer DL, Osborn P, King PS, Berg CA, Butler J, Butner J, et al. The structure of parental involvement and relations to disease management for youth with type 1 diabetes. J Pediatr Psychol. 2011;36(5):596–605. doi:10.1093/jpepsy/jsq019.
Berg CA, Butler JM, Osborn P, King G, Palmer DL, Butner J, et al. Role of parental monitoring in understanding the benefits of parental acceptance on adolescent adherence and metabolic control of type 1 diabetes. Diabetes Care. 2008;31(4):678–83. doi:10.2337/dc07-1678.
Lloyd SM, Cantell M, Pacaud D, Crawford S, Dewey D. Brief report: hope, perceived maternal empathy, medical regimen adherence, and glycemic control in adolescents with type 1 diabetes. J Pediatr Psychol. 2009;34(9):1025–9. doi:10.1093/jpepsy/jsn141.
Mlynarczyk SM. Adolescents’ perspectives of parental practices influence diabetic adherence and quality of life. Pediatr Nurs. 2013;39(4):181–9.
Ingerski LM, Anderson BJ, Dolan LM, Hood KK. Blood glucose monitoring and glycemic control in adolescence: contribution of diabetes-specific responsibility and family conflict. J Adolesc Health. 2010;47(2):191–7. doi:10.1016/j.jadohealth.2010.01.012.
Berg CA, King PS, Butler JM, Pham P, Palmer D, Wiebe DJ. Parental involvement and adolescents’ diabetes management: the mediating role of self-efficacy and externalizing and internalizing behaviors. J Pediatr Psychol. 2011;36(3):329–39. doi:10.1093/jpepsy/jsq088.
Horton D, Berg CA, Butner J, Wiebe DJ. The role of parental monitoring in metabolic control: effect on adherence and externalizing behaviors during adolescence. J Pediatr Psychol. 2009;34(9):1008–18. doi:10.1093/jpepsy/jsp022.
Hilliard ME, Holmes CS, Chen R, Maher K, Robinson E, Streisand R. Disentangling the roles of parental monitoring and family conflict in adolescents’ management of type 1 diabetes. Health Psychol. 2013;32(4):388–96. doi:10.1037/a0027811.
Wysocki T, Gavin L. Paternal involvement in the management of pediatric chronic diseases: associations with adherence, quality of life, and health status. J Pediatr Psychol. 2006;31(5):501–11. doi:10.1093/jpepsy/jsj042.
Hood KK, Butler DA, Anderson BJ, Laffel LM. Updated and revised diabetes family conflict scale. Diabetes Care. 2007;30(7):1764–9. doi:10.2337/dc06-2358.
Lewin AB, Heidgerken AD, Geffken GR, Williams LB, Storch EA, Gelfand KM, et al. The relation between family factors and metabolic control: the role of diabetes adherence. J Pediatr Psychol. 2006;31(2):174–83. doi:10.1093/jpepsy/jsj004.
Cameron FJ, Skinner TC, de Beaufort CE, Hoey H, Swift PG, Aanstoot H, et al. Are family factors universally related to metabolic outcomes in adolescents with type 1 diabetes? Diabet Med. 2008;25(4):463–8. doi:10.1111/j.1464-5491.2008.02399.x.
La Greca AM, Auslander WF, Greco P, Spetter D, Fisher Jr EB, Santiago JV. I get by with a little help from my family and friends: adolescents’ support for diabetes care. J Pediatr Psychol. 1995;20(4):449–76.
Palladino DK, Helgeson VS. Friends or foes? A review of peer influence on self-care and glycemic control in adolescents with type 1 diabetes. J Pediatr Psychol. 2012;37(5):591–603. doi:10.1093/jpepsy/jss009.
Helgeson VS, Mascatelli K, Reynolds KA, Becker D, Escobar O, Siminerio L. Friendship and romantic relationships among emerging adults with and without type 1 diabetes. J Pediatr Psychol. 2014. doi:10.1093/jpepsy/jsu069.
Saluja G, Iachan R, Scheidt PC, Overpeck MD, Sun W, Giedd JN. Prevalence of and risk factors for depressive symptoms among young adolescents. Arch Pediatr Adolesc Med. 2004;158(8):760–5. doi:10.1001/archpedi.158.8.760.
Northam EA, Matthews LK, Anderson PJ, Cameron FJ, Werther GA. Psychiatric morbidity and health outcome in type 1 diabetes—perspectives from a prospective longitudinal study. Diabet Med. 2005;22(2):152–7. doi:10.1111/j.1464-5491.2004.01370.x.
McGrady ME, Hood KK. Depressive symptoms in adolescents with type 1 diabetes: associations with longitudinal outcomes. Diabetes Res Clin Pract. 2010;88(3):e35–7. doi:10.1016/j.diabres.2010.03.025.
Herzer M, Hood KK. Anxiety symptoms in adolescents with type 1 diabetes: association with blood glucose monitoring and glycemic control. J Pediatr Psychol. 2010;35(4):415–25. doi:10.1093/jpepsy/jsp063.
Hanlan ME, Griffith J, Patel N, Jaser SS. Eating disorders and disordered eating in type 1 diabetes: prevalence, screening, and treatment options. Curr Diab Rep. 2013. doi:10.1007/s11892-013-0418-4.
Valenzuela JM, Seid M, Waitzfelder B, Anderson AM, Beavers DP, Dabelea DM, et al. Prevalence of and disparities in barriers to care experienced by youth with type 1 diabetes. J Pediatr. 2014;164(6):1369–75.e1. doi:10.1016/j.jpeds.2014.01.035. The authors find that there are several barriers to care in youth with diabetes within the US and highlight the most prominent barriers to care.
Burdick J, Chase HP, Slover RH, Knievel K, Scrimgeour L, Maniatis AK, et al. Missed insulin meal boluses and elevated hemoglobin A1c levels in children receiving insulin pump therapy. Pediatrics. 2004;113(3 Pt 1):e221–4.
Mulvaney SA, Rothman RL, Dietrich MS, Wallston KA, Grove E, Elasy TA, et al. Using mobile phones to measure adolescent diabetes adherence. Health Psychol. 2012;31(1):43–50. doi:10.1037/a0025543.
Hood KK, Rohan JM, Peterson CM, Drotar D. Interventions with adherence-promoting components in pediatric type 1 diabetes: meta-analysis of their impact on glycemic control. Diabetes Care. 2010;33(7):1658–64. doi:10.2337/dc09-2268.
Grey M, Boland EA, Davidson M, Li J, Tamborlane WV. Coping skills training for youth with diabetes mellitus has long-lasting effects on metabolic control and quality of life. J Pediatr. 2000;137(1):107–13. doi:10.1067/mpd.2000.106568.
Miller WR, Rollnick S. Motivational interviewing: helping people change. 3rd ed. New York: Guilford Press; 2013.
Gayes LA, Steele RG. A meta-analysis of motivational interviewing interventions for pediatric health behavior change. J Consult Clin Psychol. 2014;82(3):521–35. doi:10.1037/a0035917. This meta-analysis reviews the literature on motivational interviewing (MI) in pediatric medicine and finds that MI might be a helpful way to influence change in this population.
Robling M, McNamara R, Bennert K, Butler CC, Channon S, Cohen D, et al. The effect of the talking diabetes consulting skills intervention on glycaemic control and quality of life in children with type 1 diabetes: cluster randomised controlled trial (DEPICTED study). The effect of the talking diabetes consulting skills intervention on glycaemic control and quality of life in children with type 1 diabetes: cluster randomised controlled trial (DEPICTED study). BMJ. 2012;344:e2359. doi:10.1136/bmj.e2359.
Powell PW, Hilliard ME, Anderson BJ. Motivational interviewing to promote adherence behaviors in pediatric type 1 diabetes. Curr Diab Rep. 2014;14(10):531. doi:10.1007/s11892-014-0531-z.
Jaser SS, Patel N, Rothman RL, Choi L, Whittemore R. Check it! A randomized pilot of a positive psychology intervention to improve adherence in adolescents with type 1 diabetes. Diabetes Educ. 2014;40(5):659–67. doi:10.1177/0145721714535990.
Salamon KS, Hains AA, Fleischman KM, Davies WH, Kichler J. Improving adherence in social situations for adolescents with type 1 diabetes mellitus (T1DM): a pilot study. Prim Care Diabetes. 2010;4(1):47–55. doi:10.1016/j.pcd.2009.10.003.
Svoren BM, Butler D, Levine BS, Anderson BJ, Laffel LM. Reducing acute adverse outcomes in youths with type 1 diabetes: a randomized, controlled trial. Pediatrics. 2003;112(4):914–22.
Katz ML, Volkening LK, Butler DA, Anderson BJ, Laffel LM. Family-based psychoeducation and care ambassador intervention to improve glycemic control in youth with type 1 diabetes: a randomized trial. Pediatr Diabetes. 2014;15(2):142–50. doi:10.1111/pedi.12065.
Lenhart A. Pew Research Center. Teens, social media and technology overview 2015 [cited 2015 May 4th]. Available from: http://www.pewinternet.org/2015/04/09/teens-social-media-technology-2015.
Lenhart A. Pew Research Center. Cell phone ownership 2012 [cited 2015 February 11]. Available from: http://www.pewinternet.org/2012/03/19/cell-phone-ownership/.
Smith A. Pew Research Center. U.S. Smartphone Use in 2015 [cited 2015 May 4th]. Available from: http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/.
Mulvaney SA, Anders S, Smith AK, Pittel EJ, Johnson KB. A pilot test of a tailored mobile and web-based diabetes messaging system for adolescents. J Telemed Telecare. 2012;18(2):115–8. doi:10.1258/jtt.2011.111006.
Hanauer DA, Wentzell K, Laffel N, Laffel LM. Computerized Automated Reminder Diabetes System (CARDS): e-mail and SMS cell phone text messaging reminders to support diabetes management. Diabetes Technol Ther. 2009;11(2):99–106. doi:10.1089/dia.2008.0022.
Herbert L, Owen V, Pascarella L, Streisand R. Text message interventions for children and adolescents with type 1 diabetes: a systematic review. Diabetes Technol Ther. 2013;15(5):362–70. doi:10.1089/dia.2012.0291. This review outlines text messaging interventions that aim to improve glycemic control in pediatric patients with type 1 diabetes. While several interventions have been trialed, their effect on glycemic control is unclear.
Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of sweet talk, a text-messaging system to support young people with diabetes. Diabet Med. 2006;23(12):1332–8. doi:10.1111/j.1464-5491.2006.01989.x.
Brown SJ, Lieberman DA, Germeny BA, Fan YC, Wilson DM, Pasta DJ. Educational video game for juvenile diabetes: results of a controlled trial. Med Inform (Lond). 1997;22(1):77–89.
Kumar VS, Wentzell KJ, Mikkelsen T, Pentland A, Laffel LM. The DAILY (Daily Automated Intensive Log for Youth) trial: a wireless, portable system to improve adherence and glycemic control in youth with diabetes. Diabetes Technol Ther. 2004;6(4):445–53. doi:10.1089/1520915041705893.
Marrero DG, Vandagriff JL, Kronz K, Fineberg NS, Golden MP, Gray D, et al. Using telecommunication technology to manage children with diabetes: the Computer-Linked Outpatient Clinic (CLOC) study. Diabetes Educ. 1995;21(4):313–9.
Raiff BR, Dallery J. Internet-based contingency management to improve adherence with blood glucose testing recommendations for teens with type 1 diabetes. J Appl Behav Anal. 2010;43(3):487–91. doi:10.1901/jaba.2010.43-487.
Cafazzo JA, Casselman M, Hamming N, Katzman DK, Palmert MR. Design of an mHealth app for the self-management of adolescent type 1 diabetes: a pilot study. J Med Internet Res. 2012;14(3):e70. doi:10.2196/jmir.2058.
Anderson BJ, Brackett J, Ho J, Laffel LM. An office-based intervention to maintain parent-adolescent teamwork in diabetes management. Impact on parent involvement, family conflict, and subsequent glycemic control. Diabetes Care. 1999;22(5):713–21.
Laffel LM, Vangsness L, Connell A, Goebel-Fabbri A, Butler D, Anderson BJ. Impact of ambulatory, family-focused teamwork intervention on glycemic control in youth with type 1 diabetes. J Pediatr. 2003;142(4):409–16. doi:10.1067/mpd.2003.138.
Nansel TR, Iannotti RJ, Simons-Morton BG, Cox C, Plotnick LP, Clark LM, et al. Diabetes personal trainer outcomes: short-term and 1-year outcomes of a diabetes personal trainer intervention among youth with type 1 diabetes. Diabetes Care. 2007;30(10):2471–7. doi:10.2337/dc06-2621.
Holmes CS, Chen R, Mackey E, Grey M, Streisand R. Randomized clinical trial of clinic-integrated, low-intensity treatment to prevent deterioration of disease care in adolescents with type 1 diabetes. Diabetes Care. 2014;37(6):1535–43. doi:10.2337/dc13-1053.
Cook S, Herold K, Edidin DV, Briars R. Increasing problem solving in adolescents with type 1 diabetes: the choices diabetes program. Diabetes Educ. 2002;28(1):115–24.
Howe CJ, Jawad AF, Tuttle AK, Moser JT, Preis C, Buzby M, et al. Education and telephone case management for children with type 1 diabetes: a randomized controlled trial. J Pediatr Nurs. 2005;20(2):83–95. doi:10.1016/j.pedn.2004.12.010.
Wysocki T, Harris MA, Greco P, Bubb J, Danda CE, Harvey LM, et al. Randomized, controlled trial of behavior therapy for families of adolescents with insulin-dependent diabetes mellitus. J Pediatr Psychol. 2000;25(1):23–33.
Wysocki T, Harris MA, Buckloh LM, Mertlich D, Lochrie AS, Taylor A, et al. Effects of behavioral family systems therapy for diabetes on adolescents’ family relationships, treatment adherence, and metabolic control. J Pediatr Psychol. 2006;31(9):928–38. doi:10.1093/jpepsy/jsj098.
Wang YC, Stewart SM, Mackenzie M, Nakonezny PA, Edwards D, White PC. A randomized controlled trial comparing motivational interviewing in education to structured diabetes education in teens with type 1 diabetes. Diabetes Care. 2010;33(8):1741–3. doi:10.2337/dc10-0019.
Channon SJ, Huws-Thomas MV, Rollnick S, Hood K, Cannings-John RL, Rogers C, et al. A multicenter randomized controlled trial of motivational interviewing in teenagers with diabetes. Diabetes Care. 2007;30(6):1390–5. doi:10.2337/dc06-2260.
Husted GR, Thorsteinsson B, Esbensen BA, Gluud C, Winkel P, Hommel E, et al. Effect of guided self-determination youth intervention integrated into outpatient visits versus treatment as usual on glycemic control and life skills: a randomized clinical trial in adolescents with type 1 diabetes. Trials. 2014;15:321. doi:10.1186/1745-6215-15-321.
Ellis DA, Naar-King S, Chen X, Moltz K, Cunningham PB, Idalski-Carcone A. Multisystemic therapy compared to telephone support for youth with poorly controlled diabetes: findings from a randomized controlled trial. Ann Behav Med. 2012;44(2):207–15. doi:10.1007/s12160-012-9378-1.
Ellis DA, Frey MA, Naar-King S, Templin T, Cunningham P, Cakan N. Use of multisystemic therapy to improve regimen adherence among adolescents with type 1 diabetes in chronic poor metabolic control: a randomized controlled trial. Diabetes Care. 2005;28(7):1604–10.
Stanger C, Ryan SR, Delhey LM, Thrailkill K, Li Z, Li Z, et al. A multicomponent motivational intervention to improve adherence among adolescents with poorly controlled type 1 diabetes: a pilot study. J Pediatr Psychol. 2013;38(6):629–37. doi:10.1093/jpepsy/jst032.
Matam P, Kumaraiah V, Munichoodappa C, Kumar KM, Aravind S. Behavioural intervention in the management of compliance in young type-I diabetics. J Assoc Physicians India. 2000;48(10):967–71.
McNabb WL, Quinn MT, Murphy DM, Thorp FK, Cook S. Increasing children’s responsibility for diabetes self-care: the in control study. Diabetes Educ. 1994;20(2):121–4.
Viner RM, Christie D, Taylor V, Hey S. Motivational/solution-focused intervention improves HbA1c in adolescents with type 1 diabetes: a pilot study. Diabet Med. 2003;20(9):739–42.
Murphy HR, Wadham C, Hassler-Hurst J, Rayman G, Skinner TC. Randomized trial of a diabetes self-management education and family teamwork intervention in adolescents with type 1 diabetes. Diabet Med. 2012;29(8):e249–54. doi:10.1111/j.1464-5491.2012.03683.x.
de Wit M, Pulgaron ER, Pattino-Fernandez AM, Delamater AM. Psychological support for children with diabetes: are the guidelines being met? J Clin Psychol Med Settings. 2014;21(2):190–9. doi:10.1007/s10880-014-9395-2. This article finds that a large portion of pediatric diabetes treatment teams queried do not have access to a mental health specialist; this is an important finding given the several known psychosocial barriers to treatment adherence in this population.
Mann S. AAMC Approves new MCAT exam with increased focus on social, behavioral sciences 2012 [cited 2015 May 4th]. Available from: https://www.aamc.org/newsroom/reporter/march2012/276588/mcat2015.html.
Drotar D, Rohan J. Pediatric Adherence and Health Behavior Change. In: Martin L, DiMatteo R, editors. The Oxford handbook of health communication, behavior change, and treatment adherence. New York: Oxford University Press; 2014.
Chae M, Reith DM, Tomlinson PA, Rayns J, Wheeler BJ. Accuracy of verbal self-reported blood glucose in teenagers with type I diabetes at diabetes ski camp. J Diabetes Metab Disord. 2014;13(1):14. doi:10.1186/2251-6581-13-14.
Patrick K, Sallis JF, Prochaska JJ, Lydston DD, Calfas KJ, Zabinski MF, et al. A multicomponent program for nutrition and physical activity change in primary care: PACE+ for adolescents. Arch Pediatr Adolesc Med. 2001;155(8):940–6.
Acknowledgments
This work was supported by the generous backing of the Odom Family and by awards from the National Institute of Diabetes and Digestive and Kidney Diseases (K23 NK088454 to SSJ; K08DK90146 to DJM) and JDRF (Career Development Award to DJM). The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official view of the US National Institutes of Health.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Karishma A. Datye, Daniel J. Moore, William E. Russell, and Sarah S. Jaser declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This is a review article and therefore does not contain any unpublished original studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Psychosocial Aspects
Rights and permissions
About this article
Cite this article
Datye, K.A., Moore, D.J., Russell, W.E. et al. A Review of Adolescent Adherence in Type 1 Diabetes and the Untapped Potential of Diabetes Providers to Improve Outcomes. Curr Diab Rep 15, 51 (2015). https://doi.org/10.1007/s11892-015-0621-6
Published:
DOI: https://doi.org/10.1007/s11892-015-0621-6