Abstract
Purpose of Review
To describe medical therapies and mechanical circulatory support devices used in the treatment of acute right ventricular failure.
Recent Findings
Experts have proposed several algorithms providing a stepwise approach to medical optimization of acute right ventricular failure including tailored volume administration, ideal vasopressor selection to support coronary perfusion, inotropes to restore contractility, and pulmonary vasodilators to improve afterload. Studies have investigated various percutaneous and surgically implanted right ventricular assist devices in several clinical settings.
Summary
The initial management of acute right ventricular failure is often guided by invasive hemodynamic data tracking parameters of circulatory function with the use of pharmacologic therapies. Percutaneous microaxial and centrifugal extracorporeal pumps bypass the failing RV and support circulatory function in severe cases of right ventricular failure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Historically, the right ventricle (RV) was viewed as a passive conduit of limited interest to medicine as a result of several classic experiments minimizing its importance [1]. An emergence of interest led to a deeper understanding of RV function, pathophysiology, and to the development of medical therapies and mechanical circulatory support (MCS) devices expanding treatment options for a variety of disorders affecting the RV [2]. However, as robust data are limited in this field, an appreciation of physiology is requisite to select appropriate treatment strategies. Here, we review medical therapies and MCS devices used to support the acutely failing RV.
Pathophysiology of Acute Right Ventricular Failure
The RV is a high-volume, low-pressure pump facing a vascular resistance approximately one tenth that of the LV [3, 4]. Sharing the intraventricular septum, myocardial fibers, and the pericardial space, the function of both ventricles is inextricably linked through multiple mechanisms [5,6,7]. In series interdependence, decline in RV stroke volume (SV) will lead to a corresponding decrease in left ventricular (LV) filling and ejection. With parallel ventricular interdependence, leftward septal shift caused by RV dilatation within a shared pericardial space will further contribute to depressed LV SV.
As the RV is exquisitely sensitive to changes in afterload, an increase in pulmonary vascular tone is a common inciting event leading to hemodynamic collapse [1, 8]. When the RV dilates to maintain SV in the face of increased afterload, the tricuspid annulus is stretched leading to valvular regurgitation and further RV volume overload. RV dilatation promotes leftward septal shift depressing LV filling and SV while driving myocardial ischemia related to the imposed elevation in RV wall tension. The interplay of these mechanisms is a vicious cycle of auto-aggravation ultimately resulting in hypotension, decreased coronary perfusion to the RV, further myocardial ischemia, and death from obstructive shock [1, 9].
Causes of Acute Right Ventricular Failure
While common mechanisms of RV failure in the intensive care unit (ICU) are related to LV dysfunction or an acute or acute on chronic elevation in afterload, primary myocardial pathology and states of volume overload may be encountered. Management requires an understanding of the disease process to correspondingly select therapies. The following are select causes of RV failure grouped by physiology [2, 10, 11]:
-
An increase in afterload may be encountered in acute pulmonary embolism (PE), hypoxemic or hypercapnic respiratory failure, excessive airway pressures or lung volumes with mechanical ventilation, decompensation of chronic pulmonary hypertension, and left heart failure.
-
Primary myocardial dysfunction may occur in isolation (right ventricular myocardial infarction (MI), arrhythmogenic right ventricular cardiomyopathy), or concomitantly with LV failure related to the same pathology (acute myocarditis, overdose of negative inotropic medications). Primary graft dysfunction following cardiac transplant may be attributed to either mechanism.
-
Alterations in preload are encountered in the setting of aggressive volume resuscitation, left-to-right shunts (e.g., atrial septal defect), or with valvular heart disease such as severe tricuspid regurgitation. Right ventricular failure following left ventricular assist device (LVAD) implantation may lead to an increase in venous return overwhelming the RV via similar mechanisms.
Hemodynamic Assessment of Right Ventricular Failure
Multiple formulas derived from invasive hemodynamic measures assist in the assessment of RV dysfunction [10, 12]. Expert consensus statements recommend pulmonary artery catheterization for the diagnosis and monitoring of cardiogenic shock, in cases of worsening organ function, or among those being considered for MCS [12]. Selection of therapies and mechanical support often follows pulmonary artery catheterization in critically ill patients with RV failure. While an exhaustive list is beyond the scope of this review, the right atrial pressure (RAP), ratio of right atrial pressure to pulmonary capillary wedge pressure (RAP/PCWP), pulmonary artery pulsatility index (PAPi), and right ventricular stroke work index (RVSWI) are commonly used indices in clinical practice [10].
An elevated RAP/PCWP ratio describes the relative contribution of RV dysfunction in several clinical settings including RV MI and post-LVAD implantation. Values correlate to echocardiographic and hemodynamic markers of RV dysfunction as well as with adverse clinical outcomes [10, 13]. A ratio > 0.63 was shown to predict RV failure following LVAD implantation while a cutoff of > 0.86 was used as a marker of RV failure in acute MI [10]. The PAPi, defined as (PASP − PADP)/RAP (where PASP is the pulmonary artery systolic pressure, PADP the pulmonary artery diastolic pressure, RAP the right atrial pressure), is an important prognostic hemodynamic index and has been incorporated into cardiogenic shock management algorithms [14]. Simplistically, the PASP is an indicator of RV contractile function against a given afterload while an elevated RAP reflects RV failure and correlates with severity of organ dysfunction [15]. However, physiologic interpretation is more nuanced. While cutoff values vary by clinical scenario, a PAPi < 1.0 has been shown to predict poor clinical outcomes in the setting of acute MI [16].
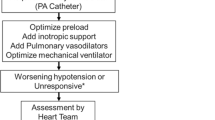
Medical Management of Acute Right Ventricular Failure
Our understanding of RV pathophysiology and therapeutics lags behind that of the LV and is often grounded in experimental models and small studies. Accordingly, a comprehensive understanding of RV physiology is requisite to tailor therapeutic strategies. Manipulation of hemodynamics in the setting of acute RV failure involves optimization of preload, restoration of systemic and coronary perfusion pressure, augmentation of contractility, and reduction in pulmonary vascular resistance (PVR). While treatment should focus on ameliorating the underlying disease process (e.g., revascularization in right ventricular myocardial infarction, reperfusion with pulmonary embolism), here we review general and pharmacologic interventions aimed at improving hemodynamics of the acutely failing RV (Table 1).
Preload Optimization: Fluids and Decongestion
Preload influences myocardial contractility and RV stroke volume according to the Frank-Starling mechanism. Excess volume loading may worsen RV overdistension and therefore cardiac output (CO) through parallel ventricular interdependence, leftward septal shift, and resultant depression of left ventricular end-diastolic volume (LVEDV) and SV [17, 18••]. The common teaching that RV failure is a preload-dependent state best managed with fluid administration is simplistic and often inaccurate [2]. While a central venous pressure (CVP) goal of 8–12 mmHg is frequently advocated in acute RV failure, this target is not well-supported by literature and relies on a static marker of volume responsiveness [18••, 19]. As an elevated CVP represents impedance to venous return, this value may better serve as a “stopping rule” to resuscitation rather than a target.
Acute RV failure is commonly mediated by an increased in PVR; PE serves as a model to illustrate a management approach. Unfortunately, studies on preload modification in acute PE yield conflicting results [17, 20, 21]. Mercat et al. investigated volume loading (500 cc of dextran 40) among 13 patients with acute PE with resultant circulatory failure and an average cardiac index of 1.6 L/min/m2. Fluid administration increased mean cardiac index to 2.0 L/min/m2, a change inversely correlated to baseline right ventricular end-diastolic volume (RVEDV) but independent of baseline CVP [20]. In a porcine model of intermediate-high risk PE, fluid loading improved RV SV, ejection fraction (EF), and CO while diuretic therapy had the opposite effect [17]. By contrast, in a randomized trial of diuretics versus volume expansion among normotensive patients with PE and RV dilatation, diuretic therapy led to an improvement in hemodynamic parameters [21]. The conflicting results render volume management a difficult subject to navigate. European Society of Cardiology (ESC) guidelines recommend ≤ 500 cc of crystalloid infusion among patients without an elevated CVP with the caveats previously described [9]. Measures of volume responsiveness are not well-validated in the setting of acute RV failure. Accordingly, an empirical, individualized approach guided by physical examination and management tailored by hemodynamic monitoring may be most appropriate.
While more nuanced in the setting of acute RV failure, diuretics are mainstay in the management of chronic RV failure. Large diuretic doses are often required to relieve volume overload given neurohormonal activation and upregulation of the renin–angiotensin–aldosterone system [2]. In a recent retrospective study of patients with decompensated RV failure secondary to severe precapillary pulmonary hypertension, intravenous diuresis was safe and associated with improved glomerular filtration [22]. While modest volume loading may be appropriate in ischemia- or infarction-induced RV dysfunction, acute and chronic high afterload states represent a different pathophysiology [22]. Consequently, specific therapies aimed to modify preload should be tailored accordingly.
Vasopressors and Restoration of Perfusion Pressure
Myocardial ischemia is the final common pathway of the RV “spiral of death.” The rise in RVSP in response to an elevation in PVR increases RV wall stress and diminishes systolic myocardial perfusion. In an experimental model of acute PE, balloon occlusion of the descending aorta reversed RV failure via augmentation of coronary perfusion. Similar effects were demonstrated with the infusion of phenylephrine and resultant increase in aortic root pressure [1, 23]. Consequently, optimizing mean arterial pressure (MAP) with vasopressors is a cornerstone in the management of acute RV failure and should be considered early among patients with systemic hypotension. A MAP ≥ 65 mmHg serves as a general guideline in shock though some experts advocate for personalized targets [18••, 24]. Elevated CVP in cases of RV failure, as a reflection of organ outflow pressure, may adversely impact microcirculatory flow and tissue perfusion. How best to incorporate this information into the clinical management of shock is not well-defined [24].
Norepinephrine, through its positive effects on RV inotropy, RV-pulmonary artery (PA) coupling, and systemic blood pressure, is the first-line vasopressor in acute RV failure [9]. In a canine model, norepinephrine infusion restored hemodynamic derangements induced by volume loading in cases of RV failure thought not only mediated by augmentation of coronary perfusion, but also through an improvement in RV inotropy [25]. Notably, at higher doses, norepinephrine leads to an increase in PVR; however, the effects vary by population studied [26]. The consequences of tachyarrhythmia and myocardial ischemia may ensue with higher dose catecholamine vasopressors (e.g., norepinephrine, epinephrine). Vasopressin is frequently selected in the setting of RV failure due to its generally neutral effects on PVR [27, 28••]. In an experimental model, vasopressin was shown to induce endothelium-dependent vasodilation of the pulmonary artery; however, vasoconstriction ensues at high doses [18••, 27]. Given lack of titratability, absence of inotropy, and paucity of evidence in the setting of acute RV failure, vasopressin is reserved as a second-line vasoconstrictor [18••, 27, 28••].
Inotropes and Augmentation of Contractility
Loss of contractility results from an interplay of RV overdistension, derangements in myocyte metabolism, and myocardial ischemia [18••]. Following the restoration of systemic blood pressure with vasopressors, inotropes may be the next appropriate management step if CO remains low [2, 18••]. As with vasopressors, studies investigating inotropic therapies in acute RV failure are small and heterogenous; rational use guided by physiology and pharmacology is paramount. At doses of up to 5 mcg/kg/min, dobutamine (a strong beta-agonist with mild alpha1-adrenergic receptor activity) increases myocardial contractility and reduces both PVR and SVR; small studies support its use in acute RV failure [18••]. At escalating doses (> 10 mcg/kg/min), PVR may rise and systemic hypotension may ensue [28••]. Current ESC guidelines recommend the administration of dobutamine in patients with low CI in the setting of acute PE provided systemic blood pressure is adequate [9].
Milrinone, a phosphodiesterase-3 inhibitor, augments myocardial contractility and vasodilates systemic and pulmonary vasculature [28••]. While the dual effect is appealing in RV failure mediated by high afterload, systemic hypotension may limit its use and require the addition of vasopressors. Several small studies have investigated nebulized milrinone in a few clinical settings; this route of administration may decrease PVR without significant effects on systemic blood pressure or V/Q mismatch [28••, 29]. Levosimendan (not approved by the FDA in any setting), a calcium sensitizer with favorable effects on the pulmonary vasculature, augments myocardial contractility without impacting myocardial oxygen demand [30]. Experimental models of PE have demonstrated favorable effects on RV-PA coupling with the administration of this therapy [9, 18••]. Presently, insufficient evidence in the setting of acute RV failure limits its use.
Pulmonary Vasodilators and Afterload Reduction
Partially selective pulmonary vasodilators, such as inhaled nitric oxide (iNO) or inhaled and parenteral prostacyclins, may be appropriate for select patients with acute RV failure and serve as adjuncts following the restoration of systemic blood pressure and CO [2]. As intravenous prostacyclins produce systemic vasodilatation, consideration should be given to inhaled agents in critically ill patients particularly when hypotension is present or anticipated [28••]. Additionally, V/Q matching may be less affected with the use of inhaled therapies which preferentially act on vasculature supplied by ventilated lung units. Importantly, pulmonary vasodilators can precipitate pulmonary edema in those with a poorly compliant or overloaded LV [31].
Inhaled nitric oxide mediates pulmonary vasodilatation by increasing levels of cyclic guanosine monophosphate (cGMP) with downstream smooth muscle relaxation. Small studies have demonstrated improvements in PVR and CO in a variety of clinical settings including ischemic RV dysfunction, post cardiac surgery, and with acute PE [28••, 31]. Administration necessitates continuous delivery typically at a dose of 20 ppm (range 5–20 ppm). Rebound pulmonary hypertension, thought related to downregulation of endogenous NO and elevated endothelin-1 levels, requires gradual and attentive weaning [28••, 31].
Epoprostenol is the preferred parenteral prostacyclin in the ICU setting due to its potency and short half-life. Systemic hypotension and effects on V/Q matching render inhaled epoprostenol (and prostacyclin derivatives) more attractive [18••, 28••]. In addition to PVR reduction, positive inotropic effects are a speculated mechanism bringing about rapid hemodynamic changes [18••]. Beneficial effects of inhaled prostacyclin are equivalent to iNO in the short term [28••]. Robust data with prostacyclins in the ICU setting is limited, with preponderance of studies demonstrating improvement in hemodynamics after cardiac surgery and transplant [28••]. Several pulmonary vasodilators with distinct mechanisms are available; however, these are generally reserved for chronic pulmonary hypertension without an established role in the acute setting [28••].
Respiratory Support
Hypoxemia, hypercapnia, and acidemia mediate pulmonary vasoconstriction and should be mitigated in acute RV failure [18••, 32]. However, achieving these targets may be challenging in acute respiratory distress syndrome (ARDS) with the goal of low lung volumes and permissive hypercapnia. Positive pressure ventilation (PPV) impacts venous return and PVR through a series of complex heart–lung interactions [6, 18••, 33]. While a detailed discussion is beyond the scope of this review, a brief consideration is essential for the provision of RV-protective ventilatory strategies.
The effects of PPV are related to transpulmonary pressure rather than intrathoracic pressure in isolation and dependent on lung compliance. That is, highly compliant lungs more readily transmit airway pressures to the vasculature. The rise in pleural pressure during PPV increases right atrial pressure and therefore may impede right heart filling and preload [33]. Pulmonary vascular resistance is a U-shaped curve with relation to lung volumes. Atelectasis leads to collapse of extra-alveolar vessels while at high lung volumes, intra-alveolar vessels collapse. Both extremes lead to an elevation in PVR [6, 33]. Accordingly, the lowest PVR exists at functional residual capacity and both atelectasis and overdistension raise RV afterload and may precipitate hemodynamic decline. Cautious adjustment of positive end-expiratory pressure (PEEP) and tidal volumes with clinical and hemodynamic monitoring is imperative in the setting of RV failure.
Mechanical Circulatory Support in Acute Right Ventricular Failure
Temporary MCS systems bypass the RV directly (removing blood from the right atrium (RA)/RV and delivering it to the PA), or indirectly (transferring venous blood to the arterial circulation such as with venoarterial extracorporeal membrane oxygenation, VA-ECMO) [10, 34, 35]. When directly bypassing the failing RV, LV preload and CO are increased while end-organs are decongested through the process of RV unloading [34]. Right ventricular assist devices (RVADs) may be further differentiated by (1) pump type—microaxial or extracorporeal centrifugal; (2) mode of insertion—percutaneous or surgical; (3) ability to splice in an oxygenator; and (4) hemodynamic effects and degree of support provided (Table 2, Fig. 1). RVADs may be used in isolation or in conjunction with left-sided MCS in cases of biventricular failure. Device characteristics, patient physiology, and center-specific expertise are incorporated into matching the appropriate therapy to the patient. Here, we review select temporary RV MCS device design, insertion, physiology, and outcomes data.
Mechanical circulatory support devices for right ventricular failure. A Intra-aortic balloon pump (IABP) is percutaneously inserted via femoral or axillary artery and positioned in the descending aorta. Counterpulsation decreases left ventricular afterload and may therefore benefit the failing right ventricle; however, robust clinical data are lacking. B Venoarterial extracorporeal membrane oxygenation (VA ECMO) is an indirect right ventricular bypass device improving systemic perfusion and oxygenation used in several clinical circumstances. C Centrifugal extracorporeal pumps are direct right ventricular bypass devices inserted either percutaneously or surgically with the ability to include an oxygenator into the circuit. D The microaxial flow pump (Impella RP) is a percutaneous direct right ventricular bypass device improving hemodynamics however does not support an oxygenator (reproduced from Akhmerov and Ramzy [42••], with permission from Elsevier)
Microaxial Flow RVAD
The Impella RP® (Abiomed, Danvers, MA, USA) is a 22 Fr microaxial continuous flow pump on an 11 Fr catheter capable of delivering a flow of up to 4 L/min. The device is placed percutaneously through the femoral vein and with fluoroscopic guidance, maneuvered through the right heart chambers into position with the outflow catheter resting within the proximal pulmonary artery and the corresponding inflow within the inferior vena cava. Indications for use include acute right heart failure due to acute myocardial infarction and post pericardiotomy shock (i.e., in the setting of heart transplantation or LVAD implant) [36]. Use of this device has been reported in right heart failure following PE and from complications due to COVID-19 [37, 38].
While randomized clinical data is not available, a prospective cohort study (RECOVER RIGHT) of 30 patients with refractory RV failure provided safety and efficacy data for the device. Specifically, patients had immediate hemodynamic improvement following Impella insertion with an increase in cardiac index (average 1.8 to 3.3 L/min/m2) and decrease in central venous pressure (average 19 to 13 mmHg) over an average time on support of 3.0 ± 1.5 days. Overall, 30-day survival in this cohort was approximately 73% which was mirrored in subsequent registry data [36, 39, 40]. Major complications such as access site bleeding, tricuspid insufficiency, and hemolysis were uncommon. Post-marketing data initially indicated worse outcomes; however, improper patient selection was thought to be a significant contributor. Clinical data in scenarios such as acute PE are limited to case series; however, this is a promising target for future study particularly with an updated catheter system that can be placed through the right internal jugular vein in development [37, 41].
Percutaneous Extracorporeal Centrifugal Flow RVADs
Extracorporeal centrifugal flow percutaneous RVADs, such as the LifeSPARC® Pump (LivaNova, UK), formerly TandemHeart, or CentriMag RVAD (Abbott, IL, USA) can be configured with 2 venous cannulas or a single, dual-lumen cannula. With the former approach, bilateral femoral access is used to guide one cannula to the RA and the other, to the PA [10]. However, this configuration has largely been abandoned with the introduction of the ProtekDuo® (LivaNova, UK) dual-lumen cannula allowing for single internal jugular venous site access. The 29/31F “cannula-within-a-cannula” design is inserted in a manner similar to that of a pulmonary artery catheter with inflow ports positioned in the RA and outflow ports in the PA [10, 42••, 43•]. As with any extracorporeal centrifugal pump, an oxygenator may be spliced within the circuit allowing for gas exchange [10].
Bypassing the right heart leads to improved right heart filling pressures and increased left ventricular preload, which is accomplished by either cannulation strategy [10]. Capable of delivering up to 4.5 L/min of flow, this RVAD has been used in patients with post cardiotomy RV failure including following LVAD placement, myocarditis, inferior myocardial infarction, or severe pulmonary hypertension and acute PE [44,45,46]. Initial experience of the TandemHeart as an RVAD was published in a retrospective observational registry of 46 patients who underwent percutaneous or surgical insertion in the treatment of RV failure from acute myocardial infarction, heart failure, or post cardiac surgery including LVAD placement [47]. Within 48 h post insertion, there were significant improvements in RA pressure (21 ± 8 v 16 ± 7 mmHg), PASP (43 ± 15 v 33 ± 15 mmHg), and cardiac index (1.7 ± 0.7 v 2.2 ± 0.6). In a recent systemic review of 7 studies comprised of 105 patients treated with the ProtekDuo, conversion to a surgical RVAD ranged from 11 to 35% and 30-day mortality ranged from 15 to 40% [44, 48, 49]. Complications included significant tricuspid regurgitation and rare cannula migration, hemolysis, and device thrombosis. As most of the cohort had previously undergone LVAD implant, the patients represent a different phenotype compared to acute PE and pulmonary hypertension [44].
Surgically Implanted RVAD
The CentriMag (Abbott, IL, USA) is a magnetically levitated extracorporeal centrifugal pump which may be used as part of a VA ECMO circuit or as an RVAD. The CentriMag has been used as a support device in myocarditis, cardiogenic shock, and post cardiotomy for both right and/or left heart failure; use as an RVAD is approved for up to 30 days [50]. The device is surgically inserted via thoracotomy or sternotomy with the drainage cannula positioned in the RA and the return in the PA allowing for up to 10 L/min of flow [50]. Accordingly, this approach may be appropriate among patients with a recent sternotomy. The RVAD improves flow to the left heart, increasing mean arterial pressure and mixed venous saturation, while lowering right-sided filling pressures [42••, 51]. However, the hemodynamic support offered by percutaneously inserted RVADs is often sufficient and less invasive than the surgical approach.
The magnetically levitated rotor eliminates the needs for bearings and therefore reduces the risk of hemolysis and thromboembolism [52]. As with percutaneously inserted extracorporeal centrifugal pumps, the addition of an oxygenator to the circuit (Oxy-RVAD) supports gas exchange [45]. In a retrospective review in 80 patients with RV failure, including post cardiotomy shock, post cardiac transplant, and LVAD placement, CentriMag use was associated with a 30-day survival of 64% [45, 53].
Venoarterial Extracorporeal Membrane Oxygenation
Venoarterial extracorporeal membrane oxygenation allows for up to 5–6 L/min and has several indications in the treatment of right ventricular failure such as acute PE, cardiac arrest, cardiogenic shock, post cardiac transplant allograft failure, pulmonary hypertension, or as a bridge to transplant. The VA ECMO circuit consists of a pump and controller, an oxygenator, a 23–28 Fr venous drainage cannula, and a 15–19 Fr arterial return cannula [54]. Cannulation is commonly performed percutaneously with drainage cannula placed in the femoral vein and advanced to the proximal inferior vena cava with the return cannula placed in the femoral artery. Alternative configurations such as femoral/internal jugular drainage and axillary return, as well as open central cannulation of the RA and aorta, are sometimes performed [55].
VA ECMO indirectly bypasses the heart by draining blood from the RA and returning oxygenated blood retrograde through the femoral artery. Hemodynamic changes typically include a decrease in RA and PA pressures but an increased in mean arterial pressure and therefore LV afterload. Accordingly, with concomitant LV dysfunction, elevated LV afterload may lead to pulmonary edema and a rise in PA pressures [10, 56]. In this setting, it is becoming increasingly more common to use an additional LV unloading strategy such as placement of surgical vent, an intra-aortic balloon pump (IABP), or Impella [57, 58].
As possible with other centrifugal extracorporeal pumps, VA ECMO includes an oxygenator allowing for gas exchange [59, 60]. In the setting of acute RV failure, VA ECMO acts as bridging therapy until the patient recovers or definitive treatment is available. This support strategy has been used in treatment of acute PE pending catheter directed therapy or recovery, with a reported survival range of 53–76% [61,62,63,64]. Its use in patients with pulmonary arterial hypertension bridged to lung transplant is limited to small case series with survival rates of 50–100% [65]. Additionally, VA ECMO is used as a salvage treatment for patients who develop RV failure post LVAD with reported in-hospital mortality of 25–40% [66, 67].
Selection of Mechanical Circulatory Support Devices
Currently, there are no guidelines or randomized clinical data to guide implementation or selection of devices in treatment of RV failure. Correspondingly, an understanding of patient physiology and invasive hemodynamics is imperative to select the appropriate support device. Initial strategies include treatment of reversible causes, optimization of loading conditions, and medical therapies as previously described. Refractory cases may be considered for MCS; however, an exit strategy (bridge to recovery, transplantation, durable MCS) should be addressed [10].
Factors considered in device selection include the presence of biventricular failure, isolated RV failure, and need for extracorporeal oxygenation. Anticipated duration of support as well as the need for an oxygenator must weight into the decision [10, 42••]. Patients with biventricular failure are commonly placed on VA ECMO or a combination of individual right- and left-sided support devices (i.e., Impella RP or ProtekDuo with Impella CP or Impella 5.5). With concomitant LV dysfunction, increased LV preload mediated with direct RV bypass may cause elevated left-sided filling pressures and result in pulmonary edema. Several options are available for those with isolated RV failure. Impaired gas exchange and the need for an oxygenator render the Impella RP unfavorable; VA ECMO or ProtekDuo RVAD may be appropriate in such circumstances [35, 43•]. A multidisciplinary shock team evaluation in conjunction with local expertise may be incorporated into the final decision.
Conclusions
A resurgence of interest in the RV has led to an improved understanding of hemodynamics and consequently to a more refined approach to tailored pharmacologic management. Optimization of RV preload, coronary perfusion, contractility, and pulmonary vascular tone with attention to respiratory support are cornerstones in the initial management of the acutely failing RV. In severe cases, several short-term MCS devices allowing for RV bypass are available on the market. Presently, robust outcomes data from randomized trials are lacking. As technology evolves, we hope to see less-invasive, safer options, and a better understanding of appropriate device selection.
Abbreviations
- cGMP:
-
Cyclic guanosine monophosphate
- CO:
-
Cardiac output
- CVP:
-
Central venous pressure
- EF:
-
Ejection fraction
- ICU:
-
Intensive care unit
- iNO:
-
Inhaled nitric oxide
- LV:
-
Left ventricle
- LVAD:
-
Left ventricular assist device
- LVEDV:
-
Left ventricular end-diastolic volume
- MAP:
-
Mean arterial pressure
- MCS:
-
Mechanical circulatory support
- MI:
-
Myocardial infarction
- PA:
-
Pulmonary artery
- PADP:
-
Pulmonary artery diastolic pressure
- PAPi:
-
Pulmonary artery pulsatility index
- PASP:
-
Pulmonary artery systolic pressure
- PCWP:
-
Pulmonary capillary wedge pressure
- PE:
-
Pulmonary embolism
- PEEP:
-
Positive end-expiratory pressure
- PPV:
-
Positive pressure ventilation
- PVR:
-
Pulmonary vascular resistance
- RA:
-
Right atrium
- RAP:
-
Right atrial pressure
- RV:
-
Right ventricle
- RVAD:
-
Right ventricular assist device
- RVEDV:
-
Right ventricular end-diastolic volume
- RVSWI:
-
Right ventricular stroke work index
- SV:
-
Stroke volume
- VA ECMO:
-
Venoarterial extracorporeal membrane oxygenation
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Greyson CR. Pathophysiology of right ventricular failure. Crit Care Med. 2008;36(1 Suppl):S57-65. https://doi.org/10.1097/01.Ccm.0000296265.52518.70.
Konstam MA, Kiernan MS, Bernstein D, Bozkurt B, Jacob M, Kapur NK, et al. Evaluation and management of right-sided heart failure: a scientific statement from the American Heart Association. Circulation. 2018;137(20):e578–622. https://doi.org/10.1161/cir.0000000000000560.
Dell’Italia LJ. Anatomy and physiology of the right ventricle. Cardiol Clin. 2012;30(2):167–87. https://doi.org/10.1016/j.ccl.2012.03.009.
Haddad F, Doyle R, Murphy DJ, Hunt SA. Right ventricular function in cardiovascular disease, part II: pathophysiology, clinical importance, and management of right ventricular failure. Circulation. 2008;117(13):1717–31. https://doi.org/10.1161/circulationaha.107.653584.
Friedberg MK, Redington AN. Right versus left ventricular failure: differences, similarities, and interactions. Circulation. 2014;129(9):1033–44. https://doi.org/10.1161/circulationaha.113.001375.
Mahmood SS, Pinsky MR. Heart-lung interactions during mechanical ventilation: the basics. Ann Transl Med. 2018;6(18):349. https://doi.org/10.21037/atm.2018.04.29.
Friedberg MK. Imaging right-left ventricular interactions. JACC Cardiovasc Imaging. 2018;11(5):755–71. https://doi.org/10.1016/j.jcmg.2018.01.028.
Cecconi M, Johnston E, Rhodes A. What role does the right side of the heart play in circulation? Crit Care. 2006;10(3):S5. https://doi.org/10.1186/cc4832.
Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing G-J, Harjola V-P, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41(4):543–603. https://doi.org/10.1093/eurheartj/ehz405.
Kapur NK, Esposito ML, Bader Y, Morine KJ, Kiernan MS, Pham DT, et al. Mechanical circulatory support devices for acute right ventricular failure. Circulation. 2017;136(3):314–26. https://doi.org/10.1161/circulationaha.116.025290.
Voelkel NF, Quaife RA, Leinwand LA, Barst RJ, McGoon MD, Meldrum DR, et al. Right ventricular function and failure: report of a National Heart, Lung, and Blood Institute working group on cellular and molecular mechanisms of right heart failure. Circulation. 2006;114(17):1883–91. https://doi.org/10.1161/circulationaha.106.632208.
Saxena A, Garan AR, Kapur NK, O’Neill WW, Lindenfeld J, Pinney SP, et al. Value of hemodynamic monitoring in patients with cardiogenic shock undergoing mechanical circulatory support. Circulation. 2020;141(14):1184–97. https://doi.org/10.1161/circulationaha.119.043080.
Drazner MH, Velez-Martinez M, Ayers CR, Reimold SC, Thibodeau JT, Mishkin JD, et al. Relationship of right- to left-sided ventricular filling pressures in advanced heart failure: insights from the ESCAPE trial. Circ Heart Fail. 2013;6(2):264–70. https://doi.org/10.1161/circheartfailure.112.000204.
Tehrani BN, Truesdell AG, Psotka MA, Rosner C, Singh R, Sinha SS, et al. A standardized and comprehensive approach to the management of cardiogenic shock. JACC Heart Fail. 2020;8(11):879–91. https://doi.org/10.1016/j.jchf.2020.09.005.
Lim HS, Gustafsson F. Pulmonary artery pulsatility index: physiological basis and clinical application. Eur J Heart Fail. 2020;22(1):32–8. https://doi.org/10.1002/ejhf.1679.
Korabathina R, Heffernan KS, Paruchuri V, Patel AR, Mudd JO, Prutkin JM, et al. The pulmonary artery pulsatility index identifies severe right ventricular dysfunction in acute inferior myocardial infarction. Catheter Cardiovasc Interv. 2012;80(4):593–600. https://doi.org/10.1002/ccd.23309.
Mortensen CS, Kramer A, Schultz J, Lyhne MD, Nielsen-Kudsk JE, Andersen A. Impact of preload on right ventricular hemodynamics in acute pulmonary embolism. Crit Care Med. 2020;48(12):e1306–12. https://doi.org/10.1097/ccm.0000000000004643.
•• Ventetuolo CE, Klinger JR. Management of acute right ventricular failure in the intensive care unit. Ann Am Thorac Soc. 2014;11(5):811–22. https://doi.org/10.1513/AnnalsATS.201312-446FR. This review discusses right ventricular pathophysiology and offers guidance on medical therapies in the critically ill population.
Piazza G, Goldhaber SZ. The acutely decompensated right ventricle: pathways for diagnosis and management. Chest. 2005;128(3):1836–52. https://doi.org/10.1378/chest.128.3.1836.
Mercat A, Diehl JL, Meyer G, Teboul JL, Sors H. Hemodynamic effects of fluid loading in acute massive pulmonary embolism. Crit Care Med. 1999;27(3):540–4. https://doi.org/10.1097/00003246-199903000-00032.
Ternacle J, Gallet R, Mekontso-Dessap A, Meyer G, Maitre B, Bensaid A, et al. Diuretics in normotensive patients with acute pulmonary embolism and right ventricular dilatation. Circ J. 2013;77(10):2612–8. https://doi.org/10.1253/circj.cj-13-0404.
Labrada L, Romero C, Sadek A, Belardo D, Raza Y, Forfia P. Intravenous diuresis in severe precapillary pulmonary-hypertension-related right heart failure: effects on renal function and blood pressure. J Clin Med. 2023;12(22):7149.
Spotnitz HM, Berman MA, Epstein SE. Pathophysiology and experimental treatment of acute pulmonary embolism. Am Heart J. 1971;82(4):511–20. https://doi.org/10.1016/0002-8703(71)90236-5.
Kato R, Pinsky MR. Personalizing blood pressure management in septic shock. Ann Intensive Care. 2015;5(1):41. https://doi.org/10.1186/s13613-015-0085-5.
Ghignone M, Girling L, Prewitt RM. Volume expansion versus norepinephrine in treatment of a low cardiac output complicating an acute increase in right ventricular afterload in dogs. Anesthesiology. 1984;60(2):132–5. https://doi.org/10.1097/00000542-198402000-00009.
Kerbaul F, Rondelet B, Motte S, Fesler P, Hubloue I, Ewalenko P, et al. Effects of norepinephrine and dobutamine on pressure load-induced right ventricular failure. Crit Care Med. 2004;32(4):1035–40. https://doi.org/10.1097/01.ccm.0000120052.77953.07.
Pérez-Nieto OR, Gómez-Oropeza I, Quintero-Leyra A, Kammar-García A, Zamarrón-López ÉI, Soto-Estrada M, et al. Hemodynamic and respiratory support in pulmonary embolism: a narrative review. Front Med (Lausanne). 2023;10:1123793. https://doi.org/10.3389/fmed.2023.1123793.
•• Price LC, Wort SJ, Finney SJ, Marino PS, Brett SJ. Pulmonary vascular and right ventricular dysfunction in adult critical care: current and emerging options for management: a systematic literature review. Crit Care. 2010;14(5):R169. https://doi.org/10.1186/cc9264. This review is a comprehensive summary of the evidence and guidelines in the medical management of right ventricular failure.
Wang H, Gong M, Zhou B, Dai A. Comparison of inhaled and intravenous milrinone in patients with pulmonary hypertension undergoing mitral valve surgery. Adv Ther. 2009;26(4):462–8. https://doi.org/10.1007/s12325-009-0019-4.
Hansen MS, Andersen A, Nielsen-Kudsk JE. Levosimendan in pulmonary hypertension and right heart failure. Pulm Circ. 2018;8(3):2045894018790905. https://doi.org/10.1177/2045894018790905.
Ichinose F, Roberts JD Jr, Zapol WM. Inhaled nitric oxide: a selective pulmonary vasodilator: current uses and therapeutic potential. Circulation. 2004;109(25):3106–11. https://doi.org/10.1161/01.Cir.0000134595.80170.62.
Cheifetz IM. Cardiorespiratory interactions: the relationship between mechanical ventilation and hemodynamics. Respir Care. 2014;59(12):1937–45. https://doi.org/10.4187/respcare.03486.
Cortes-Puentes GA, Oeckler RA, Marini JJ. Physiology-guided management of hemodynamics in acute respiratory distress syndrome. Ann Transl Med. 2018;6(18):353. https://doi.org/10.21037/atm.2018.04.40.
Alkhunaizi FA, Burkhoff D, Brener MI. Right-sided mechanical circulatory support - a hemodynamic perspective. Curr Heart Fail Rep. 2022;19(5):334–45. https://doi.org/10.1007/s11897-022-00562-1.
DeFilippis EM, Topkara VK, Kirtane AJ, Takeda K, Naka Y, Garan AR. Mechanical circulatory support for right ventricular failure. Card Fail Rev. 2022;8: e14. https://doi.org/10.15420/cfr.2021.11.
Anderson MB, Goldstein J, Milano C, Morris LD, Kormos RL, Bhama J, et al. Benefits of a novel percutaneous ventricular assist device for right heart failure: the prospective RECOVER RIGHT study of the Impella RP device. J Heart Lung Transplant. 2015;34(12):1549–60. https://doi.org/10.1016/j.healun.2015.08.018.
Elder M, Blank N, Kaki A, Alraies MC, Grines CL, Kajy M, et al. Mechanical circulatory support for acute right ventricular failure in the setting of pulmonary embolism. J Interv Cardiol. 2018;31(4):518–24. https://doi.org/10.1111/joic.12503.
Cohen GI, Schreiber T, Singh H, Kaki A. Percutaneous thrombectomy and right ventricular mechanical circulatory support for pulmonary embolism in a coronavirus disease 2019 patient: case report, 1-year update, and echocardiographic findings. Eur Heart J Case Rep. 2022;6(1):ytac008. https://doi.org/10.1093/ehjcr/ytac008.
Anderson M, Morris DL, Tang D, Batsides G, Kirtane A, Hanson I, et al. Outcomes of patients with right ventricular failure requiring short-term hemodynamic support with the Impella RP device. J Heart Lung Transplant. 2018;37(12):1448–58. https://doi.org/10.1016/j.healun.2018.08.001.
Botti G, Gramegna M, Burzotta F, Masiero G, Briguori C, Trani C, et al. Impella RP for patients with acute right ventricular failure and cardiogenic shock: a subanalysis from the IMP-IT registry. J Pers Med. 2022;12(9). https://doi.org/10.3390/jpm12091481.
Elder M, Blank N, Shemesh A, Pahuja M, Kaki A, Mohamad T, et al. Mechanical circulatory support for high-risk pulmonary embolism. Interv Cardiol Clin. 2018;7(1):119–28. https://doi.org/10.1016/j.iccl.2017.09.002.
•• Akhmerov A, Ramzy D. Mechanical circulatory support in right ventricular failure. Interv Cardiol Clin. 2021;10(2):185–94. https://doi.org/10.1016/j.iccl.2020.12.010. This review provides a comprehensive overview over mechanical circulatory support options in right ventricular failure.
• Kuroda T, Miyagi C, Fukamachi K, Karimov JH. Mechanical circulatory support devices and treatment strategies for right heart failure. Front Cardiovasc Med. 2022;9: 951234. https://doi.org/10.3389/fcvm.2022.951234. This review discusses temporary and durable mechanical circulatory support options in right ventricular failure.
Alam A, Baran DA, Doshi H, Van Zyl J, Patlolla S, Salem M, et al. Safety and efficacy of ProtekDuo right ventricular assist device: a systemic review. Artif Organs. 2023;47(7):1094–103. https://doi.org/10.1111/aor.14525.
Leidenfrost J, Prasad S, Itoh A, Lawrance CP, Bell JM, Silvestry SC. Right ventricular assist device with membrane oxygenator support for right ventricular failure following implantable left ventricular assist device placement. Eur J Cardiothorac Surg. 2016;49(1):73–7. https://doi.org/10.1093/ejcts/ezv116.
Lee TML, Bianchi P, Kourliouros A, Price LC, Ledot S. Percutaneous oxygenated right ventricular assist device for pulmonary embolism: a case series. Artif Organs. 2023;47(3):595–603. https://doi.org/10.1111/aor.14420.
Kapur NK, Paruchuri V, Jagannathan A, Steinberg D, Chakrabarti AK, Pinto D, et al. Mechanical circulatory support for right ventricular failure. JACC Heart Fail. 2013;1(2):127–34. https://doi.org/10.1016/j.jchf.2013.01.007.
Ravichandran AK, Baran DA, Stelling K, Cowger JA, Salerno CT. Outcomes with the tandem Protek Duo dual-lumen percutaneous right ventricular assist device. ASAIO J. 2018;64(4):570–2. https://doi.org/10.1097/MAT.0000000000000709.
Salna M, Garan AR, Kirtane AJ, Karmpaliotis D, Green P, Takayama H, et al. Novel percutaneous dual-lumen cannula-based right ventricular assist device provides effective support for refractory right ventricular failure after left ventricular assist device implantation. Interact Cardiovasc Thorac Surg. 2020;30(4):499–506. https://doi.org/10.1093/icvts/ivz322.
Chopski SG, Murad NM, Fox CS, Stevens RM, Throckmorton AL. Mechanical circulatory support of the right ventricle for adult and pediatric patients with heart failure. ASAIO J. 2019;65(2):106–16. https://doi.org/10.1097/MAT.0000000000000815.
Takayama H, Naka Y, Kodali SK, Vincent JA, Addonizio LJ, Jorde UP, et al. A novel approach to percutaneous right-ventricular mechanical support. Eur J Cardiothorac Surg. 2012;41(2):423–6. https://doi.org/10.1016/j.ejcts.2011.05.041.
John R, Long JW, Massey HT, Griffith BP, Sun BC, Tector AJ, et al. Outcomes of a multicenter trial of the Levitronix CentriMag ventricular assist system for short-term circulatory support. J Thorac Cardiovasc Surg. 2011;141(4):932–9. https://doi.org/10.1016/j.jtcvs.2010.03.046.
Bhama JK, Bansal U, Winger DG, Teuteberg JJ, Bermudez C, Kormos RL, et al. Clinical experience with temporary right ventricular mechanical circulatory support. J Thorac Cardiovasc Surg. 2018;156(5):1885–91. https://doi.org/10.1016/j.jtcvs.2018.04.094.
Friedman O, Horowitz JM, Ramzy D. Advanced cardiopulmonary support for pulmonary embolism. Tech Vasc Interv Radiol. 2017;20(3):179–84. https://doi.org/10.1053/j.tvir.2017.07.007.
Pavlushkov E, Berman M, Valchanov K. Cannulation techniques for extracorporeal life support. Ann Transl Med. 2017;5(4):70. https://doi.org/10.21037/atm.2016.11.47.
Boulate D, Luyt CE, Pozzi M, Niculescu M, Combes A, Leprince P, et al. Acute lung injury after mechanical circulatory support implantation in patients on extracorporeal life support: an unrecognized problem. Eur J Cardiothorac Surg. 2013;44(3):544–9; discussion 9–50. https://doi.org/10.1093/ejcts/ezt125.
Pan P, Yan P, Liu D, Wang X, Zhou X, Long Y, et al. Outcomes of VA-ECMO with and without left centricular (LV) decompression using intra-aortic balloon pumping (IABP) versus other LV decompression techniques: a systematic review and meta-analysis. Med Sci Monit. 2020;26: e924009. https://doi.org/10.12659/MSM.924009.
Koeckert MS, Jorde UP, Naka Y, Moses JW, Takayama H. Impella LP 2.5 for left ventricular unloading during venoarterial extracorporeal membrane oxygenation support. J Card Surg. 2011;26(6):666–8. https://doi.org/10.1111/j.1540-8191.2011.01338.x.
Kopanczyk R, Al-Qudsi OH, Uribe A, Periel L, Fiorda-Diaz J, Abdel-Rasoul M, et al. Right ventricular dysfunction in patients with coronavirus disease 2019 supported with extracorporeal membrane oxygenation. J Cardiothorac Vasc Anesth. 2022;36(2):629–31. https://doi.org/10.1053/j.jvca.2021.05.019.
Zochios V, Parhar K, Tunnicliffe W, Roscoe A, Gao F. The right ventricle in ARDS. Chest. 2017;152(1):181–93. https://doi.org/10.1016/j.chest.2017.02.019.
George B, Parazino M, Omar HR, Davis G, Guglin M, Gurley J, et al. A retrospective comparison of survivors and non-survivors of massive pulmonary embolism receiving veno-arterial extracorporeal membrane oxygenation support. Resuscitation. 2018;122:1–5. https://doi.org/10.1016/j.resuscitation.2017.11.034.
Guliani S, Das Gupta J, Osofsky R, Kraai EP, Mitchell JA, Dettmer TS, et al. Venoarterial extracorporeal membrane oxygenation is an effective management strategy for massive pulmonary embolism patients. J Vasc Surg Venous Lymphat Disord. 2021;9(2):307–14. https://doi.org/10.1016/j.jvsv.2020.04.033.
Ius F, Hoeper MM, Fegbeutel C, Kuhn C, Olsson K, Koigeldiyev N, et al. Extracorporeal membrane oxygenation and surgical embolectomy for high-risk pulmonary embolism. Eur Respir J. 2019;53(4). https://doi.org/10.1183/13993003.01773-2018.
Yusuff HO, Zochios V, Vuylsteke A. Extracorporeal membrane oxygenation in acute massive pulmonary embolism: a systematic review. Perfusion. 2015;30(8):611–6. https://doi.org/10.1177/0267659115583377.
Hoeper MM, Benza RL, Corris P, de Perrot M, Fadel E, Keogh AM, et al. Intensive care, right ventricular support and lung transplantation in patients with pulmonary hypertension. Eur Respir J. 2019;53(1). https://doi.org/10.1183/13993003.01906-2018 .
Joshi Y, Bories MC, Aissaoui N, Grinda JM, Bel A, Latremouille C, et al. Percutaneous venopulmonary artery extracorporeal membrane oxygenation for right heart failure after left ventricular assist device insertion. Interact Cardiovasc Thorac Surg. 2021;33(6):978–85. https://doi.org/10.1093/icvts/ivab197.
Riebandt J, Haberl T, Wiedemann D, Moayedifar R, Schloeglhofer T, Mahr S, et al. Extracorporeal membrane oxygenation support for right ventricular failure after left ventricular assist device implantation. Eur J Cardiothorac Surg. 2018;53(3):590–5. https://doi.org/10.1093/ejcts/ezx349.
Author information
Authors and Affiliations
Contributions
EY wrote the main manuscript text, created Table 1. MC wrote the main manuscript text, created Table 2. OF wrote the main manuscript text. JH wrote the main manuscript text.
Corresponding author
Ethics declarations
Conflict of Interest
James M. Horowitz reports consulting fees from Inari Medical and Penumbra for clinical trial design. The other authors report no conflict of interest pertinent to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yuriditsky, E., Chonde, M., Friedman, O. et al. Medical and Mechanical Circulatory Support of the Failing Right Ventricle. Curr Cardiol Rep 26, 23–34 (2024). https://doi.org/10.1007/s11886-023-02012-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-023-02012-3