Abstract
Purpose of Review
The goal of this paper is to highlight the multifaceted approach heart failure (HF) nurse practitioners (NPs) use to manage patients. We were seeking to answer if NPs have the scope of clinical skills to manage the complexity of HF patients.
Recent Findings
NP care in HF has been shown to reduce readmissions, improve timeliness of visits, decrease cost, and improve quality outcomes in small heterogeneous studies.
Summary
The evidence supports that NPs provide multifaceted, patient-centered care for at all stages on the continuum of HF. Our goals as NPs are to reduce the healthcare financial strain and improve access to high quality care. Telehealth is an emerging technology that shows promise in HF management by improving access and decreasing readmissions. Telehealth use and recognition increased with the COVID-19 pandemic. Future research should focus on NP run clinics, cost effectiveness, and quality of care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Heart failure is a destructive disease that interrupts a person’s lifestyle. It threatens quality of life by the economic challenges that come along with disease management and potential loss of employment. HF can hinder a person’s zest for life and cause a decrease in a person’s functional capacity that impedes their ability to enjoy those things in life that were once so important [1].
Globally, over 23 million people are diagnosed with heart failure (HF) and this is associated with high morbidity and mortality [2]. The 5-year mortality is still close to 50% [3]. In 2020, the prevalence of HF was 6.9 million in the USA. In addition, health care costs are predicted to rise associated with hospital admissions. Hospital readmissions for HF patients age greater than 65 remain the most common reason for hospitalization. Readmissions for HF within 30 days of discharge are still as high as 25% nationally despite substantial improvements in HF care. The incidence of developing HF over a lifetime affects males (30–42%) slightly greater than females (32–39%) respectively [2]. Many of these will be affected by multiple hospitalizations for HF over their lifetime. The post discharge mortality is 30% within the first year.
In 2020, the median cost for a HF hospitalization was estimated at approximately $15,879 per patient. It is predicted that hospital admissions will rise over the next decade, increasing hospitalizations, therefore placing an extreme financial burden and continued challenges for the healthcare system. These costs are expected to double from $30 billion to $53 billion by 2030 [2]. With the impact of this financial forecast and the disease burden of HF, it is imperative to develop new initiatives in care modalities. The use of nurse practitioner (NP) led interventions and care programs have demonstrated improved outcomes. Managing this devastating disease requires a multidisciplinary HF team and strong leadership that is not only dynamic but innovative with HF management.
Definition and Classification of HF
Historically, HF was defined as a complex chronic disease which is distinguished by a decrease in functional capacity of the heart by either impaired pumping, HF reduced ejection fraction (HFrEF), or from inadequate filling, heart failure preserved ejection fraction (HFpEF) [4]. Fifty percent of patients with HF have systolic dysfunction [5].
Recently, Bozkurt and colleagues published the consensus statement of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure released in 2021. In this report, they provided a new universal definition of HF which stated that HF is “a clinical syndrome with current or prior symptoms and/or signs caused by a structural and/or functional cardiac abnormality and corroborated by elevated natriuretic peptide levels and/or objective evidence of pulmonary or systemic congestion” [6]. The goal of this change was to standardize the definition across professional societies and countries.
The current American College of Cardiology (ACC)/American Heart Association (AHA) guidelines categorizes HF according to stage A through D. Debra Beck astutely noted that “these designations have been widely accepted within the field, although they are not well recognized by non-cardiologists, payers, or patients.” The consensus statement affirms that the current staging makes small but potentially clinically meaningful revisions to terminology that are intended to spur earlier intervention, such as targeted therapies for HF prevention. We know that persons with stages A and B have better mortality rates than those with more advanced stages such as C and D [7]. Therefore, recognizing stages A and B allows for earlier diagnosis before clinical signs and symptoms appear.
This staging of HF is intended to complement but not to replace the New York Heart Association (NYHA) functional classification. NYHA classification is an assessment tool used to characterize symptoms and functional capacity of patients with HF. It is a subjective assessment that can vary over time gauging the severity of symptoms in patients with stage C or D [8].
US Healthcare Performance
The overall performance of the US healthcare system is lacking as evidenced by the US life expectancy compared to other high-income countries. The US life expectancy was approximately 3 years less than our peer countries and then after the coronavirus-19 pandemic, the life expectancy difference increased to 5 years [9]. Previously, HF care consisted of intermittent visits to a doctor only when the patient perceived a health concern which is often under-recognized by the patient. These visits could be very infrequent, therefore limiting the opportunity for health care optimization. To address this issue, medical teams encompassed multiple clinicians including physicians, nurse practitioners (NPs), physician assistants (PAs), and pharmacists. These practitioners collaborated with primary care and specialty teams to deliver the concept of “medical home” care to patients and families [9].
The concept of the “medical home” was developed to improve health outcomes, decrease health care costs, and enhance the overall patient experience. It is intended to replace poorly coordinated, acute-focused, episodic care with coordinated, proactive, preventative, acute, chronic, long-term, and end-of-life care. The “medical home” team may include a primary care doctor, a nurse, support staff, and other health care professionals like pharmacists or social workers. This team approach works closely to get patients the care and services they need to get and stay healthy [10]. NP run HF clinics share similarities to the “medical home” model.
Nurse Practitioner Attributes
NPs are licensed health care providers who provide comprehensive, patient-centered care. NPs diagnose and treat patients, prescribe medications, refer, and manage acute and chronic diseases, while emphasizing health promotion, disease prevention, and patient satisfaction. NPs are skilled at doing things like teaching, counseling, and advocating; things we have always done as nurses. We manage some of the sickest patients’ primary care through critical care. These patients come with numerous chronic diseases and are on multiple medications. They often have limited resources to help them manage their family, social, and economic problems [11]. In order to diagnose, NPs may order testing such as but not limited to echocardiograms, stress tests, coronary artery calcium scoring, right and left heart catheterizations, electrophysiology studies, and blood work. We consult with specialty teams such as nephrology, hematology, bariatric surgery, sleep medicine, electrophysiology, interventional cardiology, and the structural heart team. We may recognize the need for physical therapy, occupational therapy, cardiac rehab, tobacco cessation, and lymphedema clinic as additional support for our patients.
There is incontrovertible evidence demonstrating that NPs have been providing, “cost-effective and high-quality care for almost 50 years.” Patients managed by NPs in an HF run clinic have “fewer unnecessary hospital readmissions, fewer potentially preventable hospitalizations, higher patient satisfaction and fewer unnecessary emergency room visits” [12].
NPs build relationships with their HF patients. Bonds are built between the NPs and patients who we take care of over many years. They often become more than merely a patient. We get to know the families, likes and dislikes, major life events, hobbies, jobs, and more. This longitudinal relationship helps us as clinicians plan a patient-centered care plan, reflective of our patients’ values and preferences and include them in shared-decision making regarding their care. As a result of these bonds, NPs can see subtle differences and recognize when their patient may be declining or having a HF exacerbation, and even approaching late stages of the disease. This allows us to pick the most opportune time to have important conversations regarding advanced HF therapies versus end-of-life care [13].
HF is one of the most complex diseases in cardiology care. Many challenges accompany the management of patients living with HF. The treatment of HF is a little of an art and a science; however, it can be time consuming and tedious.
NPs often use a multidisciplinary approach to reach desirable outcomes for HF patients. NPs work with a unified team of cardiologists, nurse educators, pharmacists, dieticians, social workers, and ancillary support staff who can make an important difference in patient care and preventing readmissions [14•]. Along with a strong HF team, the literature supports the use of pharmacologic therapies, evidence-based or guideline-directed medical therapies (GDMT) shown to improve mortality, quality of life, and reduce hospital admissions. The NPs and their team work to empower their patients to take ownership of their disease. Our team provides education to patients and families and reinforces this routinely. We focus on disease pathology, medication compliance, dietary compliance, and symptom awareness. HF is difficult for our patients because it requires lifestyle changes in addition to the medical therapies prescribed to have a successful outcome. “The majority of health outcomes are determined by daily habits and choices made at home or at work” [9]. These changes in daily habits can be a challenge for those with poor access to healthy foods such as those who live in urban food deserts and have low socioeconomic status, poor literacy, and lack of education.
In addition to GDMTs, most of our patients require diuretic management. Many patients are on a single dosing of diuretics but, more often than not, our patients are educated about diuretic titration for fluid volume overload. We educate our patients so they have the autonomy to manage and titrate their diuretic dosing which reduces an enormous strain to the nurses and office staff by decreasing calls to the clinic to speak with their NP. Patients are educated to weigh themselves daily and for a weight gain of 1.4 kg (3 pounds) or a change in NYHA functional class, use what we call their “action plan” or an extra dose of diuretic until their weight and/or symptoms return to baseline. However, patients know to call into the clinic if their “action plan” does not resolve their symptoms or make a difference in their weight. At that time, patients can be triaged over the phone and if needed an office appointment can be made on a more urgent basis hopefully diverting an admission [14•].
Medication adherence can also be a challenge for various reasons. NPs and the HF team spend a laborious amount of time reinforcing the importance of adherence. Reasons for low adherence are complex. They can range from treatment-related concerns for hypotension, more than once a day dosing, high out of pocket costs, bothersome side effects, and lack of understanding of the highly efficacious and life prolonging values of these pharmacologic therapies [15]. In addition, titrating GDMT medications to optimal doses along with flexible diuretic dosing can be overwhelming and daunting for patients. Despite all of this, assessing a patient’s ability to manage the disease remains difficult [14•]. “Compliance rates vary widely in even the best clinical trials, implying that, in real world clinical settings with unscreened patients, compliance rates are likely even lower” [14•].
NP Management of Chronic Disease and Comorbidities
Managing HF is not as simple as just managing the diagnosis of HFrEF versus HFpEF. If we only focused on the primary diagnosis and did not consider underlying comorbid factors, we may not address conditions that contribute to HF or pursue treatment options appropriate for that patient [14•].
Treating underlying chronic conditions is extremely important in the HF treatment plan. There is a myriad of underlying chronic conditions that could potentially cause or worsen HF. These include, but are not limited to hypertension, hyperlipidemia, obstructive sleep apnea, diabetes, obesity, physical inactivity, frailty, coronary artery disease, myocardial infarction, valvular heart disease, familial or genetic cardiomyopathies, peripartum cardiomyopathy, tobacco abuse, amyloidosis, cardiotoxicity with cancer or other treatments or substance abuse such as alcohol, cocaine, or methamphetamine, anemia, and iron overload.
NPs are involved in every aspect of chronic disease management. They diagnose, provide early anticipatory guidance, and coordinate care to monitor for disease progression. They also manage medications, problem-solve complications such as adverse treatment effects, caregiver fatigue, and reimbursement issues [16] (Fig. 1).
NPs play a key role in addressing and educating about behavioral risk factors that may prevent most chronic conditions. As a result, patients can learn to make better decisions that will improve their health. NPs have the clinical experience and a holistic understanding of patient well-being to provide guidance [12].
NPs are capable of facilitating and enhancing many facets in the lives of patients suffering from chronic illnesses [16]. Virani and colleagues compared the effectiveness and quality of outpatient cardiovascular disease and diabetes care delivery between advanced practice providers and physician providers in primary care and found clinically insignificant differences in care [17].
“NPs are caring for Medicare beneficiaries with complex needs at rates that match or exceed their physician colleagues. In 2017, 28.9% of Medicare beneficiaries had at least 1 visit with a NP, up from 17.1% in 2012” [18••]. NPs frequently manage more clinically and socially complex Medicare beneficiaries with a higher number of hierarchical condition categories (HCCs). This means that the beneficiaries had > 3 chronic conditions. NPs can be influential in developing new team-based care delivery systems. They are ideal to lead with this endeavor as they are experienced in caring for patients with multivariable comorbidities utilizing innovative resources [18••] (Table 1).
HF Chronic Disease Management Program
NPs’ attributes, training, and experience with managing patients and family systems position them to lead disease management programs. They bring a multifaceted approach to the complex needs of the HF patients managing multiple comorbidities all the while inspiring the patient to participate and cooperate in learning the survival skills of HF self-care management [11]. There are multiple components in a dynamic program including (1) an NP-directed chronic HF clinic, (2) a hospital to home transitional care program (TOC), (3) a guide directed medical therapy (GDMT) program, (4) remote monitoring devices, (5) telehealth opportunities, and (6) clinical research trials. NPs are integral in understanding the application of these components and have provided benefits to patients and healthcare systems with their overall impact on quality and cost savings [19]. The challenge in sustaining these programs is to document the revenue generation from such a program. Unfortunately, much of the service provided in the TOC and GDMT program is non-billable or is modest in revenue compared to staffing costs. At this time, achieving a decrease in readmission rates or length of stay is often used as the measurable outcome of success.
NP Directed Clinics
This type of clinic provides patient-centered, effective, and safe care that is evidence-based. This is the perfect venue for seeing patients referred for a myriad of reasons. The NP clinic typically will manage the HF hospital discharge follow-up visits or the frequent-flier patient with multiple readmissions who may need weekly clinic visits for closer monitoring. Patients seen in the emergency room for a short course of IV diuretics should be seen in this clinic for follow-up within 72 h. Also, other providers in primary care or cardiology services who have patients struggling with volume overload could be referred for diuretic management and support with their education and self-care management. Use of bolus IV diuretics and infusion protocols are used in many clinics. This clinic is also an ideal setting for intermittent visits for those in an active GDMT titration process. NPs have exemplary skills with care coordination in the clinic as they facilitate care with primary providers and layers of specialists. While there are studies showing positive quality outcomes of NP care that are comparable to that of physicians in primary care clinics–there is limited documentation on outcomes of NPs leading HF clinics [20].
Transitions of Care Program
These programs are designed to transition patients from hospital to home when their risk for decompensation is the highest. The program begins with intensive inpatient education and review of factors that may place them at risk for readmission. This is accomplished by using a multidisciplinary team. Discharge preparation begins with clearly communicated instructions, reconciled medication list, and outpatient plan of care including a 7-day discharge follow-up visit. Some programs utilize RNs who continue with phone assessment in the outpatient setting. This is done to monitor for evolving symptoms, continue education, and assist with assessing responses to GDMT. The program lasts approximately 4–6 weeks after discharge with the goal of reducing 30-day hospital readmission rates [21]. Historically, many of these RN-based programs were directed through home health agencies or the discharging hospital. These programs monitor daily weight, blood pressures, and pulse oximetry through technology and contact patients for symptom assessment or for any concerning parameters. Based on the data received, the patient may be directed to contact their PCP or be seen in the emergency department. While in theory, these programs should have utility, the research findings have been mixed. Two of the larger trials noted that there was no significant reduction in hospital readmissions when offering these programs [21, 22]. One reason may be that when RNs counsel patients to seek further help, the patient may not follow recommendations. Possibly the provider does not act quickly or appropriately so there is no real-time treatment. In a TOC program where an NP is embedded, the data can be reviewed directly and treatment decisions can now be real-time. Other resources such as home and telehealth visits by NPs may add benefit and improve outcomes as we know that NPs have positive impact in complex outpatient/community-based management [23]. This deserves further study. Despite these mixed reviews, TOC programs are a level1 recommendation in the 2022 AHA/ACC/HFSA guidelines. Additionally, participation in benchmark programs such as the Get with the Guidelines program through the American Heart Association or even quality benchmarks with insurance partners is a 2b recommendation. These programs outline targets for institutions to achieve based on a quality review process and are expected to produce positive outcomes for patients and institutions [24].
GDMT Program
Multiple scientific trials expound the benefits of optimizing medical therapy for improved mortality, decreased hospitalizations, and improved QOL of HF patients. In the CHAMP-HF registry trial, they noted that a predominance of HF patients eligible for medical therapy did not receive ongoing titration to achieve target doses of appropriate medications, even when there were no contraindications to therapy [25]. There are various possible explanations for this such as patient adherence, cost prohibition, provider knowledge, and time constraints on providers for the monitoring required with adjustments. Some GDMT programs utilize a process with RN telephone management directed by written practice algorithms in between provider visits to assist with titration of medications. The use of an NP-pharmacist dyad to intersperse telephone assessments by the pharmacist with face-to-face clinic visits by the NP in the chronic HF clinic looks promising as well [26]. The IMPROVE-HF trial reviewed GDMT of patients with reduced LVEF and found that “use of ‘scalable practice-specific performance improvement intervention’ correlated with improvement in application of GDMT in this subgroup of HF patients” [27].
Remote Cardiac Monitoring Devices
The use of remote cardiac monitoring (RCM) appears to be the wave of the future although its foundation goes back 1905 with the first transmission of ECG tracings via telephone. The data from these devices should allow for detection of early trends of decompensation to allow proactive treatment and avoidance of a hospitalization. This is paramount as repeat hospitalizations correlates with an increase in HF mortality [28]. In addition, the data can guide medication optimization. There are multiple modes of monitoring that provide different physiologic measurements derived from (1) weights and home measurements, (2) thoracic impedance, (3) pulmonary artery pressures, and (4) multiple sensors in CRT devices. The devices gathering the data may be implantable or wearable technologies. With the emergence of telehealth visits during the COVID-19 pandemic, a new paradigm developed coupling remote clinic visits with RCM measurements that may result in healthcare benefits. The evidence is only anecdotal at this time and its continuation will depend on the reimbursement direction for telehealth visits [29]. Enhancements to this technology, dynamic prescription of medical therapies such as diuretic sliding scales may be programmed into patient devices for self-adjustment and treatment parameters, yet advancing self-care management. Does any of this reduce costs? Many systematic reviews have tried to answer this question and while there are perceived benefits to reducing hospitalizations and improving self-care, the evidence is lacking on cost effectiveness [30].
Telehealth Visits
Telehealth visits were not routine before the COVID-19 pandemic. Reimbursement for this service from government and private payers was poor or non-existent. All of that changed in 2020. According to ACC President, Dipti Itchaporia, “Applied artificial intelligence and digital technology advances are sweeping the health care community and these advances, coupled with other health care technologies, will only continue to be developed at an ever-increasing pace” [31]. That pace was accelerated during the pandemic when virtual visits became an overnight reality in order to continue to provide care to a patient community now quarantined in their homes. One large study of 7000 patients in an academic facility found that discharge follow-up continued to occur in person but with the addition of tele-heath visits. The study results noted that both of these types of hospital discharge visits within 14 days were associated with a lower rate of readmissions than those with late or no follow-up [32].
Clinical Research Trials
Many patients are not aware of the options to participate in a clinical research trial. NPs who work in institutions with clinical research centers have a responsibility to be aware of current trials and discuss these options with their patients, especially if treatment plans are limited or if a beneficial response to GDMT is lacking. Even when a patient is responding as expected with a current therapy, some want to participate in advancing the science of HF. If there is presently no treatment for their HF, then participating in clinical trials allows the patient to be part of new treatment options that may in turn be life altering. Patients with concerns of unknown risk can still participate in a control group in a non-randomized trial and feel a sense of purpose (Fig. 1).
NP Role in Advanced HF Therapies
Even with the best clinical management, HF will often progress to advanced HF. The AHA estimates that of the over 6 million patients with HF, approximately 5% per year will progress to stage D heart failure [33]. Kalogeropoulos et al. (2017) reviewed records of one academic system’s HF program and found that over the course of 3 years, 1 in 8 patients with Stage C HF will progress to stage D HF. Furthermore, 1 in 4 patients had either progressed to stage D HF or died [34]. This information emphasizes the importance of identifying patients with advanced HF early to refer them for advanced therapies such as heart transplant or left ventricular assist device (LVAD).
NPs managing chronic HF patients are in the perfect position to identify when patients are starting to deteriorate and may benefit from advanced therapies. Baumwol (2017) identified that there are often signs that it is time to discuss advanced therapies. [35] The NP may be the first to notice that patients are having less response to diuretics or that GDMT is being down-titrated due to intolerance. Also, NPs can pick up quickly on end organ dysfunction secondary to advanced HF. These changes can be subtle and overlooked unless a skilled HF NP with a longitudinal relationship with the patient is watching closely.
In terms of advanced therapies, there is a process to evaluate patients to determine candidacy for cardiac transplant or LVAD. The process includes extensive history taking, clinical testing, and consultation with a multidisciplinary team. The NP role is fitting to meet the needs of this process as a referral and evaluation coordinator. They are trained to gather and interpret information and data in a holistic manner, which is paramount when considering the complexity of advanced therapies. This information is presented to a multidisciplinary team who then as a whole determines candidacy. The decisions made regarding candidacy are dependent on the completeness of the information presented to the team to ensure that the decision to move forward is one that will ultimately improve the patient’s quality of life.
The care for cardiac transplant and LVAD patients is highly specialized. NPs can attain the training necessary to navigate the details of this specialized care, all the while using their holistic training to incorporate all aspects of their healthcare.
Transplant patients are dependent upon immunosuppression for the survival of the cardiac graft. These medications require close monitoring for therapeutic levels and drug interactions. There is a delicate balance between immunosuppression and opportunistic infections. Watching for subtle signs of rejection adds another layer of complexity to long-term management. Additionally, there are chronic concerns such as osteoporosis due to corticosteroid use and renal and liver dysfunction as a secondary effect of the medications. NPs are well-equipped to manage all of these aspects of post-transplant care, all the while incorporating preventive care such as management of hypertension and hyperlipidemia.
LVAD patients have a different set of challenges in that there are common adverse events to address. Examples of these common adverse events are driveline infections, gastrointestinal bleeding, pump thrombosis, and stroke, just to name a few [36]. The rates of these complications have decreased in recent years with improved technology and prevention strategies. Interventions such as tight blood pressure and anticoagulation control are imperative in prevention of stroke and pump thrombosis. Restarting GDMT after implant and prescribing omega-3 fatty acids have been shown to decrease incidence of gastrointestinal bleeding. The best prevention of driveline infection is strict adherence to driveline site care which requires extensive teaching and reinforcement. In the event that a driveline infection occurs, early identification and treatment with antibiotics is life-saving. Again, NPs become specialists in managing LVAD challenges, but it is important to note that part of their success in the management of these patients lies in the relationships the NPs build with them. There is a clear partnership between the NP and the LVAD patient to improve quality of life. Furthermore, NPs often recognize when advanced therapies are no longer improving quality of life but are simply prolonging it.
NP Advocacy and Quality of Life
Quality of life (QOL) is impacted by chronic disease. HF is a chronic and progressive disease. Treatment for HF should aim to maintain the best QOL for as long as possible. QOL interventions may be specific to an individual patient and care should be patient-centered. However, in general, “the symptoms and functional severity of heart failure, medical comorbidities, and levels of anxiety and depression” appear to be among the strongest predictors of QOL in HF patients [37]. NPs are uniquely equipped to assess, treat, counsel, and coordinate care for HF patients to promote a patient’s best QOL at every stage of disease.
Providing the most comprehensive and holistic care to HF patients includes knowledge of evidence-based strategies for disease management, but it also includes timely referral for palliative care (PC) and hospice care (HC). Advance HF therapies, including medication, surgery, and mechanical circulatory support (MCS) devices which primarily aim to prolong life, do not always translate into long-term or significant relief of suffering from HF. In fact, advanced therapies like implantable cardioverter defibrillators (ICD) and left ventricular assist devices (LVADs) can significantly increase psychological distress for patients and their families [38,39,40].
The AHA definition of palliative care is “patient-and family-centered care that optimizes health-related quality of life (HRQOL) by anticipating, preventing, and treating suffering” [41]. Palliative care interventions in several RCTs were associated with the following positive outcomes: reduction in HF readmissions [42, 43], improvement in symptoms [43, 44], and improvement in NYHA class [42], also improvement in depression, anxiety [44, 45], and overall quality of life scores [42,44,45,45].
NPs ensure timely initiation of concomitant care in the hospital, community, and or home setting for patients with HF when often other providers are uncomfortable having these important serious illness conversations. There are currently no widely accepted tools to help guide timing of a palliative care referral in HF. The trajectory of HF is often difficult to predict. Therefore, timing of referral can be challenging. Barriers noted by AHA include lack of provider training about PC, provider discomfort with advanced disease or end of life conversations, reimbursement issues, and family dynamics, culture, religion, and language barriers [41]. NPs are skilled at recognizing a decline in QOL and initiating the sensitive serious illness conversation. As a result, they are often the first providers to incorporate palliative care into their care plan. PC helps HF NPs with symptom management and defining goals of care. PC offers an integrated approach to caring for individuals with life threatening health conditions, with the focus being the best QOL [46] (Fig. 2). AHA advocates for PC referrals in routine disease care for HF patients [41].
Integrating palliative care across the HF experience. “Core domains of primary palliative care (e.g., symptom assessment and management, psychosocial support, advance care planning) may be seamlessly integrated within usual heart failure (HF) disease and device management. When appropriate, specialty palliative care services may be initiated to address complex or intractable palliative needs. The timing of these referrals should be based on patient need, not prognosis, and can be initiated at any point during the HF trajectory. Given that symptoms, functional status, and quality of life are not perfectly correlated, it is important that palliative needs such as symptoms and quality of life be routinely and systematically monitored throughout the patient’s HF care trajectory” [46]. (Reprinted from: Kavalieratos D, et al. J Am Coll Cardiol. 2017 Oct 10;70(15):1919–1930, with permission from Elsevier) [46]
Palliative care is separate from hospice care, but both are a crucial part of the continuum of disease management. HC is initiated when life expectancy is 6 months or less. HC continues a focus on symptom management, care coordination, and family support. HC often allows patients to die at home. HC eases suffering for a patient at the end of life and eases burdens for families. However, like PC, HC is also still widely underutilized for patients dying with HF. (14) NPs can take the lead in facilitating quality end-of-life care for the HF patient and their families.
The Impact of the COVID-19 Pandemic on HF NPs
The COVID-19 pandemic was like an avalanche when it first hit the world in March of 2020.
The challenges for NPs in the HF clinic were numerous and evolved as the world learned more about the virus. Early in the pandemic, the federal government loosened practice restrictions on NPs to maximize the availability of clinicians to treat patients during the COVID-19 pandemic [47]. NP clinical time was expanded and talents were capitalized upon during this time of need.
NPs quickly initiated COVID-19 telehealth screening clinics that were offered to their communities while maintaining the HF clinic. There were challenges in getting patients to the clinic either because they had been infected by the virus or were afraid to leave their homes due to the virus. To accommodate patients, NPs started utilizing telehealth. “The COVID-19 pandemic was associated with about 67% decline in the total number of outpatient visits per provider by the week of April 12-18th 2020, relative to the same week in prior years.” [48]. The need for HF care did not go away but switched over to telephone or telehealth visits.
NPs were tasked to educate all patients about social distancing and isolating and once vaccines became available, the need to educate them regarding the importance of vaccination emerged. This was initially not a problem as the country had a deep fear of the getting the virus. However, over time misinformation became widespread and the use of vaccines became highly politicized. Bizarre and worrisome tales were spread quickly via social media and other outlets, which created a sense of distrust and worry in the public. Ultimately, this led to more patients declining to be vaccinated. A great deal of time was spent educating HF patients as to the importance of the COVID-19 vaccine, discrediting misinformation and alleviating concerns.
In the beginning, NPs were also administering vaccinations, given the enormous amount of the population requiring the COVID-19 vaccine. This required competency training on vaccine administration, as well as developing policies and procedure specifically related to the COVID-19 vaccine. Elements such as screening for contraindications and precautions, educating the patient, preparing, administering the vaccine, and documenting the vaccination all became important as the healthcare team strived to move towards immunity (https://www.cdc.gov/vaccines/hcp/admin/admin-protocols.html).
None of this came without a cost to the healthcare providers. “According to the American College of Cardiology Survey, The COVID-19 pandemic has taken a significant toll on cardiovascular clinicians, many of whom provide direct care to patients with or at greater risk of the virus. As a result, the prevalence of burnout among cardiovascular professionals nearly doubled when comparing pre- to peak COVID-19 levels” [49]. Among all cardiovascular clinicians, including NPs, half provided direct care to patients with COVID-19, but only one of five reported not having adequate personal protective equipment. In addition, plans to reduce clinical hours in the next year, leave their current practice, or early retirement were reported [49].
Fortunately, we have come a long way since the early days of COVID-19 now with safe vaccines and antiviral treatments. NPs play a role in screening and limiting treatment delays utilizing telehealth and new treatment options especially for our high-risk patients with a positive COVID-19 test. NPs will continue to be in the forefront of disseminating the latest clinical developments for COVID-19 into the endemic.
Conclusions
HF is one of the most challenging chronic conditions to manage. NPs are equipped to handle these challenges. NPs are able to navigate and collaborate with a multidisciplinary team to assure the best treatment for their patients. It takes a village. We need to partner with our community and agencies to increase access to care, education, screenings, and healthy food options. “There is a huge need for HF clinicians to lead building new programs or joining existing ones… it takes a different type of grind and perseverance to get programs up and running from ground zero” [1]. While HF patients can be challenging and demanding, NPs have unique abilities to care for these patients and take pride in seeing that these patients get the best HF care.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sauer AJ, Bhardw AJ, Srivastava AV. On leadership-a call to action for aspirational leadership development for programs supporting patients with heart failure. J Card Fail. 2021;27(9):1017–9.
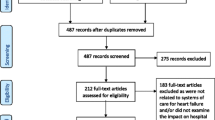
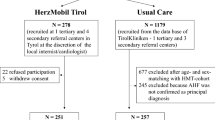
Driscoll A, Gao L, Watts JJ. Clinical effectiveness and cost-effectiveness of ambulatory heart failure nurse-led services: an integrated review. BMC Cardiovasc Disord. 2022;22:64. https://doi.org/10.1186/s12872-022-02509-9.
Virani SS, Alonso A, Benjamin E, et al. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Committee. Heart disease and stroke statistics -2020 update: A report from the American Heart Association. Circulation. 2020;141:e139-596.
Nadar SK, Shaikh MM. Biomarkers in routine heart failure clinical care. Card Fail Rev. 2019;5(1):50–6.
Feng Z, Akinrimisi OP, Gornbein JA, et al. Combination biomarkers for risk stratification in patients with chronic heart failure biomarkers prognostication in HF. J Cardiac Fail. 2021;27(12):1321–7.
Bozkurt B, Coats AJ, Tsutsui H, et al. Consensus statement universal definition and classification of heart failure: a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure Endorsed by Canadian Heart Failure Society, Heart Failure Association of India, the Cardiac Society of Australia and New Zealand, and the Chinese Heart Failure Association. J Cardiac Fail. 2021;27:387–413.
Beck DL. Multisociety consensus statement offers updated terminology for HF. Cardiology. 2021;50(6):22–3.
Heidenreich PA, Bozkurt B, Aguiar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2022;1(45):e1–138. https://doi.org/10.1161/CIR.0000000000001063.
Califf RM. The ecosystem to support people with heart failure. J Cardiac Fail. 2022;28(4):650–8.
Adams J, Grundy P, Kohn MS, et al. Patient-centered medical home. What, why, and how? Healthc Life Sci. 2009;1–32. www.semanticscholar.org/paper/Patient-centered-medical-home-What-%2C-why-and-how-Adams-Grundy/8f076ca73c026e677c23c3cde2c1e978be2013d6.
Edmunds MW. NPs and the management of chronic disease. J Nurse Pract. 2012. https://doi.org/10.1016/j.nurpra.2011.12.005.
AANP. Nurse practitioner cost effectiveness. Am Assoc Nurse Pract. 2013.
Dunlap M. I’ve had a good run. J Cardiac Fail. 2021;27(11):1290.
• Eisen HJ, Freeman R, Prutkin JM, et al. Clinics review articles. Cardiol Clin Heart Fail. 2014;32(1):170. www.cardiology.theclinics.com. Accessed 9 June, 2022. This resource outlines the role of the NP in a collegial approach with a multidisciplinary team for the care delivery of HF patients in order to prevent hospitalizations.
Bhatt AS. Adherence to evidence-based therapies in heart failure Deepening the implementation divide. J Am Coll Cardiol. 2021;9(12):887–9.
APRNs in chronic illness care. Nurse Key. 2016. https://nursekey.com/aprns-in-chronic-illness-care/. Accessed 9 June, 2022.
Virani SS, Akeroyd JM, Ramsey DJ, et al. Comparative effectiveness of outpatient cardiovascular disease and diabetes care delivery between advanced practice providers and physician providers in primary care: implications for care under the Affordable Care Act. Am Heart J. 2016;181:74–8.
•• Fraze TK, Briggs ADM, Whitcomb EK, et al. Role of nurse practitioners in caring for patients with complex health needs. Medical Care 2020;58(10):853–860. https://doi.org/10.1097/MLR.0000000000001364. Findings from this observation study suggest that NPs care for complex patients with multiple chronic conditions at a rate that is the same or higher than their physician colleagues.
Driscoll A, Gao L, Watts JJ. Clinical effectiveness and cost-effectiveness of ambulatory heart failure nurse-led services: an integrated review. BMC Cardiovasc Disord. 2022;22(1):64. Published 2022 Feb 22. https://doi.org/10.1186/s12872-022-02509-9.
Virani SS, Akeroyd JM, Ramsey DJ, et al. Comparative effectiveness of outpatient cardiovascular disease and diabetes care delivery between advanced practice providers and physician providers in primary care: implications for care under the Affordable Care Act. Am Heart J. 2016;181:74–82. https://doi.org/10.1016/j.ahj.2016.07.020.
Albert NM. A systematic review of transitional-care strategies to reduce rehospitalization in patients with heart failure. Heart Lung. 2016;45(2):100–13. https://doi.org/10.1016/j.hrtlng.2015.12.001.
Ong MK, Romano PS, Edgington S, et al. Effectiveness of remote patient monitoring after discharge of hospitalized patients with heart failure: the Better Effectiveness After Transition -- Heart Failure (BEAT-HF) randomized clinical trial [published correction appears in JAMA Intern Med. 2016 Apr;176(4):568] [published correction appears in JAMA Intern Med. 2016 Jun 1;176(6):871]. JAMA Intern Med. 2016;176(3):310–318. https://doi.org/10.1001/jamainternmed.2015.7712.
Ledwin KM, Lorenz R. The impact of nurse-led community-based models of care on hospital admission rates in heart failure patients: an integrative review. Heart Lung. 2021;50(5):685–92. https://doi.org/10.1016/j.hrtlng.2021.03.079.
Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(18):e876–94. https://doi.org/10.1161/CIR.0000000000001062.
Greene SJ, Fonarow GC, DeVore AD, Sharma PP, Vaduganathan M, Albert NM, Duffy CI, Hill CL, McCague K, Patterson JH, Spertus JA, Thomas L, Williams FB, Hernandez AF, Butler J. Titration of medical therapy for heart failure with reduced ejection fraction. J Am Coll Cardiol. 2019;73(19):2365–83. https://doi.org/10.1016/j.jacc.2019.02.015.
Shah SP, Dixit NM, Mendoza K, et al. Integration of clinical pharmacists into a heart failure clinic within a safety-net hospital. J Am Pharm Assoc (2003). 2022;62(2):575-579.e2. https://doi.org/10.1016/j.japh.2021.11.012.
Fonarow GC, Albert NM, Curtis AB, et al. Improving evidence-based care for heart failure in outpatient cardiology practices: primary results of the Registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE HF). Circulation. 2010;122(6):585–96. https://doi.org/10.1161/CIRCULATIONAHA.109.934471.
Kennel PJ, Rosenblum H, Axsom KM, et al. Remote cardiac monitoring in patients with heart failure: a review. JAMA Cardiol. 2022;7(5):556–64. https://doi.org/10.1001/jamacardio.2021.5090.
Mohebali D, Kittleson MM. Remote monitoring in heart failure: current and emerging technologies in the context of the pandemic. Heart. 2021;107(5):366–72. https://doi.org/10.1136/heartjnl-2020-318062.
Eurlings CGMJ, Boyne JJ, de Boer RA, Brunner-La Rocca HP. Telemedicine in heart failure-more than nice to have? Neth Heart J. 2019;27(1):5–15. https://doi.org/10.1007/s12471-018-1202-5.
Itchhaporia D. Optimizing remote monitoring. The Pulse of ACC-American College of Cardiology. 2021:50(12):6.
Xu H, Granger BB, Drake CD, Peterson ED, Dupre ME. Effectiveness of telemedicine visits in reducing 30-day readmissions among patients with heart failure during the COVID-19 pandemic. J Am Heart Assoc. 2022;11(7): e023935. https://doi.org/10.1161/JAHA.121.023935.
Morris AA, Khazanie P, Drazner MH, et al. Guidance for timely and appropriate referral of patients with advanced heart failure: a scientific statement from the American Heart Association. Circulation. 2021;144(15):e238–50. https://doi.org/10.1161/CIR.0000000000001016.
Kalogeropoulos AP, Samman-Tahhan A, Hedley JS, et al. Progression to stage D heart failure among outpatients with stage C heart failure and reduced ejection fraction. JACC Heart Fail. 2017;5:528–37. https://doi.org/10.1016/j.jchf.2017.02.020.
Baumwol J. “I Need Help”-a mnemonic to aid timely referral in advanced heart failure. J Heart Lung Transplant. 2017;36(5):593–4. https://doi.org/10.1016/j.healun.2017.02.010.
Mehra MR, Cleveland JC Jr, Uriel N, et al. Primary results of long-term outcomes in the MOMENTUM 3 pivotal trial and continued access protocol study phase: a study of 2200 HeartMate 3 left ventricular assist device implants. Eur J Heart Fail. 2021;23(8):1392–400. https://doi.org/10.1002/ejhf.2211.
Freedland KE, Rich MW, Carney RM. Improving quality of life in heart failure. Curr Cardiol Rep. 2021;23(11):159. Published 2021 Oct 1. https://doi.org/10.1007/s11886-021-01588-y.
Van Den Broek KC, Heijmans N, Van Assen MA. Anxiety and depression in patients with an implantable cardioverter defibrillator and their partners: a longitudinal study. Pacing Clin Electrophysiol. 2013;36(3):362–71. https://doi.org/10.1111/pace.12055.
Modica M, Minotti A, De Maria R, et al. Coping, mood, quality of life, and outcomes in recipients of left ventricular assist devices: a cluster analysis. Psychosom Med. 2019;81(2):192–9. https://doi.org/10.1097/PSY.0000000000000658.
Waldenburger N, Steinecke M, Peters L, Jünemann F, Bara C, Zimmermann T. Depression, anxiety, fear of progression, and emotional arousal in couples after left ventricular assist device implantation. ESC Heart Fail. 2020;7(5):3022–8. https://doi.org/10.1002/ehf2.12927.
Braun LT, Grady KL, Kutner JS, et al. Palliative care and cardiovascular disease and stroke: a policy statement from the American Heart Association/American Stroke Association. Circulation. 2016;134(11):e198–e225. https://doi.org/10.1161/CIR.0000000000000438.
Brännström M, Boman K. Effects of person-centered and integrated chronic heart failure and palliative home care. PREFER: a randomized controlled study. Eur J Heart Fail. 2014;16(10):1142–51. https://doi.org/10.1002/ejhf.151.
Wong FK, Ng AY, Lee PH, et al. Effects of a transitional palliative care model on patients with end-stage heart failure: a randomized controlled trial. Heart. 2016;102(14):1100–8. https://doi.org/10.1136/heartjnl-2015-308638.
Sidebottom AC, Jorgenson A, Richards H, Kirven J, Sillah A. Inpatient palliative care for patients with acute heart failure: outcomes from a randomized trial. J Palliat Med. 2015;18(2):134–42. https://doi.org/10.1089/jpm.2014.0192.
Rogers JG, Patel CB, Mentz RJ, et al. Palliative care in heart failure: the PAL-HF randomized, controlled clinical trial. J Am Coll Cardiol. 2017;70(3):331–41. https://doi.org/10.1016/j.jacc.2017.05.030.
Kavalieratos D, Gelfman LP, Tycon LE, Riegel B, Bekelman DB, Ikejiani DZ, Goldstein N, Kimmel SE, Bakitas MA, Arnold RM. Palliative care in heart failure: rationale, evidence, and future priorities. J Am Coll Cardiol. 2017;70(15):1919–30. https://doi.org/10.1016/j.jacc.2017.08.036.
Zolot J. COVID-19 brings changes to NP scope of practice. AJN, Am J Nurs. 2020;120(8):14. https://doi.org/10.1097/01.NAJ.0000694516.02685.29.
Chatterji P, Li Y. Effects of the COVID-19 pandemic on outpatient providers in the United States. Med Care. 2021;59(1):58–61. https://doi.org/10.1097/MLR.0000000000001448.
Mehta LS. ACC survey: burnout rates double for cardiology clinicians amid COVID-19. Cardiology: A Member Publication of the American College of Cardiology. 2021;50(6).
Acknowledgements
The authors would like to acknowledge Mickenzie McLucas for developing Fig. 1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Kathaleen King-Dailey reports: Vice-President of Nurse Practitioners of Central Pennsylvania, Communications Committee member for the American Association of Heart Failure Nurses, and for the Pennsylvania Coalition of Nurse Practitioners. Suzanne Frazier reports: President – NPs of Central PA (a regional group of the Pennsylvania Coalition of Nurse Practitioners). The other authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Heart Failure
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
King-Dailey, K., Frazier, S., Bressler, S. et al. The Role of Nurse Practitioners in the Management of Heart Failure Patients and Programs. Curr Cardiol Rep 24, 1945–1956 (2022). https://doi.org/10.1007/s11886-022-01796-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-022-01796-0