Abstract
Purpose of Review
This review aims to summarize the epidemiology, current pathophysiologic understanding, and state-of-the-art treatment of venous thromboembolism (VTE) in cancer patients.
Recent Findings
The risk of VTE varies among cancer patients. Recently introduced prediction models better identify those at high risk of VTE. New mechanisms underlying hypercoagulability in cancer have been uncovered. Initial data on the efficacy of direct oral anticoagulants (DOACs) compared with low-molecular weight heparin to treat VTE in patients with cancer are promising. However, they may be associated with higher risk of gastrointestinal bleeding.
Summary
VTE causes significant morbidity and mortality in cancer patients. Our understanding of the mechanisms of VTE, including those associated with cancer treatments, has significantly grown. The assessment of the benefit/risk balance of VTE treatment remains challenging in many patients with cancer. The introduction of DOACs has expanded treatment options, but knowledge on their efficacy and safety is incomplete.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Virchow’s triad of hypercoagulability, blood stasis, and endothelial injury underpins our basic understanding of the mechanisms of venous thrombosis, and cancer is often associated with the presence of these three risk factors. The association of cancer and thrombosis was first made famous by Armand Trousseau in the 1860s [1], when he described multiple cancer patients who presented with phlegmasia alba dolens (the Latin words for painful white inflammation) caused by deep vein thrombosis (DVT) of the leg, as well as with migratory thrombophlebitis, for which his eponymous, and famously self-diagnosed, syndrome is named. A large body of subsequent literature has confirmed the link between venous thromboembolism (VTE) and cancer and has highlighted the worse prognosis, distinct pathophysiologic mechanisms, and need for different approaches to prophylaxis and treatment. This review will discuss the epidemiology, mechanisms, and current management of cancer-associated VTE.
Epidemiology and Risk Stratification
A significant proportion of VTE events occur in patients with a diagnosis of cancer [2•]. In the largest registry, the Registro Informatizado de Enfermedad TromboEmbólica (RIETE), cancer that was newly diagnosed or actively being treated was reported in 17% (n = 6075) of 35,359 patients with VTE [3]. In an analysis of 1897 incident cases of VTE in the Worcester, MA, metropolitan area, 20.9% had a diagnosis of active malignancy [4]. Overall, the risk of VTE appears to increase 4- to 7-fold in cancer patients [5, 6]. The absolute risk of VTE in cancer patients varies from 0.5 to 20% depending on the cancer type, stage of disease, and other patient-associated risk factors [7]. The risk is highest in patients who are receiving chemotherapy or are admitted to the hospital and/or undergoing surgery. These patients have a higher chance of infection, anemia, immobility, and renal and pulmonary disease, all of which increase VTE risk.
Cancer location and histologic subtype play a significant part in determining the risk of VTE. Brain and pancreatic malignancies appear to consistently be associated with the highest risk of thromboembolism, with stomach and other digestive cancers (e.g., esophageal, biliary), ovarian, bone, kidney, and lung adenocarcinoma also conferring high risk [7,8,9]. Apart from prostate cancer, regional or metastatic spread is associated with a 1.5- to 4-fold and 1.5- to 22-fold increase in the risk of VTE, respectively, compared to localized disease, depending on the histologic type [10]. In patients presenting with concurrent VTE at the time of cancer diagnosis, approximately 50% have metastatic disease [10, 11]. The risk of VTE is also elevated in all hematologic malignancies, with the exception of indolent lymphomas, and is highest in aggressive non-Hodgkin lymphomas and multiple myeloma [12, 13]. Although at a lower relative risk, most thrombotic events are encountered in patients with breast, lung, colon, and prostate cancer given the higher overall prevalence of these malignancies [8]. Patients are at the highest risk for VTE within 3 months of their initial cancer diagnosis [6, 7]. More advanced, metastatic, and aggressive malignancies that are associated with a low annual survival rate are also at the highest risk for thromboembolism [2•].
Risk prediction models have been developed and validated to determine which cancer patients are higher risk for VTE. The Khorana score incorporates five predictive variables designed to be assessed before the initiation of chemotherapy and assigns one point to each (Table 1) [14•]. Rates of VTE in the highest risk group with ≥ 3 points were 7.1 and 6.7% in the development and validation cohort, respectively. The Khorana score has been validated in a more heterogeneous population of cancer patients who were not necessarily undergoing chemotherapy, and its predictive power is further enhanced by the addition of d-dimer and soluble P-selectin measurements as biomarkers [15]. A more recently developed clinical prediction model incorporates only two variables: tumor-site risk (low-intermediate, high, and very high) plus continuous d-dimer measurements and could outperform previous risk calculators for predicting the development of VTE [16]. These prediction scores can be used to increase awareness of the risk of VTE in cancer patients and providers with the goal to reduce time to diagnosis and treatment. In addition, screening for VTE in high risk cancer patients may have some clinical utility, as venous ultrasound prior to chemotherapy detected occult DVT in 9% of patients with Khorana score ≥ 3 in a small single-center study of 35 patients [17].
Presentation
Compared to patients without cancer, malignancy-associated VTE is more likely to present with a higher thrombus burden and/or development of thrombosis at atypical sites [18]. Patients are more likely to present with bilateral lower extremity DVT, iliocaval DVT, Budd-Chiari, syndrome, extrahepatic portal or mesenteric vein thrombosis, or upper extremity thrombosis even in the absence of an indwelling venous device [18, 19]. Therefore, de novo presentation of VTE at an atypical location should increase the suspicion for occult malignancy.
Prognosis
Development of VTE during cancer is associated with a poor prognosis and greater healthcare utilization and costs [2•]. Patients with cancer who develop VTE fare worse than those who do not develop thrombosis, and patients with VTE who have cancer have higher mortality than those with VTE who do not have cancer. In an analysis of the RIETE registry, among 35,539 patients with VTE, cancer was present in 6075 patients and was the strongest risk factor for all-cause and pulmonary embolism (PE)-related mortality, increasing risk approximately 3-fold [3]. In an analysis of over 235,000 patients from the California Cancer Registry, diagnosis of VTE at the time of, or within 1 year of cancer diagnosis was a significant predictor of death, independent of age, race, and stage of cancer, with a median overall relative risk of 3.7 [10]. Similarly, a large retrospective Danish cohort study demonstrated that the 1-year survival of patients with VTE and cancer was 12% compared to 36% in cancer patients without VTE [11]. The poor prognosis associated with malignancy-related VTE is mostly related to the more aggressive cancers present in these patients. However, among patients with cancer, VTE-related death may be the second highest cause of mortality after cancer progression itself [20, 21].
Therapeutic anticoagulation in patients with VTE and malignancy is associated with increased risk for both VTE recurrence and major bleeding compared to those with VTE without cancer [21,22,23]. Over a 12-month treatment period with anticoagulation, recurrent VTE occurred in 20.7% of cancer patients, compared to only 6.8% of those without cancer [23]. In an analysis of 3805 patients with VTE and cancer in the RIETE registry, recurrent PE and DVT occurred in 2.4 and 2.6% of patients within 3 months of VTE diagnosis, respectively, and 44% of patients with recurrent PE died as a result [24]. Age < 65 years and cancer diagnosis within 3 months of VTE presentation were both associated with risk of VTE recurrence. Importantly, 4.1% of patients also experienced major bleeding within 3 months, with fatal bleeding occurring in 29% of patients [24]. Recent bleeding, renal impairment, immobility, and metastasis were independently associated with increased bleeding risk. Indeed, fatal bleeding is also a major cause of death in cancer patients who develop VTE. In a larger analysis from the RIETE registry of > 10,000 patients with cancer-associated VTE, the risk of death from PE is highest in the first month after PE diagnosis, whereas the risk of bleeding remained constant throughout the 12-month cohort analysis, with most cases occurring after the first month. Moreover, in patients presenting with DVT alone, more deaths resulted from bleeding than from fatal PE [21].
A clinical risk prediction tool has been developed to estimate risk of recurrent VTE during the first 6 months in cancer patients treated with anticoagulation. In the Ottawa prognostic score, factors predictive of recurrent VTE were female gender, lung cancer, and previous VTE (+ 1 point each), whereas protective factors included breast cancer (− 1 point) and tumor-nodes-metastasis (TNM) stage I disease (− 2 points). Those with a score ≤ 0 had a 4% risk of recurrence, whereas those with a score ≥ 1 had a 16% recurrence risk [25]. These findings have been validated in other cohorts [26].
Pathophysiology
Extensive research has been aimed at understanding the molecular pathways that underlie the hypercoagulable state of cancer. There is unlikely a unifying mechanism, but instead, a diverse set of pathophysiologic mechanisms has been implicated in various tumor types [27]. This hypercoagulability of cancer may be (1) cell-mediated through leukocytosis and thrombocytosis, (2) microparticle-based through expression of tissue factor and/or phospholipid, or (3) humoral via enhanced expression of circulating inflammatory markers (Fig. 1). These mechanisms are compounded by patient- and treatment-related factors such as immobility and hospitalization, central venous catheters, surgery, radiation therapy, and vascular toxicity of chemotherapeutic agents and adjunctive treatments.
Potential mechanisms of the prothrombotic state of cancer. Different tumors may induce thrombosis via distinctive mechanisms. Not all pathways are relevant in each case of thrombosis. Neutrophil activation can induce release of neutrophil extracellular traps (NETosis), which along with indwelling catheters and DNA release via tumor cell death lead to contact pathway activation of the coagulation cascade. Chemotherapeutic agents and tyrosine kinase inhibitors can activate vascular endothelium to express adhesion molecules such as P-selectin and adopt a prothrombotic phenotype. Thrombocytosis is induced by cytokines from the tumor microenvironment. Tissue factor may be released directly from tumor cells, via PTEN, KRAS, or p53-driven gene expression. Microparticles may be secreted by activated platelets, endothelial cells, leukocytes, and tumor cells that contain tissue factor, adhesion molecules, and negatively charged phospholipid such as phosphatidylserine. Contact pathway activation, FVII activation by tissue factor, and exposure of negatively charged phospholipid all promote thrombin generation. Thrombin cleaves fibrinogen to insoluble fibrin which traps red blood cells and along with aggregated platelets forms a venous thrombosis. FVII factor VII, FIX factor IX, FX factor X, FXI factor XI, FXII factor XII, IL-6 interleukin-6, PS phosphatidylserine, ROS reactive oxygen species, TF tissue factor, TKI tyrosine kinase inhibitor, TPO thrombopoietin, VEGF vascular endothelial growth factor
Leukocytosis is commonly found in non-hematologic cancer and may be a direct result of tumor-generated granulocyte stimulatory factors. Leukocytosis has been associated with the future development of cancer-related VTE [14•, 28]. Neutrophils, as major constituents of the thrombotic milieu, extrude neutrophil extra-cellular traps (NETs), made up of nuclear chromatin studded with granular proteins and proteases, in response to reactive oxygen species that are enriched in the hypoxic and inflammatory tumor microenvironment. NETs promote thrombosis through a variety of mechanisms including direct contact-pathway activation of the coagulation cascade by extracellular DNA, histone-induced endothelial activation, neutrophil elastase inhibition of thrombomodulin, and by providing a scaffold to promote red blood cell and platelet adhesion [29]. Venous thrombi from humans, not necessarily cancer-related, are enriched with leukocytes and contain abundant NETs [30]. Neutrophils from lung and breast cancer animal models are primed to release NETs and promote thrombosis, but a causal role for NETs in cancer thrombosis in humans has not been clearly defined [31]. Thrombocytosis is frequently found in patients with cancer, and its presence is associated with increased risk of VTE [32, 33]. Interleukin-6-induced production of thrombopoietin contributes to paraneoplastic thrombocytosis in ovarian cancer, and its presence is associated with reduced survival [34].
Microparticles (MPs) are cellular fragments 0.1–1 μm in diameter shed from platelets, endothelial cells, leukocytes, from outward blebbing of the plasma membrane. MPs can be enriched for proteins such as tissue factor (TF+) and other adhesion receptors. In addition to these procoagulant proteins, microparticles help initiate thrombosis by providing negatively charged phospholipid, such as phosphatidylserine (PS+), which allows assembly and activation of coagulation cascade enzymes [35]. Although most firmly established with pancreatic cancer, TF + MPs are released from a variety of cancers including brain, lung, ovarian, and gastric tumors, and their presence is associated with increased risk of VTE and reduced survival, especially when tissue factor activity, not just antigen, is measured [36]. The risk of TF + MP production may also increase with the severity of tumor grade and metastatic potential. Before assessment of TF+ or PS + MPs can gain widespread clinical use, assays and measurement protocols need to be standardized and validated. In addition to MP generation, tumor cells may express high levels of tissue factor, either through PTEN, KRAS, or p53-driven gene expression, or via stimulation from the hypoxic tumor microenvironment [37, 38]. Tissue factor may aid in tumor growth and metastasis via platelet activation, which can “cloak” tumor cells to avoid immune detection, and via stimulation of angiogenesis through protease-activated receptor signaling [39]. P-selectin, an adhesion protein expressed on activated platelets and endothelial cells, can promote thrombosis via leukocyte release of procoagulant microparticles and monocyte tissue factor expression. In a population of patients with various cancer types, soluble P-selectin levels above the 75% percentile were associated with a 2.5-fold increased risk of VTE [40].
Overall, the risk of VTE is significantly higher in cancer patients receiving systemic chemotherapy. Direct vascular toxicity of anti-neoplastic therapy may contribute to thrombosis risk. Endothelial cell injury from platinum-based chemotherapy may explain the higher rate of VTE in patients treated with these agents [41]. Anti-angiogenic therapy with vascular endothelial growth factor (VEGF) inhibitors such as bevacizumab, and other VEGF-signaling pathway inhibitors including sunitinib and sorafenib, are associated with both venous and arterial thrombosis presumably related to endothelial toxicity [42, 43]. Chemotherapy-induced elevations in cell-free DNA, possibly from necrotic tumor cells or via NETs, may promote thrombosis via contact activation and generation of thrombin-antithrombin complexes [44]. VTE rates are also increased in patients with multiple myeloma receiving thalidomide or lenalidomide and dexamethasone [45, 46].
Long-term central venous catheters, commonly inserted for the administration of IV chemotherapeutics, are associated with increased thrombotic risk via injury to the vessel wall during insertion, venous stasis, and direct contact pathway activation [47].
Treatment
The goals of VTE treatment in cancer patients are no different than those for patients without malignancy. Therapeutic anticoagulation should be administered with the intention of improving symptoms, achieving resolution of thrombosis and reducing the risk of VTE recurrence. However, cancer patients present with disease- and cancer treatment-specific challenges, including higher rates of recurrent VTE and uncertainly about the appropriate duration of treatment.
Thromboprophylaxis in Ambulatory Patients
Given the high thrombotic risk of oncologic patients, a number of randomized controlled trials have been conducted to assess the efficacy and safety of thromboprophylaxis during chemotherapy in the ambulatory setting. The “Prophylaxis of Thromboembolism During Chemotherapy (PROTECHT)” [48] and the “Evaluation of AVE5026 in the Prevention of Venous Thromboembolism in Cancer Patients Undergoing Chemotherapy (SAVE-ONCO)” [49] enrolled ambulatory patients with various solid malignancies, whereas the “Gemcitabine versus gemcitabine plus dalteparin thromboprophylaxis in pancreatic cancer (FRAGEM)” [50] and the “Chemotherapy With or Without Enoxaparin in Pancreatic Cancer (PROSPECT-CONKO 004)” [51] limited inclusion to pancreatic cancer (of note, the results of the latter have been published only in abstract form). Patients with metastatic breast cancer or stage III/IV lung cancer [52], glioma [53], and those with multiple myeloma treated with thalidomide [54] or lenalidomide [55] were enrolled in dedicated trials. Based on the cumulative evidence, the current American Society of Clinical Oncology Clinical Practice Guideline [56] does not recommend routine thromboprophylaxis in ambulatory cancer patients; however, individualized prophylactic treatment with LMWH can be considered in solid tumors and aspirin, or LMWH should be used in multiple myeloma patients receiving thalidomide or lenalidomide based on their thrombotic risk.
Treatment of Cancer-Associated VTE: LMWH vs Warfarin
While the principles of antithrombotic therapy apply to all patients with VTE, several factors complicate treatment in patients with cancer. The presence of drug interactions, gastrointestinal and hematologic effects of chemotherapy and radiation, including vomiting and malabsorption, and poor venous access may significantly limit the use of oral treatments. For several decades, vitamin K antagonists (VKA) such as warfarin represented the standard long-term therapy for acute VTE after an initial treatment with unfractionated heparin or, more recently, subcutaneous LMWH. Low-molecular-weight heparins present several advantages compared to oral agents including predictable pharmacokinetics that do not require monitoring of anticoagulation effect. Therefore, they may offer a more effective and safer alternative to VKA. This hypothesis was confirmed in the “Low-Molecular-Weight Heparin versus a Coumarin for the Prevention of Recurrent Venous Thromboembolism in Patients with Cancer (CLOT)” trial, which evaluated the efficacy and safety of subcutaneous dalteparin compared with warfarin for the reduction of VTE recurrence in cancer patients [57••]. At 6 months, treatment with dalteparin was associated with a significantly lower rate of VTE recurrence compared with warfarin (8.0 vs. 15.8%; HR 0.48; 95% CI 0.30–0.77; P = 0.002), with no difference in major bleeding (6 vs. 4%) or any bleeding (14 vs. 19%). Consistent with the results of the CLOT trial, the “Long-term Low-Molecular-Weight Heparin versus Usual Care in Proximal-Vein Thrombosis Patients with Cancer (LITE)” study showed that treatment with tinzaparin for 3 months was associated with a significantly reduced risk of recurrent VTE at 12 months (P = 0.044; risk ratio = 0.44) with no difference in bleeding [58]. The safety of LMWH compared with VKA in patients with cancer, has also been confirmed in smaller trials [59, 60]. More recently, the efficacy and safety of extending LMWH treatment duration to 12 months were assessed in the DALTECAN study. Interestingly, no improvement in VTE recurrence, nor an increase in bleeding rates were observed at 12 months compared to only 6 months of therapy [61]. These results support the findings that the majority of bleeding and recurrent VTE events occur early on, often within the first month, of initiating therapeutic anticoagulation. Finally, the “Comparison of Acute Treatments in Cancer Hemostasis“(CATCH) trial of 2015 compared LMWH tinzaparin with warfarin across a multinational sample size of 900 cancer patients [62]. The study found lower rates of recurrent VTE in the tinzaparin cohort compared to warfarin (7.2 vs 10.5%, respectively), but the difference was not statistically significant (p = 0.07). There were no differences in major bleeding or overall mortality between the two treatments, but a significant reduction in clinically relevant nonmajor bleeding was observed in patients receiving tinzaparin compared to those receiving warfarin.
Direct Oral Anticoagulants (DOACs) in Cancer-Associated VTE
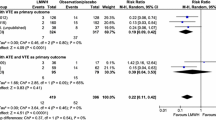
Therapeutic anticoagulation with direct oral anticoagulants (DOACs) is appealing, given the convenience of oral administration and lack of regular drug monitoring compared to LMWH and warfarin, respectively. DOACs have established efficacy for treatment of acute VTE when tested in randomized clinical trials including thousands of patients [63]. However, only about 6% of patients enrolled had a diagnosis of active cancer, and it is unclear how many of these patients had high-risk tumor types, advanced, or metastatic disease. Meta-analysis of the original DOAC-VTE trials focusing on the limited subset of patients with malignancy suggests that DOACs are safe and efficacious in the cancer population as well [63]. Recently published and ongoing trials are prospectively evaluating the efficacy and safety of DOACs versus LMWH in cancer patients. The “Edoxaban for the Treatment of Cancer-Associated Venous Thromboembolism (HOKUSAI-VTE Cancer)” study is the largest randomized trial published to date and evaluated the efficacy and safety of edoxaban vs dalteparin in cancer patients with acute symptomatic or incidental VTE [64]. The study included 1050 patients with an open label non-inferiority design. Every patient received dalteparin for 5 days and then either oral edoxaban 60 mg once daily or subcutaneous dalteparin for a minimum of 6 months to a maximum of 12 months. The primary outcome was a composite of VTE recurrence or major bleeding during the 1-year study period. Results showed that edoxaban was non-inferior to dalteparin in the primary composite outcome of recurrent VTE or in major bleeding at 12 months (12.8% edoxaban vs. 13.5% dalteparin group; P = 0.006). A non-significant reduction in VTE recurrence was seen in the edoxaban group (7.9 vs. 11.3%; P = 0.09). However, a higher rate of major bleeding in patients receiving edoxaban (6.9 vs. 4.0%; P = 0.04) was observed. Bleeding events in patients receiving edoxaban were more often gastrointestinal and occurred preferentially in patients with gastrointestinal malignancies.
The SELECT-D trial randomized 406 cancer patients with VTE (symptomatic or incidental PE, or symptomatic lower-extremity proximal DVT) to rivaroxaban or dalteparin [65]. At 6-month follow-up, rivaroxaban was associated with lower rates of VTE than dalteparin (4 vs. 11%, respectively), with no difference in major bleeding (3 vs 4%, respectively). However, the rate of clinically relevant non-major bleeding was higher with rivaroxaban than dalteparin (12.3 vs. 3%, respectively). Importantly, the protocol was amended to exclude patients with esophageal and gastrointestinal malignancies due to an imbalance in major bleeding rates compared to other trials.
In summary, data are promising that DOAC therapy might be an acceptable alternative to LMWH for treatment of cancer thrombosis. However, the observed increase in bleeding may make DOACs unsafe in patients with gastrointestinal malignancies. Additional ongoing DOAC trials will help better characterize the efficacy and safety of these agents in the treatment of malignancy-associated VTE.
Duration of Treatment
The ideal length of time that patients with VTE and cancer should receive therapeutic anticoagulation has not been definitively established. Compared to patients without malignancy, where treatment can be confined to 3 months, consensus guidelines suggest that treatment for VTE in cancer continues for at least 6 months [56]. The need for continuing anticoagulation beyond this point should take into consideration the presence of progressive or metastatic disease, ongoing chemotherapy, and risk of bleeding while receiving anticoagulation.
Screening for Cancer in Incident VTE
Unprovoked VTE may be one of the first manifestations of cancer, with the highest risk occurring within the first year of VTE diagnosis. Previous reports suggested that as many as 10% of patients presenting with unprovoked VTE would subsequently be diagnosed with cancer. These results prompted prospective investigations of an extensive versus limited oncologic screening strategy in patients presenting with unprovoked VTE. Based on a series of recent prospective, randomized controlled trials, occult cancer was detected in only about 1 in 20 patients presenting with unprovoked VTE, which nevertheless is a several-fold higher risk than that observed in the general population [66]. An extensive screening test, including computed tomography (CT) of the chest, abdomen, and pelvis or positron-emission tomography (PET)-CT plus mammography in female patients, did tend to detect occult cancer more frequently, but the results did not reach statistical significance and did not result in a reduction in cancer-related or overall mortality [67, 68]. Nevertheless, risk factors that enrich for occult cancer diagnosis in patients with unprovoked VTE have been reported. In an analysis of 5863 patients in the RIETE registry with VTE, 444 were diagnosed with occult cancer within 2 years, with the majority of cancers being detected within 6 months [69]. Age > 70 years and anemia were the two strongest risk factors (2 points), and male gender, chronic lung disease, and platelet count ≥ 350 × 109/L were also independently associated with occult cancer detection (1 point). Post-operative status and history of prior VTE were associated with lower incidence of cancer diagnosis (− 2 and − 1 points, respectively). The rates of occult cancer detection with ≤ 2 or ≥ 3 points were 5.8% (241 of 4150 patients) and 12% (203 of 1713 patients), respectively. This model requires prospective validation before selective cancer screening of high-risk VTE patients can be adopted. Consensus guidelines recommend that physicians maintain a high level of suspicion for occult cancer and perform a thorough history, physical exam, and basic blood work (complete blood count, liver function tests) along with a chest X-ray. Ensuring that all patients diagnosed with VTE are up-to-date with age-appropriate cancer screening is also essential. In contrast to VTE, superficial venous thrombosis does not appear to be associated with an increased risk for occult malignancy, although some of the results are conflicting [2•].
Special Scenarios
Intracranial Neoplasms
VTE frequently complicates primary tumors of the brain and cancers with brain metastasis. Limited published information exists to provide guidance for clinicians to weigh the benefits of therapeutic anticoagulation against the feared complication of intracranial hemorrhage (ICH), which carries a high fatality rate. Few patients with intracranial metastasis were enrolled in cancer VTE treatment trials. Certain types of brain metastasis are associated with high rates of spontaneous ICH, including renal cell carcinoma (RCC) and melanoma. A recently published control-matched cohort study of 293 patients with brain metastasis, over 50% with lung cancer, compared 104 treated with enoxaparin to 189 matched controls [70]. The rate of ICH over 1 year was not significantly different in those patients receiving enoxaparin versus controls, 19 versus 21%, respectively. Renal cell carcinoma and melanoma were the only variables independently associated with increased risk of ICH, approaching a risk of 50% at 1 year, but treatment with enoxaparin did affect this risk [70]. Traditionally, the presence of brain metastases from RCC or melanoma has been a contraindication to therapeutic anticoagulation. In contrast, the same group studied the outcomes in a matched cohort of patients with malignant primary brain tumors receiving enoxaparin compared to control and found that in glioma patients, therapeutic anticoagulation was associated with a ~ 13-fold increase in ICH [71]. Enoxaparin-associated ICH in glioma patients was associated with a 70% shortening of medial survival time compared to spontaneous ICH. These results are supported by a meta-analysis demonstrating increased risk for ICH in patients with malignant primary brain tumors treated with anticoagulation compared to those with brain metastasis [72].
Incidental VTE
The improved resolution of current imaging modalities combined with the need for frequent scans for tumor staging and assessment of treatment response has resulted in an increase in incidentally detected VTE. In fact, studies suggest that in cancer patients, almost half of all VTE diagnoses, especially PE, are detected incidentally in patients without specific symptoms [73,74,75]. This phenomenon has multiple implications. First off, it is important to confirm the accuracy of VTE diagnosis, as the thrombus is often not detected using the ideal imaging modality such as CT angiography for PE or compression duplex ultrasound for DVT. For larger proximal pulmonary embolism, this difference in imaging modality may not affect the accuracy of diagnosis. However, for more distal, subsegmental PE, the diagnosis may be ambiguous. Even dedicated CT pulmonary angiography can have interobserver disagreement about the diagnosis. Lower extremity venous duplex may be helpful in these cases, as presence of DVT would support the diagnosis of PE. Low-flow venous states due to compression by tumor or lymph nodes may result in false-positive DVT diagnosis, and compression ultrasound should confirm the diagnosis whenever possible.
Incidental VTE in cancer patients is associated with worse prognosis with regard to recurrent VTE, bleeding, and death, not dissimilar to symptomatic VTE [76, 77]. These patients require careful assessment to ascertain whether they are truly asymptomatic. Vague complaints of fatigue, malaise, or dyspnea may actually be symptoms due to VTE and therefore anticoagulation is indicated unequivocally. In patients with incidental proximal PE or VTE, anticoagulation with LMWH for at least 3–6 months is appropriate, with consideration for extended dosing depending on the status of the malignancy [78]. Incidental subsegmental PE represents a unique scenario where the decision to anticoagulate is particularly controversial. It is not clear if the presence of incidental subsegmental pulmonary embolism significantly impacts survival in cancer patients [77, 79]. In such cases, the decision to anticoagulate can be made on a case-by-case basis taking into account the patient’s functional status, prognosis, bleeding risk, and patient preference [78].
Isolated Distal DVT
In the non-cancer population, DVT that is confined to the calf veins has been demonstrated to carry a low risk of extension to proximal DVT (< 10%) and an even lower risk of PE (< 1%). Therefore, for symptomatic distal DVT, even if unprovoked, current guidelines recommend treatment with a 3-month course of anticoagulation alone, compared to indefinite anticoagulation [80]. It is even reasonable to adopt of a strategy of serial surveillance for asymptomatic isolated distal DVT in the absence of risk factors for extension [80]. The presence of cancer is, however, a strong risk factor for DVT extension, and cancer patients with isolated distal DVT should be treated with anticoagulation barring another contraindication. Among patients enrolled in the Optimisation de l’interrogatoire dans l’evaluation du risque thromboembolique veineux (OPTIMEV) with a concurrent diagnosis of cancer, isolated distal DVT was associated a similar risk of death, major bleeding, and a higher rate of VTE recurrence compared to those proximal VTE. The risk of death, major bleeding, and VTE recurrence was much higher in those with cancer-associated isolated distal DVT compared to patients without malignancy [81].
Conclusions
Patients with cancer are at increased risk for VTE, and the development of VTE in a cancer patient portends a worse prognosis. Distinct molecular mechanisms are responsible for VTE in cancer, and these mechanisms vary between cancer subtypes. Clinical risk scores can help predict the incidence of VTE in cancer patients, but further research is required to determine the optimal utilization of DVT prophylaxis in cancer patients. Guidelines recommend LMWH as the preferred agent for treatment of cancer-associated VTE, with a duration of treatment for at least 6 months. Data supporting the use of DOACs for the treatment of VTE in certain cancer types is promising but requires further validation. Future research should be aimed at developing novel diagnostics and therapeutics based on the distinct mechanisms of cancer-associated VTE.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Trousseau ACJ, Bazire PV. Lectures on clinical medicine: delivered at the hotel-Dieu. Paris: New Sydenham Society; 1872.
• Timp JF, Braekkan SK, Versteeg HH, Cannegieter SC. Epidemiology of cancer-associated venous thrombosis. Blood. 2013;122(10):1712–23. https://doi.org/10.1182/blood-2013-04-460121. This is an excellent summary of the data regarding the incidence, risk factors, and prognosis of VTE in cancer with an emphasis on the differential risk based on tumor type.
Gussoni G, Frasson S, La Regina M, Di Micco P, Monreal M, Investigators R. Three-month mortality rate and clinical predictors in patients with venous thromboembolism and cancer. Findings from the RIETE registry. Thromb Res. 2013;131(1):24–30. https://doi.org/10.1016/j.thromres.2012.10.007.
Spencer FA, Lessard D, Emery C, Reed G, Goldberg RJ. Venous thromboembolism in the outpatient setting. Arch Intern Med. 2007;167(14):1471–5. https://doi.org/10.1001/archinte.167.14.1471.
Walker AJ, Card TR, West J, Crooks C, Grainge MJ. Incidence of venous thromboembolism in patients with cancer - a cohort study using linked United Kingdom databases. Eur J Cancer. 2013;49(6):1404–13. https://doi.org/10.1016/j.ejca.2012.10.021.
Blom JW, Doggen CJ, Osanto S, Rosendaal FR. Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA. 2005;293(6):715–22. https://doi.org/10.1001/jama.293.6.715.
Horsted F, West J, Grainge MJ. Risk of venous thromboembolism in patients with cancer: a systematic review and meta-analysis. PLoS Med. 2012;9(7):e1001275. https://doi.org/10.1371/journal.pmed.1001275.
Blom JW, Vanderschoot JP, Oostindier MJ, Osanto S, van der Meer FJ, Rosendaal FR. Incidence of venous thrombosis in a large cohort of 66,329 cancer patients: results of a record linkage study. J Thromb Haemost. 2006;4(3):529–35. https://doi.org/10.1111/j.1538-7836.2006.01804.x.
Khorana AA, Dalal M, Lin J, Connolly GC. Incidence and predictors of venous thromboembolism (VTE) among ambulatory high-risk cancer patients undergoing chemotherapy in the United States. Cancer. 2013;119(3):648–55. https://doi.org/10.1002/cncr.27772.
Chew HK, Wun T, Harvey D, Zhou H, White RH. Incidence of venous thromboembolism and its effect on survival among patients with common cancers. Arch Intern Med. 2006;166(4):458–64. https://doi.org/10.1001/archinte.166.4.458.
Sorensen HT, Mellemkjaer L, Olsen JH, Baron JA. Prognosis of cancers associated with venous thromboembolism. N Engl J Med. 2000;343(25):1846–50. https://doi.org/10.1056/NEJM200012213432504.
Gade IL, Braekkan S, Naess IA, Hansen JB, Rosendaal F, Cannegieter S, et al. Epidemiology of venous thromboembolism in hematological cancers: the Scandinavian thrombosis and Cancer (STAC) cohort. Thromb Res. 2017;158:157–60. https://doi.org/10.1016/j.thromres.2017.09.002.
Falanga A, Marchetti M. Venous thromboembolism in the hematologic malignancies. J Clin Oncol. 2009;27(29):4848–57. https://doi.org/10.1200/JCO.2009.22.8197.
• Khorana AA, Kuderer NM, Culakova E, Lyman GH, Francis CW. Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood. 2008;111(10):4902–7. https://doi.org/10.1182/blood-2007-10-116327. This study established the Khorana score, which incorporates patient-specific risk-factors and tumor-specific risk factors in outpatients starting chemotherapy. The predictive power of this score can be enhanced through addition of biomarker measurement.
Ay C, Dunkler D, Marosi C, Chiriac AL, Vormittag R, Simanek R, et al. Prediction of venous thromboembolism in cancer patients. Blood. 2010;116(24):5377–82. https://doi.org/10.1182/blood-2010-02-270116.
Pabinger I, van Es N, Heinze G, Posch F, Riedl J, Reitter EM, et al. A clinical prediction model for cancer-associated venous thromboembolism: a development and validation study in two independent prospective cohorts. Lancet Haematol. 2018;5:e289–98. https://doi.org/10.1016/S2352-3026(18)30063-2.
Khorana AA, Rubens D, Francis CW. Screening high-risk cancer patients for VTE: a prospective observational study. Thromb Res. 2014;134(6):1205–7. https://doi.org/10.1016/j.thromres.2014.09.016.
Imberti D, Agnelli G, Ageno W, Moia M, Palareti G, Pistelli R, et al. Clinical characteristics and management of cancer-associated acute venous thromboembolism: findings from the MASTER registry. Haematologica. 2008;93(2):273–8. https://doi.org/10.3324/haematol.11458.
Martinelli I, De Stefano V. Rare thromboses of cerebral, splanchnic and upper-extremity veins. A narrative review. Thromb Haemost. 2010;103(6):1136–44. https://doi.org/10.1160/TH09-12-0873.
Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman GH. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J Thromb Haemost. 2007;5(3):632–4. https://doi.org/10.1111/j.1538-7836.2007.02374.x.
Trujillo-Santos J, Martos FM, Font C, Farge-Bancel D, Rosa V, Lorenzo A, et al. Analysis of clinical factors affecting the rates of fatal pulmonary embolism and bleeding in cancer patients with venous thromboembolism. Heliyon. 2017;3(1):e00229. https://doi.org/10.1016/j.heliyon.2016.e00229.
Schulman S, Zondag M, Linkins L, Pasca S, Cheung YW, de Sancho M, et al. Recurrent venous thromboembolism in anticoagulated patients with cancer: management and short-term prognosis. J Thromb Haemost. 2015;13(6):1010–8. https://doi.org/10.1111/jth.12955.
Prandoni P, Lensing AW, Piccioli A, Bernardi E, Simioni P, Girolami B, et al. Recurrent venous thromboembolism and bleeding complications during anticoagulant treatment in patients with cancer and venous thrombosis. Blood. 2002;100(10):3484–8. https://doi.org/10.1182/blood-2002-01-0108.
Trujillo-Santos J, Nieto JA, Tiberio G, Piccioli A, Di Micco P, Prandoni P, et al. Predicting recurrences or major bleeding in cancer patients with venous thromboembolism. Findings from the RIETE registry. Thromb Haemost. 2008;100(3):435–9.
Louzada ML, Carrier M, Lazo-Langner A, Dao V, Kovacs MJ, Ramsay TO, et al. Development of a clinical prediction rule for risk stratification of recurrent venous thromboembolism in patients with cancer-associated venous thromboembolism. Circulation. 2012;126(4):448–54. https://doi.org/10.1161/CIRCULATIONAHA.111.051920.
den Exter PL, Kooiman J, Huisman MV. Validation of the Ottawa prognostic score for the prediction of recurrent venous thromboembolism in patients with cancer-associated thrombosis. J Thromb Haemost. 2013;11(5):998–1000. https://doi.org/10.1111/jth.12192.
Hisada Y, Mackman N. Cancer-associated pathways and biomarkers of venous thrombosis. Blood. 2017;130(13):1499–506. https://doi.org/10.1182/blood-2017-03-743211.
Blix K, Jensvoll H, Braekkan SK, Hansen JB. White blood cell count measured prior to cancer development is associated with future risk of venous thromboembolism—the Tromso study. PLoS One. 2013;8(9):e73447. https://doi.org/10.1371/journal.pone.0073447.
Demers M, Wagner DD. NETosis: a new factor in tumor progression and cancer-associated thrombosis. Semin Thromb Hemost. 2014;40(3):277–83. https://doi.org/10.1055/s-0034-1370765.
Savchenko AS, Martinod K, Seidman MA, Wong SL, Borissoff JI, Piazza G, et al. Neutrophil extracellular traps form predominantly during the organizing stage of human venous thromboembolism development. J Thromb Haemost. 2014;12(6):860–70. https://doi.org/10.1111/jth.12571.
Demers M, Krause DS, Schatzberg D, Martinod K, Voorhees JR, Fuchs TA, et al. Cancers predispose neutrophils to release extracellular DNA traps that contribute to cancer-associated thrombosis. Proc Natl Acad Sci U S A. 2012;109(32):13076–81. https://doi.org/10.1073/pnas.1200419109.
Simanek R, Vormittag R, Ay C, Alguel G, Dunkler D, Schwarzinger I, et al. High platelet count associated with venous thromboembolism in cancer patients: results from the Vienna Cancer and thrombosis study (CATS). J Thromb Haemost. 2010;8(1):114–20. https://doi.org/10.1111/j.1538-7836.2009.03680.x.
Khorana AA, Francis CW, Culakova E, Lyman GH. Risk factors for chemotherapy-associated venous thromboembolism in a prospective observational study. Cancer. 2005;104(12):2822–9. https://doi.org/10.1002/cncr.21496.
Stone RL, Nick AM, McNeish IA, Balkwill F, Han HD, Bottsford-Miller J, et al. Paraneoplastic thrombocytosis in ovarian cancer. N Engl J Med. 2012;366(7):610–8. https://doi.org/10.1056/NEJMoa1110352.
Geddings JE, Mackman N. Tumor-derived tissue factor-positive microparticles and venous thrombosis in cancer patients. Blood. 2013;122(11):1873–80. https://doi.org/10.1182/blood-2013-04-460139.
Thaler J, Ay C, Mackman N, Bertina RM, Kaider A, Marosi C, et al. Microparticle-associated tissue factor activity, venous thromboembolism and mortality in pancreatic, gastric, colorectal and brain cancer patients. J Thromb Haemost. 2012;10(7):1363–70. https://doi.org/10.1111/j.1538-7836.2012.04754.x.
Regina S, Valentin JB, Lachot S, Lemarie E, Rollin J, Gruel Y. Increased tissue factor expression is associated with reduced survival in non-small cell lung cancer and with mutations of TP53 and PTEN. Clin Chem. 2009;55(10):1834–42. https://doi.org/10.1373/clinchem.2009.123695.
Rong Y, Post DE, Pieper RO, Durden DL, Van Meir EG, Brat DJ. PTEN and hypoxia regulate tissue factor expression and plasma coagulation by glioblastoma. Cancer Res. 2005;65(4):1406–13. https://doi.org/10.1158/0008-5472.CAN-04-3376.
Langer F, Bokemeyer C. Crosstalk between cancer and haemostasis. Implications for cancer biology and cancer-associated thrombosis with focus on tissue factor. Hamostaseologie. 2012;32(2):95–104. https://doi.org/10.5482/ha-1160.
Ay C, Simanek R, Vormittag R, Dunkler D, Alguel G, Koder S, et al. High plasma levels of soluble P-selectin are predictive of venous thromboembolism in cancer patients: results from the Vienna Cancer and thrombosis study (CATS). Blood. 2008;112(7):2703–8. https://doi.org/10.1182/blood-2008-02-142422.
Nuver J, De Haas EC, Van Zweeden M, Gietema JA, Meijer C. Vascular damage in testicular cancer patients: a study on endothelial activation by bleomycin and cisplatin in vitro. Oncol Rep. 2010;23(1):247–53.
Sonpavde G, Je Y, Schutz F, Galsky MD, Paluri R, Rosenberg JE, et al. Venous thromboembolic events with vascular endothelial growth factor receptor tyrosine kinase inhibitors: a systematic review and meta-analysis of randomized clinical trials. Crit Rev Oncol Hematol. 2013;87(1):80–9. https://doi.org/10.1016/j.critrevonc.2012.12.006.
Nalluri SR, Chu D, Keresztes R, Zhu X, Wu S. Risk of venous thromboembolism with the angiogenesis inhibitor bevacizumab in cancer patients: a meta-analysis. JAMA. 2008;300(19):2277–85. https://doi.org/10.1001/jama.2008.656.
Swystun LL, Mukherjee S, Liaw PC. Breast cancer chemotherapy induces the release of cell-free DNA, a novel procoagulant stimulus. J Thromb Haemost. 2011;9(11):2313–21. https://doi.org/10.1111/j.1538-7836.2011.04465.x.
Knight R, DeLap RJ, Zeldis JB. Lenalidomide and venous thrombosis in multiple myeloma. N Engl J Med. 2006;354(19):2079–80. https://doi.org/10.1056/NEJMc053530.
Zangari M, Anaissie E, Barlogie B, Badros A, Desikan R, Gopal AV, et al. Increased risk of deep-vein thrombosis in patients with multiple myeloma receiving thalidomide and chemotherapy. Blood. 2001;98(5):1614–5.
Verso M, Agnelli G. Venous thromboembolism associated with long-term use of central venous catheters in cancer patients. J Clin Oncol. 2003;21(19):3665–75. https://doi.org/10.1200/JCO.2003.08.008.
Agnelli G, Gussoni G, Bianchini C, Verso M, Mandala M, Cavanna L, et al. Nadroparin for the prevention of thromboembolic events in ambulatory patients with metastatic or locally advanced solid cancer receiving chemotherapy: a randomised, placebo-controlled, double-blind study. Lancet Oncol. 2009;10(10):943–9. https://doi.org/10.1016/S1470-2045(09)70232-3.
Agnelli G, George DJ, Kakkar AK, Fisher W, Lassen MR, Mismetti P, et al. Semuloparin for thromboprophylaxis in patients receiving chemotherapy for cancer. N Engl J Med. 2012;366(7):601–9. https://doi.org/10.1056/NEJMoa1108898.
Maraveyas A, Waters J, Roy R, Fyfe D, Propper D, Lofts F, et al. Gemcitabine versus gemcitabine plus dalteparin thromboprophylaxis in pancreatic cancer. Eur J Cancer. 2012;48(9):1283–92. https://doi.org/10.1016/j.ejca.2011.10.017.
Riess HPU, Opitz B, Stauch M, Reitzig P, Hahnfeld S, et al. A prospective, randomized trial of simultaneous pancreatic cancer treatment with enoxaparin and chemotherapy: final results of the CONKO-004 trial. J Clin Oncol. 2010;28(15_suppl).
Haas SK, Freund M, Heigener D, Heilmann L, Kemkes-Matthes B, von Tempelhoff GF, et al. Low-molecular-weight heparin versus placebo for the prevention of venous thromboembolism in metastatic breast cancer or stage III/IV lung cancer. Clin Appl Thromb Hemost. 2012;18(2):159–65. https://doi.org/10.1177/1076029611433769.
Perry JR, Julian JA, Laperriere NJ, Geerts W, Agnelli G, Rogers LR, et al. PRODIGE: a randomized placebo-controlled trial of dalteparin low-molecular-weight heparin thromboprophylaxis in patients with newly diagnosed malignant glioma. J Thromb Haemost. 2010;8(9):1959–65. https://doi.org/10.1111/j.1538-7836.2010.03973.x.
Palumbo A, Cavo M, Bringhen S, Zamagni E, Romano A, Patriarca F, et al. Aspirin, warfarin, or enoxaparin thromboprophylaxis in patients with multiple myeloma treated with thalidomide: a phase III, open-label, randomized trial. J Clin Oncol. 2011;29(8):986–93. https://doi.org/10.1200/JCO.2010.31.6844.
Larocca A, Cavallo F, Bringhen S, Di Raimondo F, Falanga A, Evangelista A, et al. Aspirin or enoxaparin thromboprophylaxis for patients with newly diagnosed multiple myeloma treated with lenalidomide. Blood. 2012;119(4):933–9; quiz 1093. https://doi.org/10.1182/blood-2011-03-344333.
Lyman GH, Bohlke K, Khorana AA, Kuderer NM, Lee AY, Arcelus JI, et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: American Society of Clinical Oncology Clinical Practice Guideline update 2014. J Clin Oncol. 2015;33(6):654–6. https://doi.org/10.1200/JCO.2014.59.7351.
•• Lee AY, Levine MN, Baker RI, Bowden C, Kakkar AK, Prins M, et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349(2):146–53. https://doi.org/10.1056/NEJMoa025313. This study established the basis for superiority of LMWH over warfarin for the treatment of VTE in cancer. At 6 months, treatment with dalteparin was associated with a significantly lower rate of VTE recurrence compared with warfarin, with no difference in major bleeding.
Hull RD, Pineo GF, Brant RF, Mah AF, Burke N, Dear R, et al. Long-term low-molecular-weight heparin versus usual care in proximal-vein thrombosis patients with cancer. Am J Med. 2006;119(12):1062–72. https://doi.org/10.1016/j.amjmed.2006.02.022.
Meyer G, Marjanovic Z, Valcke J, Lorcerie B, Gruel Y, Solal-Celigny P, et al. Comparison of low-molecular-weight heparin and warfarin for the secondary prevention of venous thromboembolism in patients with cancer: a randomized controlled study. Arch Intern Med. 2002;162(15):1729–35.
Deitcher SR, Kessler CM, Merli G, Rigas JR, Lyons RM, Fareed J, et al. Secondary prevention of venous thromboembolic events in patients with active cancer: enoxaparin alone versus initial enoxaparin followed by warfarin for a 180-day period. Clin Appl Thromb Hemost. 2006;12(4):389–96. https://doi.org/10.1177/1076029606293692.
Francis CW, Kessler CM, Goldhaber SZ, Kovacs MJ, Monreal M, Huisman MV, et al. Treatment of venous thromboembolism in cancer patients with dalteparin for up to 12 months: the DALTECAN study. J Thromb Haemost. 2015;13(6):1028–35. https://doi.org/10.1111/jth.12923.
Lee AYY, Kamphuisen PW, Meyer G, Bauersachs R, Janas MS, Jarner MF, et al. Tinzaparin vs warfarin for treatment of acute venous thromboembolism in patients with active Cancer: a randomized clinical trial. JAMA. 2015;314(7):677–86. https://doi.org/10.1001/jama.2015.9243.
van der Hulle T, den Exter PL, Kooiman J, van der Hoeven JJ, Huisman MV, Klok FA. Meta-analysis of the efficacy and safety of new oral anticoagulants in patients with cancer-associated acute venous thromboembolism. J Thromb Haemost. 2014;12(7):1116–20. https://doi.org/10.1111/jth.12605.
Raskob GE, van Es N, Verhamme P, Carrier M, Di Nisio M, Garcia D, et al. Edoxaban for the treatment of cancer-associated venous thromboembolism. N Engl J Med. 2018;378(7):615–24. https://doi.org/10.1056/NEJMoa1711948.
Young AM, Marshall A, Thirlwall J, Chapman O, Lokare A, Hill C, et al. Comparison of an oral factor Xa inhibitor with low molecular weight heparin in patients with cancer with venous thromboembolism: results of a randomized trial (SELECT-D). J Clin Oncol. 2018;JCO2018788034. https://doi.org/10.1200/JCO.2018.78.8034.
van Es N, Le Gal G, Otten HM, Robin P, Piccioli A, Lecumberri R, et al. Screening for occult cancer in patients with unprovoked venous thromboembolism: a systematic review and meta-analysis of individual patient data. Ann Intern Med. 2017;167(6):410–7. https://doi.org/10.7326/M17-0868.
Carrier M, Lazo-Langner A, Shivakumar S, Tagalakis V, Zarychanski R, Solymoss S, et al. Screening for occult Cancer in unprovoked venous thromboembolism. N Engl J Med. 2015;373(8):697–704. https://doi.org/10.1056/NEJMoa1506623.
Robin P, Le Roux PY, Planquette B, Accassat S, Roy PM, Couturaud F, et al. Limited screening with versus without (18)F-fluorodeoxyglucose PET/CT for occult malignancy in unprovoked venous thromboembolism: an open-label randomised controlled trial. Lancet Oncol. 2016;17(2):193–9. https://doi.org/10.1016/S1470-2045(15)00480-5.
Jara-Palomares L, Otero R, Jimenez D, Carrier M, Tzoran I, Brenner B, et al. Development of a risk prediction score for occult Cancer in patients with VTE. Chest. 2017;151(3):564–71. https://doi.org/10.1016/j.chest.2016.10.025.
Donato J, Campigotto F, Uhlmann EJ, Coletti E, Neuberg D, Weber GM, et al. Intracranial hemorrhage in patients with brain metastases treated with therapeutic enoxaparin: a matched cohort study. Blood. 2015;126(4):494–9. https://doi.org/10.1182/blood-2015-02-626788.
Mantia C, Uhlmann EJ, Puligandla M, Weber GM, Neuberg D, Zwicker JI. Predicting the higher rate of intracranial hemorrhage in glioma patients receiving therapeutic enoxaparin. Blood. 2017;129(25):3379–85. https://doi.org/10.1182/blood-2017-02-767285.
Zwicker JI, Karp Leaf R, Carrier M. A meta-analysis of intracranial hemorrhage in patients with brain tumors receiving therapeutic anticoagulation. J Thromb Haemost. 2016;14(9):1736–40. https://doi.org/10.1111/jth.13387.
Shinagare AB, Guo M, Hatabu H, Krajewski KM, Andriole K, Van den Abbeele AD, et al. Incidence of pulmonary embolism in oncologic outpatients at a tertiary cancer center. Cancer. 2011;117(16):3860–6. https://doi.org/10.1002/cncr.25941.
Font C, Farrus B, Vidal L, Caralt TM, Visa L, Mellado B, et al. Incidental versus symptomatic venous thrombosis in cancer: a prospective observational study of 340 consecutive patients. Ann Oncol. 2011;22(9):2101–6. https://doi.org/10.1093/annonc/mdq720.
Bach AG, Schmoll HJ, Beckel C, Behrmann C, Spielmann RP, Wienke A, et al. Pulmonary embolism in oncologic patients: frequency and embolus burden of symptomatic and unsuspected events. Acta Radiol. 2014;55(1):45–53. https://doi.org/10.1177/0284185113491569.
den Exter PL, Hooijer J, Dekkers OM, Huisman MV. Risk of recurrent venous thromboembolism and mortality in patients with cancer incidentally diagnosed with pulmonary embolism: a comparison with symptomatic patients. J Clin Oncol. 2011;29(17):2405–9. https://doi.org/10.1200/JCO.2010.34.0984.
O'Connell C, Razavi P, Ghalichi M, Boyle S, Vasan S, Mark L, et al. Unsuspected pulmonary emboli adversely impact survival in patients with cancer undergoing routine staging multi-row detector computed tomography scanning. J Thromb Haemost. 2011;9(2):305–11. https://doi.org/10.1111/j.1538-7836.2010.04114.x.
Di Nisio M, Lee AY, Carrier M, Liebman HA, Khorana AA. Subcommittee on H et al. diagnosis and treatment of incidental venous thromboembolism in cancer patients: guidance from the SSC of the ISTH. J Thromb Haemost. 2015;13(5):880–3. https://doi.org/10.1111/jth.12883.
van der Hulle T, den Exter PL, Planquette B, Meyer G, Soler S, Monreal M, et al. Risk of recurrent venous thromboembolism and major hemorrhage in cancer-associated incidental pulmonary embolism among treated and untreated patients: a pooled analysis of 926 patients. J Thromb Haemost. 2016;14(1):105–13. https://doi.org/10.1111/jth.13172.
Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315–52. https://doi.org/10.1016/j.chest.2015.11.026.
Galanaud JP, Sevestre MA, Pernod G, Genty C, Richelet S, Kahn SR, et al. Long-term outcomes of cancer-related isolated distal deep vein thrombosis: the OPTIMEV study. J Thromb Haemost. 2017;15(5):907–16. https://doi.org/10.1111/jth.13664.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Cardio-Oncology
Rights and permissions
About this article
Cite this article
Schmaier, A.A., Ambesh, P. & Campia, U. Venous Thromboembolism and Cancer. Curr Cardiol Rep 20, 89 (2018). https://doi.org/10.1007/s11886-018-1034-3
Published:
DOI: https://doi.org/10.1007/s11886-018-1034-3