Abstract
Purpose of Review
This study aims to determine if percutaneous coronary intervention (PCI) does improve survival in stable ischemic heart disease (SIHD).
Recent Findings
The International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial will evaluate patients with moderate to severe ischemia and will be the largest randomized trial of an initial management strategy of coronary revascularization (percutaneous or surgical) versus optimal medical therapy alone for SIHD. Although the ISCHEMIA trial may show a benefit with upfront coronary revascularization in this high-risk population, cardiac events after PCI are largely caused by plaque rupture in segments outside of the original stented segment. Furthermore, given the robust data from prior randomized trials, which showed no survival benefit with PCI, and the likelihood that the highest risk patients in ISCHEMIA will be treated with surgery, it is unlikely that the ISCHEMIA trial will show a survival benefit particular to PCI.
Recent Findings
Although PCI relieves symptoms, the evidence base indicates that it does not prolong survival in SIHD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stable ischemic heart disease (SIHD) is characterized by atherosclerotic narrowing of the coronary arteries and leads to myocardial ischemia, an imbalance of myocardial oxygen supply and demand. SIHD affects millions of patients worldwide and typically manifests as angina during exertion, mental stress, or other conditions that increase myocardial oxygen demand. The clinical significance of SIHD arises not only from symptoms due to myocardial ischemia but also from the mortality that results from the complications of coronary artery disease, particularly myocardial infarction, congestive heart failure, and ventricular arrhythmia.
While there is no doubt that acute coronary syndromes, especially ST-segment elevation myocardial infarction are best treated by coronary revascularization, SIHD may be treated by optimal medical therapy (OMT) alone or in conjunction with coronary revascularization. Large randomized clinical trials completed in the last decade (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) and Bypass Angioplasty Revascularization Investigation in Type 2 Diabetes (BARI 2D)) have found no mortality difference between an initial strategy of OMT alone and an initial strategy of OMT plus coronary revascularization [1, 2]. Recent extended (up to 15 years) follow-up of the COURAGE trial also showed identical survival curves between the initial OMT and initial PCI groups, even in subgroups with up to 50% all-cause mortality [3••]. Therefore, the data currently support the use of coronary revascularization in SIHD after a trial of OMT fails to adequately control symptoms.
Observational studies, however, suggest that patients with moderate to severe ischemia may benefit from an initial strategy of revascularization as opposed to those with mild ischemia [4, 5]. The ISCHEMIA trial, which is currently enrolling patients with moderate to severe ischemia will be the largest randomized trial of OMT alone versus coronary revascularization (PCI or coronary artery bypass graft surgery (CABG) in SIHD [6]. In this review, we consider the evidence to date that PCI might improve survival in patients with SIHD, especially in high risk subsets.
Pathophysiology
The early stages of atherosclerosis begin with a focal thickening of the intima and development of intimal xanthomas. As the disease progresses, a fibrous cap filled with smooth muscle cells in a collagenous proteoglycan matrix containing macrophages or lymphocytes develops [7]. The difference in the morphology of the fibrous cap atheroma may play a key role in outcomes between stable lesions and the unstable plaques responsible for acute myocardial infarction. A thin-cap fibroatheroma consists of a large necrotic core covered by a cap less than 65 μm in thickness. This cap may rupture and expose thrombogenic factors, leading to the initiation of the clotting cascade in the vessel and subsequent propagation of thrombus and complete vessel occlusion [8]. On the other hand, a calcified thicker fibrous cap may be less prone to rupture. Statins have been shown to maintain the integrity of the fibrous cap, and this is one of the proposed mechanisms explaining how statins prevent cardiovascular events [9]. Virmani et al. found that in a series of patients with sudden death, approximately 60% of the thrombi were due to rupture of a thin-cap atheroma [8]. The Prospective Natural-History Study of Coronary Atherosclerosis (PROSPECT) trial used intravascular ultrasonography to evaluate 697 patients undergoing elective PCI. After 3 years of follow-up, nearly 50% of events prompting angiography were attributed to progression of disease in previously identified nonobstructive lesions with thin-cap fibroatheromas and large plaque burdens, although only a small minority of such lesions (4.9%) resulted in a clinical event [10]. These findings are consistent with earlier observations of Ambrose and Little, that in patients with myocardial infarction who had previous angiograms, 88% of the culprit lesions were previously less than 50% diameter stenosis and 97% of culprit lesions were previously less than 70% diameter stenosis [11, 12]. More recent observations from the COURAGE trial show that even in a population treated with OMT, a third of clinical events result from rapid progression of disease in previously nonobstructive lesions [13]. Taken together, the insights provided by these studies suggest that PCI as a treatment for stable coronary lesions is unlikely to improve survival since many clinical events, and certainly most myocardial infarctions, are not caused by these stable lesions, but rather by rapid progression of disease in unstable plaques.
Effects of Coronary Revascularization on Survival in SIHD: Landmark Trials of Medical Therapy versus CABG
Since the first CABG in 1967 and the first balloon angioplasty in 1977, coronary revascularization has been used quite effectively to treat angina. Randomized comparison to standard medical treatment began soon after new treatments were introduced. The Veterans Administration (VA) cooperative study was a multicenter clinical trial that began in 1972 and randomized 686 patients with SIHD to either medical therapy or CABG with 11-year follow-up [14]. Overall, there was no difference in survival between the two groups (58% medical therapy vs 57% CABG). However, analysis of several high-risk subgroups (left main disease, decreased left ventricular ejection fraction, triple vessel disease) showed a survival benefit with CABG. The European Coronary Surgery Study was a multicenter trial that began in 1973 and randomized 767 males under the age of 65 with preserved left ventricular function to medical therapy versus CABG. This trial showed a 53% absolute risk reduction in mortality over a 5-year period in patients who underwent CABG [15]. The Coronary Artery Surgery Study (CASS) began in 1975, randomized 780 patients to medical therapy versus CABG, and showed a 10-year survival benefit for patients undergoing CABG with three-vessel disease and ejection fraction less than 50% (58% medical therapy vs 75% CABG, p = 0.08) [16, 17].
Following the results of these trials, it seemed that, compared to medical therapy, CABG was superior, especially in those at higher risk of adverse future events. These findings, however, were likely due to the limited medical therapy available at the time. In the CASS trial, patients randomized to medical therapy were prescribed beta-blockers and counseled on smoking cessation [17]. The number of patients on beta-blockers was 63% at 12 months, 65% at 36 months, and 64% at 60 months. Smoking cessation was only accomplished in 25% of patients contacted for follow-up. A review of these early CABG trials noted that, overall, only 3% of patients were being managed with anti-platelet therapy, half received beta-blockers, and statins were not available in many cases [18]. Clearly, the medical therapy available at the time of these trials is not comparable to contemporary OMT. Nevertheless, these landmark trials continue to inform current understanding of the benefits of CABG and underscore the concept that coronary revascularization is most likely to be beneficial in high-risk subsets with advanced severe coronary disease.
Effects of Coronary Revascularization on Survival in SIHD: CABG versus PCI
Several lines of evidence support a survival benefit for CABG compared to PCI. The nature of the disease process suggests that CABG would be protective since it maintains coronary blood flow to the distal myocardium and, thereby, attenuates the effects of plaque rupture that might occur anywhere in the native coronary artery proximal to the graft anastomosis. Furthermore, complete revascularization of all diseased vessels more commonly occurs with CABG as opposed to PCI. A meta-analysis of 35 studies including 89,883 patients found that complete revascularization occurred more commonly in patients undergoing CABG versus PCI (56 vs 25%) and that incomplete revascularization was associated with decreased long-term survival [19•]. Large registries, including the New York State Cardiac Surgery and PCI registry, showed better risk-adjusted survival for patients with multivessel coronary disease treated with CABG compared to drug-eluting stents [20]. Recently, the American College of Cardiology (ACC) Foundation/STS Collaboration on the Comparative Effectiveness of Revascularization Strategies Trial (ASCERT) used data from the American College of Cardiology PCI registry and the Society of Thoracic Surgery CABG registry to compare adjusted long-term survival in SIHD patients over the age of 65 treated between 2004 and 2007 with PCI (n = 103,549) or CABG (n = 86,244) and showed lower 4-year mortality with CABG (16.4 vs 20.8%; risk ratio, 0.79; 95% CI, 0.76 to 0.82) [21].
Although interpretation of registry data is confounded by numerous considerations, including selection bias and unmeasured co-variables, randomized trials in high-risk subgroups support the registry evidence in support of a survival benefit with CABG. For example, the Bypass Angioplasty Revascularization Investigation (BARI) trial found that in patients with diabetes treated with CABG versus percutaneous transluminal coronary balloon angioplasty (PTCA), there was a higher survival in the CABG group than in the PTCA group (57.5% CABG vs 45.5% PTCA, p = 0.025) [22]. The data in high-risk subgroups remain consistent even in the current era of contemporary surgical and percutaneous interventional techniques, including drug-eluting stents. The multicenter randomized trial, Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multi-Vessel Disease (FREEDOM), enrolled 1900 patients with diabetes and angiographically confirmed multivessel coronary artery disease with a diameter stenosis of 70% or more in two or more epicardial vessels and found that revascularization with CABG numerically decreased mortality [23]. The 5-year rates of death from any cause were 10.9% in the CABG group compared to 16.3% in the PCI group (p = 0.049) [23]. The 5-year follow-up of the multicenter Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX) trial of 1800 patients found that the major adverse cardiovascular and cerebrovascular effects were lower in patients with complex coronary stenosis (moderate to high SYNTAX scores) who underwent CABG compared to PCI (26.9 vs 37.3%, p ≤ 0.0001). Although there was no mortality benefit seen in those patients randomized to undergo CABG, the trial was underpowered to detect this difference [24•]. Sipahi et al. recently published a meta-analysis of 6055 patients randomized to either CABG or PCI for multivessel disease and showed a significant reduction in mortality with CABG as compared to PCI (risk ratio 0.73 [ 95% CI 0.62–0.86], p < 0.01) [25•]. It is important to note that up to one third of the patients included in the BARI, FREEDOM, and SYNTAX trials had acute myocardial infarction or unstable angina, and, therefore, the benefits seen in these trials are partially due to the inclusion of this subset of patients with higher risks of future adverse cardiac events than SIHD patients alone. Furthermore, the mortality benefits of CABG are relatively modest and must be balanced by consideration of the more invasive nature of CABG and the morbidities associated with CABG including an excess risk of stroke. As seen in both FREEDOM (1.8 vs 0.3%, p = 0.002) and SYNTAX trial (2.2 vs 0.6%, p = 0.003), there was a significant incidence of stroke in CABG patients [23, 24•].
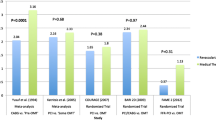
Effects of Coronary Revascularization on Survival in SIHD: Medical Therapy versus PCI
Early studies, including the Second Randomized Intervention of Angina (RITA II), Angioplasty Compared to Medicine (ACME), and Atorvastatin versus Revascularization Treatments (AVERT), compared medical therapy to PCI and showed that PCI helped relieve anginal symptoms and increased exercise capacity [26,27,28]. Keeping in mind that the medical therapy in these trials was not reflective of currently defined OMT, with only a small percentage of patients receiving anti-platelet therapy, and PCI consisted predominantly of PTCA, there was, overall, no survival benefit with PCI [29, 30].
The COURAGE and BARI-2D trials are the two major landmark contemporary clinical trials that compared OMT alone with OMT and upfront coronary revascularization, which included PCI, in patients with SIHD. The COURAGE trial was a multicenter trial of 2287 patients that enrolled SIHD patients with diameter stenosis of 70% or more in at least one epicardial coronary artery and evidence of myocardial ischemia on stress testing, or at least one coronary diameter stenosis of 80% or more and typical angina without provocative testing [1]. Medical therapy provided was truly optimal with all patients receiving antiplatelet and low-density lipoprotein-lowering medications along with aggressive treatment of hypertension and diabetes. The primary endpoint, a composite of all-cause mortality and nonfatal myocardial infarction after 4.6-year follow-up occurred in 18.5% of the OMT group and 19.0% of the PCI group (p = 0.62). The study concluded that a routine initial strategy of revascularization with PCI did not improve survival [1]. As noted in the “Introduction,” recently published 15 years follow-up from patients enrolled in the COURAGE trial continued to show no difference in overall mortality between the two groups [3••].
The BARI-2D, was a 2 × 2 multicenter randomized trial that assigned 2368 patients with both type 2 diabetes mellitus and SIHD to undergo either OMT alone or OMT and upfront revascularization with PCI or CABG and to receive insulin sensitization versus insulin provision therapy [2]. After 5-year follow-up, the rate of survival between the revascularization group and the medical therapy group did not differ significantly (87.8% in the OMT group vs 88.3% in the revascularization group, p = 0.97). There was a statistically significant reduction in major adverse cardiovascular events in those patients who underwent CABG versus those that were treated with OMT alone. However, there was no difference in terms of overall survival [2]. Table 1 summarizes key findings from trials comparing medical therapy versus PCI.
Possible Deleterious Effects of Inappropriate PCI
It is possible that deleterious effects (such as stent thrombosis) of inappropriate PCI could have adverse effects on survival. The Fractional Flow Reserve versus Angiography for Guiding Percutaneous Coronary Intervention (FAME) trial was an international multicenter study of 1005 patients with ischemic heart disease randomized to PCI guided by angiography or by measurement of fractional flow reserve (FFR) [31]. At 12 months follow-up, the primary endpoint of death, myocardial infarction and repeat revascularization occurred in 18.3% of the angiography group and 13.2% of the FFR group (p = 0.02). The benefit of FFR-guided PCI persisted with longer term follow-up to 24 months [32]. The FAME trial showed that there may be detrimental effects to intervening on nonobstructive coronary lesions. The FAME authors hypothesized in their discussion that the results obtained in COURAGE, BARI-2D, and SYNTAX may partly be due to the harmful effects of unnecessary PCI [31]. The follow-up Fractional Flow Reserve versus Angiography for Multivessel Evaluation 2 (FAME 2) trial randomized 888 patients with SIHD and a significant coronary stenosis defined as FFR ≤0.80 to either OMT alone or OMT with PCI [33]. The trial was stopped prematurely because of a significant reduction in the primary endpoint of death from any cause, nonfatal myocardial infarction, or unplanned hospitalization leading to urgent revascularization during the first 2 years with PCI (12.7% in the OMT group vs 4.3% in the OMT with PCI group, p ≤ 0.001). However, the benefit was driven completely by differences in urgent revascularization, which was a rather subjective endpoint given that providers were aware of the FFR data. The overall incidence of death and myocardial infarction were low and similar in both groups (one death in the PCI group vs three deaths in the OMT group) [33]. Despite the evidence supporting an FFR-guided strategy, providers are still reluctant to use this approach [34].
Effect of Evolving Revascularization Techniques
Coronary revascularization techniques continue to evolve, and older trials may not address the possible survival benefits of newer technologies. Only 13% of the patients in the European Coronary Surgery Study who underwent CABG received left internal mammary artery grafts [15]. In the VA cooperative study, the 30-day operative mortality rate was quite high at 5.8% and the overall graft patency rate at 1 year was only 70% [14]. Over 90% of the patients in the PCI stratum of COURAGE received bare metal stents, and 56% of patients in BARI 2D received bare metals stents while the other half received first-generation drug-eluting stents.
Multiple randomized trials as well as meta-analyses have shown superiority of second-generation drug-eluting stents, which have now become the standard of care in most cardiac catheterization laboratories [35, 36]. A recently published meta-analysis by Windecker et al. of 100 trials with 93,553 patients undergoing revascularization by CABG or PCI showed an improvement in survival as compared to medical therapy (rate ratio 0.80, 95% CI 0.70 to 0.91). The analysis demonstrated the improvement of survival to be greatest in the groups undergoing CABG or PCI with newer second-generation drug-eluting stents (Everolimus, 0.75, 0.59 to 0.96; Zotarolimus, 0.65, 0.42 to 1.00) [37•]. On the other hand, the very recently published NORSTENT trial randomized 9013 patient to PCI with second-generation drug-eluting stents versus bare metal stents. The rate of the primary composite outcome of death from any cause and nonfatal spontaneous myocardial infarction at 6 years was 16.6% for drug-eluting stents versus 17.1% for bare metal stents (p = 0.66) [38]. These results support the relevance of the COURAGE and BARI 2D findings to contemporary PCI and imply that it is unlikely that newer drug-eluting stents improve survival in SIHD.
Possible Survival Benefits of Coronary Revascularization in Higher Risk Subsets of SIHD
Left Main Disease
Patients with SIHD and significant left main coronary artery disease (greater than 50% diameter stenosis) are a subgroup of patients with worse overall outcomes compared to other patients with SIHD. The CASS Registry included 23,467 patients with angiographically proven coronary artery disease that were followed-up for 0 to 17 years [39]. The survival at 12 years of patients with two vessel disease who were initially treated with medical management was lower in those with versus without left main involvement (49 vs 60%). The survival rate further decreased in medically managed patients with three-vessel disease with versus without left main disease (35 vs 41%, p = 0.001). In addition, a subgroup analysis of the VA Cooperative Study of Surgery for Coronary Arterial Occlusive Disease showed that there was a survival benefit with CABG in 91 patients with significant left main stenosis randomized to CABG versus OMT (88 vs 65%, p = 0.016). The study found that patients with left ventricular dysfunction and left main diameter stenosis greater than 75% benefited the most from CABG( 89% survival with CABG vs 62% with OMT, p = 0.012) [40]. Similarly, an observational report of 1492 patients from the CASS Registry with left main disease showed a survival benefit of 91% in patients who underwent CABG versus 69% in those treated medically [41]. These early studies demonstrate that patients with severe left main stenosis have a survival benefit with revascularization versus medical therapy, and provide the basis for the American College of Cardiology/American Heart Association guidelines’ class I recommendation for revascularization of unprotected left main disease to improve survival for patients with SIHD [42]. Of note, there are no data from randomized trials comparing outcomes with OMT versus PCI in left main patients, and any beneficial effects of PCI on survival in SIHD patients with left main disease is speculative.
Reduced Left Ventricular Ejection Fraction
Low left ventricular ejection fraction (≤35%) in SIHD patients carries a poor prognosis and subgroup analysis from early trials first demonstrated a decrease in cardiovascular mortality with OMT and revascularization by CABG versus OMT alone [43••, 44, 45]. The Surgical Treatment for Ischemic Heart Failure (STITCH) trial, a prospective randomized control trial of patients with a left ventricular ejection fraction of less than or equal than 35%, concluded there was no significant difference in the rate of all-cause mortality between patients randomized with OMT and CABG versus OMT alone at a mean follow-up of 56 months [46]. Very recently extended follow-up (median 9.8 years) of the STITCH trial demonstrated a survival benefit for CABG (hazard ratio, 0.72; 95% CI, 0.64 to 0.82; p < 0.001 by log-rank test) [47]. As pointed out by the authors, however, it is unknown whether PCI compared to medical therapy would result in a similar benefit.
Documented Ischemia
Although COURAGE, BARI 2D, and FAME 2 showed no mortality benefit to routine revascularization, various meta-analyses have shown that there may be some survival benefit to initial revascularization strategy in SIHD patients with documented ischemia. A meta-analysis of three randomized trials including 1557 patients with documented myocardial ischemia by noninvasive imaging or abnormal FFR followed for an average of 3 years demonstrated that a strategy of initial PCI plus medical therapy versus medical therapy alone was associated with a reduction in mortality (HR, 0.52, 95% CI, 0.30–0.92; p = 0.02) [43••].
Moderate to Severe Reversible Ischemia
A critique of COURAGE and BARI2D is that they included patients with either angina without objective evidence of ischemia or evidence of mild ischemia on single photon emission computed tomography (SPECT) scan. The overall event rates were relatively low reflective of the fact that these randomized trials may have evaluated a lower risk population. Therefore, we still do not truly know whether patients with moderate to severe ischemia would benefit from an initial strategy of PCI with OMT. A COURAGE pre-specified substudy of 324 patients who underwent serial myocardial perfusion single photon emission tomography (MPS) showed that initial PCI added to OMT resulted in a higher percentage of patients with a significant reduction in ischemia versus OMT alone (33 vs 19%). This was particularly seen in patients with moderate to severe ischemia at baseline. The authors were also able to conclude that a significant reduction in ischemia was associated with lower all-cause mortality [4]. As this was a pre-specified substudy of a negative trial, this was only meant to be hypothesis generating. On the other hand, a retrospective post hoc analysis of all COURAGE patients who underwent baseline SPECT scan did not show any association between severity of ischemia and outcomes [48]. Another retrospective study of 10,627 patients undergoing exercise or adenosine stress MPS by Hachamovitch et al. showed that an initial revascularization strategy reduced the absolute and relative risk of cardiac death in patients with moderate to severe ischemia compared to those treated with medical therapy alone [5]. A retrospective Japanese multicenter study of 4629 patients with SIHD observed that patients with >10% ischemic myocardium had lower cardiac event rates when undergoing early revascularization compared to those that did not (0 vs 12.3%, p = 0.0062) [49].
The ISCHEMIA trial is an ongoing international randomized trial comparing the effectiveness of OMT plus revascularization versus OMT alone in SIHD patients with moderate to severe ischemia on noninvasive stress testing [6]. The primary endpoints are cardiovascular death or nonfatal myocardial infarction compared to an initial strategy of OMT alone. Patients that meet inclusion criteria and do not already have a diagnostic coronary angiogram at baseline undergo blinded coronary computed tomography angiography to exclude left main disease and confirm the presence of obstructive coronary artery disease prior to randomization. Of these patients, only those assigned to an initial revascularization strategy go on to coronary angiography.
Conclusions
Numerous randomized clinical trials have shown that an initial strategy of PCI has no effect on survival in SIHD when compared to an initial strategy of OMT alone. This is not surprising since subsequent cardiac events after PCI are largely caused by unstable plaque in an area outside of the originally stented segment. However, these trials also had overall relatively low event rates given the inclusion of lower risk patients. The data suggests that revascularization with CABG may have some survival benefit in high-risk patient populations prone to future adverse events since bypass grafts protect the distal myocardium from ischemia caused by proximal acute plaque rupture. Similarly, observational trials suggest that PCI may benefit patients with a large ischemic burden. The ISCHEMIA trial, the largest trial to date addressing OMT alone versus OMT with coronary revascularization, is designed to evaluate the possible benefit of upfront coronary revascularization in SIHD patients with a large ischemic burden. It is possible that ISCHEMIA may show that PCI has a survival benefit in the high-risk population with at least moderate ischemia, but given the robust data of past trials showing that PCI does not improve survival, and the likelihood that the highest risk patients in ISCHEMIA will be treated with CABG, it is unlikely that the ISCHEMIA trial will provide conclusive evidence in favor of PCI.
References
Papers of particular interest, published recently, have been highlighted as: •Of importance ••Of major importance
Boden W, et al. Optimal medical therapy with or without PCI for stables coronary disease. N Engl J Med. 2007;356(15):1503–16.
The BARI 2D Study Group. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med. 2009;360(2503):2515.
•• Sedlis SP, et al. Effect of PCI on long-Tem survival in patients with stable ischemic heart disease. N Engl J Med. 2015;373:1937–46. Long-term follow-up of the COURAGE trial (0-15 year, median 11.9 years) with total of 561 deaths found no difference in survival between OMT and PCI groups.
Shaw L, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation. 2008;117(10):1283–91.
Hachamovitch R, et al. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107:2900–7.
www.ischemiatrial.org. Last Accessed 8/17/2016
O’Brien KD, et al. Comparison of apolipoprotein and proteoglycan deposits in human coronary atheroslerotic plaques: colocalization of biglycan with apolipoproteins. Circulation. 1998;98:519–27.
Virmani R, et al. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Bio. 2000;20(5):1262.
Crisby M, et al. Pravastatin treatment increases collagen content and decreases lipid content, inflammation, metalloproteinases, and cell death in human carotid plaques: implications for plaque stabilization. Circulation. 2001;103(7):926.
Stone GW, et al. Prospect study: a prospective natural-history study of coronary atherosclerosis. PROSPECT investigator. N Engl J Med. 2011;364(3):226.
Ambrose JA, et al. Angiographic progression of coronary artery disease and the development of myocardial infarction. J Am Coll Cardiol. 1988;12(1):56–62.
Little WC, et al. Can coronary angiography predict the site of a subsequent myocardial infarction in patients with mild-to-moderate coronary artery disease? Circulation. 1988;78(5 Pt 1):1157–66.
Mancini GBJ, et al. Angiographic disease progression and residual risk of cardiovascular events while on optimal medical therapy: observations from the COURAGE trial. Circ Card Int. 2011;4(6):545–52.
The Veterans Administration Coronary Artery Bypass Surgery Cooperative Study Group. Eleven year survival in the veterans administration randomized trial of coronary bypass surgery for stable angina. N Engl J Med. 1984;311:1333–9.
European Coronary Surgery Study Group. Long-term results of a prospective randomised trial of coronary artery bypass surgery in stable angina pectoris. Lancet. 982;1173–1180
Chaitman BR, et al. Coronary Artery Surgery Study (CASS): comparability of 10 year survival in randomized and randomizable patients. J Am Coll Cardiol. 1990;16:1071–8.
CASS Principal Investigators and Their Associates. Coronary Artery Surgery (CASS): a randomized trial of coronary artery bypass surgery. Survival data. Circulation. 1983;68:939–50.
Rihal CS, Raco DL, Gersh BJ, Yusuf S. Indications for coronary artery bypass surgery and percutaneous coronary intervention in chronic stable angina: review of the evidence and methodological considerations. Circulation 2003;108:2439–2445.
• Garcia S, et al. Outcomes after complete versus incomplete revascularization of patients with multivessel coronary artery disease: a meta-analysis of 89,883 patients enrolled in randomized clinical trials and observational studies. J Am Coll Cardiol. 2013;62(16):1421–31. Meta-analysis of 35 studies including 89,883 patients which compares complete revascularization versus incomplete revascularization by CABG or PCI in patients with multivessel CAD. Approximately half of the two groups received complete revascularization and the other half received incomplete revascularization. Most patients that were revascularized by CABG achieved complete versus those that were revascularized by PCI.
Hannan EL, et al. Drug-eluting stents vs coronary-artery bypass grafting in multivessel coronary disease. N Engl J Med. 2008;358:331–4.
Weintraub WS, et al. Comparative effectiveness of revascularization strategies. N Engl J Med. 2012;366:1467–76.
BARI investigators. The final 10-year follow-up results from the BARI randomized trial. J Am Coll Cardiol. 2007;49(15):1600–6.
Farkouh ME, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012;367:2375–84.
• Mohr FW, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5 year follow-up of the randomized, clinical SYNTAX trial. Lancet. 2013;381(9867):629–38. Report of the 5 year follow-up of the SYNTAX trial, compared CABG with PCI for the treatment in patients with left main coronary disease or three vessel disease. This multicentered trial of 1800 patients randomly assigned patients to either CABG group or PCI group. After 5 year follow it was found that major adverse cardiac and cerebrovascular events were lower in the CABG versus the PCI group (26.9% vs 37.3%). This study determined that CABG should remain the standard of care in patients with complex lesions, determined by high or intermediate SYNTAX scores. For patients with low SYNTAX scores PCI was determined to be an acceptable alternative.
• Sipahi I, et al. Coronary artery bypass grafting vs percutaneous coronary intervention and long-term mortality and morbidity in multivessel disease. JAMA Intern Med. 2014;174(2):223–30. Meta-analysis of 6 randomized trials totaling 6055 patients set out to determine the comparative effects of CABG vs PCI on long term mortality and morbidity in patient with multivessel disease. This study concluded that in patients with multivessel disease, CABG compared to PCI results in a reduction in long-term mortality and myocardial infarction.
RITA-2 participants. Coronary angioplasty versus medical therapy for angina: the second Randomised Intervention Treatment of Angina (RITA-2) trial. Lancet. 1997;350(9076):461–8.
Folland ED, et al. Percuatneous transluminal coronary angioplasty versus medical therapy for stable angina pectoris: outcomes for patients with double-vessel versus single-vessel coronary artery disease in a Veterans Affairs Cooperative randomized trial. J Am Coll Cardiol. 1997;29(7):1505–11.
Pitt B, et al. Aggressive lipid-lowering therapy compared with angioplasty in stable coronary artery disease. N Engl J Med. 1999;341:70–6.
Henderson RA, et al. Second Randomized Intervention Treatment of Angina (RITA-2) trial participants. Seven-year outcome in the RITA-2 trial: coronary angioplasty versus medical therapy. J Am Coll Cardiol. 2003;42(7):1161–70.
Hartigan PM, Giacomini JC, Folland ED, Parisi AF. Two to three year follow-up of patients with single-vessel coronary artery disease randomized to PTCA or medical therapy (results of a VA cooperative study). Am J Cardiol. 1998;82(12):1445–50.
Tonino PA, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213–24.
Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary disease; 2 year follow up of the FAME study. J Am Coll Cardiol. 2010;56:177–84.
De Bruyne B, Pijls NHJ, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012;367:991–1001.
Sedlis SP, et al. Percutaneous coronary intervention: FAME is lasting. Lancet. 2015;386(10006):1806–7.
Bangalore S, et al. Short and long term outcomes with drug-eluting and bare metal coronary stents: a mixed treatment comparison analysis of 117 762 patients years of follow up from randomized trials. Circulation. 2012;125(23):2873.
Applegate RJ, et al. Long term ( three year) safety and efficacy of everolimus-eluting stents compared to paclitaxel- eluting stents ( from the SPIRIT III Trial). Am J Cardiol. 2011;107(6):833–40.
• Windecker S, Stortecky S, Juni P. Revascularisation versus medical treatment in patients with stable coronary artery disease: network meta-analysis. BMJ. 2014;348:3859. Meta-analysis of 100 trials totaling 93,553 which compares whether revascularization improves prognosis compared to medical treatment among patients with stable coronary artery disease. Among the patients with stable CAD, it was found that CABG reduces the risk of death, MI and revascularization compared to medical treatment.
Bonaa KH, Mannsverk J, Wiseth, R. et al, Drug-eluting or bare-metal stents for coronary artery disease. N Engl J Med. 2016;375:1242–1252.
M Emond, M.B Mock, K.B Davis, et al. Long-term survival of medically treated patients in the Coronary Artery Surgery Study (CASS) Registry. Circulation. 1994;90:2645–2657
Takaro T, Peduzzi P, Detre KM, et al. Survival in subgroups of patients with left main coronary artery disease. Veterans Administration Cooperative Study of Surgery for Coronary Arterial Occlusive Disease. Circulation. 1982;66:14–22.
Chaitman BR, et al. Effect of coronary bypass surgery on survival patterns in subsets of patients with left main coronary artery disease. Report of the Collaborative Study in Coronary Artery Surgery (CASS). Am J Cardiol. 1981;48(4):765.
Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines, and the American Collegge of Physicians, American Association for Thoracic Surgery, Preventative Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012; 126:e354–471.
•• Gada H, et al. Meta-analysis of trials on mortality after percutaneous coronary intervention compared with medical therapy in patients with stable coronary heart disease and objective evidence of myocardial ischemia. Am J Cardiol. 2015;115(9):1194–9. Meta-analysis of 3 randomized clinical trials totaling 1,557 patients comparing PCI with OMT in patients with documented myocardial ischemia set out to find out if those with objective ischemia would benefit from PCI versus OMT alone. PCI with OMT compared to OMT alone was associated with a reduction in mortality in RCTs that enrolled patients with objective evidence of ischemia using noninvasive stress imaging or abnormal FFR. In PCI plus MT versus MT alone 3.0% versus 5.9% of the patients died. In the analysis of pooled HR, a significant reduction in all-cause mortality was 0.52.
Velazquez EJ, et al. Long-term survival of patients with ischemic cardiomyopathy treated by coronary artery bypass grafting versus medical therapy. Ann Thorac Surg. 2012;93:523–30.
O’Connor CM, et al. Comparison of coronary artery bypass grafting versus medical therapy on long-term outcome in patients with ischemic cardiomyopathy (a 25-year experience from the Duke Cardiovascular Disease Databank). Am J Cardiol. 2002;90:101–7.
Velazquez EJ, for the STICH Investigators, et al. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med. 2011;364:1607–16.
Velasquez EJ, et al. Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med. 2016;374:1511–20.
Shaw LJ, et al. Baseline stress myocardial perfusion imaging results and outcomes in patients with stable ischemic heart disease randomized to optimal medical therapy with or without percutaneous coronary intervention. Am Heart J. 2012;164:243–50.
Moroi M, et al. Coronary revascularization does not decrease cardiac events in patients with stable ischemic heart disease but might do in those who showed moderate to severe ischemia. Int J Cardiol. 2012;158:246–52.
Acknowledgments
Binita Shah was supported in part by the Biomedical Laboratory Research & Development Service of the VA Office of Research and Development (I01BX007080).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Francisco Ujueta, Ephraim N. Weiss, Binita Shah, and Steven P. Sedlis declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Ischemic Heart Disease
Rights and permissions
About this article
Cite this article
Ujueta, F., Weiss, E.N., Shah, B. et al. Effect of Percutaneous Coronary Intervention on Survival in Patients with Stable Ischemic Heart Disease. Curr Cardiol Rep 19, 17 (2017). https://doi.org/10.1007/s11886-017-0821-6
Published:
DOI: https://doi.org/10.1007/s11886-017-0821-6