Abstract
The United States Food and Drug Administration has approved the wearable cardioverter defibrillator (WCD) for use in patients who are at high risk for sudden cardiac arrest (SCA) and who do not yet have an established indication for an implantation cardioverter defibrillator (ICD) or have contraindications for device implantation for various reasons. The WCD is typically used for primary prevention in (1) high-risk patients with reduced left ventricular ejection fraction (LVEF) ≤35 % after recent acute myocardial infarction (MI) during the 40-day ICD waiting period, (2) before and after coronary artery bypass graft or percutaneous coronary intervention during the 90-day ICD waiting period, (3) after recently diagnosed nonischemic dilated cardiomyopathy (NICM) during the 3- to 9-month medical therapy optimization period, or (4) for those with inherited proarrhythmic conditions such as long QT syndrome or hypertrophic cardiomyopathy. Unlike the automatic external defibrillator, the WCD does not require assistance from bystanders for therapy and conscious patients can delay or avert therapy with the use of response buttons. The WCD exhibits a small risk of inappropriate shock, mostly due to supraventricular tachycardia and/or electrical noise. Multiple non-randomized observational studies have shown high efficacy in detection and appropriate shock therapy for sustained ventricular tachyarrhythmias. This paper discusses the use of the WCD for prevention of SCA in patients with various cardiac substrates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last three decades, the survival of patients who are at high risk for life-threatening ventricular tachyarrhythmias has been enhanced with the use of implantable cardioverter defibrillators (ICDs) [1, 2]. Still, large numbers of high-risk patients fall outside of ICD indications, and sudden cardiac arrest (SCA) continues to be a major cause of mortality in the USA. The incidence of out-of-hospital cardiac arrest in 2014 was about 424,000 according to the American Heart Association [3]. In a multicenter observation study of out-of-hospital cardiac arrest (20,520 cardiac arrests) in North America, 22.9 % of 11,898 patients who had attempted resuscitation had VT/VF or shockable rhythm by automated external defibrillator [4]. Overall survival ranged from 3 to 16.3 % with a median of 8.4 % in the emergency medical service (EMS) treated out-of-hospital cardiac arrests. If the initial rhythm was VF, survival ranged from 7.7 to 39.9 % with a median of 22 %. Among EMS-treated out-of-hospital arrest, majority (45.4 %) were unwitnessed, 37 % were witnessed by bystanders and only 9 % by EMS personnel. Lack of access to or skill to use automated external defibrillator at the site by the bystander, delay in emergency services reaching the site, or delay in initiating cardiopulmonary resuscitation can reduce survival by 7 to 10 % with each passing minute after cardiac arrest [5]. Ischemic heart disease (most common), nonischemic dilated cardiomyopathy (NICM), hypertrophic cardiomyopathies, congenital heart disease, and genetically determined channelopathies are known to be associated with increased risk of SCA. For those patients that have already been identified as high risk for out-of-hospital cardiac arrest but are not yet candidates for and/or refuse an ICD, the wearable cardioverter defibrillator (WCD) is an additional option for prophylaxis.
History of the WCD
In December 2001, the LifeVest® wearable cardioverter defibrillator (ZOLL, Pittsburgh, USA) was FDA approved and remains the only commercially available WCD. The device is currently available in the USA, Europe, Australia, Israel, Japan, and Singapore. The most recent version is the WCD 4000 (shown below). In 2015, the FDA approved the WCD for use in children as well, provided that they meet a certain size criteria for a proper fit.
Device Description
The device total weight is 1.5 kg. as shown in Figs. 1 and 2. The WCD consists of wearable (Table 1) and non-wearable components (Table 2) [6].
Device Function
The WCD is a programmable device that monitors the patient, detects life-threatening ventricular tachyarrhythmias, and delivers treatment (cardioversion or defibrillation). There are four sensing electrodes placed against the patient’s chest to monitor ECG signals whereby arrhythmia events are detected, recorded, and stored for later adjudication. Once a malignant arrhythmia is recognized, a series of alarms are initiated.
First, the device alerts the patient using different modalities (vibration, display messages, alarm voice). A conscious patient has the option to abort the defibrillating pulse by pressing the response buttons over a period of approximately 25 s [7]. If response buttons are not used, electrical shock therapy will be delivered typically within 60 s of arrhythmia onset Fig. 3. Median time from arrhythmia to treatment is about 45 s.
In order to maintain effective monitoring and timely therapy, the device should be worn continuously except when bathing.
Some additional key points about the WCD include (1) the WCD effectively terminates VT/VF episodes and it can be programmed to different VT or VF rate thresholds (typically 150 and 200 BPM, respectively [7], (2) the WCD treats VT/VF with a biphasic shock that is programmable between 75 and 150 J [8], and (3) the WCD will alarm for severe bradyarrhythmias and asystole but it cannot provide pacing therapy.
Indication/Guidelines in Perspective
The LifeVest was FDA approved based on the WEARIT/BIROAD study that included 289 patients [9]. At this time, there are no completed randomized controlled trials. Based on current consensus statement from HRS/ACC/AHA 2014, the WCD is an option prior to an ICD implantation decision for selected patients at high risk of sudden cardiac death due to ventricular tachyarrhythmias [10]. The following situations may be considered for WCD use [11]:
-
1.
Reversible arrhythmic conditions such as myocarditis
-
2.
Potentially reversible cardiomyopathy when left ventricular function might improve such as newly diagnosed cardiomyopathy (ischemic/nonischemic) or after myocardial infarction (MI)
-
3.
ICD re-implantation delays after ICD explantation (e.g., for infection) or implantation delays due to comorbid conditions
-
4.
Transient sudden death risk such as pre-cardiac transplantation
-
5.
Prior to ICD decision for inherited arrhythmogenic conditions
WCD in Ischemic Heart Disease
Each year, an estimated 635,000 Americans are hospitalized due to MI or have a coronary heart disease death; one of every seven deaths is caused by coronary artery disease [3]. A community-based retrospective study of 2280 patients in a Midwest county (1979–1998) showed 7.5 % patients with acute MI experienced ventricular arrhythmias, most (78 %) during the first 48 h after the onset of ischemic symptoms [12]. VF occurred in 2.1 % within 48 h, 3.6 % of patients after 48 h, and ventricular tachyarrhythmia in 1.8 % of the patients. Patients who had any ventricular arrhythmia had lower left ventricular ejection fraction (LVEF), 30-day case fatality rates of 38 versus 9 % for patients who experienced none. Patients who have VF or VT after 48 h had higher 30-day case fatality rate (47 and 44 %, respectively) compared to 19 % in ventricular fibrillation before 48 h. During analysis of 40,895 patients enrolled in the Global Use of Streptokinase tPA for occluded coronary arteries (GUSTO-1) trial, 10.2 % had significant sustained ventricular tachyarrhythmias (Newby et al., 1998). Patients who had VT only, VF only, or both VT/VF had higher in-hospital mortality rates (18.6, 24 %, and 44 %, respectively) and 30-day mortality rates (18.3, 23.99, and 44.5 %, respectively) than patients without ventricular tachyarrhythmias (in-hospital mortality: 4.2 %; 30-day mortality: 4.6 %). A community-based registry (1990 to 2010) from Olmsted County shows that 34 % of patients develop new heart failure (HF), 47 % developed within 3 days and 62 % had reduced ejection fraction [13].
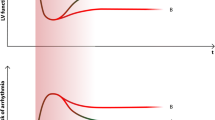
Though improvements in pharmacological and invasive strategies have shown significant reduction in mortality after MI, still, 19.6 % had HF with mortality of 11.7 % in the first 90 days based on a Danish registry of 89,389 patients [14]. The VALIANT study (Solomon et al., 2005) showed that patients with reduced systolic function (especially ≤30 %) are at highest risk for sudden cardiac death in the first 30 days after MI, with an incidence rate of 1.4 % during the first month then dropping to 0.5 % per month in the months that follow.
MADIT, MADIT II, SCD-HeFT, and MUSTT have shown survival benefit with ICD therapy after myocardial infarction with reduced left ventricular function [15–18]. These studies form the basis for current guidelines on the ICD implantation but these studies used slightly different LVEF cutoffs (EF ≤35 % in MADIT and SCD-HeFT, EF ≤30 % in MADIT II, and EF ≤40 % in MUSTT) and timing of ICD implantation (MADIT >3 weeks after MI, >2 months after CABG, >3 months after percutaneous coronary angioplasty; SCD-HeFT >3 months HF; MADIT II >1 month after MI infarction and >3 months after revascularization; MUSTT ≥4 days after myocardial infarction).
Two randomized trials evaluated the benefit of the ICD early after MI when the risk of mortality is known to be high. However, in DINAMIT, prophylactic use of the ICD in post-acute MI patients with LVEF ≤35 % failed to show mortality benefit during an observation period of 30 months [19]. This finding was later confirmed by the IRIS trial, which included patients with LVEF ≤40 % [20]. Both trials had a significantly lower risk of death from arrhythmia that was counterbalanced by an increased risk of non-arrhythmic causes of death. Speculations on why these trials were negative include competing risks of death, use of inclusion criteria that selected away from sudden death (depressed heart rate variability in DINAMIT, heart rate in IRIS), insufficient power in the trial design, and the play of chance.
The third randomized trial that failed to show a survival benefit for ICD implantation in patients with reduced LVEF was CABG-Patch [21]. This trial randomized subjects to ICD therapy with epicardial patches or no ICD at the time of CABG surgery and included the additional criterion of abnormalities on signal averaged electrocardiograms. Recovery of significant LVEF following surgery may have contributed to the failure to show benefit.
Current guidelines recommend a waiting period of 40 days after acute MI and 90 days after CABG or percutaneous coronary intervention before ICD implantation in patients with reduced LVEF (≤35 %) for primary prevention of SCA. Despite this, patients continue to be at high risk for sudden death from ventricular arrhythmia in the early post-MI phase. Since there is no established benefit from ICD implantation, the WCD is the only currently available noninvasive device that can prevent ventricular tachyarrhythmia-related death during this interim period until the indication for an ICD can be established. The ongoing Vest Prevention of Early Sudden Death Trial and VEST Registry (NCT01446965) is expected to give us insight into the impact of WCD use on mortality from sudden cardiac death in the first 3-month post-MI.
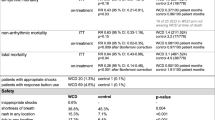
Current evidence regarding the benefit of WCD use in ischemic heart disease comes from observational studies. The WEARIT/BIROAD trial studied the role of WCD in patients with symptomatic HF with EF <30 % (177 patients in WEARIT) or patients having complications associated with high risk for sudden death after a MI or bypass surgery not receiving an ICD for up to 4 months (112 patients in BIROAD Study) [9]. Six (75 %) of eight defibrillation attempts were successful. Six of 289 patients experienced an unnecessary shock for an incidence rate of 0.67 % per month of patient use. Reek et al. reported on an observational study from Germany (1998–2001) that included 84 patients, predominantly patients with acute MI or recent CABG surgery, or waiting heart transplant [22]. Five patients had seven episodes of ventricular tachyarrhythmia successfully terminated with WCD. In 9720 total days of WCD use, one patient had an inappropriate shock due to oversensing of electrical noise.
A US-based national registry (2002–2006) showed WCD use in 3569 patients, of which recent MI and post-CABG with LVEF ≤35 % contributed to 12.5 and 8.9 % of users, respectively [23]. Inclusive of all other indications for WCD, first shock was successful in 76/76 (100 %) for unconscious VT/VF and 99 % for all VT/VF. Eight patients died after successful conversion of unconscious VT/VF. Survival occurred in 73.6 % of events and in 90 % of VT/VF events. Compliance was satisfactory with 90 % wear time in >50 % of patients, and survival was comparable to that of ICD patients from the national registry. Average use was 20 ± 3.7 h per day for patients using device >60 days (599 patients) and 17.2 ± 5.9 h for patients using less than 15 days (160 patients). During WCD period, 80 sustained VT/VF (1.7 %). Patients with LVEF ≤35 % with recent MI, post-CABG, recent NICM had statistically significant lower mortality compared to those with traditional indications of ICD. There was no significant difference between WCD and ICD patients (prospectively collected data from the Cleveland Clinic) at 3-month and 3-year follow-up. These findings suggest that the WCD is an acceptable bridge to permanent prophylaxis with an ICD.
Klein et al.’s retrospective review of 354 WCD users from Germany included 39 % early acute MI patients complicated by LVEF ≤35 % within 2 days of acute percutaneous revascularization, early (≤24 h) after survival from an aborted ventricular tachyarrhythmia, or acute pulmonary edema [24]. Twenty-nine percent of patients included post-CABG with reduced LVEF, prolonged and difficult postoperative hemodynamic recovery, or early postoperative life-threatening ventricular tachyarrhythmias. Two hundred twenty-eight episodes of sustained VT/VF events were observed in 7.6 % of patients. Out of these, 139 episodes occurred in type 2 LQT syndrome; all but six episodes terminated spontaneously while withholding the shock. In 20 of 21, treated VT/VF, the first discharge was successful (95 % success). Only three inappropriate shocks were delivered because of electrical noise.
A retrospective observational study of post-revascularization (CABG surgery or percutaneous coronary revascularization) patients with LVEF ≤35 % from the Cleveland Clinic and national WCD registries showed better survival in the WCD group compared with the no-WCD group (HR, 0.54; 95 % CI, 0.43–0.68; P < 0.0001) in the first 90 days [25••]. Zishiri et al. showed higher mortality (7 % for post-CABG and 10 % post-percutaneous coronary intervention) among 4149 patients discharged without a defibrillator compared to 809 discharged with a WCDs (90-day mortality post-coronary artery bypass graft surgery 3 and 2 % post-PCI).
Another retrospective study of the WCD registry data in early post-MI patients with reduced LVEF ≤35 % during 90-day wear period showed 1.6 % (133/8453) of patients received appropriate shocks and 91 % of these patients were resuscitated from a ventricular arrhythmia [26•].
Nonischemic Dilated Cardiomyopathy
Nonischemic dilated cardiomyopathy (NICM) is characterized as having a dilated left ventricle with systolic dysfunction without significant coronary artery disease. NICM is frequently classified by etiology such as alcohol-, chemical-, infection-, or tachycardia-induced or peripartum cardiomyopathy (PPCM) or takotsubo cardiomyopathy (TCM) [27]. At the onset, cardiomyopathies may be asymptomatic but the risk of ventricular arrhythmias is high in this population and could be the initial presentation. Among this patient group, the risk of sudden cardiac death is high due to ventricular arrhythmias [28]. Treatment of NICM is similar to ischemic cardiomyopathy with the understanding that interventions for coronary artery disease are not useful. The ICD is an effective treatment for patients at risk of SCA due to sustained ventricular arrhythmias, but it is not indicated for patients with suspected reversible cardiomyopathies. Thus, ICD guidelines stress their use only when the cardiomyopathy is deemed irreversible. Unlike an ICD, the noninvasive nature of the WCD fits well conceptually with disease etiologies that feature the potential for recovery. Several types of NICM, such as alcohol or tachycardia induced, PPCM, and TCM are frequently reversible within the first few weeks to months after the initial diagnosis using optimal medical therapy. Use of a temporary external device to treat potential ventricular arrhythmias during this period of time can be of benefit. Previous studies have shown the effectiveness of the WCD in other potentially reversible NICM [29•]. In a single center retrospective study, 254 patients received WCD over 10 years for newly diagnosed NICM which consisted of idiopathic NCM (82 %), tachycardia induced (15 %), valvular with recent repair/replacement (2 %), and TCM (1 %) [30].
A recent retrospective study showed that the WCD prevents SCA in newly diagnosed NICM related to alcohol abuse. In this study, 5.5 % of patients received at least one appropriate shock. Also, 33 % of patients experienced improvement in EF during the 3-month follow-up, showing the potential reversibility of the disease [31].
The left ventricular dysfunction in TCM is transient with good prognosis after treatment and recovery. But the short-term risk of sudden cardiac arrest from ventricular arrhythmias is still present. Deeprasertkul et al. reviewed the use of WCD in this patient population [32]. Of the 102 patients with TCM, two (2 %) had VT/VF terminated by shocks and one patient had two inappropriate shocks from signal artifact. Two of them had bradyarrhythmias (2 %). Five patients died after WCD discontinuation of which two had LVEF ≥35 % at the end of WCD use. They hypothesized that the risk of SCA in TCM `may persist even after the EF improves.
PPCM is a rare dilated cardiomyopathy that presents with left ventricular dysfunction, HF, and risk of SCA. In the USA, 2.1 % of the women with PPCM had cardiac arrest and in-hospital mortality was 1.3 % [33]. In a German multicenter experience, 3 of the 22 patients with PPCM with LV dysfunction prescribed a WCD, had four episodes of VF terminated by the WCD [34].
WCD is not infrequently used during cancer chemotherapy to balance the SCA risk from drug-induced long QT syndrome or chemotherapy-induced cardiomyopathy. The potential reversible cardiomyopathy and uncertain prognosis enhance the desirability of noninvasive therapies. Also, the WCD has an advantage over the ICD in that it can be removed during radiation treatment and when MRI is required. A retrospective study was conducted by Everitt et al. on the use of WCD in cancer patients [35]. Of 23,797 patients with WCD, 59 (0.02 %) patients had cancer or chemotherapy-induced cardiomyopathy. Fifty-four of 59 patients needed a defibrillator based on ventricular dysfunction. Six of the 59 patients (10 %) had removal of the earlier implanted ICD due to thrombus or infection. Four of the 59 patients (7 %) had shocks on five occasions which were successful during 3-month follow-up. One shock was inappropriately delivered for rapid atrial fibrillation. There were 11 deaths, but none were related to WCD failure. These observations suggest that the WCD may protect cancer patients from SCA risk if the risk is transient or related to treatment or if an ICD is contraindicated.
Myocarditis leads to HF and arrhythmias predisposing to SCA in patients with left ventricular dysfunction. Myocarditis may cause 8–12 % of all sudden deaths, but there is no clear documentation of the incidence of sudden death in myocarditis. In a case report by Prochnau, a 32-year-old woman presented with VF arrest and was diagnosed to have viral myocarditis with normal ejection fraction [36]. WCD was given to her as a bridge to prevent recurrent VT/VF until a repeat cardiac MRI was done in 3 months. She had an episode of VF terminated successfully by WCD shocks 2 months after the initial event. Repeat cardiac MRI showed ongoing disease. An ICD was implanted thereafter. 12 months after ICD implantation, she had a VF shock despite normal EF. WCD may be a safe and efficacious alternative to bridge patients with myocarditis transiently when the prognosis is uncertain.
Other Indications for WCD
The WCD can be used as a bridging therapy for various conditions apart from ischemic or NICM.
Patients waiting for heart transplantation are prone to ventricular arrhythmias and SCA. A national database identified 121 patients awaiting a heart transplant who were prescribed a WCD; 83 patients were on the transplant list or being evaluated for heart transplant, and 33 patients were waiting for re-transplantation. Ventricular arrhythmias were noted in seven patients (6 %); all episodes were terminated with WCD shocks; two patients had atrial fibrillation with rapid ventricular response resulting in inappropriate shock [37•].
A retrospective study was done in patients using WCD after ICD removal for cardiac device infections [38•]. Of the 97 patients, three had WCD shocks; sustained VT was treated by WCD in two patients, whereas the third patient had two inappropriate shocks. Three patients died outside the hospital when not wearing the WCD, with overall mortality of 8.2 %. Chung et al. reported 638 patients who had ICD removal; the incidence of SCA was 7.6 % [23]. Healy et al. created a model to study the cost effectiveness of WCD for SCA prevention after removal of infected ICD. They considered four options that included discharge to home with or without WCD, discharge to skilled nursing facility with no WCD, or observation in hospital. They found that the most cost-effective treatment option is to discharge patients home with a WCD, with an incremental cost effectiveness of $20,300/life-year and $26,436/quality-adjusted-life-year in comparison to discharging patients without WCD. Both hospital monitoring and discharging to skilled nursing facility were associated with higher costs and worse clinical outcomes. The cost effectiveness of WCD was better when the re-implantation time was at least 2 weeks [39].
The WEARIT-II registry enrolled 2000 patients into three categories [40]. Apart from ischemic and nonischemic group, patients with congenital/inherited heart disease were also included (n = 268): 61 % of patients had congenital heart disease, 53 % had inherited heart disease like hypertrophic cardiomyopathy (25 %), arrhythmogenic right ventricular dysplasia in 23 %, long QT syndrome in 10 %, and Brugada syndrome in 1 %. Probability of VT/VF was significantly higher in ischemic and congenital/inherited heart disease groups with a rate of 3 % at 3-month follow-up. Also, the rate on treatment for VT/VF episodes was higher in the same group.
A retrospective study was conducted in patients with congenital structural heart disease (CSHD) and inherited arrhythmias (IAs) to assess the outcomes in the prevention of SCA with WCD. The main indication for WCD was pending genetic testing and transplant listing in IA and CSHD groups, respectively. In IA group, three VA were treated by WCD shocks whereas no VA occurred in the CSHD group. Survival rates were lower in CSHD group (87 %) compared to IA group at 1 year of follow-up (P = 0.02) [41].
Inappropriate Shocks
nappropriate shocks are uncommon and may occur from electrical noise from poor skin-electrode contact or supraventricular tachyarrhythmias. Feldman et al. reported inappropriate shocks in 2.1 % of patients during 901 months of WCD use (0.7 % per month) [9]. Chung et al. reported inappropriate shocks in 1.9 % of patients at a rate of 1.4 % per month [23].
Conclusion
Many patients with ischemic or nonischemic cardiomyopathies inherited arrhythmogenic disorders, or other heart disease may have a transient or changing risk of SCA. In the aggregate, WCD studies demonstrate the effectiveness of the device in treating SCA during the risk period. The WCD safely allows the patient to be home, while being medically optimized and evaluated for the next step of care. Further studies with the WCD may better assess the longer term survival benefit and understand the predictors of LVEF recovery so that appropriate steps can be taken at the outset.
Abbreviations
- WCD:
-
Wearable cardioverter defibrillator
- SCA:
-
Sudden cardiac arrest
- ICD:
-
Implantable cardioverter defibrillator
- LVEF:
-
Left ventricle ejection fraction
- MI:
-
Myocardial infarction
- NICM:
-
Nonischemic dilated cardiomyopathy
- VT:
-
Ventricular tachycardia
- VT:
-
Ventricular tachycardia
- VF:
-
Ventricular fibrillation
- HF:
-
Heart failure
- CABG:
-
Coronary artery bypass grafting
- TCM:
-
Takotsubo cardiomyopathy
- PPCM:
-
Peripartum cardiomyopathy
- CSHD:
-
Congenital structural heart disease
- IAs:
-
Inherited arrhythmias
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mirowski M, Reid PR, Mower MM, et al. Termination of malignant ventricular arrhythmias with an implanted automatic defibrillator in human beings. N Engl J Med. 1980;303:322–4.
Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;51:e1–62.
Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–322.
Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–31.
Ilkhanoff L, Goldberger JJ. Out-of-hospital cardiac arrest: getting beyond the tip of the iceberg. Circulation. 2012;126:793–6.
U.S. Food and Drug Administration. Summary of Safety and Effectiveness Data, PO100300 Lifecor, Inc. WCD 2000 System. 2001. http://www.accessdata.fda.gov/cdrh_docs/pdf/p010030b.Pdf
Dillon KA, Szymkiewicz SJ, Kaib TE. Evaluation of the effectiveness of a wearable cardioverter defibrillator detection algorithm. J Electrocardiol. 2010;43:63–7.
Reek S, Geller JC, Meltendorf U, et al. Clinical efficacy of a wearable defibrillator in acutely terminating episodes of ventricular fibrillation using biphasic shocks. Pacing Clin Electrophysiol. 2003;26:2016–22.
Feldman AM, Klein H, Tchou P, et al. Use of a wearable defibrillator in terminating tachyarrhythmias in patients at high risk for sudden death: results of the WEARIT/BIROAD. Pacing Clin Electrophysiol. 2004;27:4–9.
Kusumoto FM, Calkins H, Boehmer J, et al. HRS/ACC/AHA expert consensus statement on the use of implantable cardioverter-defibrillator therapy in patients who are not included or not well represented in clinical trials. J Am Coll Cardiol. 2014;64:1143–77.
Francis J, Reek S. Wearable cardioverter defibrillator: a life vest till the life boat (ICD) arrives. Indian Heart J. 2014;66:68–72.
Henkel DM, Witt BJ, Gersh BJ, et al. Ventricular arrhythmias after acute myocardial infarction: a 20-year community study. Am Heart J. 2006;151:806–12.
Gerber Y, Weston SA, Enriquez-Sarano M, et al. Mortality associated with heart failure after myocardial infarction: a contemporary community perspective. Circ Heart Fail. 2016;9:e002460.
Gjesing A, Gislason GH, Kober L, et al. Nationwide trends in development of heart failure and mortality after first-time myocardial infarction 1997–2010: a Danish cohort study. Eur J Intern Med. 2014;25:731–8.
Moss AJ, Hall WJ, Cannom DS, et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter Automatic Defibrillator Implantation Trial Investigators. N Engl J Med. 1996;335:1933–40.
Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;346:877–83.
Bardy GH, Lee KL, Mark DB, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–37.
Buxton AE, Lee KL, Fisher JD, et al. A randomized study of the prevention of sudden death in patients with coronary artery disease. Multicenter Unsustained Tachycardia Trial Investigators. N Engl J Med. 1999;341:1882–90.
Hohnloser SH, Kuck KH, Dorian P, et al. Prophylactic use of an implantable cardioverter-defibrillator after acute myocardial infarction. N Engl J Med. 2004;351:2481–8.
Steinbeck G, Andresen D, Seidl K, et al. Defibrillator implantation early after myocardial infarction. N Engl J Med. 2009;361:1427–36.
Bigger Jr JT. Prophylactic use of implanted cardiac defibrillators in patients at high risk for ventricular arrhythmias after coronary-artery bypass graft surgery. Coronary Artery Bypass Graft (CABG) Patch Trial Investigators. N Engl J Med. 1997;337:1569–75.
Reek S, Meltendorf U, Geller JC, et al. The wearable cardioverter defibrillator (WCD) for the prevention of sudden cardiac death—a single center experience. Z Kardiol. 2002;91:1044–52.
Chung MK, Szymkiewicz SJ, Shao M, et al. Aggregate national experience with the wearable cardioverter-defibrillator: event rates, compliance, and survival. J Am Coll Cardiol. 2010;56:194–203.
Klein HU, Meltendorf U, Reek S, et al. Bridging a temporary high risk of sudden arrhythmic death. Experience with the wearable cardioverter defibrillator (WCD). Pacing Clin Electrophysiol. 2010;33:353–67.
Zishiri ET, Williams S, Cronin EM, et al. Early risk of mortality after coronary artery revascularization in patients with left ventricular dysfunction and potential role of the wearable cardioverter defibrillator. Circ Arrhythm Electrophysiol. 2013;6:117–28. This observational study demonstrates that survivors of coronary artery bypass graft surgery or post percutaneous coronary intervention with low left ventricular ejection fraction ≤35% are at increased risk of mortality and WCD use was associated with lower mortality compared to the non users.
Epstein AE, Abraham WT, Bianco NR, et al. Wearable cardioverter-defibrillator use in patients perceived to be at high risk early post-myocardial infarction. J Am Coll Cardiol. 2013;62:2000–7. This study shows that during the waiting period after myocardial infarction the risk of sudden cardiac arrest is highest in the first month and WCD successfully treated sudden cardiac arrest.
Hookana E, Junttila MJ, Puurunen VP, et al. Causes of nonischemic sudden cardiac death in the current era. Heart Rhythm. 2011;8:1570–5.
Kuriachan VP, Sumner GL, Mitchell LB. Sudden cardiac death. Curr Probl Cardiol. 2015;40:133–200.
Duncker D, Haghikia A, Konig T, et al. Risk for ventricular fibrillation in peripartum cardiomyopathy with severely reduced left ventricular function-value of the wearable cardioverter/defibrillator. Eur J Heart Fail. 2014;16:1331–6. This study shows that peripartum cardiomyopathy patients with reduced ejection are at increased risk of ventricular tachyarrhythmia and WCD prevents sudden cardiac arrest.
Singh M, Wang NC, Jain S, et al. Utility of the wearable cardioverter-defibrillator in patients with newly diagnosed cardiomyopathy: a decade-long single-center experience. J Am Coll Cardiol. 2015;66:2607–13.
Salehi N, Nasiri M, Bianco NR et al. The wearable cardioverter-defibrillator in non-ischemic cardiomyopathy: a United States National Data Base analysis. Can J Cardiol. 2016. doi:10.1016/j.cjca.2015.12.035.
Deeprasertkul PO, M.; Bianco, B.R.; Salehi, N et al. National experience with wearable cardioverter-defibrillator use in takotsubo cardiomyopathy. The Journal of Innovations in Cardiac Rhythm Management 2014;5:1707–1713.
Honigberg MC, Givertz MM. Arrhythmias in peripartum cardiomyopathy. Card Electrophysiol Clin. 2015;7:309–17.
Duncker D, Bauersachs J, Hilfiker-Kleiner D, et al. Underestimated risk for life-threatening ventricular arrhythmias in newly diagnosed peripartum cardiomyopathy? Eur Heart J. 2015;36:1067–8.
Everitt MDV, A.; Saarel, E.V. The wearable external cardiac defibrillator for cancer patients at risk for sudden cardiac death. Community Oncol 2011;8:400-403.
Prochnau D, Surber R, Kuehnert H, et al. Successful use of a wearable cardioverter-defibrillator in myocarditis with normal ejection fraction. Clin Res Cardiol. 2010;99:129–31.
Opreanu M, Wan C, Singh V, et al. Wearable cardioverter-defibrillator as a bridge to cardiac transplantation: a national database analysis. J Heart Lung Transplant. 2015;34:1305–9. This study shows that WCD is reasonable bridge therapy to prevent sudden cardiac arrest while waiting cardiac transplantation.
Tanawuttiwat T, Garisto JD, Salow A, et al. Protection from outpatient sudden cardiac death following ICD removal using a wearable cardioverter defibrillator. Pacing Clin Electrophysiol. 2014;37:562–8. This study shows that WCD provides protection from sudden cardiac arrest when ICD is removed for cardiac device related infections.
Healy CA, Carrillo RG. Wearable cardioverter-defibrillator for prevention of sudden cardiac death after infected implantable cardioverter-defibrillator removal: a cost-effectiveness evaluation. Heart Rhythm. 2015;12:1565–73.
Kutyifa V, Moss AJ, Klein H, et al. Use of the wearable cardioverter defibrillator in high-risk cardiac patients: data from the Prospective Registry of Patients Using the Wearable Cardioverter Defibrillator (WEARIT-II Registry). Circulation. 2015;132:1613–9.
Rao M, Goldenberg I, Moss AJ, et al. Wearable defibrillator in congenital structural heart disease and inherited arrhythmias. Am J Cardiol. 2011;108:1632–8.
Acknowledgments
We would like to thank Nicole Bianco, PhD, and Steven J. Szymkiewicz, MD, from Zoll Medical Corporation for providing figures, device information, and reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of theTopical Collection on Invasive Electrophysiology and Pacing
Rights and permissions
About this article
Cite this article
Lamichhane, M., Safadi, A., Surapaneni, P. et al. Use of the Wearable Cardioverter Defibrillator in High-Risk Populations. Curr Cardiol Rep 18, 78 (2016). https://doi.org/10.1007/s11886-016-0746-5
Published:
DOI: https://doi.org/10.1007/s11886-016-0746-5