Abstract
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is a genetically determined disease which predisposes to life-threatening ventricular arrhythmias. The main goal of ARVC therapy is prevention of sudden cardiac death (SCD). Implantable cardioverter defibrillator (ICD) is the most effective therapy for interruption of potentially lethal ventricular tachyarrhythmias. Despite its life-saving potential, ICD implantation is associated with a high rate of complications and significant impact on quality of life. Accurate risk stratification is needed to identify individuals who most benefit from the therapy. While there is general agreement that patients with a history of cardiac arrest or hemodynamically unstable ventricular tachycardia are at high risk of SCD and needs an ICD, indications for primary prevention remain a matter of debate. The article reviews the available scientific evidence and guidelines that may help to stratify the arrhythmic risk of ARVC patients and guide ICD implantation. Other therapeutic strategies, either alternative or additional to ICD, will be also addressed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is a genetic heart muscle disease characterized by the peculiar right ventricular (RV) involvement [1]. The hallmark pathologic feature is the progressive loss of RV myocardium and its replacement by fibrofatty scar [2, 3]. The clinical profile of ARVC was first reported in 1982 as a new clinical entity with the original designation of “dysplasia,” since it was initially believed to be a developmental defect of the RV myocardium [4]. Molecular genetics later revealed that ARVC is an inherited cardiomyopathy resulting from genetically defective desmosomal proteins that lead to progressive myocyte death and subsequent repair by fibrofatty replacement [5, 6]. ARVC is one of the main causes of sudden cardiac death (SCD) in young people and athletes [7, 8].
Prevention of SCD is the most important objective of clinical management of ARVC patients, and implantation of a cardioverter defibrillator (ICD) is the only effective strategy. Other antiarrhythmic therapies (both drugs and catheter ablation) can relieve symptoms but did not demonstrate to protect from SCD [9]. However, the survival benefit of ICD treatment is obtained at the expense of possible complications (such as lead failure) and significant impact on quality of life. As such, appropriate risk stratification is warranted to identify patients at highest arrhythmic risk of SCD who will benefit the most from ICD therapy. This article reviews the current knowledge on arrhythmic risk stratification in ARVC and indication for ICD implantation.
Clinical Manifestations and Diagnosis
The clinical manifestations of the disease usually occur between the second and forth decade of life and mostly consist of ECG depolarization and repolarization changes, typically localized to the right precordial leads (V1–V3/V4), structural abnormalities such as global or regional dysfunction of the RV, and, most importantly, ventricular arrhythmias, ranging from isolated premature ventricular beats to ventricular tachycardia (VT) or ventricular fibrillation (VF) [1, 2]. In the early disease phase, VF may reflect acute ventricular electrical instability related to “hot phases” characterized by acute myocyte death and reactive inflammation similarly to acute myocarditis. Instead, older patients with a long-lasting disease more often experience scar-related, re-entrant sustained VT [10, 11]. More recently, it has been postulated that genetically determined abnormalities in desmosomal proteins may lead to gap junction remodeling and ion channel interference. This, in turn, may create substrates for anisotropic and delayed intraventricular conduction unrelated to fibrofatty scar, which may predispose to lethal arrhythmias in the pre-phenotypic phase of the disease [12–16].
The diagnostic criteria for ARVC were first proposed by an International Task Force in 1994 and were based on major and minor criteria encompassing electrocardiographic, arrhythmic, morphological, histopathological, and genetic factors, as no single criterium is enough accurate for ARVC diagnosis [17]. In 2010, the diagnostic criteria were revised with the aim to improve the diagnostic sensitivity for identification of early/minor phenotypes, particularly in the setting of familial ARVC [18]. Currently, the diagnosis of ARVC requires a combination of different criteria from various diagnostic categories such as (1) histopathological abnormalities at endomyocardial biopsy, (2) morpho-functional abnormalities consisting of regional RV wall motion abnormalities plus RV dilation or global RV dysfunction; (3) depolarization abnormalities such as epsilon waves, delayed S-wave upstroke in V1–V3, and late potentials at signal averaged ECG; (4) T-wave inversion; (5) ventricular arrhythmias; and (6) positive family history or positive molecular genetics analysis.
Although the classic disease phenotype is characterized by predominant RV involvement, genotype-phenotype correlation studies have recently identified clinical variants with early and greater left ventricular (LV) involvement (“left dominant” ARVC) [19]. These variants mirror the classic ARVC phenotype and are characterized by LV wall motion abnormalities, T-wave inversion in the infero-lateral ECG leads, and ventricular arrhythmias with a right bundle branch block origin (suggesting LV origin). Contrast-enhanced cardiac magnetic resonance typically shows LV late gadolinium enhancement (suggesting myocardial scar) with a subepicardial/midmyocardial distribution, particularly in the lateral LV segments. This variant is more difficult to diagnose, as many features overlap with other diseases such as dilated cardiomyopathy and previous myocarditis.
Efficacy of ICD Therapy for Prevention of Sudden Death
The natural history of ARVC is primarily characterized by the risk of SCD that can occur in the early phase of the disease during adolescences and young adulthood. No prospective randomized trials have been performed on ARVC patients, but data from observational studies on large populations of patients have established that ICD therapy reduces mortality and improves long-term outcome of selected high-risk ARVC patients [20–24]. The ICD intervention rate reported in these studies was between 48 and 78 % during a follow-up of 2–7 years, and many of these patients experienced multiple ICD discharges or even VT storm. Freedom from ICD interventions for fast VT (>240 bpm) or VF was used in many studies to evaluate the survival benefit of ICD therapy, based on the assumption that these arrhythmias would have been fatal if they had not been interrupted by the device. In the largest multicenter study, the fast VT/VF-free survival rate was 72 % at 36 months compared with the actual patient survival of 98 %, with an estimate survival benefit of 26 % [20]. A large single-center study estimated that ICD therapy improved survival by 35 % at 7 years of follow-up [21]. Other studies confirmed a rate of “life-saving” ICD interventions between 30 and 50 % during follow-up and revealed that, in many patients, the first appropriate intervention occurred more than a year after implantation [22–24].
This finding suggests that ICD implantation is a lifelong preventive measure with life-saving interventions occurring even after particularly long phases of dormant ventricular electrical instability.
Clinical Tools for Risk Stratification
The adverse prognosis of ARVC patients has been initially overestimated by early reports on patients with severe clinical manifestations [25–28], while modern studies on a broader range of ARVC patients (including asymptomatic family members or genetically affected individuals with no phenotypic manifestations) have reported a much lower risk of SCD (<1 %/year) [5, 29–33]. Risk stratification is mainly based on the arrhythmic history and the degree of phenotypic expression as evaluated with ECG and imaging modalities. Several follow-up studies from different centers have identified a number of risk markers (Table 1). However, evaluating the relative weight of each marker is difficult because of the small sample sizes and the heterogeneity of variables tested in each study.
There is general agreement that a history of cardiac arrest or unstable VT confers the highest risk of SCD. The prognostic role of unexplained syncope (i.e., non-neurally mediated) and hemodynamically stable VT is controversial, as they have been associated with an increased arrhythmic risk in some but not in all studies [20, 23, 30]. Moderate to severe dysfunction of the RV and involvement of the LV have been found to be independently associated with poor arrhythmic outcome in different prospective studies [21, 34]. Among ECG parameters, greater extent of T-wave inversion across the 12 leads has been associated with poorer arrhythmic prognosis during follow-up. A possible explanation is that the extent of negative T-waves across ECG leads predicts the severity of RV fibrofatty scar, which constitutes the substrate for ventricular arrhythmias [35].
Electrophysiological Study
Programmed ventricular stimulation (PVS) during electrophysiological study is an important tool in the clinical management of symptomatic ARVC patients because it may provide useful information regarding the effect of antiarrhythmic drugs and may help to optimize antitachycardia pacing protocols in patients undergoing ICD implantation [21]. In asymptomatic patients, PVS may be performed to evaluate ventricular arrhythmia inducibility, but its prognostic role remains controversial. The rationale for the use of PVS as a risk stratification tool is that scar-related re-entry is the main arrhythmic mechanism in the overt phase of ARVC; on the other hand, the progressive nature of ARVC with scar substrates that change over time may limit its predictive ability [36]. Different studies provided conflicting results concerning the prognostic role of PVS, and its inclusion among criteria for ICD implantation remains controversial [20, 23, 24, 37•, 38]. A large multicenter study on patients who received an ICD for primary prevention showed that the incidence of life-saving interventions on fast VT/VF did not significantly differ between patients who were and were not inducible at PVS [23]. The North American Multidisciplinary study confirmed that inducible VT or VF did not predict appropriate interventions on fast VT/VF during follow-up of ICD carriers with ARVC [37•]. In patients reported by the Johns Hopkins University School of Medicine group, inducibility was the most significant independent predictor of appropriate ICD interventions on VT in general, but not for interventions on fast VT/VF only. Finally, in a Swiss study by Saguner et al., inducible VT was an independent predictor of a composite endpoint including cardiac death, heart transplantation, unstable VT/VF, and syncope [38].
In addition to PVS, electrophysiologic study may be completed with endocardial voltage mapping. This technique consists in the measurement of the amplitude of endocardial electrograms recorded in different sites of the RV using a mapping catheter. A dedicated software allows reconstructing a three-dimensional map of the RV with different colors corresponding to different amplitude of local ventricular electrograms. It has been demonstrated that, based on signal amplitude, areas of healthy myocardium can be differentiated from areas of fibrofatty replacement [39, 40]. Recent studies showed that demonstration and quantification of bipolar RV electroanatomic scar area [41•] as well as identifications of scar-related fractionated electrograms and late potentials [42] on endocardial voltage mapping predicted arrhythmic events during follow-up (Fig. 1). However, because the technique is invasive, expensive, and technically demanding, it should be reserved to selected patients and performed in specialized centers by experienced operators.
Correlation between extent of fibrofatty scar and arrhythmic risk in arrhythmogenic right ventricular cardiomyopathy (ARVC). Top: representative examples of bipolar endocardial voltage mapping (EVM) studies in three different ARVC patients. The technique allows building a three-dimensional colorimetric map of the right ventricle (RV). Areas of healthy myocardium appear violet (voltage of local bipolar electrograms >1.5 mV) while electroanatomic scars, corresponding to fibrofatty replacement, appear red (voltage of local bipolar electrograms <0.5 mV). a Right oblique anterior view of EVM showing mild fibrofatty replacement of the RV (8.4 % of total RV area) with electroanatomic scars confined to the infero-basal and outflow tract regions. b Right oblique anterior view of EVM showing a large electroanatomic scar covering 19.4 % of the RV area with involvement of the infero-basal, antero-lateral, and outflow tract regions. c Antero-posterior view of EVM showing diffuse RV involvement (68.1 % of total RV area). Bottom: correlation between the presence (d) and extent (e) of bipolar RV electroanatomic scar and incidence of arrhythmic events during follow-up in a group of 69 ARVC patients [38]. The data confirm the correlation between the degree of ARVC phenotypic expression and arrhythmic risk (modified with permission from Zorzi et al. [38] and Migliore et al. [41•])
Molecular Genetics
Gender is the most important genetic factor that impacts on the prognosis of ARVC. Males develop a more severe disease phenotype and are more likely to experience arrhythmic events than females [5, 32, 43, 44–47]. A possible explanation is that female estrogens, such as 17-beta-extradiol, may exert a protective role by inhibiting myocardial cell apoptosis [48], which plays a role in myocyte death and subsequent fibrofatty myocardial replacement in ARVC [49].
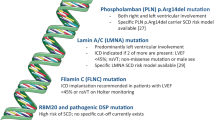
There is no demonstration that mutations in specific desmosomal genes or type of mutation (missense versus non-missense) confers a higher arrhythmic risk, although a more prevalent LV involvement is associated with desmoplakin gene mutation [5, 43, 50, 51]. Instead, carrying more than one gene mutation (i.e., compound and digenic heterozygosity) not only accounts for a greater penetrance and severity of phenotypic expression [43, 50–53], but also increases the risk of lethal arrhythmias. In a prospective study on 134 desmosomal gene mutation carriers, demonstration of multiple desmosomal gene mutations on genotype identified individuals at increased risk of major arrhythmic events since birth and remained an independent determinant of adverse outcome at multivariable analysis [5].
Arrhythmic Risk of Genotype-Positive Patients with No or Mild Disease Expression
The arrhythmic risk stratification traditionally relies on the presence and severity of the ARVC phenotypic expression. Accordingly, the risk of SCD among desmosomal gene mutation carriers is considered low [9]. Recent experimental studies suggested that genetically determined abnormalities of desmosomal proteins may result in secondary dysfunction of both voltage-gated sodium channels and gap junction proteins. As a consequence, desmosomal gene mutation carriers may harbor arrhythmogenic mechanisms at a molecular and cellular level similarly to those with Brugada syndrome before and/or independently of structural fibrofatty myocardial replacement [12–16, 54]. This primarily electrical disorder may account for SCD during the so-called “concealed” (pre-clinical) phase of the disease. However, three recent prospective studies from different centers found that DS-gene mutation carriers with no or borderline ARVC phenotype had a favorable outcome over a long-term follow-up and confirmed that the arrhythmic risk of these individuals remains low until the disease becomes clinically overt (Fig. 2) [47, 55•, 56•].
Arrhythmia-free survival in carriers of desmosomal gene mutations. Right: Kaplan-Meier analysis of survival from sustained ventricular arrhythmias or sudden death according to the degree of phenotypic expression in a cohort of 136 desmosomal gene mutation carriers. The risk of patients with no or mild phenotypic expression who did not fulfill criteria for “definite” ARVC according to the 2010 International Task Force Criteria showed a good outcome with only 1 out of 76 individuals experiencing sudden cardiac death during a long-term follow-up (and no events in the remaining). The patient was found to be affected by “left-dominant” arrhythmogenic cardiomyopathy at autopsy. Left: Kaplan-Meier analysis of survival from sustained ventricular arrhythmias or sudden death in the subgroup of 40 patients with “definite ARVC” according to the presence or absence of major arrhythmic risk factors (syncope, non-sustained ventricular tachycardia, moderate or severe ventricular dysfunction) (reproduced with permission from Zorzi et al. [55•], by permission of Oxford University Press)
On the other hand, it should be highlighted that there are rare ARVC phenotypic variants, typically observed among desmoplakin gene mutation carriers, which are characterized by early and dominant LV involvement. As mentioned, LV ARVC is characterized by epicardial fibrofatty scar of the LV wall, which is difficult to detect by ECG and echocardiography and acts as a concealed substrate for life-threatening arrhythmic events and SCD. Detection of subepicardial scar requires more sophisticated imaging tools such as contrast-enhanced cardiac magnetic resonance, and use of this technique may improve our ability to refine arrhythmic risk stratification particularly in family members or desmosomal gene mutation carriers (Fig. 3) [55•, 57].
Post-contrast cardiac magnetic resonance findings of an asymptomatic desmoplakin gene mutation with left-dominant arrhythmogenic cardiomyopathy. Four-chamber (a) and short-axis (b) views showing late gadolinium enhancement mostly involving the subepicardial layer of the posterolateral left ventricular wall at mid-basal level (white arrows), in the absence of other morpho-functional ventricular abnormalities typical of arrhythmogenic cardiomyopathy. Both electrocardiogram and echocardiogram were normal (reproduced with permission from Zorzi et al. [55•], by permission of Oxford University Press)
Indications for ICD Implantation
There is general agreement that patients who have survived cardiac arrest due to VF or suffered hemodynamically unstable VT are at high risk of SCD and benefit from an aggressive therapy with ICD implantation for secondary prevention. Although an aggressive management approach with broad indications to prophylactic ICD implantation in ARVC patients, also for those with mild or no phenotypic expression, has been the practice in the past, the current management guidelines based on the available data that the arrhythmic risk correlates with the severity of the disease phenotype recommend that patients with no risk factors are treated conservatively [9].
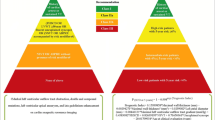
Table 2 summarizes indications for ICD therapy in ARVC proposed by three main consensus documents. The 2008 ACC/AHA/HRS “Guidelines for device-based therapy of cardiac rhythm abnormalities” [58] provided general recommendations for ICD implantation in patients with history of cardiac arrest, sustained VT, severe LV dysfunction, unexplained syncope, and inducible VT/VF at PVS irrespective of the underlying disease. With regard to ARVC, the indication to ICD implantation for primary prevention in patients with ≥1 arrhythmic risk factors was classified as a class IIa. The 2015 European Society of Cardiology “Guidelines on Ventricular Arrhythmias and Prevention of Sudden Cardiac Death” included a specific section on ARVC [59•]. The only class I recommendation for ICD implantation is a history of cardiac arrest or hemodynamically unstable VT. According to ESC Guidelines, an ICD should also be considered in patients with a history of well-tolerated sustained VT (class IIa) and may be considered in patients with ≥1 recognized arrhythmic risk factors (class IIb), balancing the risk of ICD therapy, including long-term complications, and the benefit for the patient. Recently, an International Task Force of experts from both Europe and USA produced a consensus documents on treatment of ARVC [60••]. This International Task Force document provided a summary of existing evidence and a straightforward set of recommendations aimed to guarantee adequate prevention of SCD in patients at risk, yet avoiding overtreatment in asymptomatic patients or healthy gene carriers. With regard to indications to ICD implantation, the document defined three groups of ARVC patients according to their arrhythmic risk (Fig. 4). The “high-risk” group category includes patients with a history of cardiac arrest or hemodynamically unstable VT or those with severe ventricular dysfunction, either right (RV fractional area change ≤17 % or RV ejection fraction ≤35 %) or left (LV ejection fraction ≤35 %). The indication to ICD implantation in this subset of patients was a class I. The “intermediate risk” category included primary prevention patients with ≥1 risk factors reported in Table 1. There was general agreement that syncope, non-sustained VT, or moderate right (RV fractional area change 17–24 % or RV ejection fraction 36–40 %) and/or left (LV ejection fraction 36–45 %) ventricular dysfunction should be deemed “major” risk factors and an ICD reasonably indicated (class IIa). On the other hand, ICD therapy may be considered in selected patients with ≥1other risk factors, whose arrhythmic risk is not sufficiently high to warrant systematic ICD implantation (class IIb). Finally, the low-risk category includes ARVC patients with mild phenotypic expression and no risk factors or carriers of pathogenic mutations with no signs of disease. For these patients who have an estimated annual event rate <1 %/year, ICD therapy is not recommended [23, 32, 56•].
Risk stratification and indications to ICD implantation according to the 2015 International Task Force consensus document on treatment of arrhythmogenic right ventricular cardiomyopathy. ARVC arrhythmogenic right ventricular cardiomyopathy, ICD implantable cardioverter defibrillator, NSVT non-sustained ventricular tachycardia, VT ventricular tachycardia
Other Therapies to Prevent Sudden Death
Physical exercise may promote ventricular arrhythmias and SCD in two ways. First, by increasing myocardial wall stress, it may accelerate the physiopathological process of myocyte death and fibrofatty replacement [61]. Second, adrenergic stimulation during sports activity may trigger VF in affected individuals, as suggested by the fact that ARVC patients have a fivefold higher risk to die suddenly during sports activity than at rest [7]. Recent studies in desmosomal gene mutation carriers showed that individuals who practiced competitive sports activity showed a more severe disease phenotype and a higher risk of malignant ventricular arrhythmias [62•, 63]. As a consequence, patients with a definite diagnosis of ARVC (and possibly even young carriers of desmosomal gene mutations with no features of the disease) should be restricted from participation in athletic activities, with the possible exception of recreational low-intensity sports (Fig. 5) [60••, 64]. In addition, there is a strong rationale for the use of beta blockers in ARVC because of the recognized pro-arrhythmic role of adrenergic stimulation and because they lower the mechanical stress on myocytes with genetically defective desmosomes. As a result, the recent Task Force consensus document on ARVC therapy states that beta blockers should be considered in all ARVC patients, particularly in those with a history of ventricular arrhythmias [60••].
Influence of sports activity in the pathophysiology of arrhythmogenic cardiomyopathy, from desmosomal gene mutation to sudden cardiac death. Sports activity may promote development of phenotypic expression, accelerate disease progression, and trigger life-threatening ventricular arrhythmias (reproduced with permission from Corrado et al. [64], by permission of Oxford University Press)
Finally, antiarrhythmic drug therapy and catheter ablation aim to improve quality of life by preventing symptomatic ventricular arrhythmias but should not be considered as an alternative to ICD implantation because they did not demonstrate to prevent SCD.
Conclusions
Indications for prophylactic ICD therapy in ARVC patients with no previous cardiac arrest or unstable VT remain a matter of debate. The decision should be made on a case-by-case basis, by balancing the strength of the arrhythmic risk factors with the significant risk of device-related complications as well as with the impact of ICD on quality of life. Indications for ICD implantation may vary in different countries as a consequence of several factors, so threshold for implantation is generally lower in the USA in comparison with Europe. However, there is general agreement among experts from both sides of the ocean that ARVC patients with no risk factors or desmosomal gene mutation carriers with no or mild phenotypic expressions have a low arrhythmic risk and do not require an ICD.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Basso C, Corrado D, Marcus F, Nava A, Thiene G. Arrhythmogenic right ventricular cardiomyopathy. Lancet. 2009;373:1289–300.
Corrado D, Basso C, Thiene G, et al. Spectrum of clinicopathologic manifestations of arrhythmogenic right ventricular cardiomyopathy/dysplasia: a multicenter study. J Am Coll Cardiol. 1997;30:1512–20.
Basso C, Thiene G, Corrado D, Angelini A, Nava A, Valente M. Arrhythmogenic right ventricular cardiomyopathy. Dysplasia, dystrophy, or myocarditis? Circulation. 1996;94:983–91.
Marcus FI, Fontaine GH, Guiraudon G, Frank R, Laurenceau JL, Malergue C, et al. Right ventricular dysplasia: a report of 24 adult cases. Circulation. 1982;65:384–98.
Rigato I, Bauce B, Rampazzo A, et al. Compound and digenic heterozygosity predicts lifetime arrhythmic outcome and sudden cardiac death in desmosomal gene-related arrhythmogenic right ventricular cardiomyopathy. Circ Cardiovasc Genet. 2013;6:533–42.
Basso C, Bauce B, Corrado D, Thiene G. Pathophysiology of arrhythmogenic cardiomyopathy. Nat Rev Cardiol. 2012;9:223–33.
Corrado D, Basso C, Rizzoli G, Schiavon M, Thiene G. Does sports activity enhance the risk of sudden death in adolescents and young adults? J Am Coll Cardiol. 2003;42:1959–63.
Thiene G, Nava A, Corrado D, Rossi L, Pennelli N. Right ventricular cardiomyopathy and sudden death in young people. N Engl J Med. 1988;318:129–33.
Migliore F, Zorzi A, Silvano M, Rigato I, Basso C, Thiene G, et al. Clinical management of arrhythmogenic right ventricular cardiomyopathy: an update. Curr Pharm Des. 2010;16:2918–28.
Thiene G, Corrado D, Nava A, Rossi L, Poletti A, Boffa GM, et al. Right ventricular cardiomyopathy: is there evidence of an inflammatory aetiology? Eur Heart J. 1991;12:22–5.
Patrianakos AP, Protonotarios N, Nyktari E, Pagonidis K, Tsatsopoulou A, Parthenakis FI, et al. Arrhythmogenic right ventricular cardiomyopathy/dysplasia and troponin release. Myocarditis or the “hot phase” of the disease? Int J Cardiol. 2012;157:e26–8.
Cerrone M, Lin X, Zhang M, et al. Missense mutations in plakophilin-2 cause sodium current deficit and associate with a Brugada syndrome phenotype. Circulation. 2014;129:1092–103.
Delmar M, Liang FX. Connexin43 and the regulation of intercalated disc function. Heart Rhythm. 2012;9:835–8.
Gomes J, Finlay M, Ahmed AK, et al. Electrophysiological abnormalities precede overt structural changes in arrhythmogenic right ventricular cardiomyopathy due to mutations in desmoplakin—a combined murine and human study. Eur Heart J. 2012;33:1942–53.
Rizzo S, Lodder EM, Verkerk AO, Wolswinkel R, Beekman L, Pilichou K, et al. Intercalated disc abnormalities, reduced Na(+) current density, and conduction slowing in desmoglein-2 mutant mice prior to cardiomyopathic changes. Cardiovasc Res. 2012;95:409–18.
Sato PY, Musa H, Coombs W, Guerrero-Serna G, Patino GA, Taffet SM, et al. Loss of plakophilin-2 expression leads to decreased sodium current and slower conduction velocity in cultured cardiac myocytes. Circ Res. 2009;105:523–6.
McKenna WJ, Thiene G, Nava A, Fontaliran F, Blomstrom-Lundqvist C, Fontaine G, et al. Diagnosis of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Task Force of the Working Group Myocardial and Pericardial Disease of the European Society of Cardiology and of the Scientific Council on Cardiomyopathies of the International Society and Federation of Cardiology. Br Heart J. 1994;71:215–8.
Marcus FI, McKenna WJ, Sherrill D, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Circulation. 2010;121:1533–41.
Sen-Chowdhry S, Syrris P, Prasad SK, Hughes SE, Merrifield R, Ward D, et al. Left-dominant arrhythmogenic cardiomyopathy: an under-recognized clinical entity. J Am Coll Cardiol. 2008;52:2175–87.
Corrado D, Leoni L, Link MS, et al. Implantable cardioverter-defibrillator therapy for prevention of sudden death in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation. 2003;108:3084–91.
Wichter T, Paul M, Wollmann C, et al. Implantable cardioverter/defibrillator therapy in arrhythmogenic right ventricular cardiomyopathy: single-center experience of long-term follow-up and complications in 60 patients. Circulation. 2004;109:1503–8.
Roguin A, Bomma CS, Nasir K, et al. Implantable cardioverter-defibrillators in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy. J Am Coll Cardiol. 2004;43:1843–52.
Corrado D, Calkins H, Link MS, et al. Prophylactic implantable defibrillator in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia and no prior ventricular fibrillation or sustained ventricular tachycardia. Circulation. 2010;122:1144–52.
Bhonsale A, James CA, Tichnell C, et al. Incidence and predictors of implantable cardioverter-defibrillator therapy in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy undergoing implantable cardioverter-defibrillator implantation for primary prevention. J Am Coll Cardiol. 2011;58:1485–96.
Blomstrom-Lundqvist C, Sabel KG, Olsson SB. A long term follow up of 15 patients with arrhythmogenic right ventricular dysplasia. Br Heart J. 1987;58:477–88.
Marcus FI, Fontaine GH, Frank R, Gallagher JJ, Reiter MJ. Long-term follow-up in patients with arrhythmogenic right ventricular disease. Eur Heart J. 1989;10(Suppl D):68–73.
Hulot JS, Jouven X, Empana JP, Frank R, Fontaine G. Natural history and risk stratification of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Circulation. 2004;110:1879–84.
Lemola K, Brunckhorst C, Helfenstein U, Oechslin E, Jenni R, Duru F. Predictors of adverse outcome in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy: long term experience of a tertiary care centre. Heart. 2005;91:1167–72.
Peters S. Long-term follow-up and risk assessment of arrhythmogenic right ventricular dysplasia/cardiomyopathy: personal experience from different primary and tertiary centres. J Cardiovasc Med (Hagerstown). 2007;8:521–6.
Watkins DA, Hendricks N, Shaboodien G, et al. Clinical features, survival experience, and profile of plakophylin-2 gene mutations in participants of the arrhythmogenic right ventricular cardiomyopathy registry of South Africa. Heart Rhythm. 2009;6:S10–7.
Pinamonti B, Dragos AM, Pyxaras SA, Merlo M, Pivetta A, Barbati G, et al. Prognostic predictors in arrhythmogenic right ventricular cardiomyopathy: results from a 10-year registry. Eur Heart J. 2011;32:1105–13.
Bhonsale A, James CA, Tichnell C, Murray B, Madhavan S, Philips B, et al. Risk stratification in arrhythmogenic right ventricular dysplasia/cardiomyopathy-associated desmosomal mutation carriers. Circ Arrhythm Electrophysiol. 2013;6:569–78.
Saguner AM, Ganahl S, Baldinger SH, et al. Usefulness of electrocardiographic parameters for risk prediction in arrhythmogenic right ventricular dysplasia. Am J Cardiol. 2014;113:1728–34.
Saguner AM, Vecchiati A, Baldinger SH, et al. Different prognostic value of functional right ventricular parameters in arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circ Cardiovasc Imaging. 2014;7:230–9.
Zorzi A, Migliore F, Elmaghawry M, et al. Electrocardiographic predictors of electroanatomic scar size in arrhythmogenic right ventricular cardiomyopathy: implications for arrhythmic risk stratification. J Cardiovasc Electrophysiol. 2013;24:1321–7.
Tschabrunn CM, Marchlinski FE. Ventricular tachycardia mapping and ablation in arrhythmogenic right ventricular cardiomyopathy/dysplasia: lessons learned. World J Cardiol. 2014;6:959–67.
Link MS, Laidlaw D, Polonsky B, Zareba W, McNitt S, Gear K, et al. Ventricular arrhythmias in the North American multidisciplinary study of ARVC: predictors, characteristics, and treatment. J Am Coll Cardiol. 2014;64:119–25. The North American multidisciplinary study on ARVC patients failed to demonstrate that inducible ventricular tachycardia at programmed ventricular stimulation is independently associated with arrhythmic events during follow-up.
Saguner AM, Medeiros-Domingo A, Schwyzer MA, et al. Usefulness of inducible ventricular tachycardia to predict long-term adverse outcomes in arrhythmogenic right ventricular cardiomyopathy. Am J Cardiol. 2013;111:250–7.
Corrado D, Basso C, Leoni L, et al. Three-dimensional electroanatomic voltage mapping increases accuracy of diagnosing arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation. 2005;111:3042–50.
Corrado D, Basso C, Leoni L, et al. Three-dimensional electroanatomical voltage mapping and histologic evaluation of myocardial substrate in right ventricular outflow tract tachycardia. J Am Coll Cardiol. 2008;51:731–9.
Migliore F, Zorzi A, Silvano M, et al. Prognostic value of endocardial voltage mapping in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circ Arrhythm Electrophysiol. 2013;6:167–76. The study evaluated the presence and degree of fibro-fatty myocardial scar with invasive endocardial voltage mapping and demonstrated a correlation between scar extent and arrhythmic risk, supporting the phenotype-based risk stratification strategy.
Santangeli P, Dello Russo A, Pieroni M, et al. Fragmented and delayed electrograms within fibrofatty scar predict arrhythmic events in arrhythmogenic right ventricular cardiomyopathy: results from a prospective risk stratification study. Heart Rhythm. 2012;9:1200–6.
Cox MG, van der Zwaag PA, van der Werf C, et al. Arrhythmogenic right ventricular dysplasia/cardiomyopathy: pathogenic desmosome mutations in index-patients predict outcome of family screening: Dutch arrhythmogenic right ventricular dysplasia/cardiomyopathy genotype-phenotype follow-up study. Circulation. 2011;123:2690–700.
Dalal D, Molin LH, Piccini J, et al. Clinical features of arrhythmogenic right ventricular dysplasia/cardiomyopathy associated with mutations in plakophilin-2. Circulation. 2006;113:1641–9.
Nava A, Bauce B, Basso C, Muriago M, Rampazzo A, Villanova C, et al. Clinical profile and long-term follow-up of 37 families with arrhythmogenic right ventricular cardiomyopathy. J Am Coll Cardiol. 2000;36:2226–33.
Bauce B, Frigo G, Marcus FI, et al. Comparison of clinical features of arrhythmogenic right ventricular cardiomyopathy in men versus women. Am J Cardiol. 2008;102:1252–7.
Protonotarios A, Anastasakis A, Panagiotakos DB, Antoniades L, Syrris P, Vouliotis A, et al. Arrhythmic risk assessment in genotyped families with arrhythmogenic right ventricular cardiomyopathy. Europace. 2015.
Patten RD, Pourati I, Aronovitz MJ, et al. 17beta-estradiol reduces cardiomyocyte apoptosis in vivo and in vitro via activation of phospho-inositide-3 kinase/Akt signaling. Circ Res. 2004;95:692–9.
Valente M, Calabrese F, Thiene G, Angelini A, Basso C, Nava A, et al. In vivo evidence of apoptosis in arrhythmogenic right ventricular cardiomyopathy. Am J Pathol. 1998;152:479–84.
Quarta G, Muir A, Pantazis A, Syrris P, Gehmlich K, Garcia-Pavia P, et al. Familial evaluation in arrhythmogenic right ventricular cardiomyopathy: impact of genetics and revised task force criteria. Circulation. 2011;123:2701–9.
Fressart V, Duthoit G, Donal E, et al. Desmosomal gene analysis in arrhythmogenic right ventricular dysplasia/cardiomyopathy: spectrum of mutations and clinical impact in practice. Europace. 2010;12:861–8.
Bauce B, Nava A, Beffagna G, et al. Multiple mutations in desmosomal proteins encoding genes in arrhythmogenic right ventricular cardiomyopathy/dysplasia. Heart Rhythm. 2010;7:22–9.
Xu T, Yang Z, Vatta M, et al. Compound and digenic heterozygosity contributes to arrhythmogenic right ventricular cardiomyopathy. J Am Coll Cardiol. 2010;55:587–97.
Kaplan SR, Gard JJ, Protonotarios N, et al. Remodeling of myocyte gap junctions in arrhythmogenic right ventricular cardiomyopathy due to a deletion in plakoglobin (Naxos disease). Heart Rhythm. 2004;1:3–11.
Zorzi A, Rigato I, Pilichou K, et al. Phenotypic expression is a prerequisite for malignant arrhythmic events and sudden cardiac death in arrhythmogenic right ventricular cardiomyopathy. Europace. 2015; in press. The study investigated the arrhythmic risk of desmosomal gene mutations carriers, comparing those with overt ARVC with those with no or mild phenotypic expression.
Te Riele AS, James CA, Groeneweg JA, et al. Approach to family screening in arrhythmogenic right ventricular dysplasia/cardiomyopathy. Eur Heart J. 2015. The study from the John Hopkins group confirmed that family members of arrhythmogenic cardiomyopathy show a low risk of events until the disease becomes overt.
te Riele AS, Bhonsale A, James CA, et al. Incremental value of cardiac magnetic resonance imaging in arrhythmic risk stratification of arrhythmogenic right ventricular dysplasia/cardiomyopathy-associated desmosomal mutation carriers. J Am Coll Cardiol. 2013;62:1761–9.
Epstein AE, Dimarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: executive summary. Heart Rhythm. 2008;5:934–55.
Priori SG, Blomstrom-Lundqvist C, Mazzanti A, et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC) Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Europace. 2015;17(11):1601–87. The European Heart Association guidelines on ventricular arrhythmias and prevention of sudden cardiac death specifically address indications to ICD implantation in arrhythmogenic cardiomyopathy.
Corrado D, Wichter T, Link MS, et al. Treatment of arrhythmogenic right ventricular cardiomyopathy/dysplasia: an international task force consensus statement. Eur Heart J. 2015;36(46):3227–37. This is a consensus document from many experts from both Europe and US specifically addressing the treatment of ARVC.
Kirchhof P, Fabritz L, Zwiener M, et al. Age- and training-dependent development of arrhythmogenic right ventricular cardiomyopathy in heterozygous plakoglobin-deficient mice. Circulation. 2006;114:1799–806.
James CA, Bhonsale A, Tichnell C, Murray B, Russell SD, Tandri H, et al. Exercise increases age-related penetrance and arrhythmic risk in arrhythmogenic right ventricular dysplasia/cardiomyopathy-associated desmosomal mutation carriers. J Am Coll Cardiol. 2013;62:1290–7. The study demonstrated that a history of competitive sports activity is associated with increased disease penetrance and higher risk of ventricular arrhythmias in desmosomal-gene mutation carriers.
Saberniak J, Hasselberg NE, Borgquist R, Platonov PG, Sarvari SI, Smith HJ, et al. Vigorous physical activity impairs myocardial function in patients with arrhythmogenic right ventricular cardiomyopathy and in mutation positive family members. Eur J Heart Fail. 2014;16:1337–44.
Corrado D, Zorzi A. Arrhythmogenic right ventricular cardiomyopathy and sports activity. Eur Heart J. 2015;36:1708–10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Alessandro Zorzi, Ilaria Rigato, Barbara Bauce, Cristina Basso, Gaetano Thiene, Sabino Iliceto, and Domenico Corrado declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Funding
This article was funded by University of Padua Research Grant TRANSAC, Padova.
Additional information
This article is part of the Topical Collection on Myocardial Disease
Rights and permissions
About this article
Cite this article
Zorzi, A., Rigato, I., Bauce, B. et al. Arrhythmogenic Right Ventricular Cardiomyopathy: Risk Stratification and Indications for Defibrillator Therapy. Curr Cardiol Rep 18, 57 (2016). https://doi.org/10.1007/s11886-016-0734-9
Published:
DOI: https://doi.org/10.1007/s11886-016-0734-9