Abstract
Arrhythmogenic right ventricular dysplasia/cardiomyopathy (ARVD/C) is an inherited cardiomyopathy characterized by ventricular arrhythmias, right ventricular dysfunction, and sudden cardiac death. Since the first description of ARVD/C in 1982, there have been major advances in the diagnosis and management of the disease. For instance, the discovery of desmosomal abnormalities as a genetic basis for ARVD/C; the importance of proband status and ventricular ectopy for risk stratification of patients at risk for sudden cardiac death; and the critical role that exercise plays in the development and progression of ARVD/C, just to name a few. From a treatment perspective, the placement of implantable cardioverter defibrillators in those at risk for sudden cardiac death and ablation techniques have also evolved over time. In 2010, an update of the 1994 Task Force Diagnostic criteria for ARVD/C was published with the hope to increase diagnostic sensitivity. This update incorporates new knowledge and technology to assess structural cardiac abnormalities and is the standard for diagnosis today.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arrhythmogenic right ventricular dysplasia/cardiomyopathy (ARVD/C) is an inherited cardiomyopathy characterized pathologically by replacement of the cardiac myocytes with fibrofatty tissue; this predisposes patients to ventricular arrhythmias, right ventricular failure, and increased risk of sudden cardiac death (SCD). Although structural involvement of the right ventricle predominates, a left dominant form is also seen.
ARVD/C was first described in 1982 [1]; since then, significant advances have been made in the understanding different aspects of this disease. The 2010 Task Force Criteria (TFC) improved diagnostic sensitivity by taking into account electrophysiological abnormalities, genetic testing, and cardiac structural abnormalities.
Genetic testing of probands and family members has become a very important part of the diagnosis and screening of ARVD/C since desmosomal mutations can be found in up to 60 % of affected individuals [2, 3].
The treatment of ARVD/C is aimed at reducing the risk of sudden cardiac death by properly risk-stratifying patients that would benefit from an implantable cardioverter defibrillator (ICD). Antiarrhythmic drugs and catheter ablation are also commonly used to improve quality of life by preventing ventricular arrhythmias. Another important consideration in patients with ARVD/C is exercise restriction to prevent disease progression.
The purpose of this article is to review the current state of knowledge of ARVD/C, natural history, clinical presentation, diagnosis, and treatment of the disease.
ARVD/C Overview
Clinical Presentation and Natural History
ARVD/C is a rare inherited cardiomyopathy, with an estimated prevalence of 1 per 5000 individuals [4]. Patients usually present in the second to fifth decade of life with symptoms that can be correlated with the presence of ventricular arrhythmias, such as syncope, palpitations, and lightheadedness, with progression to heart failure being uncommon [3, 5].
Dalal et al. [5] studied 100 patients diagnosed with ARVD/C. During a median follow-up of 6 years, 47 patients received an ICD, 29 of whom received an appropriate ICD therapy. At follow-up, 66 patients were alive (44 had an ICD, 5 had signs of heart failure, 2 had heart transplant, 18 were on drug therapy). Twenty-three patients died at presentation (21 SCD, 2 noncardiac deaths) and 11 died during follow-up (10 SCD, 1 biventricular heart failure). Of the total number of patients that died (n = 34), only three were diagnosed while living and one had an ICD implanted. They concluded that once the diagnosis of ARVD/C is certain and patients receive an ICD the mortality is low. Also, the progression to heart failure in this population was uncommon (<10%).
The presentation, clinical course, and survival outcomes of a cohort of 439 index patients who met 2010 TFC for ARVD/C were reported by Groeneweg et al. [3] The mean age at presentation was 36 ± 14 years, and mutations were identified in 63 % (n = 276) individuals. Most patients were symptomatic at presentation (n = 419). Forty-eight (11 %) presented with a cardiac arrest, 25 were resuscitated, and 23 died and the diagnosis was established at autopsy. An additional of 220 (50 %) patients presented with a sustained ventricular arrhythmia. During follow-up, 212 out of 245 patients with a sustained ventricular arrhythmia (VA) or resuscitated SCD and 139 out of 171 patients without a sustained VA received an ICD. Sixty-five patients did not have an ICD implanted during follow-up, and 31 (48 %) of them experienced sustained VA during follow-up. Recurrent sustained VA on follow-up was seen in a total of 72 % (n = 301) index patients. After a median follow-up of 7 years, 10 (3 %) of patients with an ICD died (3 with heart failure, 2 SCD, 2 of a combination of arrhythmias and heart failure, and 3 of noncardiac causes). Eleven (17 %) patients without an ICD died (10 SCD, 1 with heart failure). During long-term follow-up, 54 patients (13 %) developed symptomatic heart failure and 18 (4 %) underwent cardiac transplantation with 4 dying during follow-up. Overall 391/416 index patients (94 %) who presented alive were alive at last follow-up. They concluded that ICD implantation reduced the incidence of SCD during follow up and that the long-term outcome was favorable in those that were diagnosed and treated appropriately.
Recently, Te Riele and colleagues [6] compared clinical characteristics and outcomes between a cohort of 75 pediatric-onset cases of ARVD/C (mean age at presentation 15.3 ± 2.4 years) and 427 adult patients (mean age at presentation 38.6 ± 13.4). They found that pediatric patients were more likely to present with sudden cardiac death (p = 0.003) or resuscitated cardiac arrest, compared to adults who presented most commonly with sustained ventricular tachycardia (p = 0.359). However, once ARVD/C is diagnosed, they found that survival free from sustained ventricular tachycardia, cardiac transplantation, and death was similar between the two groups after more than 8 years of follow-up.
Although ARVD/C is predominantly a disease of the right ventricle [7–10], it is now well established that involvement of the left ventricle (LV) may occur. Left dominant arrhythmogenic cardiomyopathy usually presents with early involvement of the LV in the absence of significant RV systolic dysfunction. It has been reported that LV dominant disease is more commonly seen in individuals with mutations in desmoplakin or phospholamban [10].
Genetics
ARVD/C is commonly inherited in an autosomal dominant manner with incomplete penetrance and variable expressivity. In a minority of cases, ARVD/C can also be inherited in an autosomal recessive pattern as part of a cardiocutaneous syndrome such as Naxos disease or Carvajal syndrome [11].
The identification of a plakoglobin (JUP) mutation that affects a key component of desmosomes in Naxos syndrome led to several studies investigating their role in other arrhythmogenic cardiomyopathies. Subsequently, several ARVD/C-associated mutations were identified: plakophilin-2 (PKP2), desmoplakin (DSP), desmoglein-2 (DSG2), and desmocollin-2 (DSC2) [2, 10]. Mutations in several non-desmosomal genes such as cardiac ryanodine receptor (RyR2), phospholamban (PLN), transmembrane protein 43 (TMEM43), Titin, and transforming growth factor β3 (TGFβ3) have also been observed in atypical forms of ARVD/C. Mutations in desmosomal proteins can be identified in approximately 60 % of ARVD/C patients [3, 10]. Thus, lack of an identifiable mutation does not exclude the disease.
The genetic findings of 577 patients from 241 unrelated families, selected based on the presence of an ARVD/C-related mutation, have been reported [10]. The majority of participants in the study 80 % (n = 463) were the carriers of a PKP2 mutation, with fewer heterozygous carriers for other mutations associated with ARVD/C (31 DSG2, 31 PLN, 19 DSP, 8 DSC2, 2 JUP, and 1 TMEM43). Four percent (n = 22) of participants carried two or more pathogenic mutations. The authors found that patients presenting with SCD/ventricular fibrillation (VF) were younger (median 23 vs. 36 years) than those presenting with sustained monomorphic ventricular tachycardia (VT). They also noticed that there was an association of genotype with clinical course and disease expression. The patients that had more than one mutation, earlier occurrence of sustained VT/VF, lower VT/VF free survival, and more frequent left ventricular dysfunction, heart failure, and cardiac transplantation, than those with only one mutation. Lastly, men were more likely more likely to be symptomatic probands and they had earlier and more severe arrhythmic expression.
Pathophysiology
The genetics of ARVD/C support the hypothesis that this is a disease of desmosomal dysfunction. Although the pathogenesis of ARVD/C is not fully understood, it has been hypothesized that abnormalities in the desmosomal proteins may lead to impaired mechanical coupling between individual cells, which then causes myocyte uncoupling resulting in inflammation, fibrosis, and adipocytosis. This is especially true in situations that increase myocardial strain, such as exercise.
This pathogenic model explains the observation of an earlier onset of ARVD/C and a higher risk of SCD among those who participate in strenuous exercise. It would also explain the fact that the RV is more often affected, due to its thinner and more distensible wall than the LV. Furthermore, these defects in myocyte mechanical coupling may lead to impairment in electrical coupling. This remains an active area of investigation.
Diagnosis of ARVD/C
The diagnosis of ARVD/C is made through a scoring system with major and minor criteria, based on demonstrating a combination of ventricular dysfunction and structural alterations, tissue characterization, electrocardiographic repolarization/depolarization abnormalities, ventricular arrhythmias, family history, and genetic testing. A definite diagnosis is made if a patient has “4 points,” with a major criterion equal to 2 points and a minor criterion equal to “1 point.” A borderline diagnosis is made with “3 points” and a possible diagnosis with “2 points.” The original 1994 Task Force Criteria were updated and published in 2010; their aim was to increase diagnostic sensitivity by integrating new knowledge and technology [12] (Table 1).
It is important to note that there is no gold standard diagnostic test for ARVD/C. On initial evaluation, all patients should have a physical exam and comprehensive clinical history that includes information about family history of sudden death and arrhythmias and an ECG, 24-h Holter monitoring, signal-averaged ECG, and comprehensive imaging of both ventricles should also be obtained. Although MRI is a very important diagnostic tool, it can also be a common cause for misdiagnosis (Fig. 1) [13]. If the initial workup is suggestive but not diagnostic of ARVD/C, an electrophysiology study should be considered to establish the diagnosis. Right ventriculography and endomyocardial biopsy were also used to aid in the diagnosis of ARVD/C in the past, but they are rarely used currently.
Cardiac MRI of a patient with ARVD/C. Bright blood images in the right ventricular outflow tract (RVOT) plane obtained in end diastole (a) and end systole (b) show microaneurysms (arrows) in the RV free wall with persistent bulge in both phases. Short-axis bright blood images obtained in end diastole (c) and end systole (d) demonstrate dyskinesis at the acute angle of the RV and hypokinesis in the inferior wall (arrowheads) (Reproduced from Calkins [14], with permission from Elsevier.)
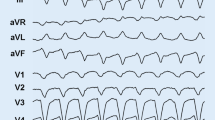
The diagnosis of ARVD/C should be considered in individuals without known heart disease, who present with frequent PVCs or symptomatic ventricular tachycardia, especially if there is left bundle branch block (LBBB) morphology with superior axis, if the VT occurs in a patient with T wave inversions in the right precordial leads, or if the LBBB VT ECG pattern is not typical of idiopathic RVOT VT [14].
The differential diagnosis for ARVD/C should include cardiac sarcoidosis, idiopathic right ventricular outflow tract ventricular tachycardia, and VT arising from the aortic root. For patients that present with symptoms of RV systolic heart failure, RV infarct or pulmonary hypertension should be considered. Dilated cardiomyopathy should also be kept in mind when there is evidence of biventricular heart failure, as well as biventricular arrhythmogenic cardiomyopathy when there is significant ventricular ectopy [15].
Management
After establishing the right diagnosis, the most important step is accurate risk stratification of patients at risk for sudden cardiac death and deciding if they would benefit from an ICD. Another component of management is minimizing ICD therapies whether it is with medication or catheter ablation. And the final component of management is preventing progression of the disease.
Establishing an Accurate Diagnosis
The first step is to establish an accurate diagnosis of ARVD/C. Misdiagnosis of ARVD/C is common due to lack of awareness of the 2010 Task Force Criteria and misinterpretation of MR imaging.
Risk Stratification and ICD implantation
Prevention of sudden cardiac death is the most important goal of management. More than 50 % of patients with ARVD/C that have received an ICD have appropriate device interventions during follow-up [16, 17].
Bhonsale et al. [16] studied 84 patients with definite or probable ARVD/C who had an ICD implanted for primary prevention of sudden cardiac death. They reported that over a mean follow-up of 4.7 ± 3.4 years, 40 patients (48 %) received appropriate ICD therapy, with 16 (19 %) of them having interventions for potentially fatal rapid VF. The predictors for appropriate ICD therapy that were significant in this study were the presence of nonsustained ventricular tachycardia (NSVT), proband status, inducibility at electrophysiology study (EPS), and premature ventricular contraction count >1000/24 h. NSVT and EPS remained as significant predictors on multivariable analysis. The authors also observed that there is an increased risk of ventricular arrhythmias and ICD interventions in the presence of multiple risk factors. Lastly, more frequent ventricular ectopy was associated with progressively more common ICD therapy.
Recently, an international task force consensus statement for the treatment of ARVD/C has been published [18••]. Their recommendation is that patients with ARVD/C who have experienced hemodynamically unstable VT or VF, and those with severe systolic dysfunction of RV, LV, or both irrespective of arrhythmias, should receive an ICD (class I). An ICD should be considered in ARVD/C patients that have experienced hemodynamically stable sustained VT and also in individuals with unexplained syncope, moderate ventricular dysfunction, or NSVT (class IIa).
Minimizing Symptoms and Preventing ICD Interventions
Pharmacologic Therapy
Few studies have been done to establish the efficacy and safety of pharmacologic therapy in ARVD/C. Beta-blockers are used for almost all patients with the disease based on the fact that they reduce risk of sudden cardiac death in patients without ARVD/C. Furthermore, high-dose isoproterenol can trigger VT in patients with the disease [19, 20] and most of the arrhythmias and SCD are triggered by exercise. In summary, beta-blocker therapy is recommended in ARVD/C patients with recurrent VT, appropriate ICD therapies, or inappropriate ICD interventions resulting from sinus tachycardia, supraventricular tachycardia, or atrial fibrillation/flutter with high-ventricular rate (class I). Beta-blocker therapy should be considered in all patients with ARVD/C irrespective of arrhythmias (class IIa) [18••].
ACE inhibitors are commonly used as afterload reducers in patients with ARVD/C. Even though there are no published trials in patients with ARVD/C, there is enough data supporting the use of these medications in a broader population of patients with cardiomyopathy [14].
When it comes to antiarrhythmic agents, the goal is to improve quality of life by preventing symptomatic ventricular arrhythmias and ICD discharges. Again, there are no randomized control trials to compare the different antiarrhythmic drugs available, but amiodarone and sotalol are commonly used.
Catheter Ablation
Catheter ablation is an option for treatment of patients with ARVD/C who have ventricular tachycardia. It is important to recognize that the role of catheter ablation in patients with ARVD/C is not curative but improves quality of life by decreasing the frequency of episodes of VT.
Several studies have evaluated the outcomes of catheter ablation of VT in patients with ARVD/C [21–23]. Dalal et al. reported on a cohort of 24 patients with ARVD/C who underwent VT ablation [21]. There was a high rate of recurrence of VT in ARVD/C patients undergoing radiofrequency catheter ablation (RFA). The cumulative VT-free survival was 75 % at 1.5 months, 50 % at 5 months, and 25 % at 14 months. Another study [22] reported on an expanded series of 87 patients who underwent a total of 175 VT ablations. The freedom from VT was 47 % at 1 year, 21 % at 5 years, and 15 % at 10 years, over a follow-up of 88.3 ± 66 months. After epicardial ablation, the cumulative freedom of VT was 64 % at 1 year and 45 % at 5 years.
Most recently, a single center experience on 30 ARVD/C patients who underwent endo-/epicardial mapping and epicardial catheter ablation of VT has been published [23]. Eight (27 %) patients had VT recurrence after epicardial RFA. Most of the VT recurrences occurred during exercise, in the first year after the procedure, had fast cycle lengths and required an ICD intervention for termination. VT-free survival was 83 % at 6 months, 76 % at 12 months, and 70 % at 24 months. There was a significant reduction of VT burden (P < 0.001).
The current recommendations for catheter ablation are for patients with incessant VT or frequent appropriate ICD therapies despite maximal pharmacological therapy. An epicardial approach is for those who fail one or more attempts of endocardial VT ablation (class I) [18••].
Exercise Restriction
The observation that there is a disproportionate number of athletes among patients with ARVD/C led to the hypothesis that exercise is an environmental factor in the pathogenesis of this disease. Consequently, many studies have reported that there is a clear relationship between ARVD/C and exercise. Furthermore, endurance exercise can evoke an earlier presentation of ARVD/C and have a more severe clinical course manifested by earlier onset arrhythmias, structural dysfunction, heart failure, and need for transplant [24–27].
The role of exercise in patients with and without mutations as well as the important question of a safe exercise threshold has been reported by the Johns Hopkins ARVD/C Program [28••, 29••, 30]. These studies have shown that patients with ARVD/C should not practice high endurance exercise, regardless of their genotype. Although it might be potentially safe for healthy mutation carriers to practice the minimum exercise a healthy adult recommended by the American Heart Association (AHA), there is still more research needed to find what is the threshold needed to trigger the onset of ARVD/C.
In summary, exercise restriction is a key component in the management of ARVD/C. Recently, an update to the 36th Bethesda Conference Eligibility Recommendations for Competitive Athletes with Cardiovascular Abnormalities’ has been published by the AHA and the American College of Cardiology [31]. The current recommendation is avoidance of all competitive activities for patients with probable, borderline, or definite diagnosis of ARVD/C except for sports with a low cardiovascular demand (class III, Level of Evidence C).
The ARVD/C treatment consensus statement, published by Corrado et al. [17], concluded that patients with a definite diagnosis of ARVD/C should not participate in competitive or endurance sports (class I) with the possible exception of recreational low-intensity sports (class IIa). Restriction from competitive sports may be considered in ARVD/C family members that are healthy gene carriers (class IIa) and those that have an unknown genotype.
Prevent Progression
It is important to note that no studies have examined the extent and rate of progression of ARVD/C. One of the most important tools in preventing disease progression is restriction of exercise. We have outlined the considerable data supporting this relationship in the section above.
Cardiac Transplantation
Cardiac transplantation is reserved for patients that have intractable arrhythmias and/or heart failure. Tedford et al. [32] reviewed 18 ARVD/C patients who underwent heart transplantation. The mean age of the first symptom was 24 ± 13 years, with an average age at transplantation of 40 ± 14 years. Patients who received a transplant had a more prolonged course of the disease and a relatively early onset.
Summary and Conclusion
ARVD/C is an inherited cardiomyopathy characterized clinically by ventricular arrhythmias, sudden death, and right ventricular dysfunction. Due the variable penetrance and expressivity of ARVD/C, the diagnosis is often challenging and requires a multifaceted approach to patient evaluation. The management of ARVD/C is aimed at decreasing the incidence of sudden cardiac death by identifying the patients that would benefit from an ICD. ICDs significantly reduce mortality in patients with ARVD/C. Antiarrhythmic drugs and VT ablation are used to decrease the burden of symptomatic ventricular arrhythmias. Exercise restriction is key to prevent disease progression. Cardiac transplantation is reserved for patients that have intractable arrhythmias and/or heart failure.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Marcus FI, Fontaine GH, Guiraudon G, et al. Right ventricular dysplasia: a report of 24 adult cases. Circulation. 1982;65(2):384–98.
Den Haan AD, Tan BY, Zikusoka MN, et al. Comprehensive desmosome mutation analysis in North Americans with arrhythmogenic right ventricular dysplasia/cardiomyopathy. Circ Cardiovasc Genet. 2009;5:428–35.
Groeneweg J, Bhonsale A, James C, et al. Clinical presentation, long-term follow-up, and outcomes of 1001 arrhythmogenic right ventricular dysplasia/cardiomyopathy patients and family members. Circ Genet. 2015;8(3):437–46.
Peters S, Trummel M, Meyners W. Prevalence of right ventricular dysplasia: cardiomyopathy in a non-referral hospital. Int J Cardiol. 2004;97:499–501.
Dalal D, Nasir K, Bomma C, et al. Arrhythmogenic right ventricular dysplasia: a United States experience. Circulation. 2005;112(25):3823–32.
Te Riele AS, Sawant AC, James C, et al. Arrhythmogenic right ventricular dysplasia/cardiomyopathy in the pediatric population clinical characterization and comparison with adult-onset disease. JACCCEP. 2015;1(6):551–60.
Jain A, Tandri H, Calkins H, et al. Role of cardiovascular magnetic resonance imaging in arrhythmogenic right ventricular dysplasia. J Cardiovasc Magn Reson. 2008;10(1):10–32.
Rastegar N, Burt JR, Corona-Villalobos CP, et al. Cardiac MR findings and potential diagnostic pitfalls in patients evaluated for arrhythmogenic right ventricular cardiomyopathy. Radiographics. 2014;34(6):1553–70.
Rastegar N, Zimmerman SL, Te Riele AS, et al. Spectrum of biventricular involvement on CMR among carriers of ARVD/C-associated mutations. JACC Cardiovasc Imaging. 2015;8(7):863–4.
Bhonsale A, Groeneweg JA, James CA, et al. Impact of genotype on clinical course in arrhythmogenic right ventricular dysplasia/cardiomyopathy-associated mutation carriers. Eur Heart J. 2015;36(14):847–55.
Protonotarios N, Tsatsopoulou A. Naxos disease and Carvajal syndrome: cardiocutaneous disorders that highlight the pathogenesis and broaden the spectrum of arrhythmogenic right ventricular cardiomyopathy. Cardiovasc Pathol. 2004;13(4):185–94.
Marcus FI, McKenna WJ, Sherrill D, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Circulation. 2010;13:1533–41.
Bomma C, Rutberg J, Tandri H, et al. Misdiagnosis of arrhythmogenic right ventricular dysplasia (ARVD). J Cardiovasc EP. 2004;15(3):300–6.
Calkins H. Arrhythmogenic right ventricular dysplasia/cardiomyopathy—three decades of progress. Circ J. 2015;79(5):901–13.
Calkins H. Arrhythmogenic right ventricular dysplasia. Curr Probl Cardiol Mar. 2013;38:103–23.
Bhonsale A, James CA, Tichnell C, et al. Incidence and predictors of implantable cardioverter-defibrillator therapy in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy undergoing implantable cardioverter-defibrillator implantation for primary prevention. J Am Coll Cardiol. 2011;14:1485–96.
Piccini JP, Dalal D, Roguin A, et al. Predictors of appropriate implantable defibrillator therapies in patients with arrhythmogenic right ventricular dysplasia. Heart Rhythm. 2005;2(11):1188–94.
Corrado D, Wichter T, Link MS, et al. Treatment of arrhythmogenic right ventricular cardiomyopathy/dysplasia: an international task force consensus statement. Eur Heart J. 2015;36(46):3227–37. This document provides a guide to clinical practice for the management of ARVD/C based on recommendations and levels of evidence of specific management options.
Philips B, Madhavan S, James C, et al. High prevalence of catecholamine-facilitated focal ventricular tachycardia in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy. Circ Arrhythm Electrophysiol. 2013;6(1):160–6.
Denis A, Sacher F, Derval N, et al. Diagnostic value of isoproterenol testing in arrhythmogenic right ventricular cardiomyopathy. Circ Arrhythm Electrophysiol. 2014;7(4):590–7.
Dalal D, Jain R, Tandri H, et al. Longterm efficacy of catheter ablation of ventricular tachycardia in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy. J Am Coll Cardiol. 2007;50:432–40.
Philips B, Madhavan S, James C, et al. Outcomes of catheter ablation of ventricular tachycardia in arrhythmogenic right ventricular dysplasia/cardiomyopathy (ARVD/C). Circ Arrhythm Electrophysiol. 2012;5:499–505.
Philips B, Te Riele AS, Sawant A, et al. Outcomes and VT recurrence characteristics after epicardial ablation of ventricular tachycardia in arrhythmogenic right ventricular dysplasia/cardiomyopathy. Heart Rhythm. 2015;12:716–25.
Corrado D, Basso C, Rizzoli G, et al. Does sports activity enhance the risk of sudden death in adolescents and young adults? J Am Coll Cardiol. 2003;42(11):1959–63.
La Gerche A, Burns AT, Mooney DJ, et al. Exercise‐induced right ventricular dysfunction and structural remodelling in endurance athletes. Eur Heart J. 2012;33:998–1006.
Saberniak J, Hasselberg NE, Borgquist R, et al. Vigorous physical activity impairs myocardial function in patients with arrhythmogenic right ventricular cardiomyopathy and in mutation positive family members. Eur J Heart Fail. 2014;16(12):1337–44.
Ruwald AC, Marcus F, Estes III NA, et al. Association of competitive and recreational sport participation with cardiac events in patients with arrhythmogenic right ventricular cardiomyopathy: results from the North American multidisciplinary study of arrhythmogenic right ventricular cardiomyopathy. Eur Heart J. 2015;36(27):1735–43.
James CA, Bhonsale A, Tichnell C, et al. Exercise increases age-related penetrance and arrhythmic risk in arrhythmogenic right ventricular dysplasia/cardiomyopathy associated desmosomal mutation carriers. J Am Coll Cardiol J Am Coll Cardiol. 2013;62(14):1290–7. This was the first study that evaluated the role of exercise in ARVD/C in patients that have a pathogenic desmosomal mutation.
Sawant AC, Bhonsale A, Te Riele AS, et al. Exercise has a disproportionate role in the pathogenesis of arrhythmogenic right ventricular dysplasia/cardiomyopathy in patients without desmosomal mutations. J Am Heart Assoc. 2014 Dec 16;3(6). This study showed that high intensity exercise also has an impact on the development of ARVD/C among patients without mutations and it negatively modifies cardiac structure and promotes arrhythmias.
Sawant AC, Te Riele AS, Tichnell C, et al. Safety of American Heart Association-recommended minimum exercise for desmosomal mutation carriers. Heart Rhythm. 2016;13(1):199–20.
Maron BJ, Udelson JE, Bonow RO, et al. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task Force 3: hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy and other cardiomyopathies, and myocarditis: a scientific statement from the American Heart Association and American College of Cardiology. Circulation. 2015;132(22):e273–80.
Tedford RJ, James C, Judge DP, et al. Cardiac transplantation in arrhythmogenic right ventricular dysplasia/cardiomyopathy. J Am Coll Cardiol. 2012;59(3):289–90.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Gabriela and M. Orgeron have no conflict of interest.
Dr. Hugh Calkins is a consultant for St. Jude Medical and Medtronic. He also receives research support from St. Jude Medical and Boston Scientific.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Invasive Electrophysiology and Pacing
Rights and permissions
About this article
Cite this article
Orgeron, G.M., Calkins, H. Advances in the Diagnosis and Management of Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy. Curr Cardiol Rep 18, 53 (2016). https://doi.org/10.1007/s11886-016-0732-y
Published:
DOI: https://doi.org/10.1007/s11886-016-0732-y