Abstract
Purpose of Review
Overactive bladder (OAB) and interstitial cystitis/bladder pain syndrome (IC/BPS) are defined as syndromes consisting of “urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence” and “an unpleasant sensation perceived to be related to the urinary bladder, associated with lower urinary tract symptoms,” respectively. Distinguishing between the two diagnoses can be challenging and although OAB and IC/BPS are traditionally considered separate conditions, more evidence is emerging to suggest a continuum between the symptoms. This review considers the two conditions existing on a continuum by reviewing relevant definitions, phenotypes, and treatment considerations.
Recent Findings
Recent studies have suggested that up to 25% of patients with IC/BPS reported urge incontinence and 35% of patients with OAB described bladder pain. Analysis assessing validated questionnaires revealed that scores could distinguish controls from patients with storage LUTS but were not able to distinguish between those with OAB and IC/BPS. A novel scoring system spanning domain of urgency incontinence and bladder pain was validated and provided 91% diagnostic accuracy.
Summary
OAB and IC/BPS symptoms overlap significantly and it remains unclear if patients with IC/BPS and OAB are unique populations or specific phenotypes of the same condition. We propose that “OAB-dry” patients without fear of leakage may represent a variant of IC/BPS. Unbiased phenotyping based on more accurate symptomatic descriptions may help reveal the correlations of variants of lower urinary tract symptoms with both prognosis and treatment responses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The International Urogynecological Association (IUGA)/International Continence Society (ICS), the American Urological Association (AUA), and Society of Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction (SUFU) define overactive bladder (OAB) as a syndrome of urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence, in the absence of urinary tract infection or other pathology [1, 2•]. Urgency is described as a complaint of a sudden, compelling desire to pass urine which is difficult to defer [1]. SUFU/AUA defines interstitial cystitis/bladder pain syndrome (IC/BPS) as an unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder, associated with lower urinary tract symptoms of longer than 6-week duration, in the absence of infection or other identifiable causes [3]. ICS defines IC/BPS as a compelling need to urinate due to pain or an unpleasant sensation that is difficult to defer. There is no consensus between international societies on the exact definition or nomenclature, but all agree that diagnosis depends on presence of pain, pressure, discomfort, and at least one urinary symptom [4].
Distinguishing between the two diagnoses, as well as identifying the coexistence of both, remains challenging. Although OAB and IC/BPS are traditionally considered two separate conditions, more evidence is emerging to suggest a continuum between the two [5,6••,7]. Over half of women with OAB report symptoms of pain, pressure, or discomfort associated with the urge to urinate [8]. Similarly, studies have demonstrated patients with IC/BPS possess a high prevalence of lower urinary tract symptoms such as urgency and frequency [9]. Should therapy directed at either urinary urgency or bladder pain fail to be efficacious, one may have to consider an alternative diagnosis and treatment [10]. IC/BPS is important to consider as an alternative diagnosis in treatment refractory OAB [11]. This is especially true in cases of the “dry” type of OAB, particularly when there is an uncomfortable urge and no fear of leakage. In fact, it has been suggested that this phenotype maybe more consistent with IC/BPS [6••]. Similarly, differentiating phenotypes of IC/BPS may be critical to appropriately direct therapies [12].
Prior efforts to standardize diagnosis of IC/BPS, such as the using National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) criteria or demonstrating Hunner’s lesions, were deemed too restrictive [13]. NIDDK criteria were originally developed to aid in structuring research reporting, but such rigorous criteria excluded many IC/BPS patients when implemented clinically. Similarly, only a minority of patients with IC/BPS are found with Hunner’s lesions. Perhaps considering the two conditions as a spectrum of disease might broaden a clinician’s toolbox and formulary. This review strives to reconsider the concept of the two conditions as a continuum.
Patient History
Urgency characterizes OAB and is also highly prevalent in IC/BPS symptomology. In fact, in 1988, Abrams published the ICS standardized term urinary urgency, which was defined as a strong desire to void accompanied by the fear of leakage or fear of pain [14]. The terminology that physicians use to describe symptoms during patient interviews may confound the distinction between the two conditions. Frequently, the language used to classify a patient’s bladder sensations does not reflect the description provided by the patient [15]. In a focus group study by Heeringa et al., normal bladder sensations in patients’ own terms were often described not as urgency, but as “pressure” and “tingling”; urgency to void was not a pathologic sensation but an intensification of a normal desire to void for both healthy and OAB patients [16]. It may be that healthy persons are better able to choose which sensations reach a conscious level, while OAB patients are less able to suppress awareness such sensations [16]. OAB and IC/BPS patients often describe their urinary urgency as pressure, awareness, or discomfort; the similar descriptors may confound the clinician’s ability to distinguish urinary urgency from bladder pain, the hallmark symptom of IC/BPS [17].
Focus groups of OAB patients previously demonstrated frequent misconceptions among patients and poor communication regarding storage symptoms between the physician and patient [18]. Patients who were able to express their feelings and opinions fully and who perceived that a full discussion of the problem had taken place exhibit improved symptom resolution, functional and physiologic status, and pain control [19].
Greenberg et al. examined the relationship between urgency and pain in IC/BPS. The majority (65%) of the 173 respondents agreed that urgency was linked to relief of pain, while 21% of the respondents linked urgency to fear of incontinence. In cases where there was fear of leakage (n = 36), there was also the urge to relieve pain 64% of the time [20]. Clinicians have long recognized the complexity of assessing symptomatology in OAB and IC/BPS. Since symptoms are subjective, questionnaires have been used for objective assessment of symptoms during diagnosis and follow-up.
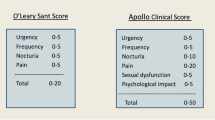
Our group recently developed a nomogram to distinguish the fundamental features of OAB and IC/BPS, with the goal of improving patient screening and classification. Validated questionnaires, the female Genitourinary Pain Index (fGUPI), OAB Questionnaire, Interstitial Cystitis Symptom Index, and Interstitial Cystitis Problem Index were retrospectively reviewed in a cohort of 50 patients with OAB, IC/BPS, and controls. Questionnaire scores were able to distinguish controls from patients with storage LUTS but were not able to discern between OAB and IC/BPS. Eight individual questions from these questionnaires were significantly different between OAB and IC/BPS patients, spanning two distinct symptom domains: urgency incontinence and bladder pain. In combination with a bother score to distinguish symptomatic patients, a novel scoring system describing these domains was used to create a nomogram, subsequently validated in a second cohort of 150 patients. This simple nomogram provided 91% diagnostic accuracy, which may facilitate better classification or prognostic stratification for patients with complex presentations. This study also observed that 25% of patients diagnosed with IC/BPS also demonstrated urge incontinence, while 35% of patients with OAB described bladder pain as well [6••].
We previously conducted separate focus groups of women with OAB-wet and OAB-dry [5]. OAB-dry without fear of leakage was considered to correlate with a pain syndrome. As urgency is not specific to any clinical entity, an older definition of OAB included fear of leakage in the criteria [21], which may better define the OAB population. Some experts believe that OAB-dry without leakage should not fall under the umbrella of OAB [5].
Reynolds et al. examined relationships between OAB symptoms, somatic symptoms, and specific chronic pain conditions in which central sensitization is thought to play a primary role. Among 116 women with OAB, over half (54%) associated the urge to urinate with pain, pressure, or discomfort. There was a significant positive correlation between OAB symptoms, somatic symptoms, and overall pain intensity [8]. Similarly, the Multidisciplinary Approach to the Study of Chronic Pelvic Pain (MAPP) Research Network has also reported patients with chronic pelvic pain have associated non-urologic functional somatic syndromes. Thirty-eight percent of 424 patients declared associated syndromes, such as fibromyalgia, irritable bowel syndrome, or chronic fatigue syndrome [22].
FitzGerald et al. evaluated patients with IC/BPS, OAB, SUI, and controls to describe the location of urinary urgency or bladder discomfort. Controls localized the sensation to suprapubic area only, more than half of IC/BPS patients localized the urge to void to the suprapubic and vulvar/urethral regions. About 20% of OAB patients localized urge to the same places. Most OAB patients described the sensation in the suprapubic area only. Some IC/BPS patients, however, reported their urinary discomfort as in the low back, upper and lateral buttocks, lower abdomen, and upper thighs [17], which could represent a different phenotypic variant.
Exam Findings
When considering the diagnosis IC/BPS or OAB, it is imperative to include at a minimum a thorough history, physical exam, and urinalysis and to consider the possibility of confounding diagnosis (e.g., malignancy, neurological disease) [2•, 3]. Physical exam may demonstrate suprapubic tenderness, anterior vaginal wall and bladder tenderness, or trigger points in the levator ani musculature [11, 23]. Pelvic floor spasm may be interpreted as pain in both IC/BPS and OAB, but transvaginal palpation of the bladder that does not elicit pain is less likely in IC/BPS [11].
In the National Institutes of Health (NIH) Interstitial Cystitis Database (ICDB) study, 17.5% of patients exhibited involuntary bladder contractions during urodynamics studies [24]. Glomerulations found cystoscopically were used as criteria in the past, but according to Waxman et al., were no more frequent in IC/BPS patients than in normal controls [25]. The ICDB study also did not observe an association between the presence of bloody effluence or glomerations after hydrodistention with symptoms of urinary pain or urgency; however, the study did note increased urgency in patients with a bladder capacity ≤ 400 ml. There was an association between Hunner’s lesions and pain during the 4 weeks preceding cystoscopy with hydrodistention. Hunner’s lesions were also associated with increasing levels of bodily pain [26]. However, Hunner’s lesions may be present in as few as 4% of IC/BPS patients [11], thus using a Hunner’s lesion as inclusion criteria may be too strict. In fact, a growing number of clinicians support the separation of patients with Hunner’s lesions from those without ulceration with independent diagnostic terminology [27]. Additionally, glomerulations are not specific to IC/BPS and do not help guide treatment options or correlate with treatment outcomes [11].
Experts treating OAB have widely varying practice regarding use of anatomic and functional studies with cystoscopy and urodynamics, likely because there is no reliable objective test to diagnose this condition [28]. The 2019 AUA/SUFU Guidelines pertaining to the diagnosis and treatment of non-neurogenic OAB in adults only categorize a careful history, physical exam, and urinalysis as absolutely necessary. Other components of a workup, including urine cultures, post-void residual, bladder diaries, and symptom questionnaires are left to the discretion of the physician. In fact, the guidelines specifically state that urodynamics, cystoscopy, and imaging studies should not be used in the initial workup of the uncomplicated OAB patient [2•]. The 2014 AUA guidelines pertaining to IC/BPS syndrome, however, recommend a broader initial workup in the patient presenting with an “unpleasant” sensation related to the bladder, present for more than 6 weeks without another identifiable cause including history/physical exam, post-void residual, voiding diary, urinalysis and culture, cytology (if smoking history), and symptom questionnaires [3].
Overlapping Therapies
As many symptoms of IC/BPS and OAB overlap, it is not surprising that common treatments have been employed for both conditions. While treatment for both are aimed at alleviation of symptoms and improving quality of life, IC/BPS and OAB treatment guidelines differ substantially. The evidence to guide therapeutic decisions in IC/BPS is lacking in comparison with the robust literature on OAB. Studies of IC/BPS patients have widely variable inclusion criteria, methodology, and outcomes measures. Guidelines exist, however, to help clinicians and patients move on to new therapies as needed. The 2019 AUA/SUFU OAB guidelines recommend behavioral therapies, pharmacologic management, PTNS/neuromodulation/intradetrusor onabotulinum toxin A, and augmentation/diversion as progressively employed treatments. The AUA guidelines pertaining to patients with uncomplicated confirmed IC/BPS are relatively more complex, but overlap with OAB treatment guidelines in several ways (although there are important differences, e.g., oral anticholinergics). Specifically, behavioral modification, oral medications (amitriptyline, cimetidine, PPS), cystoscopy/hydrodistention/fulguration, intradetrusor onabotulinum toxin A/neuromodulation, cyclosporine, and surgery are the escalating recommended treatments [3].
Considering these two diseases as a spectrum may help explain treatment failures and help expand potential therapeutic options. For example, refractory OAB has no standardized definition but the name implies incomplete symptom response to behavioral and pharmacologic therapy [10]. Perhaps an explanation for treatment failure in a proportion of OAB patients is the misdiagnosis in a patient who actually has IC/BPS [10, 29].
Antimuscarinic and sympathomimetic therapies are well-established options for OAB to ameliorate symptoms of urgency and frequency. The use of these therapeutic agents, however, is not well established in IC/BPS. In fact, according to NIDDK criteria, a response to antimuscarinics excludes a diagnosis of IC/BPS. While antimuscarinics do not appear to decrease urinary frequency in IC/BPS patients [30•], a large proportion of IC/BPS patients take such medications [31]. One study demonstrated some success with anticholinergics in combination with intravesical medications [32]. Mirabegron, a beta-3 adrenergic receptor agonist, may be a useful adjunct to help with urgency, but not necessarily pain, in IC/BPS patients [33•]. Of note, OAB and IC/BPS both share high rates of treatment failures and non-compliance with medication [29, 34].
Sacral neuromodulation (SNM) is used for urinary frequency, urgency, and urgency incontinence in OAB patients. Use in IC/BPS patients is limited [35•], but has demonstrated efficacy in helping the frequency/urgency component of IC/BPS. SNM was noted to improve the average global response assessment scale in IC/BPS patients who had failed prior therapies in a small series. Revision and explanation rates, however, were high due to lack of efficacy [36].
A prospective, multicenter, randomized, double-blinded, placebo-controlled clinical trial studied the use of onabotulinumtoxin-A in IC/BPS. Forty patients who had failed at least 6 months of conventional treatment and met NIDDK criteria for IC/PBS but lacked Hunner’s lesions received onabotulinumtoxin-A followed by hydrodistention. In comparison with 20 patients who received normal saline followed by hydrodistention, the onabotulinumtoxin-A group had significantly decreased visual analog scores (VAS) for pain (baseline 5.3 ± 2.6; 8 weeks 2.7 ± 2.7) compared with the normal saline group (p = 0.021; baseline 3.7 ± 2.9; 8-week follow-up 2.8 ± 2.5). The study also demonstrated an increased bladder capacity in the onabotulinumtoxin-A group in comparison with the controls (onabotulinumtoxin-A, baseline 264 ± 120.1; 8 weeks 332 ± 157.5, and normal saline, baseline 297 ± 115.7; 8 week 154.5 ± 102.9, p = 0.020). Significantly higher rates of dysuria were seen in the onabotulinumtoxin-A-treated group (13% and 16% at 4 and 8 weeks, respectively) in comparison with the normal saline group (1% at both 4 and 8 weeks). There was no difference in the rate of UTI or hematuria in the two groups and only one patient in the onabotulinumtoxin-A group experienced urinary retention [37••].
Conclusions
OAB and IC/BPS symptoms overlap significantly and the conditions have been demonstrated to coexist in many patients. IC/BPS and OAB have heterogeneous presentations and response to therapy with a paucity of distinguishing features. At this time, we are still learning which IC/BPS patients will respond to individual therapies. Clinical phenotyping and classification of IC/BPS variants [12] has been suggested, as has the stratification of OAB [28], as methods to help guide diagnosis and treatment. Such work is currently being done by the Multidisciplinary Approach to the study of Chronic Pelvic Pain (MAPP) Network and the Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN) and may help explain therapeutic failures and guide treatment in the future [12].
It is not clear if patients with IC/BPS and OAB are unique populations or specific phenotypes of the same condition [6••] and we conclude that OAB-dry without fear of leakage may actually be a variant of IC/BPS. Unbiased phenotyping based on more accurate symptomatic descriptions may help reveal the correlations of variants of lower urinary tract symptoms with both prognosis and treatment responses.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20.
• Lightner DJ, Gomelsky A, Souter L, Vasavada SP. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU Guideline Amendment 2019. J Urol. 2019;202(3):558–63. https://doi.org/10.1097/JU.0000000000000309Updated AUA/SUFU guidelines pertaining to the diagnosis and treatment of AUA and OAB. The current guideline included updates pertaining to relevant literature published through October 2018.
Hanno PM, Erickson D, Moldwin R, Faraday MM, The American Urological Association. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol. 2015;193(5):1545–53.
Malde S, Palmisani S, Al-Kaisy A, Sahai A. Guideline of guidelines: bladder pain syndrome. BJU Int. 2018;122(5):729–43.
Anger JT, Le TX, Nissim HA, Rogo-Gupta L, Rashid R, Behniwal A, et al. How dry is “OAB-dry”? Perspectives from patients and physician experts. J Urol. 2012;188(5):1811–5.
•• Ackerman AL, Lai HH, Parameshwar PS, Eilber KS, Anger JT. Symptomatic overlap in overactive bladder and interstitial cystitis/bladder pain syndrome: development of a new algorithm. BJU Int. 2019;123(4):682–93 In this study, a novel scoring system including urgency incontinence and bladder pain was validated with 91% accuracy in differentiating between OAB and IC/BPS.
Kowalik CG, Cohn JA, Delpe S, Kaufman MR, Wein A, Dmochowski RR, et al. Painful bladder symptoms related to somatic syndromes in a convenience sample of community women with overactive bladder symptoms. J Urol. 2018;200(6):1332–7.
Reynolds WS, Mock S, Zhang X, Kaufman M, Wein A, Bruehl S, et al. Somatic syndromes and chronic pain in women with overactive bladder. Neurourol Urodyn. 2017;36(4):1113–8.
Sammarco AG, Kobernik EK, Haefner HK, Till SR, Berger MB. Lower urinary tract symptoms in a chronic pelvic pain population. Female pelvic medicine & reconstructive surgery. 2019.
Apostolidis A, Averbeck MA, Sahai A, Rahnama’i MS, Anding R, Robinson D, et al. Can we create a valid treatment algorithm for patients with drug resistant overactive bladder (OAB) syndrome or detrusor overactivity (DO)? Results from a think tank (ICI-RS 2015). Neurourol Urodyn. 2017;36(4):882–93.
Macdiarmid SA, Sand PK. Diagnosis of interstitial cystitis/ painful bladder syndrome in patients with overactive bladder symptoms. Rev Urol. 2007;9(1):9–16.
Nickel JC, Shoskes D, Irvine-Bird K. Clinical phenotyping of women with interstitial cystitis/painful bladder syndrome: a key to classification and potentially improved management. J Urol. 2009;182(1):155–60.
Hanno PM, Landis JR, Matthews-Cook Y, Kusek J, Nyberg L Jr. The diagnosis of interstitial cystitis revisited: lessons learned from the National Institutes of Health Interstitial Cystitis Database study. J Urol. 1999;161(2):553–7.
Abrams P, Blaivas JG, Stanton SL, Andersen JT. The standardisation of terminology of lower urinary tract function. The International Continence Society Committee on Standardisation of Terminology. Scand J Urol Nephrol Suppl. 1988;114:5–19.
Heeringa R, de Wachter SG, van Kerrebroeck PE, van Koeveringe GA. Normal bladder sensations in healthy volunteers: a focus group investigation. Neurourol Urodyn. 2011;30(7):1350–5.
Heeringa R, van Koeveringe GA, Winkens B, van Kerrebroeck PE, de Wachter SG. Do patients with OAB experience bladder sensations in the same way as healthy volunteers? A focus group investigation. Neurourol Urodyn. 2012;31(4):521–5.
FitzGerald MP, Kenton KS, Brubaker L. Localization of the urge to void in patients with painful bladder syndrome. Neurourol Urodyn. 2005;24(7):633–7.
Smith AL, Nissim HA, Le TX, Khan A, Maliski SL, Litwin MS, et al. Misconceptions and miscommunication among aging women with overactive bladder symptoms. Urology. 2011;77(1):55–9.
Stewart MA. Effective physician-patient communication and health outcomes: a review. Cmaj. 1995;152(9):1423–33.
Greenberg P, Brown J, Yates T, Brown V, Langenberg P, Warren JW. Voiding urges perceived by patients with interstitial cystitis/painful bladder syndrome. Neurourol Urodyn. 2008;27(4):287–90.
Abrams P, Hanno P, Wein A. Overactive bladder and painful bladder syndrome: there need not be confusion. Neurourol Urodyn. 2005;24(2):149–50.
Krieger JN, Stephens AJ, Landis JR, Clemens JQ, Kreder K, Lai HH, et al. Relationship between chronic nonurological associated somatic syndromes and symptom severity in urological chronic pelvic pain syndromes: baseline evaluation of the MAPP study. J Urol. 2015;193(4):1254–62.
Lapides J. Observations on interstitial cystitis. Urology. 1975;5(5):610–1.
Nigro DA, Wein AJ, Foy M, Parsons CL, Williams M, Nyberg LM Jr, et al. Associations among cystoscopic and urodynamic findings for women enrolled in the Interstitial Cystitis Data Base (ICDB) Study. Urology. 1997;49(5A Suppl):86–92.
Waxman JA, Sulak PJ, Kuehl TJ. Cystoscopic findings consistent with interstitial cystitis in normal women undergoing tubal ligation. J Urol. 1998;160(5):1663–7.
Messing E, Pauk D, Schaeffer A, Nieweglowski M, Nyberg LM Jr, Landis JR, et al. Associations among cystoscopic findings and symptoms and physical examination findings in women enrolled in the Interstitial Cystitis Data Base (ICDB) Study. Urology. 1997;49(5A Suppl):81–5.
Fall M, Logadottir Y, Peeker R. Interstitial cystitis is bladder pain syndrome with Hunner’s lesion. Int J Urol. 2014;21(Suppl 1):79–82. https://doi.org/10.1111/iju.12325.
Lee UJ, Scott VC, Rashid R, Behniwal A, Wein AJ, Maliski SL, et al. Defining and managing overactive bladder: disagreement among the experts. Urology. 2013;81(2):257–62.
Nitti VW, Kopp Z, Lin AT, Moore KH, Oefelein M, Mills IW. Can we predict which patient will fail drug treatment for overactive bladder? A think tank discussion. Neurourol Urodyn. 2010;29(4):652–7.
• Kim A, Hoe KO, Shin JH, Choo MS. Evaluation of the incidence and risk factors associated with persistent frequency in interstitial cystitis/bladder pain syndrome and the efficacy of antimuscarinic treatment. Investig Clin Urol. 2017;58(5):353–8 This study reported thatantimuscarinics do not appear to decrease urinary frequency in IC/BPS patients.
Anger JT, Zabihi N, Clemens JQ, Payne CK, Saigal CS, Rodriguez LV. Treatment choice, duration, and cost in patients with interstitial cystitis and painful bladder syndrome. Int Urogynecol J. 2011;22(4):395–400.
Taneja R, Jawade KK. A rational combination of intravesical and systemic agents for the treatment of interstitial cystitis. Scand J Urol Nephrol. 2007;41(6):511–5.
• Di Lena M, Tolls V, Kelly KL, Nickel JC. Mirabegron as adjuvant treatment for patients with interstitial cystitis/bladder pain syndrome. Can Urol Assoc J. 2018;12(3):E100–e4 Mirabegron, a beta-3 adrenergic receptor agonist, may be a useful adjunct to help with urgency, but not necessarily pain, in IC/BPS patients.
Kim TH, Lee KS. Persistence and compliance with medication management in the treatment of overactive bladder. Investig Clin Urol. 2016;57(2):84–93.
• Tutolo M, Ammirati E, Van der Aa F. What is the best treatment option for coexisting pelvic floor dysfunctions? Eur Urol Focus. 2017;3(6):532–4 Sacral neuromodulation (SNM) is used for urinary frequency, urgency, and urgency incontinence in OAB patients. Use in IC/BPS patients is limited (35), but has demonstrated efficacy in helping the frequency/urgency component of IC/BPS.
Gajewski JB, Al-Zahrani AA. The long-term efficacy of sacral neuromodulation in the management of intractable cases of bladder pain syndrome: 14 years of experience in one centre. BJU Int. 2011;107(8):1258–64.
•• Kuo HC, Jiang YH, Tsai YC, Kuo YC. Intravesical botulinum toxin-A injections reduce bladder pain of interstitial cystitis/bladder pain syndrome refractory to conventional treatment—a prospective, multicenter, randomized, double-blind, placebo-controlled clinical trial. Neurourol Urodyn. 2016;35(5):609–14 This prospective, multicenter, randomized, double-blinded, placebo-controlled clinical trial studied the use of Onabotulinumtoxin-A in IC/BPS patients. Onabotulinumtoxin-A was associated with significantly decreased visual analog scores (VAS) for pain and increased bladder capacity in comparison to controls.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Jennifer T. Anger is an expert witness for Boston Scientific. Dr. Kai B. Dallas, Dr. Lenore A. Ackerman, and Dr. Carrie S. Stewart declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All procedures performed in studies involving human participants performed by the authors were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Reconstructed Bladder Function & Dysfunction
Rights and permissions
About this article
Cite this article
Dallas, K.B., Stewart, C.S., Ackerman, L.A. et al. OAB and IC/BPS: Two Conditions or a Continuum of One?. Curr Bladder Dysfunct Rep 15, 15–20 (2020). https://doi.org/10.1007/s11884-019-00567-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-019-00567-y