Abstract
Purpose of Review
The majority of international guidelines for cardiovascular disease (CVD) prevention recommend moderate intake of low fat or fat-free products, and limiting full fat dairy food because of its high saturated fatty acid content. Recent equivocal observational studies and greater understanding of the complex nature of dairy foods has led to reappraisal for some types of dairy foods.
Recent Findings
Current guidelines from major cardiovascular societies have differed; interpretation of major observational studies has been inconsistent. Apart from the adverse effect of butter, consumption of more complex dairy products notably fermented varieties, yogurt in particular, appears to be inversely associated with outcomes of CVD and type 2 diabetes (T2D). Reduced fat in dairy food appears advantageous but is no longer a unanimous view although is preferred for people at increased CVD risk and dyslipidemia.
Summary
Changed evidence has led to new advice regarding consumption of some dairy foods. The apparent beneficial effects of cheese, fermented milk, and yogurt allow for increased consumption of nutritious staple foods. Reduced fat yogurt may be desirable as part of diets for individuals with CVD or T2D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The associations between major food groups and cardiovascular disease (CVD) and type 2 diabetes mellitus (T2D) have been more contentious with respect to dairy foods than with other foods. The recent 2019 American College of Cardiology/American Heart Association (ACC/AHA) guidelines that are predominantly clinical but include brief commentaries on diet have mostly avoided advice based on individual nutrients and have opted for more or less recommended food groups [1•]. Notably, mention of dairy foods is absent. The reasoning is as follows: “The evidence is mixed with regard to the effectiveness of dairy intake to reduce ASCVD (atherosclerotic cardiovascular disease) risk factors which is why it is not included in the list of foods for their recommendation”.
By contrast, the 2019 European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) guidelines detail foods that raise LDL cholesterol and by inference raise the risk of CVD accordingly [2•]. Their recommendations for dairy food consumption is given under three headings: (i) “To be preferred: skimmed milk and yoghurt”; (ii) “To be used in moderation: low-fat milk, low-fat cheese, and other milk products”; and (iii) “To be chosen occasionally in limited amounts: regular cheese, whole milk, cream, and yoghurt”. There is reference to preferred fats/oils: “Unsaturated fat-rich oils from safflower, sunflower, rapeseed, flaxseed, corn, olives, or soybean were shown to reduce LDL cholesterol levels (− 042 to − 0.20 mmol/L) when used in substitution of saturated fatty acid-rich fats like butter or lard”.
These are substantial differences from the four major organisations that influence guidance to the health profession in the cardiovascular area. The change from previous AHA positions is substantial. In 2006 advice was to consume low-fat dairy: “Select fat-free skim milk and low-fat (1%) dairy products” [3]. The purpose of this review is to analyse the relevant recent publications up to August 2021 and attempt to provide a consensus of the views in those reports.
Nature and Limitations of Evidence
Most of the evidence to be reviewed is not based on randomized controlled trials (RCTs) but on observational studies and prospective cohort studies which are population studies that collectively reflect the eating habits of tens or hundreds of thousands of free-living individuals. The large numbers provide confidence in the outcome results especially if based on lengthy periods of close observation. Nevertheless, the data reflect recollected eating patterns, approximate amounts of foods, and imprecise measurements. Importantly, in many instances, they do not adequately account for confounders of which the foods that are substituted for changes in dairy consumption are important. The matrix of most dairy foods is complex comprising a number of nutrients within differing physical formats including changes due to fermentation.
The predictive reliability of observational and cohort studies has been attempted by simulating a target trial of previously recommended dietary interventions sustained over many years using data from observational and cohort studies [4•]. The estimated 20-year risk of all-cause mortality through implementation of AHA food-based goals [5], using data from three prospective cohort studies of men [Health Professional Follow-up Study (HFPS)] and women (Nurses’ Health Studies I and II, NHS, and NHS II) [6•], was not markedly dissimilar from the actual mortalities. The estimated 20-year mortality risks under a dietary intervention versus no intervention were 21.9% compared with 25.8%, respectively, in the HPFS; 10.0% compared with 12.6%, respectively, in the NHS; and 2.1% compared with 2.5%, respectively, in the NHS II [4•]. These data support the interpretation of such studies provided duration is long and population size large, the conclusion being that adherence to the earlier food-based AHA Dietary Goals starting in mid-life may reduce the 20-year risk of mortality.
In the absence of RCTs, the focus has been in recent years on food groups rather than on nutrients and on estimating risks and benefits by patterns of healthy eating.
Dairy Consumption and Cardiovascular Disease
Advice regarding the inadvisability of consuming dairy food arose from a general guidance to avoid fatty foods with high-saturated fatty acid content. Such foods included fatty meats especially processed meats and fried foods with the focus on “total fat”. The approximate fat content of cow’s milk is 3–4% and the fatty acid composition of dairy fat varies with the breed and nutrition. Only recently has advice regarding dairy intake taken into account the whole food and the compositional variety in the matrix of individual products. Such recognition has modified attitudes while not entirely dismissing the importance of the fat content. The evidence relating to differing interpretations and guidance is the substance of this review.
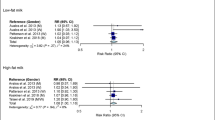
Well researched meta-analyses of the association of dairy foods with cardiovascular health have been published with increasing frequency. Fontecha et al. have analyzed 12 meta-analyses involving RCTs as well as the updated meta-analyses of RCTs [7]. Consumption of total dairy products, with either regular- or low-fat content or with different dose-responses, showed no association or lower risk of total incidence and mortality for CVD, coronary heart disease (CHD), and ischemic and hemorrhagic stroke. Meta-analyses of RCTs that investigated the potential effects of dairy products on selected biomarkers of CVD risk showed no adverse effects on blood lipids and blood pressure. However, fermented milks (i.e. yogurt, cheese) decreased those CVD risk biomarkers [7]. Based on data from 31 cohort studies, Alexander et al. reported an inverse trend between total dairy consumption and CVD and fatal and non-fatal CHD, which appears to have been driven by intake of cheese (Hazzard Ratio, HR of 0.86 for each 600 g/day of total dairy and 0.86 for each 50 g/day cheese intake) [8•]. High-fat dairy food tended to be positively associated with CHD contrasting with the inverse association with low-fat total dairy (HR 0.90). Gholami et al. reporting on 27 cohort studies found an inverse association between total dairy intake and CVD (HR 0.90) [9]. By contrast, neither Gholami et al. nor Bechthold et al. reporting on 24 cohort studies observed any effect of total dairy consumption on fatal and non-fatal CHD events [9, 10]. Surprisingly, the effect of total dairy on stroke was more striking than on CHD. Alexander et al. showed total dairy intake, including full-fat and low-fat dairy, was associated significantly and inversely with total stroke (HR 0·91) [8•]. Similarly, Gholami et al. reported a significant inverse association between total dairy intake, mainly attributable to low-fat dairy products, and stroke (HR 0.88) [9]. As with CHD, cheese intake was significantly inversely associated with total stroke (HR 0·87) [8•]. Cheese intake was also generally inversely associated with stroke in each of the 5 meta-analyses quoted by Fontecha et al. that had been published since 2014 [7]. Butter showed no association with CVD but the amounts consumed were small, interpretations based on increments of 10–14 g/day.
The conclusions indicate little association in either direction between total dairy consumption and CHD, but possibly an inverse association with stroke. Since the risk factors for CVD generally apply to both CHD and stroke, there may have been unrecognised confounding factors.
In one of the largest meta-analyses, Guo et al. reported on 29 prospective cohort studies including 928,465 participants of whom about one-tenth died, 28,419 suffered incident CHD events and 25,416 CVD events [11]. No associations were observed with total dairy or milk intake whether of low-fat or high-fat variety. This meta-analysis differed from those reported above in that it showed a modest but significant inverse association between total fermented dairy products (yogurt, cheese, and fermented milk; per 20 g/day) with mortality (HR 0.98) and CVD risk (HR 0.98) but not for CHD [11]. Further analyses showed cheese associated with a lower risk of CVD (HR 0.98 per 10 g/day), but not yogurt. In contrast, a recent report suggests a protective link between yogurt consumption and CVD. Cruijsen et al. have recently reported that during a 12-year follow-up of the Alpha Omega Cohort from the Netherlands that included 48,473 person-years and 2035 deaths, yogurt consumption was inversely associated with CVD mortality (HR 0.96 per 25 g/day) and all-cause mortality (HR 0.98 per 25 g/day) in patients with a history of myocardial infarction [12].
A further consideration is the nature of foods that substitute when dairy intake is reduced or increased. Brassard et al. have shown an attenuation in CVD risk when dairy food is replaced by unsaturated oil and wholegrain foods but not when substituted by refined carbohydrates or trans-fats [13]. Similar conclusions were drawn by Chen et al. based on data from three large US prospective cohort studies comprising 5,158,337 person-years who experienced 8974 CHD and 14,815 CVD events [14]. Dairy consumption compared with an equivalent amount of energy from carbohydrates (excluding fruit and vegetables) was not associated with total CVD events including both CHD and stroke. However, event rates were reduced when dairy fat was partially substituted by polyunsaturated fat (5% energy substitution led to a calculated 24% reduction in CVD risk) and by whole-grain foods, but not by refined carbohydrates or other animal fats, the latter increasing risk by 6%. In a large multi-racial study in the USA that included 36,364 person-years of follow-up between 2000 and 2010, full-fat dairy was inversely associated with subsequent CVD risk whereas meat fat was positively associated [15].
The issue of fat content was not resolved by the above meta-analyses since there were reports of lower HR for CHD and stroke with low-fat dairy in some but the converse or no difference in others. In other individual population studies, the findings also differed for total dairy although the potential benefit of fermented dairy foods was in general confirmed. One of the largest prospective cohorts is the Pan-European EPIC cohort [16•]. Reporting on 409,885 individuals from 9 countries who experienced 7198 CHD events during a mean of 12.6 years, only the consumption of meat was a significant predictor of CHD (HR 1.19 for a 100 g/day increment in red and processed meat). By contrast, the two fermented dairy foods yogurt and cheese were inversely associated with CHD events (yogurt HR 0.93 per 100 g/day increments; cheese HR 0.92 per 30 g/day increments). Similar conclusions were drawn from the Danish Diet, Cancer and Health Study of 54,903 individuals prospectively followed 15.9 years [17]. Risk of myocardial infarction was lower when low-fat or whole-fat milk was partially substituted by yogurt (HR 0.89 and 0.87, respectively for each 200 g/day replaced); or cheese (HR 0.96 and 0.95, respectively for every 20 g/day substituted for 200 g/day either full-fat or low-fat milk).
A study from Iran reported the 11-year follow-up of a prospective cohort in Golestan Province that included 42,403 participants and 1467 deaths from CVD [18]. Comparing the highest and the lowest quintiles for total dairy consumption showed 28% lower risk of CVD mortality. The main contributions to the reduced CVD were low-fat dairy (HR 0.74), yogurt (HR 0.84), and cheese (HR 0.74). Higher intake of high-fat dairy food and milk was not associated with CVD mortality. The foods displaced by dairy are not clear which is a recurring problem in nutritional epidemiology. This issue was addressed in the Australian Longitudinal Study on Women’s Health that also reported lower CVD risk among 7679 women free of CVD at baseline [19]. During a 15-year follow-up, women consuming large amounts of dairy especially yogurt and total fermented dairy products had a lower CVD risk (HR 0.84); however, the significance was diminished when other food components and total energy intake were taken into account.
In contrast to reports of a benefit or no effect of dairy on CVD, the recently published 2017 follow-up of 102,521 post-menopausal women in the Women’s Health Initiative (1,876,205 person-years, including 6993 deaths from CVD) showed consumption of total dairy protein was positively associated with higher risk of CVD (HR 1.11) [20]. In a Mendelian randomization analysis, Tognon et al. examined 103,256 adults (7121 deaths; mean follow-up of 13.7 years) from Northern Sweden [21]. Using a lactase single nucleotide polymorphism (an index of diary consumption), high consumers of non-fermented milk (≥ 2.5 times/day) experienced a 32% increased risk of all-cause mortality compared with those who consumed milk ≤ 1 time/week. Intake of low-fat milk reduced the risk; fermented milk and cheese were HR 0.90 and 0.93, respectively. Butter consumption increased risk (HR 1.11) confirming a previous finding also from Sweden. In the Swedish Mammography Cohort that included 33,636 women with 1392 cases during a follow-up of 11.6 years, there was a 34% higher CHD risk with butter intake whereas cheese was inversely associated (HR 0.74) [22].
Potential biomarkers of dairy have examined the relationship between intake and subsequent CVD events [23]. A 22-year study of 2907 adults aged ≥ 65 years and free of CVD at baseline measured three such biomarkers, the odd-chain saturated fatty acids pentadecanoic (C15:0), heptadecanoic (C17:0), and trans-palmitoleic (trans-16:1n-7) acids, serially over time [24]. However, none predicted future CVD.
Conclusions
The overall evidence likely supports the recent 2019 summary statement by Mozaffarian that “…dairy consumption is part of a healthy diet without strong evidence to favor reduced-fat products, while intakes of fermented dairy products such as yogurt and cheese appear especially beneficial” [25•]. Whereas this is applicable to a general population and likely important to patients with T2D (discussed below), it may not be the best advice to those individuals at high CVD risk because of the effects of dairy fat on LDL cholesterol, a major CVD risk factor. However not all experts agree with Mozaffarian [25•]. In review of trending nutrition controversies relevant to cardiovascular practice, Freeman et al. concluded “…there is general consensus that full-fat dairy products are major sources of saturated fat and sodium in the U.S. diet, and thus, should be limited; nevertheless reduced fat dairy products remain a convenient source of some essential vitamins and minerals, as well as high-quality protein” [26•].
Dairy Consumption and T2Diabetes
Inverse associations between total dairy consumption, particularly fermented dairy products and CVD, have strengthened in recent years. Whether the potential benefits on incident T2D would flow on to lowered risk for CVD is less certain but could be expected. Three recent reports have examined data from self-reported T2D cases from the Health Professionals Follow-Up Study (1986–2012), Nurses’ Health Study (1984–2012), and Nurses’ Health Study II (1991–2013). In the first report, dairy fat consumption obtained from 16,511 incident cases of T2D showed no association when compared with equivalent energy from carbohydrates (HR 0.98) [6•]. However, calculated HRs through dietary substitutions showed that replacing 5% of calories from dairy fat with animal fats (other than from dairy) increased risk of T2D by 17% whereas substituting 5% dairy food energy by whole-grains lowered risk by 7%. Replacement by refined grains increased risk marginally by 4%.
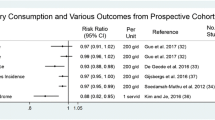
A second report assessed how changes in dairy foods, determined from serial questionnaires, related to incident diabetes [27]. After multivariable adjustment, a decrease in total dairy by > 1 serving/day over a 4-year period associated with 11% higher incidence of T2D, compared with maintaining a relatively stable consumption. Changes in low-fat milk, whole milk, and cream were not significantly associated with T2D. Increasing yogurt by > 0.5 serving/day associated with an 11% reduced T2D risk, whereas increasing cheese by > 0.5 serving/day associated with a 9% higher risk compared with maintaining stable intakes. Substituting 1 serving/day of yogurt or reduced-fat milk for cheese associated with lower T2D risk (16% and 12%, respectively).
The third report investigated differences in T2D risk by replacing consumption of red meat by other major dietary proteins assessed during sequential 4-year periods [28]. A decrease in red meat per serving/day during a 4-year period associated with a lower risk of T2D in the subsequent 4-year period when replaced with low-fat or high-fat dairy (HR 0.82 and HR 0.82, respectively), and comparable with a serving of fish or poultry (0.87 and 0.82, respectively).
In a meta-analysis reporting 4–22 cohort studies and from 4–23 populations including 64,227–566,875 participants for periods from 4 to 30 years, dairy consumption was available in 4810–44,474 cases of T2D in the two aggregated cohorts [29•]. Most studies reported inverse associations between total dairy foods and T2D incidence (HR 0.86–0.91) as well as for individual dairy products. The strongest inverse associations were with low-fat products (HR 0.81–0.83), especially low-fat milk (HR 0.82) and yogurt (HR 0.74–0.86); that for cheese was moderate. Dose–response analyses showed a decreased T2D risk for 200–400 g/day of total dairy products (HR 0.93–0.97) and 200 g/day of low-fat dairy products (HR 0.88–0.91).
A meta-analysis of 22 cohorts comprising 579,832 individuals and 43,118 cases of T2D confirmed the above findings of reduced incidence among those eating more yogurt (HR 0.86 for an intake of 80 g/day) and low-fat dairy (4% lower risk per 200 g/day) [30]. A systematic review and meta-analysis published in 2020, reported a 27% risk reduction for T2D with yogurt consumption [31]. Of note, cheese associated with a significant 24% increase in T2D risk.
A Mendelian randomization study based on a lactase polymorphism carried out in 97,811 individuals from a Danish general population failed to demonstrate any association between T2D and milk consumption [32].
In the PREDIMED Study (PREvencion con DIeta MEDiterranea), 266 incident cases of T2D were reported over 4.3 years [33]. One serving daily of butter (12 g) and cheese (30 g) were both positively associated with T2D (HR 2.42 and 1.32, respectively), whereas whole-fat yogurt intake showed a 35% inverse association in this small cohort.
Using metabolomics profiling, Drouin-Chartier et al. showed a number of lipid species, mainly phospholipids, correlate with dairy consumption elicited through questionnaires [34]. Subsequent analyses examined associations between multivariate models of metabolites and incident T2D in 3 cohorts: baseline PREDIMED, 1-year follow-up PREDIMED, and a composite of the 3 major US cohorts. The findings while interesting are inconsistent. The baseline PREDIMED group showed that a composite of 38 unique metabolites representing, separately, consumption of total dairy, low-fat dairy, fermentable dairy, milk, and yogurt correlated inversely with T2D in agreement with other studies. However, the metabolite score modelling for the US cohorts showed a significant inverse correlation only for total dairy and milk, whereas the 1-year PREDIMED cohort following intervention with a Mediterranean diet showed a significant association only with intake of milk.
Biomarkers of dairy intake such as plasma pentadecanoic, heptadecaenoic, and trans-palmitoleic acids have been inversely associated with significantly lower risk for T2D [35]. This conclusion was based on 16 prospective cohort studies including 63,682 participants and 15,180 incident cases of T2D over a 9-year follow-up conducted among populations of differing ethnicity. In adjusted models, the HR for incident T2D per cohort specific 10th to 90th percentile range was 0.80 for 15:0, 0.65 for 17:0, 0.82 for t16:1n7; and 0.71 for their sum. Similar associations for 15:0, 17:0, and the sum of all three fatty acids were present in both genders, but with women experiencing a 20–27% lower risk than men. However, not all studies agree with this finding and a recent review documents studies that have shown both negative and positive associations between odd-chain fatty acids and T2D [23]. Odd-chain fatty acids, 15:0 in particular, are useful biomarkers of total dairy fat and are useful for monitoring dietary compliance [23]. However, there are a number of limitations, and thus, caution is warranted in the interpretation of associations between these biomarkers and CVD risk.
Conclusions
The evidence consistently suggests consuming dairy foods does not impact adversely on incident T2D and that fermented dairy foods especially yogurt, low-fat more than full-fat, may modify the risk of developing T2D. Within the context of current recommendations for plant-based foods, emphasizing whole grains, vegetables, fruits, and legumes and exclude animal products to prevent diabetes [36], it may be appropriate to include fermented dairy foods in a healthy pattern of eating.
Dairy Consumption and Cardio-Metabolic Risk
The effects of different dairy foods on LDL cholesterol especially when studied at equivalent fat content have been largely resolved. RCTs have compared butter and cheese mostly and have consistently shown a significantly greater increase in LDL cholesterol with butter [13, 37]. In fact, butter is a reliable positive control in trials of dietary fats and oils. In the EPIC–Norfolk Study in the United Kingdom, LDL cholesterol was inversely associated with an increase in total low-fat dairy and positively with high-fat dairy (total, butter, and high-fat cheese) [38•]. In an RCT that involved participants substituting 4.5% of energy with butter or refined olive oil, consumption of butter significantly increased LDL cholesterol when compared with olive oil [39].
Measurements of total “cardio-metabolic risk” or metabolic syndrome, comprising effects on plasma lipids, insulin sensitivity (mostly assayed by glycated hemoglobin) and adiposity, have improved with low-fat dairy products in some [23, 40•] but not all studies [23, 41, 42]. One study showed deterioration in insulin sensitivity after 12 weeks with 3.3 servings/day of either low-fat or full-fat dairy food [42]. By contrast, the PREDIMED Trial reported that in 930 incident cases of metabolic syndrome developed over 3.2 years, HRs for the comparison of extreme tertiles were 0.72 for low-fat dairy; 0.73 for low-fat yogurt; 0.78 for whole-fat yogurt; and 0.80 for low-fat milk; but 1.31 for cheese [43]. In a study of overweight and obese subjects, lysophosphatidylcholine, lyso-platelet-activating factor and several phospholipid fatty acids all indicative of dairy consumption, significantly associated with better insulin sensitivity [44].
Effects of dairy consumption on blood pressure have been inconclusive. In an RCT that compared 6-week isoenergetic diets comprising one daily serving of 31% fat cheddar cheese, with 3 daily servings of 1% fat milk and a dairy-free control diet, neither the low-fat nor the regular-fat dairy diets influenced ambulatory blood pressure [45]. The full-fat cheese diet raised plasma LDL cholesterol (5.8% and 7.0% compared with the control and milk diets, respectively) and LDL particle size compared with the other two periods. Milk and cheese raised plasma triglycerides (9.9% and 10.5%, respectively compared with the control diet), but there were no effects on C-reactive protein or glucose-insulin homeostasis.
Additional Aspects
The physical state of the lipid globules is important as demonstrated by the LDL cholesterol raising potential of butter compared with that of cheese or cream in which the milk fat is enclosed in a milk-fat globule membrane that is missing in butter [46]. This was demonstrated in an 8-week RCT of 40 g/day milk fat consumed either as butter or whipped cream (milk fat encased in globule membrane).
The effects of individual saturated fatty acids have generated considerable debate. For Jersey cows, dairy fat comprises 32% palmitic (C16:0), 14% stearic (C18:0), 11% myristic (C14:0), and 4% lauric acids (C12:0). Ruminant trans-fatty acids that account for 4% of fat in dairy food appear insufficient to increase LDL cholesterol, although when consumed in greater amount will raise LDL cholesterol, as would industrially hydrogenated vegetable oils [47]. Robust RCTs have shown almost similar increments in LDL cholesterol with myristic and palmitic fatty acids, and substantially greater increase when compared to oleic acid [48]. In fact, it has been suggested that myristic acid may be the most potent LDL cholesterol raising fatty acid in milk fat [49]. Lauric acid, a major component of coconut milk, raises LDL cholesterol compared with olive oil but not by as much as palmitic acid [50]. By contrast, stearic acid is neutral in its effect on LDL cholesterol [51].
A2 Milk for which largely unsubstantiated claims include favorable effects on CHD and type 1 diabetes has captured a minor percentage of the milk market. Most cow milk contains both A1 and A2 caseins, whereas human, goat, sheep, and other contain mostly A2 β-casein. The European Food Safety Authority comprehensively examined all of the claims and concluded that there was neither any cause-effect evidence of harmful A1 protein nor clear benefit from consuming A2 protein [52].
Conclusions
-
1.
Evidence regarding increased risk of consuming dairy food for future CVD remains uncertain. The risk is minor if at all for healthy individuals without CVD risk factors. For people at increased CVD risk, including individuals with T2D, some modification of dairy intake appears to reduce risk.
-
2.
The complex nature of dairy foods justifies distinguishing between butter that has the highest fat content and is frequently associated positively with increased CVD risk, and other dairy foods. Fermented dairy foods, fermented milk, yogurt, and cheese are more often than not negatively associated with CVD risk.
-
3.
With respect to T2D, evidence is more convincing that consuming fermented dairy foods, especially low-fat yogurt may contribute to prevention. Incident diabetes occurs less often in individuals whose intake of yogurt is at least 200 g/day.
-
4.
Cardiometabolic health as judged by reduced levels of LDL cholesterol and greater insulin sensitivity but not by lower blood pressure associates with greater consumption of low-fat fermented dairy foods.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
• Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):E596-E646. https://doi.org/10.1161/Cir.0000000000000678. Recent United States guidelines that include brief dietary advice but with no guidance on dairy food consumption.
• Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–88. https://doi.org/10.1093/eurheartj/ehz455. Recent European guidelines providing more specific guidance on limiting full-fat dairy food especially for persons at increased CVD risk.
American Heart Association Nutrition C, Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114(1):82–96. doi:https://doi.org/10.1161/CIRCULATIONAHA.106.176158.
• Chiu YH, Chavarro JE, Dickerman BA, Manson JE, Mukamal KJ, Rexrode KM et al. Estimating the effect of nutritional interventions using observational data: the American Heart Association's 2020 Dietary Goals and mortality. Am J Clin Nutr. 2021. doi:https://doi.org/10.1093/ajcn/nqab100. Interesting study that estimated 20-year mortality rates under dietary intervention based on much earlier AHA guidance, versus no dietary intervention, using recent hard data from major cohort studies. The data showed mortality rates not markedly dissimilar between the estimated and actual rates supporting the strength of the guidelines.
Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. https://doi.org/10.1161/CIRCULATIONAHA.109.192703.
• Ardisson Korat AV, Li Y, Sacks F, Rosner B, Willett WC, Hu FB et al. Dairy fat intake and risk of type 2 diabetes in 3 cohorts of US men and women. Am J Clin Nutr. 2019;110(5):1192–200. doi:https://doi.org/10.1093/ajcn/nqz176. Based on dairy food consumption from the three large long-term cohorts in the United States those individuals, women and men, who developed incident type 2 diabetes showed no association with dairy food compared with those consuming equivalent energy from carbohydrate. However replacement of dairy fat with equivalent fat from other animal sources led to more cases of diabetes whereas replacement with equal energy from whole grains lowered risk.
Fontecha J, Calvo MV, Juarez M, Gil A, Martinez-Vizcaino V. Milk and dairy product consumption and cardiovascular diseases: an overview of systematic reviews and meta-analyses. Adv Nutr. 2019;10(suppl_2):S164-S89. doi:https://doi.org/10.1093/advances/nmy099.
• Alexander DD, Bylsma LC, Vargas AJ, Cohen SS, Doucette A, Mohamed M et al. Dairy consumption and CVD: a systematic review and meta-analysis. Br J Nutr. 2016;115(4):737–50. doi:https://doi.org/10.1017/S0007114515005000. Valuable overview of findings from 12 meta-analyses and RCTs that concluded an absence of association between dairy consumption and major cardiovascular outcomes although individual meta-analyses showed that fermented dairy products, yogurt in particular, were associated with reduced CVD edvents including stroke
Gholami F, Khoramdad M, Esmailnasab N, Moradi G, Nouri B, Safiri S, et al. The effect of dairy consumption on the prevention of cardiovascular diseases: a meta-analysis of prospective studies. J Cardiovasc Thorac Res. 2017;9(1):1–11. https://doi.org/10.15171/jcvtr.2017.01.
Bechthold A, Boeing H, Schwedhelm C, Hoffmann G, Knuppel S, Iqbal K, et al. Food groups and risk of coronary heart disease, stroke and heart failure: a systematic review and dose-response meta-analysis of prospective studies. Crit Rev Food Sci Nutr. 2019;59(7):1071–90. https://doi.org/10.1080/10408398.2017.1392288.
Guo J, Astrup A, Lovegrove JA, Gijsbers L, Givens DI, Soedamah-Muthu SS. Milk and dairy consumption and risk of cardiovascular diseases and all-cause mortality: dose-response meta-analysis of prospective cohort studies. Eur J Epidemiol. 2017;32(4):269–87. https://doi.org/10.1007/s10654-017-0243-1.
Cruijsen E, Jacobo Cejudo MG, Kupers LK, Busstra MC, Geleijnse JM. Dairy consumption and mortality after myocardial infarction: a prospective analysis in the Alpha Omega Cohort. Am J Clin Nutr. 2021;114(1):59–69. https://doi.org/10.1093/ajcn/nqab026.
Brassard D, Tessier-Grenier M, Allaire J, Rajendiran E, She Y, Ramprasath V, et al. Comparison of the impact of SFAs from cheese and butter on cardiometabolic risk factors: a randomized controlled trial. Am J Clin Nutr. 2017;105(4):800–9. https://doi.org/10.3945/ajcn.116.150300.
Chen M, Li Y, Sun Q, Pan A, Manson JE, Rexrode KM, et al. Dairy fat and risk of cardiovascular disease in 3 cohorts of US adults. Am J Clin Nutr. 2016;104(5):1209–17. https://doi.org/10.3945/ajcn.116.134460.
de Oliveira Otto MC, Mozaffarian D, Kromhout D, Bertoni AG, Sibley CT, Jacobs DR Jr, et al. Dietary intake of saturated fat by food source and incident cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis. Am J Clin Nutr. 2012;96(2):397–404. https://doi.org/10.3945/ajcn.112.037770.
• Key TJ, Appleby PN, Bradbury KE, Sweeting M, Wood A, Johansson I et al. Consumption of meat, fish, dairy products, and eggs and risk of ischemic heart disease. Circulation. 2019;139(25):2835–45. doi:https://doi.org/10.1161/CIRCULATIONAHA.118.038813. Major multi-population study, the Pan-European EPIC cohort reported on 409,885 individuals experiencing 7198 CHD events over mean of 12.6 years. Total dairy was not a predictor of future events but increased consumption of yogurt and cheese were significantly associated with reduced risk.
Kvist K, Laursen ASD, Overvad K, Jakobsen MU. Substitution of milk with whole-fat yogurt products or cheese is associated with a lower risk of myocardial infarction: the Danish diet, cancer and health cohort. J Nutr. 2020;150(5):1252–8. https://doi.org/10.1093/jn/nxz337.
Farvid MS, Malekshah AF, Pourshams A, Poustchi H, Sepanlou SG, Sharafkhah M, et al. Dairy food intake and all-cause, cardiovascular disease, and cancer mortality: the Golestan cohort study. Am J Epidemiol. 2017;185(8):697–711. https://doi.org/10.1093/aje/kww139.
Buziau AM, Soedamah-Muthu SS, Geleijnse JM, Mishra GD. Total fermented dairy food intake is inversely associated with cardiovascular disease risk in women. J Nutr. 2019;149(10):1797–804. https://doi.org/10.1093/jn/nxz128.
Sun Y, Liu B, Snetselaar LG, Wallace RB, Shadyab AH, Kroenke CH, et al. Association of major dietary protein sources with all-cause and cause-specific mortality: prospective cohort study. J Am Heart Assoc. 2021;10(5):e015553. https://doi.org/10.1161/JAHA.119.015553.
Tognon G, Nilsson LM, Shungin D, Lissner L, Jansson JH, Renstrom F, et al. Nonfermented milk and other dairy products: associations with all-cause mortality. Am J Clin Nutr. 2017;105(6):1502–11. https://doi.org/10.3945/ajcn.116.140798.
Patterson E, Larsson SC, Wolk A, Akesson A. Association between dairy food consumption and risk of myocardial infarction in women differs by type of dairy food. J Nutr. 2013;143(1):74–9. https://doi.org/10.3945/jn.112.166330.
Riserus U, Marklund M. Milk fat biomarkers and cardiometabolic disease. Curr Opin Lipidol. 2017;28(1):46–51. https://doi.org/10.1097/MOL.0000000000000381.
de Oliveira Otto MC, Lemaitre RN, Song X, King IB, Siscovick DS, Mozaffarian D. Serial measures of circulating biomarkers of dairy fat and total and cause-specific mortality in older adults: the Cardiovascular Health Study. Am J Clin Nutr. 2018;108(3):476–84. https://doi.org/10.1093/ajcn/nqy117.
• Mozaffarian D. Dairy foods, obesity, and metabolic health: the role of the food matrix compared with single nutrients. Adv Nutr. 2019;10(5):917S-23S. doi:https://doi.org/10.1093/advances/nmz053. Recent review of the evidence relating dairy consumption to CVD outcomes recommending inclusion of dairy products within a healthy diet especially that of fermented dairy products such as yogurt and cheese.
• Freeman AM, Morris PB, Aspry K, Gordon NF, Barnard ND, Esselstyn CB et al. A Clinician's Guide for Trending Cardiovascular Nutrition Controversies: Part II. J Am Coll Cardiol. 2018;72(5):553–68. doi:https://doi.org/10.1016/j.jacc.2018.05.030. Recent review that addressed advice to cardiologists stressing that full-fat sources of dairy foods were major sources of saturated fat and sodium and should be limited, other than reduced fat dairy products that provided nutritional benefit.
Drouin-Chartier JP, Li Y, Ardisson Korat AV, Ding M, Lamarche B, Manson JE, et al. Changes in dairy product consumption and risk of type 2 diabetes: results from 3 large prospective cohorts of US men and women. Am J Clin Nutr. 2019;110(5):1201–12. https://doi.org/10.1093/ajcn/nqz180.
Wurtz AML, Jakobsen MU, Bertoia ML, Hou T, Schmidt EB, Willett WC, et al. Replacing the consumption of red meat with other major dietary protein sources and risk of type 2 diabetes mellitus: a prospective cohort study. Am J Clin Nutr. 2021;113(3):612–21. https://doi.org/10.1093/ajcn/nqaa284.
• Alvarez-Bueno C, Cavero-Redondo I, Martinez-Vizcaino V, Sotos-Prieto M, Ruiz JR, Gil A. Effects of milk and dairy product consumption on type 2 diabetes: overview of systematic reviews and meta-analyses. Adv Nutr. 2019;10(suppl_2):S154-S63. doi:https://doi.org/10.1093/advances/nmy107. Further analysis of incident type 2 dibetes participants in 4–22 cohort studies in whom dairy consumption was documented in 4810 - 44,474 showing that in the majority of the cohorts there was an inverse association between total dairy intake and diabetes. The strongest inverse associations were for low-fat dairy products especially low-fat milk and yogurt.
Gijsbers L, Ding EL, Malik VS, de Goede J, Geleijnse JM, Soedamah-Muthu SS. Consumption of dairy foods and diabetes incidence: a dose-response meta-analysis of observational studies. Am J Clin Nutr. 2016;103(4):1111–24. https://doi.org/10.3945/ajcn.115.123216.
Companys J, Pla-Paga L, Calderon-Perez L, Llaurado E, Sola R, Pedret A, et al. Fermented dairy products, probiotic supplementation, and cardiometabolic diseases: a systematic review and meta-analysis. Adv Nutr. 2020;11(4):834–63. https://doi.org/10.1093/advances/nmaa030.
Bergholdt HK, Nordestgaard BG, Ellervik C. Milk intake is not associated with low risk of diabetes or overweight-obesity: a Mendelian randomization study in 97,811 Danish individuals. Am J Clin Nutr. 2015;102(2):487–96. https://doi.org/10.3945/ajcn.114.105049.
Guasch-Ferre M, Becerra-Tomas N, Ruiz-Canela M, Corella D, Schroder H, Estruch R, et al. Total and subtypes of dietary fat intake and risk of type 2 diabetes mellitus in the Prevencion con Dieta Mediterranea (PREDIMED) study. Am J Clin Nutr. 2017;105(3):723–35. https://doi.org/10.3945/ajcn.116.142034.
Drouin-Chartier JP, Hernandez-Alonso P, Guasch-Ferre M, Ruiz-Canela M, Li J, Wittenbecher C, et al. Dairy consumption, plasma metabolites, and risk of type 2 diabetes. Am J Clin Nutr. 2021;114(1):163–74. https://doi.org/10.1093/ajcn/nqab047.
Imamura F, Fretts A, Marklund M, Ardisson Korat AV, Yang WS, Lankinen M, et al. Fatty acid biomarkers of dairy fat consumption and incidence of type 2 diabetes: a pooled analysis of prospective cohort studies. Plos Med. 2018;15(10):e1002670. https://doi.org/10.1371/journal.pmed.1002670.
Jardine MA, Kahleova H, Levin SM, Ali Z, Trapp CB, Barnard ND. Perspective: plant-based eating pattern for type 2 diabetes prevention and treatment: efficacy, mechanisms, and practical considerations. Adv Nutr. 2021. https://doi.org/10.1093/advances/nmab063.
Nestel PJ, Chronopulos A, Cehun M. Dairy fat in cheese raises LDL cholesterol less than that in butter in mildly hypercholesterolaemic subjects. Eur J Clin Nutr. 2005;59(9):1059–63. https://doi.org/10.1038/sj.ejcn.1602211.
• Trichia E, Luben R, Khaw KT, Wareham NJ, Imamura F, Forouhi NG. The associations of longitudinal changes in consumption of total and types of dairy products and markers of metabolic risk and adiposity: findings from the European Investigation into Cancer and Nutrition (EPIC)-Norfolk study, United Kingdom. Am J Clin Nutr. 2020;111(5):1018–26. doi:https://doi.org/10.1093/ajcn/nqz335. The EPIC Norfolk Study conducted in the United Kingdom reported that among individuals consuming low-fat dairy LDL-cholesterol levels were lower than among those consuming high-fat dairy (butter and high-fat cheese) in whom LDL-cholesterol increased.
Engel S, Tholstrup T. Butter increased total and LDL cholesterol compared with olive oil but resulted in higher HDL cholesterol compared with a habitual diet. Am J Clin Nutr. 2015;102(2):309–15. https://doi.org/10.3945/ajcn.115.112227.
• Mozaffarian D. Dairy foods and type 2 diabetes: profiling our metabolites and health. Am J ClinNutr. 2021. doi:https://doi.org/10.1093/ajcn/nqab134. Review of the effects of dairy food intake on parameters of the metabolic syndrome or cardio-metabolic health showing improved profiles associating with low-fat dairy products.
Raziani F, Tholstrup T, Kristensen MD, Svanegaard ML, Ritz C, Astrup A, et al. High intake of regular-fat cheese compared with reduced-fat cheese does not affect LDL cholesterol or risk markers of the metabolic syndrome: a randomized controlled trial. Am J Clin Nutr. 2016;104(4):973–81. https://doi.org/10.3945/ajcn.116.134932.
Schmidt KA, Cromer G, Burhans MS, Kuzma JN, Hagman DK, Fernando I, et al. The impact of diets rich in low-fat or full-fat dairy on glucose tolerance and its determinants: a randomized controlled trial. Am J Clin Nutr. 2021;113(3):534–47. https://doi.org/10.1093/ajcn/nqaa301.
Babio N, Becerra-Tomas N, Martinez-Gonzalez MA, Corella D, Estruch R, Ros E, et al. Consumption of yogurt, low-fat milk, and other low-fat dairy products is associated with lower risk of metabolic syndrome incidence in an elderly mediterranean population. J Nutr. 2015;145(10):2308–16. https://doi.org/10.3945/jn.115.214593.
Nestel PJ, Straznicky N, Mellett NA, Wong G, De Souza DP, Tull DL, et al. Specific plasma lipid classes and phospholipid fatty acids indicative of dairy food consumption associate with insulin sensitivity. Am J Clin Nutr. 2014;99(1):46–53. https://doi.org/10.3945/ajcn.113.071712.
Rancourt-Bouchard M, Gigleux I, Guay V, Charest A, Saint-Gelais D, Vuillemard JC, et al. Effects of regular-fat and low-fat dairy consumption on daytime ambulatory blood pressure and other cardiometabolic risk factors: a randomized controlled feeding trial. Am J Clin Nutr. 2020;111(1):42–51. https://doi.org/10.1093/ajcn/nqz251.
Rosqvist F, Smedman A, Lindmark-Mansson H, Paulsson M, Petrus P, Straniero S, et al. Potential role of milk fat globule membrane in modulating plasma lipoproteins, gene expression, and cholesterol metabolism in humans: a randomized study. Am J Clin Nutr. 2015;102(1):20–30. https://doi.org/10.3945/ajcn.115.107045.
Motard-Belanger A, Charest A, Grenier G, Paquin P, Chouinard Y, Lemieux S, et al. Study of the effect of trans fatty acids from ruminants on blood lipids and other risk factors for cardiovascular disease. Am J Clin Nutr. 2008;87(3):593–9. https://doi.org/10.1093/ajcn/87.3.593.
Zock PL, de Vries JH, Katan MB. Impact of myristic acid versus palmitic acid on serum lipid and lipoprotein levels in healthy women and men. Arterioscler Thromb. 1994;14(4):567–75. https://doi.org/10.1161/01.atv.14.4.567.
Kris-Etherton PM, Yu S. Individual fatty acid effects on plasma lipids and lipoproteins: human studies. Am J Clin Nutr. 1997;65(5 Suppl):1628S-S1644. https://doi.org/10.1093/ajcn/65.5.1628S.
Denke MA, Grundy SM. Comparison of effects of lauric acid and palmitic acid on plasma lipids and lipoproteins. Am J Clin Nutr. 1992;56(5):895–8. https://doi.org/10.1093/ajcn/56.5.895.
Yu S, Derr J, Etherton TD, Kris-Etherton PM. Plasma cholesterol-predictive equations demonstrate that stearic acid is neutral and monounsaturated fatty acids are hypocholesterolemic. Am J Clin Nutr. 1995;61(5):1129–39. https://doi.org/10.1093/ajcn/61.4.1129.
Scientific Report of EFSA prepared by a DATEX Working Group. Review of the potential health impact of β-casomorphins and related peptides. EFSA Scientific Report. 2009;231:1–107. https://doi.org/10.2903/j.efsa.2009.231r.
Funding
TAM is supported by an NH&MRC Senior Fellowship.
Author information
Authors and Affiliations
Contributions
PJN and TAM performed the literature search, drafted and critically revised the work.
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
All reported studies with human subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nestel, P.J., Mori, T.A. Dairy Foods: Is Its Cardiovascular Risk Profile Changing?. Curr Atheroscler Rep 24, 33–40 (2022). https://doi.org/10.1007/s11883-022-00984-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11883-022-00984-1