Abstract
Purpose of Review
In this review article, we focus on the mechanisms and features of acute coronary syndromes (ACS) with no ruptured plaque (NONRUPLA) highlighting the uncertainties over diagnostic evaluation and treatment.
Recent Findings
The most common cause of ACS is obstruction due to atherosclerotic plaque ruptured or erosion. In 14% of patients who present in the Emergency Department as myocardial infarction, the final diagnosis is ACS with NONRUPLA. Although the clinical presentation of NONRUPLA may mimic myocardial infarction, the underlying pathogenesis is different, and it may guide therapeutic approaches and overall prognosis that vary according to etiology.
Summary
The possible mechanisms of ACS with NONRUPLA are coronary embolism, acute dissection of the aorta or coronary artery, vasospasm, microvascular dysfunction, the imbalance between oxygen demand and supply, coronary trauma and stent complications, direct cellular toxicity and damage, Takotsubo syndrome, and myocardial infarction with non-obstructive coronary arteries (MINOCA).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute coronary syndrome (ACS) with no ruptured plaque (NONRUPLA) occurs in 14% of patients who present in the Emergency Department as myocardial infarction [1].
The possible mechanisms of ACS with NONRUPLA are wide ranging and can include coronary embolism, acute dissection of the aorta or coronary artery, vasospasm, microvascular dysfunction, the imbalance between oxygen demand and supply, coronary trauma and stent complications, direct cellular toxicity and damage, Takotsubo syndrome and myocardial infarction with non-obstructive coronary arteries (MINOCA) (Fig. 1).
Although clinical presentation (Table 1) may mimic myocardial infarction, the underlying pathogenesis of ACS with NONRUPLA may guide therapeutic approaches and overall prognosis. Therefore, in this review article, we focus on the mechanisms and features of ACS with NONRUPLA highlighting the uncertainties over diagnostic evaluation and treatment.
Mechanism of NONRUPLA
Coronary Embolism (CEm)
The underlying cause for more than 3% of ACS is coronary embolism (CEm). The embolism may be direct (caused by thrombotic materials originating from left heart chambers), paradoxical (caused by thrombotic material in the venous circulation), or iatrogenic [2]. Infective endocarditis used to be the most common cause of CEm but in the current population, non-infected valvular disease (prosthetic valve) is the most frequent cause. Other causes for CEm are arrhythmias, mural thrombus in the left ventricle due to idiopathic dilated cardiomyopathy, neoplastic disease, bone marrow, air emboli, even suture material, or talc following heart surgery [3].
The clinical presentation is related to the size of the embolus. For example, a smaller embolus will lodge more distally rather than a larger embolus that might impact a major coronary artery. The presentation may be typical of ACS with acute chest pain, electrocardiographic, and enzyme changes, or atypical such as dyspnea and congestive heart failure. In one of four patients, it is unrecognized due to either the mild symptoms that are ignored by the patient or the lack of symptoms. More commonly, the embolic infarcts are anterior, probably due to hemodynamic factors that favor diastolic blood flow into the left coronary artery, 75% of all cases [4, 24].
Once CEm is diagnosed by the demonstration of normal coronary arteries in the patient and a lack of collateral vessels in selective coronary arteriography, treatment should start immediately with long-term anticoagulants to prevent growth and additional new emboli. Also, additional antiplatelet drugs should be considered in patients with prosthetic heart valves [3, 25].
Infective endocarditis (infection of the endocardial surface of the heart, usually the valves) is no longer the most common cause of CEm because of recent improvements in diagnosis and management, so the incidence of CEm is relatively low, ranging from 3 to 11% [26], although autopsies have shown microemboli in 60% of patients with infective endocarditis. Mechanisms for myocardial ischemia in patients with infective endocarditis include coronary compression secondary to periannular aortic valve complications, CEm, obstruction of the coronary ostium due to large vegetation, coronary atherosclerosis, and severe aortic insufficiency [27]. The important difference is that in this case, thrombolysis should be avoided (high hemorrhagic risk), and the treatment approach should focus on i.v. antibiotics, surgical replacement of the infected valve, and future prevention of CEm by eliminating the source of embolization [25].
Acute Dissection of the Coronary Artery or Aorta
Spontaneous coronary artery dissection (SpCADis) is another cause of ACS with NONRUPLA, especially in young women, and it is diagnosed in up to 4% of ACS and 43% of pregnancy-related myocardial infarction. The dissection can occur anywhere of the intima, media, or adventitia of the artery wall by two mechanisms, intima tear or medial hemorrhage. There are a variety of causes such as fibromuscular dysplasia (coronary tortuosity, dilation/ectasia, stenoses), pregnancy (progesterone and estrogen can weaken arterial wall and create a prothrombotic state, hemodynamic changes during pregnancy can increase shear stress, microstructural changes in the aorta and coronary arteries).
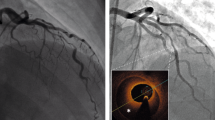
Most commonly, SpCADis presents as STEMI (24–87%), ventricular arrhythmias (3–10%), shock, and death. The challenge is diagnosis by coronary angiography, which is the first-line choice in acute coronary syndrome, but in this case, the layers of the arterial wall suffer and not the lumen itself, so optical coherence tomography (OCT) and intravascular ultrasound (IVUS) are the gold standard techniques.
As far as the management is concerned, SpCADis seems to heal spontaneously, and a conservative approach is preferred, except for patients with unstable symptoms, hemodynamic instability, or left main dissection. Beta-blockers reduce shear stress and arrhythmias and improve long-term survival (as in atherosclerotic ACS). Aspirin seems reasonable to use (low hemorrhage risk). Anticoagulation therapies may resolve the overlying thrombus but should be avoided due to the potential risk of extending the dissection. Patients with SpCADis should be followed frequently for cardiac events [5].
Type A aortic dissection can cause malperfusion and eventually ACS with NONRUPLA most commonly in the elderly (over 65 years) men. The underlying pathogenesis usually is intima tear in segments exposed to the greatest shear stress (right lateral wall in the ascending aorta), and aortic dissection is the result of remodeling of the aortic wall structure as a result of inflammation and extracellular matrix degradation. Accurate and rapid diagnosis and appropriate interventions are needed in the case of acute aortic dissection involving the coronary artery. Contrast-enhanced computed tomography (CT) can detect aortic dissection with high sensitivity, but ECG-gated CT with high spatial and temporal resolution is preferred as there are fewer motion artifacts and so improved diagnostic accuracy. The appropriate treatment is surgical, whereas antiplatelet, anticoagulant, and fibrinolytic therapies should be avoided [6, 7].
Vasospasm and Microvascular Dysfunction
Coronary artery spasm is one of the most common epicardial causes of ACS with NONRUPLA [8, 9]. Coronary artery spasm is a result of coronary vascular smooth muscle hyperactivity (excessive vascular smooth muscle contraction) and endothelial cell dysfunction (lack of vasorelaxant agents) [10]. Interestingly, focal and diffuse vasospasms have different pathophysiologies. In the first case, vasospasm is likely related to localized epithelial dysfunction of epicardial coronaries and local atherosclerotic lesion, whereas diffuse vasospasm is more related to coronary microvascular dysfunction. Coronary artery spasm may present as an ACS in 1% of patients, with chest pain at rest and usually from midnight to early morning when vagal tone is highest [8, 10] and is more common in smokers men aged 40–70 (endothelial damage and inflammation due to smoking-induced oxidative stress that eventually leads in the exaggerated contraction of vascular smooth muscle cells) [8]. ECG changes usually develop as ST depression (subendocardial myocardial ischemia) and as ST elevation only when there is a spasm of the main artery; however, they may appear ordinary at the start of coronary artery spasm or in mild coronary artery spasm. In all the other cases, the coronary artery spasm is diagnosed with invasive or noninvasive provocation tests [10]. As far as long-term treatment is concerned, calcium channel blockers and nicorandil are a better option than nitrates (chronic therapy has more side effects, increased cardiac events, tolerance, increased sensitivity to vasoconstrictors). Long-term prognosis of patients with coronary microvascular spasm seems to be beneficial at least regarding mortality; however, angina persists in about one-third of patients in spite of treatment with calcium channel blockers [11].
Varying degrees of disruption (structural, functional, and extravascular) of the normal coronary physiology end up in coronary microvascular dysfunction (CMD) [12, 13]. More commonly, CMD appears in women (there is an association between hormone therapy and shorter menopausal duration with CMD), presenting with symptoms of ischemia but normal coronary arteries in angiography [14]. Typically, CMD is classified into four categories (with or without epicardial CAD, myocardial disease, and iatrogenic). There are many invasive and noninvasive diagnostic tools (i.e., coronary blood flow measurement, coronary flow reserve, cardiac magnetic resonance imaging (MRI), and positron emission tomography) that unfortunately cannot visualize directly the microcirculation but they can quantify myocardial blood flow and indicate necrosis [13, 15]. As shown by Camici in lab tests, anti-hypertensive treatment on CMD not only affects hyperemic coronary blood flow but also reverse arteriolar remodeling, as all the anti-hypertensive drugs, especially perindopril and candesartan, reduce the medial thickness and interstitial fibrosis.
Imbalance Between Oxygen Demand and Supply and Other Mechanisms
Myocardial infarction resulting from the imbalance between oxygen supply (hypoxemia, anemia, hypotension) and demand (tachycardia, tachyarrhythmias, hypertension) is referred to as type 2 myocardial infarction (T2MI) in the new definition of myocardial infarction and is well known. Patients with T2MI are older non-smokers women with atypical presentation (dyspnea, arrhythmia), with comorbidities such as diabetes, chronic kidney disease, hypertension, and heart failure, usually diagnosed as non-STE-ACS. The trigger is mostly operative stress, sepsis, arrhythmias (tachyarrhythmias, atrial fibrillation), heart failure, or anemia. Because of a lack of evidence-based treatment guidelines, the correction of the underlying cause is the main treatment target. Traditional cardiovascular treatment is questionable, although patients with T2MI are commonly prescribed conventional therapies (β-blockers, angiotensin-converting enzyme inhibitors, statins warfarin, etc.). As far as the outcome, in-hospital and 30-day death rates are three times higher (compared with T1MI). The same is also true for 1-year mortality. Therefore, it is very important to clarify the diagnostic criteria and to establish evidence-based management options of T2MI [16, 17••, 18, 19].
Takotsubo: a Myocardial Infarction Mimic
Takotsubo syndrome (TS) represents a microvascular cause of NONRUPLA acute episodes. Its prevalence is reported to range between 1.2 and 2.2% of all ACS [20]. Post-menopausal females with a history of physical or emotional stress tend to present TS more often. Its pathophysiology remains still unclear although several pathogenetic mechanisms have been proposed, such as multi-vessel epicardial spasm, catecholamine-induced myocardial stunning, spontaneous coronary thrombus lysis, and acute microvascular spasm. Galiuto L. et al. [28] showed in 2010 that irrespective of its etiology, reversible coronary microvascular dysfunction is a common pathophysiological determinant of TS. Indeed, the extent of myocardial hypoperfusion at myocardial contrast echocardiography was similar in patients suffering from TS and in patients suffering from ST elevation MI, whereas a transient significant improvement of myocardial perfusion and of LV function during adenosine infusion was observed in the former only. Electrocardiographic (ECG) abnormalities in TS are most often observed in the acute or sub-acute phase and include ST segment elevation and T-wave inversion [21].
However, Shimizu et al. [22] report three “patterns” of TS: “reverse Takotsubo” with basal akinesia and apical hyperkinesia, “mid-ventricular type” with medio-ventricular ballooning and basal and apical hyperkinesia, “localized type” with ballooning of a limited number of myocardial regions.
Left ventriculography after documentation of MINOCA allows the diagnosis of TS. Cardiac MRI with contrast shows the typical left ventricle dysfunction without detectable myocardial necrosis after gadolinium administration [29].
In TS, left ventricle dysfunction may require treatment with β-blockers, angiotensin-converting enzyme inhibitors, and diuretics, sometimes combined with anticoagulant therapy in patients at risk of ventricular mural thrombus [20, 21].
MINOCA
Myocardial infarction with no obstructive coronary arteries (MINOCA) is a syndrome with variant causes divided into three major mechanisms: epicardial (coronary spasm, plaque disruption, coronary dissection), microvascular (microvascular dysfunction, thrombosis/emboli, myocardial disorders (myocarditis), Takotsubo syndrome), and noncardiac causes (pulmonary embolism, etc.)
MINOCA occurs in 10% of all myocardial infarctions with no obstructive coronary arteries and presents more often in women and has a higher adjusted risk of mortality in 1 year (4.7%) compared with obstructive coronary syndromes. Despite the fact that coronary arteries are normal (or seem normal), one of four patients will continue to experience angina 1 year after the first episode [23].
In MINOCA, it is especially important to clarify the underlying mechanism in order to achieve the best treatment strategy. Cardiac MRI is the preferred diagnostic modality, as it identifies 87% of the underlying cause. Additionally, diagnostic tests such as provocative spasm testing and intravascular ultrasound can be used to clarify the cause.
Conventional postinfarct therapies with statins, angiotensin-converting enzyme inhibitors, β-blockers, etc. seem to reduce the hazard ratio of major adverse cardiovascular events; in opposite, dual antiplatelet therapy tends to increase bleeding rate [30,31,32].
Cardiac MRI is the key diagnostic tool to be employed in MINOCA patients because in addition to providing confirmation of the diagnosis of myocardial infarction with no obstructive coronary arteries, it also provides insights into the differential diagnosis of MINOCA. Late gadolinium enhancement (LGE) can assist the localization of the area of myocardial damage [33]. The presence and pattern of any LGE may point towards a vascular or non-vascular cause. However, there is a subgroup of MINOCA patients that have no evidence of LGE, myocardial edema, or wall motion abnormalities on cardiac magnetic resonance [29, 34]. LGE on cardiac MRI is able to detect as little as 1 g of infarcted myocardium with current techniques [35, 36]. Thus, some patients with normal cardiac magnetic resonance may have too little myonecrosis to be detected. It may also be possible that necrotic myocytes may be distributed over a larger area, and thus not amenable to detection by LGE imaging (Table 2).
Conclusion
In conclusion, many possible mechanisms can provoke acute coronary syndrome with no obstructive plaque (NONRUPLA). Despite the fact that the clinical presentation is similar to that of myocardial infarction with coronary atherosclerosis, patients with NONRUPLA have lower baseline cardiovascular risk compared with obstructive ACS and the lower mortality rate on the first 6 months of the episode that does not persist after a year. As shown in long-term follow-up, patients with NONRUPLA have the same mortality rate as patients with obstructive ACS emphasizing the need for rapid application of the best-known therapy and further research on the underlying mechanisms and the therapeutic approaches of NONRUPLA.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Pasupathy S, et al. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries. Circulation. 2015;131(10):861–70.
Guner A, et al. ST segment elevation myocardial infarction possibly caused by thromboembolism from left atrial appendage thrombus after incomplete surgical ligation. Echocardiography. 2018;35(11):1889–92.
Charles RG, Epstein EJ. Diagnosis of coronary embolism: a review. J R Soc Med. 1983;76(10):863–9.
Charles RG, et al. Coronary embolism in valvular heart disease. Q J Med. 1982;51(202):147–61.
Saw J, Mancini GBJ, Humphries KH. Contemporary review on spontaneous coronary artery dissection. J Am Coll Cardiol. 2016;68(3):297–312.
Gawinecka J, Schonrath F, von Eckardstein A. Acute aortic dissection: pathogenesis, risk factors and diagnosis. Swiss Med Wkly. 2017;147:w14489.
Ichihashi T, et al. Acute myocardial infarction due to spontaneous, localized, acute dissection of the sinus of Valsalva detected by intravascular ultrasound and electrocardiogram-gated computed tomography. Heart Vessel. 2016;31(9):1570–3.
Kim JB, et al. Clinical characteristics and outcomes of patients with coronary artery spasm who initially presented with acute myocardial infarction. Coron Artery Dis. 2018;29(1):60–7.
Pristipino C, et al. Major racial differences in coronary constrictor response between japanese and caucasians with recent myocardial infarction. Circulation. 2000;101(10):1102–8.
Zaya M, Mehta PK, Merz CN. Provocative testing for coronary reactivity and spasm. J Am Coll Cardiol. 2014;63(2):103–9.
Masumoto A, Mohri M, Takeshita A. Three-year follow-up of the Japanese patients with microvascular angina attributable to coronary microvascular spasm. Int J Cardiol. 2001;81(2–3):151–6.
Camici PG, d’Amati G, Rimoldi O. Coronary microvascular dysfunction: mechanisms and functional assessment. Nat Rev Cardiol. 2015;12(1):48–62.
Shome JS, et al., Current perspectives in coronary microvascular dysfunction. Microcirculation, 2017. 24(1).
Lanza GA, Crea F. Primary coronary microvascular dysfunction: clinical presentation, pathophysiology, and management. Circulation. 2010;121(21):2317–25.
Hermens JA, et al. Evidence of myocardial scarring and microvascular obstruction on cardiac magnetic resonance imaging in a series of patients presenting with myocardial infarction without obstructed coronary arteries. Int J Card Imaging. 2014;30(6):1097–103.
Gupta S, et al. Type 2 versus type 1 myocardial infarction: a comparison of clinical characteristics and outcomes with a meta-analysis of observational studies. Cardiovasc Diagn Ther. 2017;7(4):348–58.
•• Lambrakis K, et al. The appropriateness of coronary investigation in myocardial injury and type 2 myocardial infarction (ACT-2): a randomized trial design. Am Heart J. 2019;208:11–20 In this randomized multicenter trial, the clinical and economic impact of early invasive management with coronary angiography in T2MI in terms of all-cause mortality and cost-effectiveness has been evaluated.
McCarthy CP, Januzzi JL Jr, Gaggin HK. Type 2 myocardial infarction- an evolving entity. Circ J. 2018;82(2):309–15.
Mihatov N, Januzzi JL Jr, Gaggin HK. Type 2 myocardial infarction due to supply-demand mismatch. Trends Cardiovasc Med. 2017;27(6):408–17.
Roshanzamir S, Showkathali R. Takotsubo cardiomyopathy a short review. Curr Cardiol Rev. 2013;9(3):191–6.
Cacciotti L, et al. Observational study on Takotsubo-like cardiomyopathy: clinical features, diagnosis, prognosis and follow-up. BMJ Open. 2012;2(5):e001165.
Shimizu M, et al. Recurrent episodes of takotsubo-like transient left ventricular ballooning occurring in different regions: a case report. J Cardiol. 2006;48(2):101–7.
Safdar B, et al. Presentation, clinical profile, and prognosis of young patients with myocardial infarction with nonobstructive coronary arteries (MINOCA): results from the VIRGO Study. J Am Heart Assoc. 2018;7(13):e009174.
Prizel KR, Hutchins GM, Bulkley BH. Coronary artery embolism and myocardial infarction. Ann Intern Med. 1978;88(2):155–61.
Roxas CJ, Weekes AJ. Acute myocardial infarction caused by coronary embolism from infective endocarditis. J Emerg Med. 2011;40(5):509–14.
Roux V, et al. Coronary events complicating infective endocarditis. Heart. 2017;103(23):1906–10.
Harinstein ME, Marroquin OC. External coronary artery compression due to prosthetic valve bacterial endocarditis. Catheter Cardiovasc Interv. 2014;83(3):E168–70.
Galiuto L, et al. Reversible coronary microvascular dysfunction: a common pathogenetic mechanism in apical ballooning or Tako-Tsubo syndrome. Eur Heart J. 2010;31(11):1319–27.
Collste O, et al. Myocardial infarction with normal coronary arteries is common and associated with normal findings on cardiovascular magnetic resonance imaging: results from the Stockholm Myocardial Infarction with Normal Coronaries study. J Intern Med. 2013;273(2):189–96.
Gu XH, et al. Association between depression and outcomes in Chinese patients with myocardial infarction and nonobstructive coronary arteries. J Am Heart Assoc. 2019;8(5):e011180.
Montone RA, Russo M, Niccoli G. MINOCA: current perspectives. Aging (Albany NY). 2018;10(11):3044–5.
•• Pasupathy S, Tavella R, Beltrame JF. Myocardial infarction with nonobstructive coronary arteries (MINOCA): the past, present, and future management. Circulation. 2017;135(16):1490–3 This article represents a major step forward in MINOCA and thereby warrants taking stock of the past, present, and future management strategies of this intriguing condition.
Agewall S, et al. ESC working group position paper on myocardial infarction with non-obstructive coronary arteries. Eur Heart J. 2017;38(3):143–53.
Gerbaud E, et al. Cardiac magnetic resonance imaging for the diagnosis of patients presenting with chest pain, raised troponin, and unobstructed coronary arteries. Int J Card Imaging. 2012;28(4):783–94.
Laraudogoitia Zaldumbide E, et al. The value of cardiac magnetic resonance in patients with acute coronary syndrome and normal coronary arteries. Rev Esp Cardiol. 2009;62(9):976–83.
Saba L, Fellini F, De Filippo M. Diagnostic value of contrast-enhanced cardiac magnetic resonance in patients with acute coronary syndrome with normal coronary arteries. Jpn J Radiol. 2015;33(7):410–7.
Author information
Authors and Affiliations
Contributions
Dr. Oikonomou, Prof. Siasos, and Prof. Tousoulis have reviewed the article; all the other authors have drafted the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
No potential conflicts of interest. No financial support.
Dr. Leopoulou has nothing to disclose.
Dr. Mistakidi has nothing to disclose.
Dr. Oikonomou has nothing to disclose.
Dr. Latsios has nothing to disclose.
Dr. Papaioannou has nothing to disclose.
Dr. Deftereos has nothing to disclose.
Dr. Siasos has nothing to disclose.
Dr. Antonopoulos has nothing to disclose.
Dr. Charalambous has nothing to disclose.
Dr. Tousoulis has nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Vascular Biology
Rights and permissions
About this article
Cite this article
Leopoulou, M., Mistakidi, V.C., Oikonomou, E. et al. Acute Coronary Syndrome with Non-ruptured Plaques (NONRUPLA): Novel Ideas and Perspectives. Curr Atheroscler Rep 22, 21 (2020). https://doi.org/10.1007/s11883-020-00839-7
Published:
DOI: https://doi.org/10.1007/s11883-020-00839-7