Abstract
High-density lipoprotein cholesterol (HDL-C) levels are inversely related to risk of atherosclerotic cardiovascular disease (ASCVD). However, the simplistic assumption that HDL-C levels directly and causally impact atherogenesis has been challenged in recent years. The purpose of this article is to review the current state of knowledge regarding genetically determined HDL-C levels and ASCVD risk and determine what insight these studies provide into the causal relationship between HDL and atherosclerosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epidemiological studies over the past six decades have established an inverse relationship between plasma levels of high-density lipoprotein cholesterol (HDL-C) and the risk of atherosclerotic cardiovascular disease (ASCVD) [1, 2]. A large body of experimental data has established a number of anti-atherosclerotic properties of HDL particles [3, 4], fuelling interest in the concept of HDL-based therapeutics to prevent or reverse ASCVD. However, the “HDL hypothesis” [5] has fallen on hard times over the past several years [6], and uncertainty has developed surrounding the causal role of HDL in atherosclerosis. Several lines of evidence have conspired to cast doubt on a causal role of HDL in atherogenesis [6], including the failure of clinical trials of drugs aimed at raising HDL-C levels [7–12] and Mendelian randomization studies that have brought into question whether genetically determined changes in HDL-C levels impact ASCVD risk [13–15].
Human genetics has been one of the major sources of our knowledge of HDL metabolism and function [16]. The purpose of this review is to summarize what has been learned from human genetic studies regarding a causal role for HDL in atherosclerosis.
Mendelian Disorders of HDL
Pathogenic mutations in three genes, namely ABCA1, APOA1, and LCAT, cause rare Mendelian disorders of low HDL-C [16, 17]. Each of these is characterized by near absence of HDL in blood and in theory should serve as ideal experiments of nature to determine the role of HDL in atherogenesis. However, the rarity of these conditions, as well issues related to selection basis in terms of the patients that come to clinical attention, has made accurate estimation of the risk of ASCVD in these conditions challenging.
Most series of Tangier disease patients have reported an increased prevalence of ASCVD relative to population controls [18–20]. However, it is apparent that Tangier disease does not confer the dramatically elevated risk of premature ASCVD that is seen in Mendelian condition of high LDL-C, such as familial hypercholesterolemia (FH) [21]. There is tremendous inter-individual variability among patients with TD in susceptibility to ASCVD [22], which may relate to differences in the severity of the underlying mutation and the corresponding impairment in cholesterol efflux [23]. Studies of individuals heterozygous for mutations in ABCA1 have generally reported increased prevalence of clinical [24, 25] or subclinical ASCVD [26, 27]. Certain variants in ABCA1 also impact ASCVD risk in the general population [28], though somewhat paradoxically, this effect appears to be independent of HDL-C levels.
Early studies of APOA1 deficiency suggested that these patients develop premature ASCVD [29, 30]. In general, the risk of ASCVD in APOA1 deficiency is thought to be higher than in Tangier disease or familial LCAT deficiency [20]. One reason for this difference may be that plasma LDL-C levels, which are reduced in Tangier disease, are relatively normal in APOA1 deficiency. Combined mutations in ABCA1 and APOA1 have been reported to be associated with premature ASCVD in very rare cases [22].
While data are conflicting, the bulk of evidence appears to suggest that familial LCAT deficiency does not increase the risk of ASCVD [20, 31–33]. Imaging studies have also reported conflicting result regarding subclinical atherosclerosis in heterozygous carriers of LCAT mutations [34–36].
Genome-Wide Association Studies and Mendelian Randomization
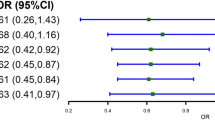
Genome-wide association studies (GWAS) have identified 71 loci associated with HDL-C levels [37]. Of these, 46 loci are associated with HDL-C without statistically significant associations with other lipid parameters. In addition to their role in identifying genetic variants that are associated with plasma lipids and risk for ASCVD, human genetic studies also provide an opportunity to infer the causal relationship between an exposure (genetically determined HDL-C levels) and outcome (ASCVD risk). Such Mendelian randomization studies have consistently reported that genetic risk scores constructed from variants that associate with HDL-C levels from GWAS, or individual variants that associate with HDL-C levels, do not impact ASCVD risk [13–15, 38, 39, 40•, 41, 42]. Collectively, these studies provide one of the strongest arguments against a causal role for HDL-C in atherosclerosis.
While these studies provide strong evidence that genetically determined elevations in HDL-C do not impact ASCVD risk, there are a number of caveats. Firstly, the magnitude of change in HDL-C conferred by these genetic variants are often very small, typically in the range of 0.01–0.1 mmol/L (0.38–3.8 mg/dL). Whether such small changes in HDL-C are enough to modify risk in an individual patient is uncertain. Secondly, the use of genetic risk scores is problematic in that the biological function of most of the variants included is unknown. As a result, predicting what effect these genetic variants may have on ASCVD risk is challenging. This is critical because the complexity of HDL metabolism means that not every variant that raises plasma HDL-C levels can be assumed to reduce ASCVD risk. This is highlighted by the fact that the genetic risk score used in one of the seminal Mendelian randomization studies included a variant in SCARB1 [13], which raises HDL-C but based on its biological function would be expected to increase ASCVD risk (see below). If these genetic risk scores include a combination of variants with varying effects on ASCVD risk (increase, decrease or no effect), it could explain why the genetic risk score as a whole does not appear to modulate ASCVD risk.
One exception to this relates to the cholesterol ester transfer protein (CETP) gene. A number of Mendelian randomization studies have used variants in the CETP gene that associate with increased HDL-C as an instrument to determine the impact of high HDL-C on ASCVD risk [43, 44]. These studies consistently report a reduction in ASCVD risk in patients with genetically reduced CETP activity and increased HDL-C. However, in addition to raising HDL-C levels, these genetic variants also reduce LDL-C, TG, and non-HDL-C. Whether the reduction in ASCVD risk is due to the increased HDL-C, decreased non-HDL-C, or a combination of both is unknown.
Rare Variant Association Studies
The availability of very large cohorts of patients that have been genotyped or sequenced has created new opportunities to investigate the impact of rare genetic variants that influence HDL metabolism on atherosclerosis. This approach was powerfully demonstrated in a recent study of the scavenger receptor B1, SCARB1, gene [45••]. Pioneering studies in mice had established that SCARB1 plays a key role in HDL metabolism and functions as a hepatic HDL-C receptor [46, 47]. Despite having elevated HDL-C, mice with deletion of Scarb1 have increased atherosclerosis [48, 49]. Mechanistically, this is explained by impaired reverse cholesterol transport in these mice due to reduced hepatic HDL-C uptake [50].
Until recently, the extent to which these observations could be extrapolated to humans was unknown. In 2011, the first humans with heterozygous mutations in SCARB1 were described [51, 52]. These patients have elevated HDL-C, exactly as predicted from studies in mice. However, the number of patients with these rare mutations was too small to assess the risk of ASCVD. In 2016, Zanoni et al. described a patient homozygous for a rare variant in SCARB1 (p.P376L) which resulted in loss-of-function of the encoded protein [45••]. This patient had significantly elevated HDL-C levels and evidence of subclinical atherosclerosis. Leveraging the availability of large case–control cohorts of patients with ASCVD, the authors then investigated the role of p.376 L in ASCVD risk in ∼137,000 individuals. They found that p.376 L conferred an increased risk for coronary heart disease with an odds ratio of 1.79, P = 0.018 [45••], providing clear evidence that this rare genetic variant in a hepatic HDL receptor leads to elevated HDL-C and increased risk of ASCVD.
While it is possible that SCARB1 may impact ASVCD risk independently of its effect on HDL metabolism, this study provides one of the most compelling examples of human genetic variation in an HDL-related gene that impacts susceptibility to ASCVD. Unexpectedly (although presaged by studies in mice [46, 47]), this variant causes increased HDL-C and increased ASCVD, which would seem to be in contrast with the inverse epidemiological relationship between HDL-C levels and ASCVD risk. This example therefore establishes the crucial importance of what impact a genetic variant has on flux through the HDL pathway rather than simply the HDL-C level, and cautions against simplistic interpretations between the HDL-C level and ASCVD risk. This study also demonstrates the tremendous opportunity offered by large cohorts of genotyped cases and controls for identifying rare genetic variants that affect ASCVD in humans.
Rare variants in APOA1 also appear to impact ASCVD risk. A large re-sequencing study of APOA1 reported an increased risk for myocardial infarction in (HR 1.7) among individuals with non-synonymous variants in this gene [53]. A rare variant study of ∼33,000 ASCVD cases and 236,000 controls identified five genetic variants that were associated with lipid levels and coronary artery disease [40•]. One of these was a novel missense variant, p.V43L, in APOA1 with an allele frequency of 0.7 %. This variant was associated with a 0.17 mmol/L (6.5 mg/dL) increase in HDL-C levels and a 26 % reduction in risk for coronary artery disease. These data are consistent with the concept that p.V43L is a gain-of-function variant in APOA1 that raises HDL and reduces risk for ASCVD. While this variant was also associated with both triglycerides and non-HDL-C levels [40•], the strongest association with blood lipids was with HDL-C, and the known biological role of apolipoprotein A-I as the principal apolipoprotein of HDL supports that its effect on ASCVD is via its role in HDL metabolism. Additional studies will be needed to confirm this association and determine the mechanism by which this variant raises HDL-C levels.
Making Sense of HDL and ASCVD Risk
How can we reconcile the seemingly disparate findings from human genetic studies regarding HDL and atherosclerosis? Certain Mendelian disorders of HDL appear to impact ASCVD risk (APOA1 deficiency and Tangier disease), whereas others seemingly do not (familial LCAT deficiency). Mendelian randomization studies consistently show no impact of genetically determined changes in HDL-C levels on ASCVD risk. Rare variant studies have identified specific mutations that impact key proteins in HDL biology and do modulate ASCVD risk.
One important factor in interpreting these results is the interactions between different lipoprotein classes as part of normal lipid physiology and the pleiotropic effects of genetic variants on lipid levels. For example, most loss-of-function mutations in ABCA1 result in not only low HDL-C but also low LDL-C, and indeed, patients with Tangier disease typically have a ∼40 % reduction in LDL-C levels [54]. These changes in lipid levels would be predicted to have conflicting results on ASCVD risk, which may partially explain the less-than-anticipated increase in ASCVD rates in patients with Tangier disease. Mendelian randomization studies have attempted to address this by focusing on genetic variation for which there is statistically significant associations with HDL-C levels and not other lipid levels [13, 38]. However, in so doing, these studies typically use genetic variants in genes for which the functional role in lipid metabolism is unknown. Consequently, predicting how they might impact ASCVD risk is problematic.
A critical theme to emerge from these studies is that the level of HDL-C may be considerably less important than the mechanism by which that HDL-C level was achieved. This concept explains why some genetic variants that impact HDL-C do influence ASCVD risk [40•] whereas others do not [13]. The primacy of mechanism over static HDL-C level is perhaps most clearly demonstrated by loss-of-function variants in SCARB1 that raise HDL-C and increase ASCVD risk [45••]. Whereas a simplistic interpretation based on observational epidemiology is that raised HDL-C should lower ASCVD risk, a deeper understanding of the role of SCARB1 in HDL biology, based on a large body of work in animal and cellular models, predicts that blocking a critical step in hepatic HDL uptake and thereby impairing flux through the reverse cholesterol transport pathway would be expected to increase ASCVD risk. The implications for drug development are that attention should be focused on pharmacological targets predicted to increase flux through the HDL pathway, rather than on those that simply raise HDL-C levels.
A limitation in the field remains our inability to accurately measure HDL function or flux and the inadequacy of HDL-C levels as a metric of atheroprotection. Improved biomarkers of HDL functionality, such as efflux potential [55, 56], may help provide additional insight into the function of specific genetic variants on HDL function. Rare variant studies in large cohorts of patients, such as those performed for variants in SCARB1 [45••] and APOA1 [40•], provide an outstanding opportunity to investigate the impact of pathogenic variants in genes that impact HDL through established mechanisms. Such studies may well yield additional examples of genetic variants that influence HDL-C and ASCVD risk.
Conclusions
Human genetics provides a complex and, at times, discordant picture of the relationship between HDL and atherosclerosis. Although many outstanding questions remain, recent developments have helped to fill in some of the gaps and allow a more complete picture to emerge. While genetically determined alterations in HDL-C levels do not appear to influence ASCVD risk as a whole, specific genetic mechanisms that impact key steps in HDL metabolism do modulate ASCVD risk in ways that are predictable based on an understanding of HDL biology. Sufficient examples from human genetics now exist whereby alterations in HDL-C levels are associated with changes in ASCVD risk to support the body of evidence from epidemiology and preclinical studies that HDL is a causal factor in atherogenesis. What is clear is that the relationship between HDL and atherosclerosis is complex, intriguing, and that the final chapter has not yet been written.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Barr DP, Russ EM, Eder HA. Protein-lipid relationships in human plasma. II. In atherosclerosis and related conditions. Am J Med. 1951;11(4):480–93.
Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am J Med. 1977;62(5):707–14.
Nicholls SJ, Tuzcu EM, Sipahi I, Schoenhagen P, Crowe T, Kapadia S, et al. Relationship between atheroma regression and change in lumen size after infusion of apolipoprotein A-I Milano. J Am Coll Cardiol. 2006;47(5):992–7. doi:10.1016/j.jacc.2005.11.040.
Plump AS, Scott CJ, Breslow JL. Human apolipoprotein A-I gene expression increases high density lipoprotein and suppresses atherosclerosis in the apolipoprotein E-deficient mouse. Proc Natl Acad Sci U S A. 1994;91(20):9607–11.
Miller GJ, Miller NE. Plasma-high-density-lipoprotein concentration and development of ischaemic heart-disease. Lancet. 1975;1(7897):16–9.
Ng DS, Wong NC, Hegele RA. HDL—is it too big to fail? Nat Rev Endocrinol. 2013;9(5):308–12. doi:10.1038/nrendo.2012.238.
Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M, et al. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007;357(21):2109–22. doi:10.1056/NEJMoa0706628.
Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J, et al. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med. 2012;367(22):2089–99. doi:10.1056/NEJMoa1206797.
Boden WE, Probstfield JL, Anderson T, Chaitman BR, Desvignes-Nickens P, Koprowicz K, et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011;365(24):2255–67. doi:10.1056/NEJMoa1107579.
HPS2-THRIVE randomized placebo-controlled trial in 25 673 high-risk patients of ER niacin/laropiprant: trial design, pre-specified muscle and liver outcomes, and reasons for stopping study treatment. Eur Heart J. 2013;34(17):1279–91. doi:10.1093/eurheartj/eht055.
Group HTC, Landray MJ, Haynes R, Hopewell JC, Parish S, Aung T, et al. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med. 2014;371(3):203–12. doi:10.1056/NEJMoa1300955.
Keene D, Price C, Shun-Shin MJ, Francis DP. Effect on cardiovascular risk of high density lipoprotein targeted drug treatments niacin, fibrates, and CETP inhibitors: meta-analysis of randomised controlled trials including 117 411 patients. BMJ. 2014;349:g4379. doi:10.1136/bmj.g4379.
Voight BF, Peloso GM, Orho-Melander M, Frikke-Schmidt R, Barbalic M, Jensen MK, et al. Plasma HDL cholesterol and risk of myocardial infarction: a mendelian randomisation study. Lancet. 2012;380(9841):572–80. doi:10.1016/S0140-6736(12)60312-2.
Haase CL, Tybjaerg-Hansen A, Grande P, Frikke-Schmidt R. Genetically elevated apolipoprotein A-I, high-density lipoprotein cholesterol levels, and risk of ischemic heart disease. J Clin Endocrinol Metab. 2010;95(12):E500–10. doi:10.1210/jc.2010-0450.
Haase CL, Tybjaerg-Hansen A, Qayyum AA, Schou J, Nordestgaard BG, Frikke-Schmidt R. LCAT, HDL cholesterol and ischemic cardiovascular disease: a Mendelian randomization study of HDL cholesterol in 54,500 individuals. J Clin Endocrinol Metab. 2012;97(2):E248–56. doi:10.1210/jc.2011-1846.
Brunham LR, Hayden MR. Human genetics of HDL: insight into particle metabolism and function. Prog Lipid Res. 2015;58:14–25. doi:10.1016/j.plipres.2015.01.001.
McKusick VA. Mendelian inheritance in man and its online version, OMIM. Am J Hum Genet. 2007;80(4):588–604. doi:10.1086/514346.
Schaefer EJ, Zech LA, Schwartz DE, Brewer Jr HB. Coronary heart disease prevalence and other clinical features in familial high-density lipoprotein deficiency (Tangier disease). Ann Intern Med. 1980;93(2):261–6.
Serfaty-Lacrosniere C, Civeira F, Lanzberg A, Isaia P, Berg J, Janus ED, et al. Homozygous Tangier disease and cardiovascular disease. Atherosclerosis. 1994;107(1):85–98.
Santos RD, Asztalos BF, Martinez LR, Miname MH, Polisecki E, Schaefer EJ. Clinical presentation, laboratory values, and coronary heart disease risk in marked high-density lipoprotein-deficiency states. J Clin Lipidol. 2008;2(4):237–47. doi:10.1016/j.jacl.2008.06.002.
Nordestgaard BG, Chapman MJ, Humphries SE, Ginsberg HN, Masana L, Descamps OS, et al. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European Atherosclerosis Society. Eur Heart J. 2013;34(45):3478–90a. doi:10.1093/eurheartj/eht273.
Hovingh GK, Kuivenhoven JA, Bisoendial RJ, Groen AK, van Dam M, van Tol A, et al. HDL deficiency and atherosclerosis: lessons from Tangier disease. J Intern Med. 2004;255(2):299–301.
Singaraja RR, Brunham LR, Visscher H, Kastelein JJ, Hayden MR. Efflux and atherosclerosis: the clinical and biochemical impact of variations in the ABCA1 gene. Arterioscler Thromb Vasc Biol. 2003;23(8):1322–32. doi:10.1161/01.ATV.0000078520.89539.77.
Clee SM, Kastelein JJ, van Dam M, Marcil M, Roomp K, Zwarts KY, et al. Age and residual cholesterol efflux affect HDL cholesterol levels and coronary artery disease in ABCA1 heterozygotes. J Clin Invest. 2000;106(10):1263–70. doi:10.1172/JCI10727.
Frikke-Schmidt R, Nordestgaard BG, Schnohr P, Steffensen R, Tybjaerg-Hansen A. Mutation in ABCA1 predicted risk of ischemic heart disease in the Copenhagen City Heart Study Population. J Am Coll Cardiol. 2005;46(8):1516–20. doi:10.1016/j.jacc.2005.06.066.
van Dam MJ, de Groot E, Clee SM, Hovingh GK, Roelants R, Brooks-Wilson A, et al. Association between increased arterial-wall thickness and impairment in ABCA1-driven cholesterol efflux: an observational study. Lancet. 2002;359(9300):37–42. doi:10.1016/S0140-6736(02)07277-X.
Bochem AE, van Wijk DF, Holleboom AG, Duivenvoorden R, Motazacker MM, Dallinga-Thie GM, et al. ABCA1 mutation carriers with low high-density lipoprotein cholesterol are characterized by a larger atherosclerotic burden. Eur Heart J. 2013;34(4):286–91. doi:10.1093/eurheartj/ehs376.
Frikke-Schmidt R, Nordestgaard BG, Jensen GB, Steffensen R, Tybjaerg-Hansen A. Genetic variation in ABCA1 predicts ischemic heart disease in the general population. Arterioscler Thromb Vasc Biol. 2008;28(1):180–6. doi:10.1161/ATVBAHA.107.153858.
Norum RA, Lakier JB, Goldstein S, Angel A, Goldberg RB, Block WD, et al. Familial deficiency of apolipoproteins A-I and C-III and precocious coronary-artery disease. N Engl J Med. 1982;306(25):1513–9. doi:10.1056/NEJM198206243062503.
Schaefer EJ, Heaton WH, Wetzel MG, Brewer Jr HB. Plasma apolipoprotein A-1 absence associated with a marked reduction of high density lipoproteins and premature coronary artery disease. Arteriosclerosis. 1982;2(1):16–26.
Calabresi L, Simonelli S, Gomaraschi M, Franceschini G. Genetic lecithin:cholesterol acyltransferase deficiency and cardiovascular disease. Atherosclerosis. 2012;222(2):299–306. doi:10.1016/j.atherosclerosis.2011.11.034.
Kunnen S, Van Eck M. Lecithin:cholesterol acyltransferase: old friend or foe in atherosclerosis? J Lipid Res. 2012;53(9):1783–99. doi:10.1194/jlr.R024513.
Carlson LA. Fish eye disease: a new familial condition with massive corneal opacities and dyslipoproteinaemia. Eur J Clin Invest. 1982;12(1):41–53.
Duivenvoorden R, Holleboom AG, van den Bogaard B, Nederveen AJ, de Groot E, Hutten BA, et al. Carriers of lecithin cholesterol acyltransferase gene mutations have accelerated atherogenesis as assessed by carotid 3.0-T magnetic resonance imaging [corrected]. J Am Coll Cardiol. 2011;58(24):2481–7. doi:10.1016/j.jacc.2010.11.092.
Calabresi L, Baldassarre D, Simonelli S, Gomaraschi M, Amato M, Castelnuovo S, et al. Plasma lecithin:cholesterol acyltransferase and carotid intima-media thickness in European individuals at high cardiovascular risk. J Lipid Res. 2011;52(8):1569–74. doi:10.1194/jlr.P014977.
Hovingh GK, Hutten BA, Holleboom AG, Petersen W, Rol P, Stalenhoef A, et al. Compromised LCAT function is associated with increased atherosclerosis. Circulation. 2005;112(6):879–84. doi:10.1161/CIRCULATIONAHA.105.540427.
Global Lipids Genetics C, Willer CJ, Schmidt EM, Sengupta S, Peloso GM, Gustafsson S, et al. Discovery and refinement of loci associated with lipid levels. Nat Genet. 2013;45(11):1274–83. doi:10.1038/ng.2797.
Holmes MV, Asselbergs FW, Palmer TM, Drenos F, Lanktree MB, Nelson CP, et al. Mendelian randomization of blood lipids for coronary heart disease. Eur Heart J. 2015;36(9):539–50. doi:10.1093/eurheartj/eht571.
Johannsen TH, Kamstrup PR, Andersen RV, Jensen GB, Sillesen H, Tybjaerg-Hansen A, et al. Hepatic lipase, genetically elevated high-density lipoprotein, and risk of ischemic cardiovascular disease. J Clin Endocrinol Metab. 2009;94(4):1264–73. doi:10.1210/jc.2008-1342.
• Helgadottir A, Gretarsdottir S, Thorleifsson G, Hjartarson E, Sigurdsson A, Magnusdottir A, et al. Variants with large effects on blood lipids and the role of cholesterol and triglycerides in coronary disease. Nat Genet. 2016;48(6):634–9. doi:10.1038/ng.3561. This study examined the role of rare variants on blood lipids and coronary disease risk in a very large cohort of patients. It identified a rare coding variant in APOA1 that raises HDL-C and reduced risk of coronary disease by 26%.
Frikke-Schmidt R, Nordestgaard BG, Stene MC, Sethi AA, Remaley AT, Schnohr P, et al. Association of loss-of-function mutations in the ABCA1 gene with high-density lipoprotein cholesterol levels and risk of ischemic heart disease. JAMA. 2008;299(21):2524–32. doi:10.1001/jama.299.21.2524.
Do R, Willer CJ, Schmidt EM, Sengupta S, Gao C, Peloso GM, et al. Common variants associated with plasma triglycerides and risk for coronary artery disease. Nat Genet. 2013;45(11):1345–52. doi:10.1038/ng.2795.
Niu W, Qi Y. Circulating cholesteryl ester transfer protein and coronary heart disease: mendelian randomization meta-analysis. Circ Cardiovasc Genet. 2015;8(1):114–21. doi:10.1161/CIRCGENETICS.114.000748.
Johannsen TH, Frikke-Schmidt R, Schou J, Nordestgaard BG, Tybjaerg-Hansen A. Genetic inhibition of CETP, ischemic vascular disease and mortality, and possible adverse effects. J Am Coll Cardiol. 2012;60(20):2041–8. doi:10.1016/j.jacc.2012.07.045.
•• Zanoni P, Khetarpal SA, Larach DB, Hancock-Cerutti WF, Millar JS, Cuchel M, et al. Rare variant in scavenger receptor BI raises HDL cholesterol and increases risk of coronary heart disease. Science. 2016;351(6278):1166–71. doi:10.1126/science.aad3517. This study leverages the power of large cohorts of genotyped patients and provides one of the most convincing examples of a rare genetic variant in an HDL-related gene that impacts risk of coronary disease. Unexpectedly, this genetic variant increases HDL-C levels and increases risk of coronary disease. This is explained by the fact that this variant impairs hepatic HDL uptake, a key step in reverse cholesterol transport.
Acton S, Rigotti A, Landschulz KT, Xu S, Hobbs HH, Krieger M. Identification of scavenger receptor SR-BI as a high density lipoprotein receptor. Science. 1996;271(5248):518–20.
Rigotti A, Trigatti BL, Penman M, Rayburn H, Herz J, Krieger M. A targeted mutation in the murine gene encoding the high density lipoprotein (HDL) receptor scavenger receptor class B type I reveals its key role in HDL metabolism. Proc Natl Acad Sci U S A. 1997;94(23):12610–5.
Trigatti B, Rayburn H, Vinals M, Braun A, Miettinen H, Penman M, et al. Influence of the high density lipoprotein receptor SR-BI on reproductive and cardiovascular pathophysiology. Proc Natl Acad Sci U S A. 1999;96(16):9322–7.
Van Eck M, Twisk J, Hoekstra M, Van Rij BT, Van der Lans CA, Bos IS, et al. Differential effects of scavenger receptor BI deficiency on lipid metabolism in cells of the arterial wall and in the liver. J Biol Chem. 2003;278(26):23699–705. doi:10.1074/jbc.M211233200.
Zhang Y, Da Silva JR, Reilly M, Billheimer JT, Rothblat GH, Rader DJ. Hepatic expression of scavenger receptor class B type I (SR-BI) is a positive regulator of macrophage reverse cholesterol transport in vivo. J Clin Invest. 2005;115(10):2870–4. doi:10.1172/JCI25327.
Vergeer M, Korporaal SJ, Franssen R, Meurs I, Out R, Hovingh GK, et al. Genetic variant of the scavenger receptor BI in humans. N Engl J Med. 2011;364(2):136–45. doi:10.1056/NEJMoa0907687.
Brunham LR, Tietjen I, Bochem AE, Singaraja RR, Franchini PL, Radomski C, et al. Novel mutations in scavenger receptor BI associated with high HDL cholesterol in humans. Clin Genet. 2011;79(6):575–81. doi:10.1111/j.1399-0004.2011.01682.x.
Haase CL, Frikke-Schmidt R, Nordestgaard BG, Tybjaerg-Hansen A. Population-based resequencing of APOA1 in 10,330 individuals: spectrum of genetic variation, phenotype, and comparison with extreme phenotype approach. PLoS Genet. 2012;8(11):e1003063. doi:10.1371/journal.pgen.1003063.
Schaefer EJ, Brousseau ME, Diffenderfer MR, Cohn JS, Welty FK, O’Connor Jr J, et al. Cholesterol and apolipoprotein B metabolism in Tangier disease. Atherosclerosis. 2001;159(1):231–6.
Rohatgi A, Khera A, Berry JD, Givens EG, Ayers CR, Wedin KE, et al. HDL cholesterol efflux capacity and incident cardiovascular events. N Engl J Med. 2014. doi:10.1056/NEJMoa1409065.
Khera AV, Cuchel M, de la Llera-Moya M, Rodrigues A, Burke MF, Jafri K, et al. Cholesterol efflux capacity, high-density lipoprotein function, and atherosclerosis. N Engl J Med. 2011;364(2):127–35. doi:10.1056/NEJMoa1001689.
Acknowledgments
LRB is supported by a Heart & Stroke Foundation of Canada National New Investigator Award and is a Canadian Institute of Health Research New Investigator. His laboratory is supported by an Emerging Research Leaders Initiative grant from the Heart & Stroke Foundation of Canada.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Liam R. Brunham declares no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Genetics
Rights and permissions
About this article
Cite this article
Brunham, L.R. HDL as a Causal Factor in Atherosclerosis: Insights from Human Genetics. Curr Atheroscler Rep 18, 71 (2016). https://doi.org/10.1007/s11883-016-0623-0
Published:
DOI: https://doi.org/10.1007/s11883-016-0623-0