Abstract
Obesity and hypertension are growing epidemics in the modern world. Lifestyle changes and medical treatment for obesity have disappointing long-term results and albeit drugs for hypertension are usually very effective, the necessity of multiple pills and frequent side effects make the adherence to treatment a huge challenge for healthcare systems. Bariatric/metabolic surgery is a very effective treatment and an exponential number of studies have been showing its positive impact beyond weight loss, mainly on type 2 diabetes. There is also growing evidence suggesting that bariatric/metabolic surgery is associated with reduced incidence of cardiovascular events, but the impact on hypertension and other components of metabolic syndrome usually derive from trials’ secondary end points. Taking this limitation in mind, bariatric/metabolic surgery action on blood pressure is reaching a significant proportion of hypertension resolution or improvement. In this review, we discussed the current evidence on the impact of bariatric/metabolic surgery on blood pressure control and pointed out perspectives in this research area.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity and its comorbidities are the major health problem of the modern world. There is a close association of obesity with type 2 diabetes (T2D) and insulin resistance, dyslipidemia, hypertension, and even cancer. Most of the comorbidities increase cardiovascular risk and the control of obesity and its consequences are a difficult and costly challenge for governments and their healthcare systems [1].
Weight gain has an important relation to the increased risk of developing hypertension, but not all obese individuals are hypertensive and it is not clear why some of the obese patients have normal blood pressure. It is conceivable that ethnic and genetic factors may play a role in these differences.
The National Health and Nutritional Examination Survey (NHANES) III showed that the prevalence of hypertension among men and women is 15 % at a BMI <25 kg/m2, and at a BMI >30 kg/m2, it is 42 and 38 %, respectively [2].
The Brazilian National Survey of Health 2013 (http://www.ibge.gov.br/home/estatistica/populacao/pns/2013/default.shtm) showed that 21.4 % of Brazilian citizens have hypertension and 1.5 % have already had a stroke, the more severe consequence of high blood pressure (BP).
Another survey from Brazil carried over the telephone, the VIGITEL 2014 (http://www.endocrino.org.br/media/uploads/PDFs/ppt-vigitel-2014-.pdf), showed that 52.5 % of the Brazilian population is overweight and 17.9 % is obese. This data indicates that this country is rapidly becoming one of the most obese countries in the world, and the incidence of hypertension will increase as fast as obesity.
Despite the recognized elevation of BP with aging, the Coronary Artery Risk Development in Young Adults (CARDIA) study pointed out that those who maintained their weight (less than 2 kg/m2 of BMI gain) for 15 years had no significant increase in BP; nevertheless, those who gained more than 2 kg/m2 of BMI had substantial BP increase [3].
Unfortunately, medical treatment of obesity including lifestyle modifications has been very disappointing and, currently, the only effective treatment with better long-term results is bariatric surgery.
Mechanisms of Obesity-Related Hypertension
Despite the existence of direct correlations between weight gain and hypertension, the mechanisms that explain these relationships are not well understood.
The knowledge of these mechanisms can help us to understand how bariatric/metabolic surgery can play an important role for the treatment of morbidly obese hypertensive patients.
Insulin Resistance and Sympathetic Hyperactivity
Insulin resistance is commonly observed in the obese population and its main consequence is hyperinsulinemia.
There is some controversy about the role of insulin in the pathogenesis of hypertension in obese patients, but a number of evidence have demonstrated that the sympathetic nervous system (SNS) can be stimulated by insulin, and consequently, activity can be overexpressed in the presence of hyperinsulinemia [4].
Thus, a direct stimulation of SNS and a direct action on the kidney promoting sodium retention may explain the relationship of insulin and BP.
Leptin
Although high leptin levels are not frequently seen in obese patients, it can have a role for the elevation of BP because it stimulates the SNS like insulin.
Renin-Angiotensin-Aldosterone System
Obesity activates the renin-angiotensin-aldosterone system (RAAS) and the mechanisms that support this elevation include SNS stimulation, angiotensin production by adipocytes, and the effects of free fatty acids on aldosterone production [4].
Sodium Metabolism
Obese patients have low natriuretic peptide levels [5] and a predisposition to reabsorb sodium trough the kidney due to the overstimulation of RAAS. In order to maintain the sodium balance and volume homeostasis, these patients need a higher arterial pressure.
Sleep Apnea
Sleep apnea is a sleep disorder breathing characterized by partial or total upper airway obstructions during sleep promoting reductions in the intrathoracic pressure, intermittent hypoxia, and sleep fragmentation [6]. These factors may contribute to increase blood pressure by inducing sympathetic hyper activation, decreased baroreceptor sensitivity, endothelial dysfunction, and arterial stiffness, among others [7]. The main treatment for sleep apnea—namely, continuous positive airway pressure (CPAP)—is able to improve several pathways involved in hypertension promoting modest but significant blood pressure reduction mainly in patients with resistant hypertension [8].
Adiponectin
Adiponectin is an adipokine that is downregulated by genetic factors and environmental factors as high-fat diet and sedentary lifestyle that increase the risk obesity [9]. A systematic review showed an inverse correlation between BP and levels of adiponectin. It can be considered a biomarker and can have a role in the development of hypertension related to obesity [10].
The Impact of Bariatric/Metabolic Surgery on Hypertension
In 1983, looking for improvement in heart disease risk factors, Gleysteen, presented for the first time, hypertension resolution in 66.6 % (10/15) of his patients after a Roux-en-Y gastric bypass (RYGB) with 12 months of follow up [11].
Walter Pories in 1992 published the first clue that T2D could be a surgical disease, with a provocative title: “Is type II diabetes mellitus a surgical Disease?”, leading to an exponential growth of evidences indicating the beneficial effects of bariatric surgery over T2D, and the so-called metabolic surgery started to develop. In that article, he referred resolution of diabetes and hypertension in 88 and 68.1 % respectively [12].
Probably, the results in favor of T2D resolution led to preferential interest in it, but not in other conditions that are part of metabolic syndrome, as arterial hypertension.
In order to bring the most important data about blood pressure control with metabolic surgery, this review is based on prospective studies with longer follow-up, randomized trials, and systematic reviews (Table 1). Most of the data about hypertension were derived from secondary endpoints of metabolic surgery in T2D patients within trials that were aimed at glycemic control.
Experimental Evidence
Very few experimental studies have demonstrated the relationship between bariatric surgery and the resolution of hypertension.
The first to point out experimental benefits of sleeve gastrectomy (SG) in the reduction of BP were Rodríguez et al. They studied diet-induced obese Wistar rats (DIO), which have a higher blood pressure than lean Wistar rats. Although they showed a BP decrease in the pair-feeding and caloric restriction rats, SG rats had the lowest blood pressure level which constitutes an evidence of mechanisms beyond weight loss [21].
To investigate how bariatric surgery benefits the cardiovascular system and reduces blood pressure, Zhang et al. did an RYGB surgery in spontaneously hypertensive rats (SHRs) and showed a significant reduction in BP. They demonstrated, through an elegant experiment, an improvement on cardiac and vascular remodeling and dysfunction and confirmed that RYGB significantly inhibited the overdrive of the SNS [22].
Clinical Evidence
As T2D resolution with metabolic surgery is currently the hottest topic in our field, there are a few studies focused specifically in the resolution or amelioration of hypertension.
From our perspective, the outcomes on hypertension after metabolic surgery are very similar to what happens in T2D patients. Very early in the postoperative period, even before weight loss, many patients show a significant decrease in BP. Many patients are discharged from the hospital without medication and some of them will never take them again. Ahmed et al. demonstrated an impressive reduction in hypertensive patients and medication usage as soon as the first postoperative week. “Resolution” was present in 78 % (45/58) of patients and the total number of medications dropped from 71 (58 patients) to 23, a reduction of 68 % [23].
Nonrandomized Trials
The Swedish Obese Subjects (SOS) study, a prospective controlled study with the longest follow-up, showed an association of bariatric surgery and reduced incidence of fatal and total cardiovascular (CV) events. The better outcome of CV events after bariatric surgery had a positive relationship with higher baseline levels of insulin, but not with baseline BMI [24].
A substudy derived from SOS compared the effects of two surgical techniques (RYGB and vertical banded gastroplasty (VBG)/adjustable gastric banding (AGB)) and a non-operated control group over BP and salt intake. RYGB showed a significantly lower systolic and diastolic blood pressure when compared to the other groups. The number of antihypertensive medications was also significantly lower in the RYGB group. The most interesting issue about this study is that restrictive procedures such as VBG/AGB and control group showed a linear association of weight reduction and changes in blood pressure; however, in RYGB, this relation was absent. Other mechanistic factors, as a diuretic and a natriuretic effect, probably increased the effects after RYGB besides weight reduction per se [25].
A prospective study, published by our group, enrolled 66 grade 1 obese T2D patients submitted to RYGB presented 58 % (15 of 26) resolution of hypertension, with a blood pressure below 130/80 mmHg without medications. The median follow-up was 5 years (1–6) [17].
Another prospective study with 6 years of follow-up, which aimed to compare weight loss and cardio metabolic endpoint among three groups of patients (one submitted to RYGB and two control non-operated groups) demonstrated significant improvement of hypertension in the RYGB’s patients. The remission rate was defined as the maintenance of BP below140/90 mmHg without drugs. After 2 and 6 years of follow-up, 53 and 42 % remitted, respectively. Despite the observation of some recurrences in the surgical group, the two control groups achieved only 18 and 9 % remission rates after 6 years. The authors cited the difficulty to retain patients as a potential introduction of bias [16].
The Longitudinal Assessment of Bariatric Surgery (LABS) consortium was formed to acquire long-term data of bariatric procedures performed in USA [26]. LABS-2 studied the incidence and remission rates of comorbidities. It included 1738 patients submitted to RYGB and 610 submitted to AGB with 3 years of follow-up. Hypertension was present in 68.9 % of RYGB and 62.7 % of AGB patients and remission rate at 3 years was 38.2 and 17.4 % for patients submitted to RYGB and AGB, respectively. An interesting observation that was not mentioned by other studies is the incidence of de novo hypertension after the bariatric procedure, which was 12.6 % in RYGB and 18.1 % in AGB [18•].
These nonrandomized trials did not clearly indicate the number of patients who achieved controlled blood pressure with fewer medications than in the baseline. The reduction in the number of medications increases the adherence to treatment that is one of the biggest challenges in the treatment of any chronic diseases.
Differences in remission and incidence between RYGB and AGB in LABS-2 showed that the modification in gastrointestinal anatomy is a key factor for hypertension resolution independent of weight loss.
Biliopancreatic Diversion with Duodenal Switch (BPD-DS) creates the greatest change in gastrointestinal anatomy among bariatric procedures. Although it is a very potent metabolic procedure, it has not been performed in large scale because of its technical complexity and greater incidence of long-term nutritional complications.
Picard Marceau, the surgeon who introduced this technique, published his long-term results with 5 to 20 years of follow-up: 68 % (1789 patients) of his cohort had hypertension. For the long-term analysis, they had data from 1211 patients (67.7 %) and among them, they observed that 64 % discontinued and 31 % decreased medication, which demonstrates that 95 % of the patients had a resolution or amelioration of hypertension. They also concluded that in 915 patients with paired data before and 10 years after surgery, a significant reduction in systolic and diastolic blood pressure was observed [19•].
Randomized Trials
The current evidence about the impact of bariatric surgery on blood pressure derived from randomized trials is scarce. Particularly, no single study was primarily powered to examine the effects of bariatric surgery on blood pressure control.
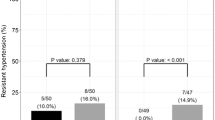
Our group did a randomized trial with super obese patients to compare the impact of long (50/150 cm) versus very long (100/250 cm) RYGB’s limbs over metabolic comorbidities. Patients with blood pressure over 140/90 mmHg were considered hypertensive. Results showed no significant difference between groups in the control of hypertension, but 55 % of all hypertensive patients got the disease controlled without medications in mean follow-up of 48 months (6–56) [20].
The Surgical Therapy and Medications Potentially Eradicate Diabetes Efficiently (STAMPEDE) trial was designed to compare the intensive medical treatment (IMT) with two surgical procedures, RYGB and SG, with the primary goal of improving glycemic control in obese patients. History of hypertension was seen in 60, 70, and 60 % of IMT, RYGB, and SG groups, respectively. Although it was not possible to demonstrate significant differences in terms of BP values between groups, they pointed out a significant reduction in the number of antihypertensive medications, which is the most important indicator to define better control of hypertension.
In the first year, 59 % of patients in the RYGB group and 60 % from the SG group quit antihypertensive medications, which can be considered as the resolution of hypertension. Specifically, about angiotensin-converting enzyme inhibitor (ACE) or angiotensin-receptor blocker (ARB) usage, it decreased from 74 to 18 % in the RYGB group and from 61 to 22 % in the SG group [27].
In the third year of follow-up, they showed a slight increase of the use of ACE or ARB medications, 23.9 and 27.7 % of patients in the RYGB and SG groups, respectively. These results kept the statistical significance compared to IMT arm [28••].
STAMPEDE patients entered the study with controlled blood pressure and this is a critical issue to evaluate results about hypertension modification.
A critical analysis of another randomized trial designed to study T2D patients, published by Mingrone et al., showed patients with uncontrolled BP (over 130 × 85 mmHg) at baseline in all studied groups, conventional medical treatment (CMT), RYGB and BPD.
In the second year of follow-up, they showed a better control of blood pressure in all groups and antihypertensive drugs were reduced or discontinued in 70, 80, and 85 % of patients in the CMT, RYGB and BPD groups, respectively [29]. Data from the CMT group was difficult to analyze because the weight loss in this group was significantly lower than in the surgical groups, and there was no evident reason to have a reduction in medications similar to the surgical arms.
In the fifth year of follow-up, patients of all groups maintained a better controlled blood pressure, but a greater number of patients in the CMT group required medications to control hypertension (73 %) than those in the surgical groups did (58 % in the RYGB group and 32 % in the BPD group). Although BPD patients had better results initially, they also “paid a higher price” because of the increased frequency of multiple nutritional complications [30•].
The Diabetes Surgery study, a multicenter randomized study with 120 patients, compared lifestyle modification with IMT and RYGB. The primary endpoint of the study was to achieve a composite triple endpoint, controlled glycemia, BP, and cholesterol. In the medical management group, 73 % were on antihypertensive treatment and 68 % of those in the surgical group were on treatment.
In the first publication, with 12 months of follow-up, the authors did not observe differences between groups on achieving systolic blood pressure below 130 mmHg (medical treatment 79 % and surgery 84 %). Assuming that hypertension might be easier to control than T2D, the number of medications must be used to prove if there were differences between groups, but there was no mention of that information [31].
In the second paper, with 24 months of follow-up, the number of patients with systolic BP <130 mmHg in the medical management group, decreased from 79 to 69 %, while in the surgical group, 80 % of patients kept the target. Indeed, the most important is that the frequency of patients without antihypertensive medications after 24 months increased from 20 to 52 % in the surgical group and from 14 to 28 % in the medical management group (odds ratio of 3.7, 95 % CI 1.4–9.6) [32••].
The absence of significant reductions in blood pressure cannot be considered a failure of metabolic surgery to control it. Courcoulas et al., in their three-arm randomized trial, compared RYGB, AGB, and lifestyle modification with medical treatment (LS/MT) aiming to evaluate T2D remission. In the first year of follow-up, they did not show significant reductions in BP, but antihypertensive medications were discontinued in 58 % in the GB group, 54 % in the AGB, and only 13 % in the LS/MT. The incidence of hypertension at baseline was 50 % for RYGB arm, 59 % for AGB, and 70 % for LS/MT. After 1 year, it was 38, 32, and 74 %, respectively, reinforcing the impact of surgery on hypertension remission [33].
Their second publication with 3 years of follow-up showed that only RYGB achieved significant improvement in systolic and diastolic blood pressure compared to the other two groups [34].
Halperin et al. achieved a highly significant reduction on the number of antihypertensive medications in their trial that compared RYGB with LS/MT after 12 months of follow-up. The treatment goal to systolic BP <130 mmHg was achieved by 73 % of patients in the RYGB groups and by 52 % in the LS/MT group [35].
All randomized trials until now focused on T2D patients while other components of metabolic syndrome were not present in all studied subjects. Another problem to evaluate hypertension in those trials is what they considered resolution or amelioration and how patients’ BP was at baseline. Ideally, patients should enroll with controlled BP (under 130/85 mmHg) using antihypertensive medications according to the patient’s particular needs. Therefore, the reduction in the number of medications with adequate BP control after the treatment seems to be the best way to evaluate results.
Systematic Reviews
A landmark in bariatric surgery, the systematic review published by Buchwald, showed resolution of hypertension in 61.7 % and improvement in 78.5 % of patients [13].
Since this review, the number of studies has grown exponentially, mainly dedicated to the treatment of uncontrolled T2D. As a consequence, some new systematic reviews have been published. Unfortunately, all of them share the same limitations: loss of follow-up, a very common problem in bariatric surgery; weak studies’ designs, most of them done in a retrospective fashion; a lack of clear definition of resolution or improvement of comorbidities; and finally, a variety of bariatric procedures and multiple technical modifications for the same procedure that could negatively impact on the results.
The only systematic review that focused specifically on hypertension defined resolution as a discontinuation of antihypertensive drugs and improvement as a reduction of them. Fifty-seven studies were included with a total of 51,241 patients. Of these, 54.1 % of the patients had hypertension, 50 % resolved, and 63.7 % improved. For studies with a follow-up greater than 1 year, the odds ratio for a patient with hypertension to get it resolved was 2.29 times greater than the unresolved after a bariatric operation [14••].
A meta-analysis and meta-regression that evaluated the long-term impact (5 years of follow-up) of bariatric surgery on T2D, hypertension, and hyperlipemia showed that the relative risk reduction of hypertension after bariatric surgery was 54 % and it reached a plateau 20 months after surgery. They also pointed out an 18 % risk reduction for a decrease of 5 BMI units [36].
As SG is gaining popularity, a systematic review that evaluates RYGB versus SG became an important need for the bariatric community to help with the decision on the best surgical procedure. Li et al reviewed 62 studies with 18,455 patients. Twenty-one studies reported hypertension resolution and the odds ratio favoring RYGB for the resolution of hypertension was 1.43. RYGB achieved a 60 % resolution while SG 51 % [15].
Perspectives
This review showed that metabolic surgery has a positive impact on the control of hypertension and cardiovascular risk, but there is no randomized trial to corroborate this observation.
We designed the first randomized trial to address this important question, the gastric bypass to treat obese patients with steady hypertension (GATEWAY) study. This ongoing randomized study is comparing the impact of RYGB and CMT on BP control. The primary aim is to evaluate the efficacy of RYGB to reduce the number of medications used for maintaining BP control (<140 × 90 mmHg). Secondary aims include 24-h ambulatory blood pressure monitoring (ABPM), central BP, augmentation index, arterial stiffness (evaluated by pulse wave velocity), and impact over sleep apnea. Patients will be followed-up for 5 years [37].
Conclusion
Bariatric surgery is the most efficient and durable treatment for morbid obesity and its comorbidities. Besides weight loss, recent trials focused on the remission of T2D, but their data pointed out benefits that go beyond diabetes resolution.
Hypertension remission rate is one of them. Probably, the most important, given its high prevalence when associated to obesity and a high CV risk related to high BP.
The status of blood pressure at baseline and the definition of hypertension resolution or improvement have a great variability between studies, making the interpretation of results controversial.
Some studies showed no reduction in BP after surgery because hypertensive patients had entered the study with a controlled BP, but they observed a significant reduction in the number of medications. This fact must be considered an indirect way to demonstrate reduction in BP.
In conclusion, bariatric surgery has the potential to reduce CV risk through the resolution or improvement of hypertension and can facilitate its treatment by reducing the necessity of medications resulting in a better adherence to treatment.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Obesity: Preventing and managing the global epidemic. Report of a WHO Consultation on Obesity. Geneva, 3-5 June 1997. World Health Organization, 1998. Division of Noncommunicable Diseases. Programme of Nutrition, Family and Reproductive Health. WHO/NUT/NCD/98.1: 1–158.
Brown CD, Higgins M, Donato KA, et al. Body mass index and the prevalence of hypertension and dyslipidemia. Obes Res. 2000;8:605–19. doi:10.1038/oby.2000.79.
Lloyd-Jones DM, Liu K, Colangelo LA, et al. Consistently stable or decreased body mass index in young adulthood and longitudinal changes in metabolic syndrome components: the Coronary Artery Risk Development in Young Adults Study. Circulation. 2007;115:1004–11. doi:10.1161/CIRCULATIONAHA.106.648642.
Landsberg L, Aronne LJ, Beilin LJ, et al. Obesity-related hypertension: pathogenesis, cardiovascular risk, and treatment. J Clin Hypertens. 2012;15:14–33. doi:10.1111/jch.12049.
Arora P, Reingold J, Baggish A, et al. Weight loss, saline loading, and the natriuretic peptide system. J Am Heart Assoc. 2014;4:e001265. doi:10.1161/JAHA.114.001265.
Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G. Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol. 2013;62:569–76. doi:10.1016/j.jacc.2013.05.045.
Pedrosa RP, Krieger EM, Lorenzi-Filho G, Drager LF. Recent advances of the impact of obstructive sleep apnea on systemic hypertension. Arq Bras Cardiol. 2011;97:e40–7.
Drager L, Borges FF, Lorenzi-Filho G. Effectiveness of continuous positive airway pressure in lowering blood pressure in patients with obstructive sleep apnea: a critical review of the literature. IBPC Vol. 2016;9:43–7. doi:10.2147/IBPC.S70402.
Kadowaki T. Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome. J Clin Invest. 2006;116:1784–92. doi:10.1172/JCI29126.
Kim DH, Kim C, Ding EL, et al. Adiponectin levels and the risk of hypertension: a systematic review and meta-analysis. Hypertension. 2013;62:27–32. doi:10.1161/HYPERTENSIONAHA.113.01453.
Gleysteen JJ, Barboriak JJ. Improvement in heart disease risk factors after gastric bypass. Arch Surg. 1983;118:681–4.
Pories WJ, MacDonald KG, Flickinger EG, et al. Is type II diabetes mellitus (NIDDM) a surgical disease? Ann Surg. 1992;215:633–42– discussion 643.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37. doi:10.1001/jama.292.14.1724.
Wilhelm SM, Young J, Kale-Pradhan PB. Effect of bariatric surgery on hypertension: a meta-analysis. Ann Pharmacother. 2014;48:674–82. doi:10.1177/1060028014529260. This is the only meta-analysis designed to study the effect of bariatric surgery on hypertension. It showed 50 % resolution.
Li J, Lai D, Wu D. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy to treat morbid obesity-related comorbidities: a systematic review and meta-analysis. Obes Surg. 2015;26:429–42. doi:10.1007/s11695-015-1996-9.
Adams TD, Davidson LE, Litwin SE, et al. Health benefits of gastric bypass surgery after 6 years. JAMA. 2012;308:1122–31. doi:10.1001/2012.jama.11164.
Cohen RV, Pinheiro JC, Schiavon CA, et al. Effects of gastric bypass surgery in patients with type 2 diabetes and only mild obesity. Diabetes Care. 2012;35:1420–8. doi:10.2337/dc11-2289.
Courcoulas AP. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA. 2013;310:1–10. doi:10.1001/jama.2013.280928. LABS-2 is a multicenter observational cohort study with 2458 participants that studied incidence and remission of comorbidities.
Marceau P, Biron S, Marceau S, et al. Long-term metabolic outcomes 5 to 20 years after biliopancreatic diversion. Obes Surg. 2015;25:1584–93. doi:10.1007/s11695-015-1599-5. A prospective cohort with 2615 patients submitted to BPD-DS with a long follow-up (5–20 years) that showed 64 % resolution and 31 improvement of hypertension.
Pinheiro JS, Schiavon CA, Pereira PB, et al. Long-long limb Roux-en-Y gastric bypass is more efficacious in treatment of type 2 diabetes and lipid disorders in super-obese patients. Surg Obes Relat Dis. 2008;4:521–5. doi:10.1016/j.soard.2007.12.016.
Rodríguez A, Becerril S, Valentí V, et al. Short-term effects of sleeve gastrectomy and caloric restriction on blood pressure in diet-induced obese rats. Obes Surg. 2012;22:1481–90. doi:10.1007/s11695-012-0702-4.
Zhang H, Pu Y, Chen J, et al. Gastrointestinal intervention ameliorates high blood pressure through antagonizing overdrive of the sympathetic nerve in hypertensive patients and rats. J Am Heart Assoc. 2014;3:e000929. doi:10.1161/JAHA.114.000929.
Ahmed AR, Rickards G, Coniglio D, et al. Laparoscopic Roux-en-Y gastric bypass and its early effect on blood pressure. Obes Surg. 2008;19:845–9. doi:10.1007/s11695-008-9671-z.
Sjöström L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307:56–65. doi:10.1001/jama.2011.1914.
Hallersund P, Sjöström L, Olbers T, et al. Gastric bypass surgery is followed by lowered blood pressure and increased diuresis—long term results from the Swedish Obese Subjects (SOS) study. PLoS ONE. 2012;7:e49696. doi:10.1371/journal.pone.0049696.
Belle SH, Berk PD, Courcoulas AP, et al. Safety and efficacy of bariatric surgery: longitudinal assessment of bariatric surgery. SOARD. 2007;3:116–26. doi:10.1016/j.soard.2007.01.006.
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366:1567–76. doi:10.1056/NEJMoa1200225.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370:2002–13. doi:10.1056/NEJMoa1401329. Randomized control trial that compared IMT with 2 surgical procedures, RYGB and SG. The authors showed a significant reduction of antihypertensive medications with a controlled blood pressure.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366:1577–85. doi:10.1056/NEJMoa1200111.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386:964–973. doi: 10.1016/S0140-6736(15)00075-6. Randomized control trial with the longest follow-up that compared CMT with two surgical procedures, BPD and RYGB. Authors showed a greater reduction of antihypertensive medications in the surgical group.
Ikramuddin S, Korner J, Lee W-J, et al. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA. 2013;309:2240–9. doi:10.1001/jama.2013.5835.
Ikramuddin S, Billington CJ, Lee W-J, et al. Roux-en-Y gastric bypass for diabetes (the Diabetes Surgery Study): 2-year outcomes of a 5-year, randomised, controlled trial. Lancet Diab Endocrinol. 2015;3:413–22. doi:10.1016/S2213-8587(15)00089-3. Randomized control trial that compared IMT with RYGB. Authors showed a greater reduction of antihypertensive medications with a controlled blood pressure in the surgical group.
Courcoulas AP, Goodpaster BH, Eagleton JK, et al. Surgical vs medical treatments for type 2 diabetes mellitus. JAMA Surg. 2014;149:707. doi:10.1001/jamasurg.2014.467.
Courcoulas AP, Belle SH, Neiberg RH, et al. (2015) Three-year outcomes of bariatric surgery vs lifestyle intervention for type 2 diabetes mellitus treatment. JAMA Surg. 2015;150(10):931–940. doi:10.1001/jamasurg.2015.1534
Halperin F, Ding S-A, Simonson DC, et al. Roux-en-Y gastric bypass surgery or lifestyle with intensive medical management in patients with type 2 diabetes. JAMA Surg. 2014;149:716. doi:10.1001/jamasurg.2014.514.
Ricci C, Gaeta M, Rausa E, et al. Long-term effects of bariatric surgery on type ii diabetes, hypertension and hyperlipidemia: a meta-analysis and meta-regression study with 5-year follow-up. Obes Surg. 2014;25:397–405. doi:10.1007/s11695-014-1442-4.
Schiavon CA, Ikeoka DT, de Sousa MG, et al. Effects of gastric bypass surgery in patients with hypertension: rationale and design for a randomised controlled trial (GATEWAY study). BMJ Open. 2014;4:e005702. doi:10.1136/bmjopen-2014-005702.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Carlos Aurelio Schiavon, Luiz A. Bortolotto, Celso Amodeo, Dimas Ikeoka, Otávio Berwanger, and Ricardo Vitor Cohen declare that they have no conflict of interest.
Luciano F. Drager declares personal fees from Ethicon for the development of an educational presentation/service on a speakers’ bureau.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Lipid and Metabolic Effects of Gastrointestinal Surgery
Rights and permissions
About this article
Cite this article
Schiavon, C.A., Drager, L.F., Bortolotto, L.A. et al. The Role of Metabolic Surgery on Blood Pressure Control. Curr Atheroscler Rep 18, 50 (2016). https://doi.org/10.1007/s11883-016-0598-x
Published:
DOI: https://doi.org/10.1007/s11883-016-0598-x