Abstract
The initial observation of functional recovery in dysfunctional myocardium following revascularization led to the introduction of the concept of hibernating myocardium. Since then, the pathophysiologic basis of hibernating myocardium has been well described. Multiple imaging modalities have been utilized to prospectively detect viable myocardium and thus predict its functional recovery following revascularization. It has been hypothesized that viability imaging will be instrumental in the selection of patients with ischemic cardiomyopathy likely to benefit from revascularization. Multiple observational studies built a large body of evidence supporting this concept. However, data from prospective studies failed to substantiate utility of viability testing. This review aims to summarize the current literature and describe the role of viability imaging in current clinical practice as well as future directions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hibernating myocardium has been described as “a state of persistently impaired myocardial and left ventricular (LV) function at rest due to reduced coronary blood flow that can be partially or completely restored to normal if the myocardial oxygen supply/demand relationship is favorably altered, either by improving blood flow and/or by reducing demand” [1]. The term hibernating myocardium was coined after observing that certain dysfunctional myocardial segments regained normal function after Coronary Artery Bypass Surgery (CABG) and demonstration of metabolic activity in these segments on positron emission tomography (PET) imaging. In addition to myocardial scarring and stunning, hibernating myocardium contributes to left ventricular dysfunction seen in ischemic cardiomyopathy (ICM). Currently, 5.7 million patients suffer from heart failure in the USA alone with an annual incidence of 870,000 cases. The foreseen increase in the prevalence of HF will top 8 million by 2030 [2]. Coronary artery disease (CAD) is a contributing factor in 50–70 % of all cases of heart failure [3]. Heart failure is associated with significant morbidity and mortality, and revascularization plays a significant role in management of these patients.
Pathophysiology
There are multiple mechanisms by which obstructive CAD leads to LV systolic dysfunction in ischemic cardiomyopathy (ICM). In a normal heart, myocardial oxygen extraction is near maximal and there are limited anaerobic reserves. Therefore, acute ischemia caused by even a small reduction in myocardial blood flow has been shown to reduce myocardial contractility [4]. Myocardial stunning is defined as myocardial dysfunction that persists after an episode of transient ischemia despite the absence of irreversible damage. There is a perfusion-contraction mismatch, that is, the presence of decreased contractility despite normal perfusion [5]. Various mechanisms including generation of oxygen-derived free radicals, excitation-contraction uncoupling due to sarcoplasmic reticulum dysfunction, and calcium overload have been proposed to cause myocardial stunning [6].
Hibernating myocardium is a state of persistently reduced myocardial contractility due to reduced coronary blood flow at rest, which is partially or completely reversible upon revascularization. In hibernation, there is perfusion-contraction matching, and it is considered an adaptive response of the myocardium to chronically reduced blood supply. Metabolic changes similar to stunning such as generation of free radicals and depletion of ATP also occur in hibernating myocardium. In addition, cellular changes such as loss of myofibrils, disorganization of the myofilaments, and appearance of large areas filled with glycogen have been demonstrated in hibernating myocytes. Cellular degeneration and reparative fibrosis have also been observed in areas of hibernating myocardium, potentially making these areas less likely to recover after revascularization [7]. Myocardial infarction (MI) is caused by acute severe reduction in coronary blood flow which ultimately results in irreversible necrosis of cardiac myocytes. Myocardial scar can result from a prior MI or as a consequence of chronic hibernation leading to irreversible structural changes and fibrosis. Areas of hibernating myocardium and myocardial scar contribute to the development of ICM, and it is imperative to differentiate between the two as hibernating myocardium has the potential to recover functionally.
Assessment of Myocardial Viability in Chronic ICM
Hibernating myocardium can be most accurately defined by functional recovery following revascularization. Myocardial viability is the term prospectively applied to hibernating myocardium and demonstrates intact cell membrane and metabolism, and contractile reserve. Multiple imaging modalities have been used to identify and quantify viable myocardium prior to revascularization, to predict functional recovery after revascularization and thus aiding in decision making in the management of patients with ICM [8]. Different attributes of hibernating myocardium can be used to detect viable myocardium by various imaging modalities such as integrity of the cell membrane using 99mTechnitium Sestamibi and 201 Thallium Single Photon Emission CT (SPECT) imaging, metabolic imaging with FDG positron emission tomography (PET), contractile reserve using dobutamine stress echocardiography (DSE)/SPECT/Cardiac Magnetic Resonance (CMR), and scar imaging using CMR.
Contractile reserve of the viable myocardium can be detected by low dose dobutamine echocardiography (LDDE). Hibernating myocardial segments are hypokinetic or akinetic on baseline echocardiogram and show improved contractility with low-dose dobutamine (LDD) infusion. Improvement in contractility of myocardial segments on LDD infusion predicts functional recovery following revascularization with reasonable accuracy [9]. In a pooled analysis, LDDE was found to have a mean sensitivity of 84 % and a mean specificity of 81 % to detect recovery of contractile function after revascularization [8].
SPECT tracers used to assess myocardial viability detect the integrity of the cell membrane and Na/K Pump with 201Tl and preserved mitochondrial function with Tc-99m Sestamibi [10] (see Fig. 1). Although Tc-99m Sestamibi is primarily considered as a perfusion agent, quantitative analysis of Tc-99m Sestamibi uptake on rest injection images can be used to assess viable myocardium and its sensitivity can be increased by use of nitrate injection [11, 12]. There are various imaging protocols available to quantify distribution of these tracers in the myocardium, and various diagnostic criteria are used to define viable myocardium. A pooled analysis of 201 Thallium rest redistribution studies demonstrated a sensitivity and specificity of 86 and 59 %, respectively, for predicting functional recovery after revascularization [13]. Mean sensitivity and specificity were 81 and 66 % for pooled analysis of studies using Technitium-99m sestamibi tracer.
In PET imaging, NH3 is used as the perfusion tracer and F18 FDG is the most commonly used tracer for assessment of metabolic activity [14]. Hibernating/viable myocardium preferentially utilizes glucose instead of free fatty acids. Viable myocardium is detected on PET imaging by areas of reduced perfusion and preserved FDG uptake (areas of mismatch). In a pooled analysis, the mean sensitivity and specificity of FDG PET studies were 93 and 58 %, and the mean positive predictive value (PPV) and negative predictive value (NPV) were 71 and 86 % [11].
CMR can be used for the assessment of myocardial viability using multiple techniques: measuring end diastolic wall thickness (EDWT), assessing myocardial contractility using LDD infusion, and detecting delayed enhancement (DE) using gadolinium-based contrast agents [15]. DE CMR imaging is based on the premise that gadolinium does not penetrate tissues with intact cell membranes but accumulates in infarcted tissue and thus making the infarcted tissue appear hyperenhanced/bright. Due to the superior spatial resolution, DE CMR can detail the extent and transmurality of scar tissue (see Figs. 2 and 3). A 50 % cutoff of LV wall hyperenhancement is generally used to determine whether or not a LV segment will recover function following revascularization (hyperenhancement <50 % wall thickness implies viable myocardium) [16]. A meta-analysis of 11 studies using DE CMR found the mean sensitivity and specificity for predicting functional recovery of contractility following revascularization to be 95 and 51 %, respectively, whereas the PPV was 69 % and NPV was 90 % [15]. In the same meta-analysis, nine studies of dobutamine stress CMR using LDD infusion demonstrated a sensitivity and specificity of 81 and 91 %, whereas the PPV and NPV were 93 and 75 %, respectively. EDWT of <5.5–6 mm on CMR likely represents areas of scar and can be used to identify areas of myocardium that are not viable. In a meta-analysis of four studies using EDWT, the mean-weighted sensitivity and specificity were 96 and 38 %, whereas the PPV and NPV were 71 and 85 %, respectively [15]. Based on these findings, it can be concluded that DE CMR provides the highest sensitivity and NPV for predicting recovery of functionality after revascularization, whereas LDD CMR provides the highest specificity and PPV of any currently available test to evaluate myocardial viability. Combining these two modalities may have a role in improving accuracy of myocardial viability assessment.
SPECT Versus CMR Comparison for Detecting Subendocardial Infarcts
In 2003, Wagner et al. [17] published an analysis of 92 patients with known or suspected coronary artery disease who underwent both CMR and SPECT. They found that all segments with transmural MI were identified by both modalities; however, nearly half (47 %) of all segments with subendocardial infarctions were missed by SPECT. This lack of sensitivity was attributed to the low spatial resolution of SPECT (around 10 mm), compared to CMR spatial resolution of 1–2 mm [17].
Assessment of Myocardial Viability After AMI
Rischpler et al. studied the use of FDG PET and DE CMR in 20 patients 5–7 days after AMI [18]. Patients underwent repeat CMR at 6 months to evaluate functional recovery of myocardial segments, with functional recovery defined as improvement in the wall motion score by at least one point in each previously dysfunctional segment. Functional recovery was significantly better in segments found to be viable on CMR and PET compared to nonviable segments. Sixty-five percent of viable segments on CMR had functional recovery, and 78 % of PET viable segments showed functional recovery.
Viability and Revascularization in Ischemic Cardiomyopathy (ICM)
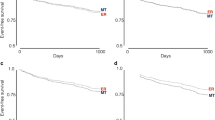
Multiple observational studies have shown improved outcomes after revascularization in patients with ICM and presence of myocardial viability on imaging. A meta-analysis of 24 viability studies performed prior to 1999 including 3088 patients demonstrated that in patients with presence of viability, revascularization was associated with 79.6 % reduction in annual mortality (3.2 versus 16 %) compared to medical therapy alone [19]. A subsequent meta-analysis of 14 nonrandomized studies published between 1998 and 2006 also showed significant reduction in annual mortality in patients with ischemic LV dysfunction and viable myocardium with revascularization compared to medical therapy (3.71 % versus 10.64) [20]. These studies also demonstrated that patients with ICM and nonviable myocardium had increased mortality irrespective of therapy compared to patients with viable myocardium. A recent meta-analysis of previously published 32 observational studies demonstrated that patients with viability had a significant reduction in mortality with revascularization compared to medical therapy (7.3 vs 27.4 %, RR 0.31, 95 % CI 0.25–0.39) over a mean follow-up of 28 months [21]. In the same study, in patients without viability, revascularization did not show significant improvement in mortality compared to medical therapy (RR 0.92, 95 % CI 0.78–1.09). However, in addition to a non-randomized trial design and selection bias, there are many shortcomings in the studies included in these meta-analyses. Most patients were not on currently accepted optimal medical therapy including ACE inhibitors, beta blockers, and mineralocorticoid inhibitors, and use of implantable defibrillators was low.
A few randomized trials have prospectively evaluated the impact of viability on revascularization-related outcomes. The viability sub-study of the STICH trial is the largest randomized study so far assessing effects of viability on outcomes with revascularization compared to optimal medical therapy alone [22••, 23]. The main STITCH trial randomized 1212 patient with CAD and left ventricular ejection fraction (LVEF) <35 % to optimal medical therapy or optimal medical therapy with CABG. There was no significant difference in the primary endpoint of all-cause mortality between the two groups. Viability testing was optional and patients were not randomized based on the presence or absence of viability. Of the 1212 enrolled patients, 601 underwent viability testing. Viability was assessed using SPECT in 471 patients and DSE in 280 patients (150 patients had both viability studies). Viability was classified in a binary fashion (present or absent) using prespecified criteria. For SPECT, viability was defined as ≥11 viable segments based on relative tracer activity using a 17-segment model. For DSE, viability was defined as ≥5 segments with abnormal resting systolic function manifesting contractile reserve with dobutamine using a 16-segment model. Myocardial viability was present in 487 (81 %) patients. Patients with viable myocardium had lower overall rates of death than those without viable myocardium (hazard ratio 0.64; 95 % CI 0.48–0.86; p = 0.003). However, in patients with myocardial viability revascularization with CABG did not show any improvement in mortality compared to medical therapy alone (HR 0.86; 95 % CI 0.64–1.16). In a recent analysis, patients were analyzed in two groups using median left ventricular end systolic volume index (ESVI) [24]. Overall, there was no interaction between ESVI, viability status, and treatment assignment to CABG versus medical therapy with respect to survival (p = 0.491). In patients with viability, effect of CABG compared to medical therapy in patients with ESVI <84 ml/m2 (HR 0.85; 95 % CI 0.56 to 1.29) was not different to that of patients with ESVI >84 ml/m2 (HR 0.87; 95 % CI 0.57 to 1.31). Furthermore, no significant differences were noted when the data was analyzed in an as-treated manner compared to intention-to-treat.
The results of the STICH trial are contrary to what previous observational studies have shown. Possible explanations for these findings include high adherence to guideline-directed medical therapy and lower mortality in patients receiving medical therapy alone (about 7 % per year). The prospective randomized nature of study may have eliminated selection bias that was likely present in the retrospective observational studies. Other limitations include different thresholds used in the definition of viability between SPECT and DSE, viability classified in a binary rather than continuous fashion and significant crossover between the treatment arms. Moreover, the STICH viability trial was merely a sub-study that was not powered to detect a difference between the two groups and the use of viability testing was not randomized [25].
Another prospective randomized trial, the Heart Failure Revascularization trial (HEART) was terminated early with enrollment of only 138 of the planned 800 patients [26•]. It included patients with LVEF ≤35 % and the presence of viability on imaging (primarily DSE) randomized to invasive strategy with intent to revascularization versus medical therapy alone. After a median follow-up of 59 months, there were 25 (37 %) deaths in those assigned to the conservative strategy and 26 (38 %) in those assigned to the invasive strategy. Although HEART did not show any difference in mortality between the two groups, there are significant limitations of HEART including lack of power to detect a difference in mortality and about 30 % of patients randomized to invasive strategy not undergoing revascularization.
The F-18-Fluorodeoxyglucose Positron Emission Tomography Imaging-Assisted Management of Patients with Severe Left Ventricular Dysfunction and Suspected Coronary Disease (PARR-2) trial evaluated PET-guided strategy for management of patients with LV dysfunction [27••]. Patients were randomized to management assisted by FDG PET (n = 218) or standard care (n = 212). The primary composite outcome of death, MI, and hospitalization for cardiac cause at 1 year was not significantly different in the PET arm versus the standard arm (30 vs 36 %). However, in the PET arm, approximately 25 % of patients did not receive PET-guided treatment. In patients who received PET-guided therapy, a significant reduction in the primary endpoint was noted. Recently, the 5-year follow-up of the PARR-2 study was published and continued to show lack of difference in outcome between the two groups [28•] (see Table 1).
Viability and Revascularization in Patients with Recent Myocardial Infarction
Long-term follow-up of viability-guided angioplasty after acute myocardial infarction (VIAMI) trial was recently published [29]. VIAMI trial included stable patients 48 h after ST elevation myocardial infarction who were not treated by primary or rescue percutaneous coronary intervention (PCI). Patients underwent low-dose DSE 72 hours after their MI for assessment of viability. Viability was defined as the improvement of wall motion abnormalities (WMAs) in two or more segments of the infarct zone. Patients with viability in the infarct area on noninvasive imaging were randomized to either PCI or conservative management. Patients were followed up for a median of 8 years. The combined endpoint of death, recurrent MI, and unstable angina was 20.8 % in the invasive group and 32.7 % in the conservative group (HR 0.59; 95 % CI 0.36–0.99, p = 0.049). No differences in mortality (8.5 vs. 8.2 %, p = 0.80) or recurrent MI (7.5 vs. 10.9 %, p = 0.48) were noted.
Viability and Prognosis in ICM
Observational studies have shown that in patients with ICM with the presence of viable myocardium, treatment with medical therapy alone portends worse prognosis [21]. Taking into account the results of the prospective randomized trials, this finding is likely a result of selection bias as patients with significant comorbid conditions and shorter expected survival may not have been offered revascularization. In the 5-year follow-up of the prospective, randomized STICH trial, overall mortality was higher in patients with nonviable myocardium compared to those with viability in unadjusted analysis (51 vs 37 %, HR = 0.64, p = 0.003). However, it was not significant after adjustment for significant baseline prognostic variables (p = 0.21). However, there was no excess mortality in patients with viability who were treated medically compared to those who underwent surgical revascularization (see Table 1).
Current Utility of Viability Assessment
The role of revascularization in patients with ischemic LV dysfunction for the purpose of improving LV function is not clear. There are very few prospective randomized trials that have evaluated viability assessment prior to revascularization, and these have failed to show a significant difference in outcomes with revascularization compared to medical therapy. It is important to note that optimal medical therapy has improved mortality in this high-risk patient population with an annual mortality of 7 % in the STICH trial. Therapy with carvedilol has been shown to improve LVEF in patients with ICM and presence of viability [30]. Other limitations in these prospective trials include various methods used to assess viability with varied accuracies and different thresholds used to define viability. Moreover, the probability of LV functional improvement is multifactorial and may not be captured solely by viability imaging. Factors that affect functional recovery include presence and magnitude of ischemia, stage of cellular degeneration within the viable myocytes, degree of LV remodeling, timing of revascularization, and success of revascularization. Thus, based on current evidence, decision for revascularization should not be solely based on presence of myocardial viability.
Future Perspective
Myocardial viability has been well described as one of the mechanisms causing ischemic LV dysfunction with a potential for functional recovery after revascularization. The hypothesis that accurate viability assessment in patients with ischemic cardiomyopathy will identify patients most likely to benefit from revascularization has been tested in multiple observational studies and few prospective trials, with conflicting results. There is still a need to more definitively test this hypothesis. There are few ongoing trials that will address this question.
Revascularization for ischemic ventricular dysfunction (REVIVED-BCIS2) is a prospective randomized control trial, which will include patients with ischemic LV dysfunction with LVEF ≤30 % [31]. All patients will undergo viability assessment using DSE or DE CMR, and patients with viability in >30 % of the dysfunctional areas will be enrolled and randomized to PCI plus optimal medical therapy (OMT) or OMT alone. Cardiac imaging in ischemic heart failure (AIMI-HF) is a prospective randomized trial that is currently enrolling patients with LVEF <45 % and suspected or known CAD [32]. Patients will be randomized to advanced imaging strategies using PET/CMR or CTA or standard imaging strategies using SPECT followed by management that will be guided by these imaging strategies. The primary objective of this trial is to evaluate the effect of these two imaging strategies on the composite clinical endpoint of cardiac death, MI, resuscitated cardiac arrest, and cardiac rehospitalization. Lastly, the Cardiac FDG PET Registry (CADRE) is a large multicenter registry that will evaluate impact of FDG PET myocardial viability assessment in management of patients with severe LV systolic dysfunction (LVEF <35 %) [33].
Conclusion
Recovery of contractile function in hibernating myocardium has been well described and supported by observational data. However, prospective randomized studies have failed to demonstrate any significant interaction between the presence of viable myocardium and clinical outcomes following revascularization. Until data from ongoing clinical trials become available, presence or absence of viable myocardium should be considered along with other clinical factors for decision making in the management of patients with ischemic cardiomyopathy.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Rahimtoola SH. The hibernating myocardium. Am Heart J. 1989;117(1):211–21.
Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–e322.
Roger VL. Epidemiology of heart failure. Circ Res. 2013;113(6):646–59.
Vatner SF. Correlation between acute reductions in myocardial blood flow and function in conscious dogs. Circ Res. 1980;47(2):201–7.
Heusch G. The regional myocardial flow-function relationship: a framework for an understanding of acute ischemia, hibernation, stunning and coronary microembolization. Circ Res 2013. 1980;112(12):1535–7.
Bolli R. Mechanism of myocardial “stunning”. Circulation. 1990;82(3):723–38.
Elsasser A, Schlepper M, Klovekorn WP, et al. Hibernating myocardium: an incomplete adaptation to ischemia. Circulation. 1997;96(9):2920–31.
Bax JJ, Wijns W, Cornel JH, Visser FC, Boersma E, Fioretti PM. Accuracy of currently available techniques for prediction of functional recovery after revascularization in patients with left ventricular dysfunction due to chronic coronary artery disease: comparison of pooled data. J Am Coll Cardiol. 1997;30(6):1451–60.
La Canna G, Alfieri O, Giubbini R, Gargano M, Ferrari R, Visioli O. Echocardiography during infusion of dobutamine for identification of reversibly dysfunction in patients with chronic coronary artery disease. J Am Coll Cardiol. 1994;23(3):617–26.
Allman KC. Noninvasive assessment myocardial viability: current status and future directions. J Nucl Cardiol. 2013;20(4):618–37. quiz 638-619.
Udelson JE, Coleman PS, Metherall J, et al. Predicting recovery of severe regional ventricular dysfunction. Comparison of resting scintigraphy with 201Tl and 99mTc-sestamibi. Circulation. 1994;89(6):2552–61.
Sciagra R, Bisi G, Santoro GM, et al. Comparison of baseline-nitrate technetium-99m sestamibi with rest-redistribution thallium-201 tomography in detecting viable hibernating myocardium and predicting postrevascularization recovery. J Am Coll Cardiol. 1997;30(2):384–91.
Bax JJ, Poldermans D, Elhendy A, Boersma E, Rahimtoola SH. Sensitivity, specificity, and predictive accuracies of various noninvasive techniques for detecting hibernating myocardium. Curr Probl Cardiol. 2001;26(2):147–86.
Tillisch J, Brunken R, Marshall R, et al. Reversibility of cardiac wall-motion abnormalities predicted by positron tomography. N Engl J Med. 1986;314(14):884–8.
Romero J, Xue X, Gonzalez W, Garcia MJ. CMR imaging assessing viability in patients with chronic ventricular dysfunction due to coronary artery disease: a meta-analysis of prospective trials. J Am Coll Cardiol Img. 2012;5(5):494–508.
Kim RJ, Wu E, Rafael A, et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000;343(20):1445–53.
Wagner A, Mahrholdt H, Holly TA, et al. Contrast-enhanced MRI and routine single photon emission computed tomography (SPECT) perfusion imaging for detection of subendocardial myocardial infarcts: an imaging study. Lancet. 2003;361(9355):374–9.
Rischpler C, Langwieser N, Souvatzoglou M, et al. PET/MRI early after myocardial infarction: evaluation of viability with late gadolinium enhancement transmurality vs. 18F-FDG uptake. Eur Heart J Cardiovasc Imaging. 2015;16(6):661–9.
Allman KC, Shaw LJ, Hachamovitch R, Udelson JE. Myocardial viability testing and impact of revascularization on prognosis in patients with coronary artery disease and left ventricular dysfunction: a meta-analysis. J Am Coll Cardiol. 2002;39(7):1151–8.
Camici PG, Prasad SK, Rimoldi OE. Stunning, hibernation, and assessment of myocardial viability. Circulation. 2008;117(1):103–14.
Orlandini A, Castellana N, Pascual A, et al. Myocardial viability for decision-making concerning revascularization in patients with left ventricular dysfunction and coronary artery disease: a meta-analysis of non-randomized and randomized studies. Int J Cardiol. 2015;182:494–9.
Bonow RO, Maurer G, Lee KL, et al. Myocardial viability and survival in ischemic left ventricular dysfunction. N Engl J Med. 2011;364(17):1617–25. This is the largest study to date to prospectively assess myocardial viability and clinical outcomes after revascularization.
Velazquez EJ, Lee KL, Deja MA, et al. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med. 2011;364(17):1607–16.
Bonow RO, Castelvecchio S, Panza JA, et al. Severity of Remodeling, Myocardial Viability, and Survival in Ischemic LV Dysfunction After Surgical Revascularization. J Am Coll Cardiol Img. 2015;8(10):1121–9.
Chareonthaitawee P, Gersh BJ, Panza JA. Is viability imaging still relevant in 2012? J Am Coll Cardiol Img. 2012;5(5):550–8.
Cleland JG, Calvert M, Freemantle N, et al. The Heart Failure Revascularisation Trial (HEART). Eur J Heart Fail. 2011;13(2):227–33. Prospective comparison of conservative management versus revacsularization in patients with heart failure and a reduced LVEF but who have evidence of substantial myocardial viability.
Beanlands RS, Nichol G, Huszti E, et al. F-18-fluorodeoxyglucose positron emission tomography imaging-assisted management of patients with severe left ventricular dysfunction and suspected coronary disease: a randomized, controlled trial (PARR-2). J Am Coll Cardiol. 2007;50(20)):2002–12. The largest study to date with random allocation to myocardial viability imaing.
Shukla BAMA T, Nichol G, Davies RA, Duchesne L, Ruddy TD, Chow B, et al. Long term follow up of outcomes with f-18-fluorodeoxyglucose positron emission tomography imaging- assisted management of patients with severe left ventricular dysfunction secondary to coronary disease: 5-year follow-up of the parr-2 randomized controlled trial. Can J Cardiol. 2014;30(10):S266. Five year results of the PARR 2 study.
van Loon RB, Veen G, Baur LH, Twisk JW, van Rossum AC. Long-term follow-up of the viability guided angioplasty after acute myocardial infarction (VIAMI) trial. Int J Cardiol. 2015;186:111–6.
Cleland JG, Pennell DJ, Ray SG, et al. Myocardial viability as a determinant of the ejection fraction response to carvedilol in patients with heart failure (CHRISTMAS trial): randomised controlled trial. Lancet. 2003;362(9377):14–21.
Perera D. Study of Efficacy and Safety of Percutaneous Coronary Intervention to Improve Survival in Heart Failure (REVIVED-BCIS2). 2013.
O’Meara E, Mielniczuk LM, Wells GA, et al. Alternative Imaging Modalities in Ischemic Heart Failure (AIMI-HF) IMAGE HF Project I-A: study protocol for a randomized controlled trial. Trials. 2013;14:218.
Rob Beanlands RSB. Cardiac FDG PET Viability Registry (CADRE). 2008.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Pavan Patel, Alexander Ivanov, and Kumudha Ramasubbu declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Coronary Heart Disease
Rights and permissions
About this article
Cite this article
Patel, P., Ivanov, A. & Ramasubbu, K. Myocardial Viability and Revascularization: Current Understanding and Future Directions. Curr Atheroscler Rep 18, 32 (2016). https://doi.org/10.1007/s11883-016-0582-5
Published:
DOI: https://doi.org/10.1007/s11883-016-0582-5