Abstract
Transcatheter aortic valve replacement (TAVR) is an alternative and now recommended therapy for patients who meet indications for surgical valve replacement and are high or prohibitive surgical risk. Available TAVR technologies are rapidly emerging to treat this complex patient population. This review discusses the specific valve designs of the transcatheter heart valves currently used, newer generation modifications to overcome limitations of earlier valve designs, and novel imaging modalities, such as computed tomographic angiography-fluoroscopy and echocardiography-fluoroscopy fusion imaging, available for pre-procedural planning and intra-procedural guidance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Degenerative calcific aortic stenosis (AS) is the most common form of acquired valvular heart disease in the Western world with occurrence rates of 2 % in individuals ≥65 years of age and double with each decade thereafter [1, 2]. As the population ages, the prevalence of AS is expected to increase portending considerable morbidity and mortality if left untreated. The latency period for AS is long but once symptomatic, prognosis is poor and progression is rapid. Approximately 50 % of patients die within 2 to 3 years of developing symptoms.
Historically, the recommended treatment for severe, symptomatic AS has been surgical aortic valve replacement (SAVR). Due to advanced age and the associated high burden of comorbidities, SAVR carries significant mortality in this complex patient population. Currently, transcatheter aortic valve replacement (TAVR) is an alternative and now recommended therapy for patients who meet indications for SAVR and have a high or prohibitive surgical risk, approximately 30 to 50 % of the cases [3]. On the other hand, the role of TAVR in the intermediate risk population remains unclear and data from the recently completed Placement of Aortic Transcatheter Valve (PARTNER) IIA and ongoing Surgical Replacement and Transcatheter Aortic Valve Implantation (SurTAVI) trials will help to better define its utility. In addition, SAVR is also evolving with hybrid technologies such as collapsible, stent-mounted prostheses placed in a sutureless fashion using conventional surgical techniques in non-high-risk patients, thereby reducing aortic cross-clamp and myocardial ischemia times [4].
Available TAVR technologies are rapidly emerging, from balloon- and self-expanding transcatheter heart valves (THVs) to hybrid sutureless THVs with adjunctive use of novel imaging modalities, such as computed tomographic angiography (CTA)-fluoroscopy and echocardiography-fluoroscopy fusion imaging. This review discusses the specific designs of several THVs currently used, evolving valve modifications to overcome limitations of earlier valve designs, as well as the newer imaging technologies now available for pre-procedural planning and guidance of THV implantation.
Balloon-Expandable Transcatheter Heart Valves
Balloon-expandable valve technology was first introduced in 2000 by Boenhoffer et al. with implantation in the pulmonic position and in 2002 by Cribier et al. in the aortic position [5, 6]. The Cribier-Edwards THV (Edwards Lifescience, Irvine, CA) consisted of a stainless steel stent frame with initially equine later bovine pericardium to generate the unidirectional, intra-annular trileaflet valve (Edwards SAPIEN THV) (Fig. 1). A fabric cuff on the proximal one third of the frame improved the seal around the native annulus. The valve was crimped onto a delivery balloon and deployed using a 22- or 24-F catheter for 23- and 26-mm valves, respectively [7].
Available transcatheter heart valve designs include the balloon-expandable valves: SAPIEN, Sapien XT, Sapien 3 (Edwards Lifesciences, Irvine CA); the self-expandable valves: CoreValve and CoreValve Evolut R (Medtronic, Minneapolis MN), Portico (St Jude Medical, St Paul MN); alternative valve designs: Lotus (Boston Scientific, Natick MA) with a mechanical deployment mechanism and Direct Flow (DF Medical, Santa Rosa CA) with dual ring inflation for expansion; and sutureless, rapid deployment valves: Perceval S (Sorin, Saluggia Italy) and Intuity (Edwards Lifesciences)
Numerous studies including the PARTNER trial and registries have shown the safety and efficacy of balloon-expandable THV. In inoperable patients, composite of death or stroke was lower after TAVR versus standard medical therapy (57 vs 81 %, p < 0.001) with a significant improvement in NYHA functional class (29.7 vs 4.8 % NYHA class I/II, p < 0.0001) sustained up to 3 years [8]. In high-risk patients, rates of death from any cause (34 vs 35 %) and improvement in NYHA functional class (84 vs 85 %) were similar between the TAVR and SAVR groups up to 2 years. However, moderate or severe paravalvular leak (PVL) occurred more frequently after TAVR (6.9 vs 0.9 % at 2-year follow-up, p < 0.001) and even mild PV regurgitation was associated with increased late mortality [9, 10]. PVL occurs due to poor valve apposition with the annulus or malpositioning of the device; it may require post-balloon valvuloplasty, valve repositioning, or valve-in-valve deployment. In addition, the incidence of major vascular complications occurred in as high as 23 % of patients, not unanticipated given the need for large-bore sheath placement and degree of calcific atherosclerotic peripheral arterial disease in this population [11].
The second-generation balloon-expandable THVs is the Sapien XT, recently FDA-approved in the USA. The stent is made of cobalt chromium, allowing for thinner and reduced number of struts. In addition, multiple changes have been made to reduce the overall profile, including (1) a more open-frame design that permits for tighter crimping, (2) scalloped leaflets and a partially closed configuration, and (3) in situ valve mounting onto the balloon [11–13]. These modifications have reduced the delivery system to 16, 18, and 20 F for their respective valve size, 23, 26, and 29 mm. The resultant profile reduction translated into a threefold reduction in major vascular events (11 vs 33 %) without compromise in valve performance [12]. In addition, an internal polyethylene terephthalate (PET) skirt was added for improved annular seal.
The latest edition to the balloon-expandable THV family is the Sapien 3, now CE-marked in Europe. Like the previous generation Sapien XT, it consists of a trileaflet pericardial bovine valve mounted in a cobalt chromium stent [13]. A unique stent and leaflet design allows for crimping to a further reduced profile, which is compatible with a 14-F expandable sheath. Some patients previously deemed unsuitable for a transfemoral TAVR approach due to small vessel diameters may benefit from this system and reduce the need for alternative access. In addition to the inner cuff, an outer PET sealing cuff is added to further fill PV gaps and reduce the risk of PV regurgitation [13]. Although limited data have been published, rates of PVL are promising with First-in-Man reports suggesting that there is no more than mild PV regurgitation present post-implantation [14].
Self-Expanding Transcatheter Heart Valves
Self-expandable valve technology was introduced in 2005, with the first implantation by Grube et al. [15]. CoreValve (Medtronic, Minneapolis, MN) is a supra-annular, initially bovine later porcine pericardium valve mounted on a self-expanding nickel-titanium (nitinol) alloy frame (Fig. 1). The advantage of nitinol is its thermal memory. At colder temperatures, it is flexible and can easily be introduced into the body; once deployed, it becomes rigid as it adapts to body temperature and regains its original shape. Nitinol allows for all valve sizes (23, 26, 29, and 31 mm) to be compressed and loaded into an 18-F delivery system.
Stent shape is that of an hourglass, with a diamond-shaped cell design that is sectioned off into areas of different radial force: the inlet portion has high radial force in order to expand against the native calcified leaflets; the middle portion, constructed to avoid obstructing the coronary arteries, allows blood to flow freely and accommodate coronary artery catheters; and the outlet portion has a flared design to fixate and facilitate co-axial positioning [1, 16]. In addition, a porcine skirt is added to the inlet portion (lowest 12 mm) for improved annular seal. The valve has the ability of being “repositionable and retrievable” while it is partially (up to two thirds) deployed. However, this entails poorly controlled pulling of the system for repositioning and dragging the exposed valve the entire length of the aorta until sheath entry.
The CoreValve system has the largest experience with self-expanding THV worldwide. Numerous trials including the recently reported CoreValve US trial have shown the safety and efficacy of self-expandable THV. In inoperable patients, composite of all-cause mortality or major stroke was lower after TAVR versus standard medical therapy (26 vs 43 %, p < 0.0001) with a significant improvement in NYHA functional class sustained up to 1 year [17]. The frequency of moderate or severe PV regurgitation was low, 11 % at discharge, and improved to 4.2 % by 1 year, potentially suggesting ongoing remodeling or expansion at the annular-THV interface. In high-risk patients, there was a significantly lower rate of mortality at 1 year compared to SAVR (14 vs 19 %, p < 0.001 for noninferiority and p = 0.04 for superiority), revealing superiority of a THV to SAVR for the first time [18].
Self-expanding THVs have been associated with significantly higher rates of conduction disturbances and need for post-procedural pacemakers. Rate of pacemaker implantation with self-expanding THV is as high as 26 % at 1 year compared to around 5 % with balloon-expandable THV [17, 18]. The greater incidence of pacemaker implantation is postulated to be due to mechanical trauma from the inflow frame at the membranous septum, in the region of the atrioventricular conduction system and left bundle branch. High radial forces in this portion of the stent, along with deep implantation within the left ventricular outflow tract, can play a role.
The next generation of CoreValve, Evolut R (Medtronic, Minneapolis, MN), employs many of the characteristics of its predecessor; however, there are several new key features that provide improved anatomical fit, annular seal, and durability [19, 20]. Along with a cell geometry and frame redesigned to optimize the interaction between the frame and the native anatomy, this valve is intended to reduce the probability of PVLs through an extended skirt. Evolut R has a shorter frame compared to the original CoreValve by approximately 10 %. It allows for a better fit, most notably in patients with an angulated anatomy. In addition, the valve leaflets are treated with alpha-amino oleic acid (AOA) to hamper calcium deposition. Overall, the most important evolution is the ability to truly resheath or recapture the partially deployed (up to 80 % of maximal deployment) THV into a 14-F sheath.
The next generation of self-expanding THV also includes the Portico THV (St. Jude Medical, St. Paul MN). This THV embodies a self-expanding nitinol frame with three bovine pericardial leaflets and a porcine pericardial sealing cuff [21, 22]. The stent frame has wide diamond-shaped cells that allow for access to the coronary arteries, while the pericardial tissue from the sealing cuff molds the calcific nodules in the annulus to reduce PVL. Similar to the Evolut R, the Portico valve has the ability to be resheathed and repositioned after it has been almost fully deployed; while the valve is partially deployed, the leaflets are fully functional and can be resheathed or repositioned until it reaches 80 % of deployment. This feature on both the Evolute R and Portico THV allows for confirmation of appropriate implantation depth and assessment for the presence of significant PVL prior to release. In addition, a short valve height is designed for optimal seal with minimal protrusion into the outflow tract, and a non-flared annular section of the stent frame is designed to mitigate conduction system interference. Portico received a European CE Mark approval in December 2013 and currently, the US IDE Portico trial is underway. The first US implants were conducted on opposite coasts with our site at Lenox Hill Hospital in New York City and the other site at Cedars-Sinai Heart Institute in Los Angeles.
Alternative Transcatheter Heart Valve Designs
Complications with the early generation THV have initiated novel THV designs. The Sadra Lotus valve (Boston Scientific, Natick, MA) consists of a nickel-titanium stent with bovine percicardial leaflets (Fig. 1). This THV has a unique mechanical deployment mechanism whereby the valve is elongated for loading but undergoes phased mechanical compression during deployment that results in a decrease in axial length, but increase in diameter and rigidity. It is fixed in place by a locking mechanism and generates significant radial force securing the valve within the annulus. A bovine pericardial cuff around the inflow allows conformation to the annulus, reducing potential for PVL. The 23- and 27-mm valves are loaded into an 18-F delivery system and can be fully repositioned and resheathed.
Early trial data from the CE mark Repositionable Percutaneous Replacement of Stenotic Aortic Valve Through Implantation of Lotus Valve System—Evaulation of Safety and Efficacy (REPRISE) II trial revealed reasonable device efficacy and safety with the ability to successfully reposition and retrieve without issue and with low rate of PVL, approximately 11 % having moderate or severe regurgitation at 30 days [23]. Pacemaker implantation rates were similar to that reported for the self-expanding THV, around 28 %. Although 41 % of implanted patients had ≥10 % oversizing, future availability of additional valve sizes may reduce annular overstretch and overall need for pacemaker.
The Direct Flow THV (Direct Flow Medical, Santa Rosa CA) is a bovine pericardial valve and, unlike all of its predecessors, is made entirely from a non-metallic framework. It relies on sequential inflation of dual rings, ventricular followed by aortic, to anchor the prosthesis to the native annulus. The rings are interconnected by a tubular bridge made from a noncompliant angioplasty balloon technology and covered with a dacron polyester fabric cuff. Positioning is first tested with a saline/contrast mixture that is subsequently replaced with an epoxy polymer that hardens in situ. The valve is fully repositionable prior to final polymer injection. Early data have demonstrated reasonable efficacy and safety with only 1.4 % having moderate or severe PVL. Overall pacemaker implantation rate was intermediate at 17 % [24].
Sutureless, Rapid Deployment Heart Valves
Sutureless aortic valves (SU-AVRs) present a new dimension for patients with severe AS, although still in its infancy. SU-AVRs are self-expanding aortic valves but instead of utilizing an entirely percutaneous approach, the hybrid procedure for implantation combines aspects of both surgical and THV with a novel rapid-deployment technique [1]. Although a nitinol stent frame is used to anchor the valve within the native annulus, either a partial or full sternotomy with cardiopulmonary bypass (CPB) is required. Traditional SAVR requires long aortic cross-clamp time in conjunction with the use of CPB; it is known that these two factors are independent predictors of survival after valve replacement and combined valve with coronary artery bypass surgery [4, 25]. However, the advantages of SU-AVRs over traditional SAVR are that cross-clamp and CPB times are significantly reduced and surgical excision of the native valve is performed with decreased incidence of PVL. Compared to percutaneous THV, SU-AVR is associated with less compression of the prosthetic leaflets in the delivery system [1, 4, 26–29]. Two SU-AVRs are under investigation: Perceval S valve (Sorin Group, Saluggia Italy) and Intuity (Edwards Lifesciences, Irvine California) (Fig. 1). There are currently no randomized trials comparing SU-AVRs to TAVRs.
The Perceval S valve is a modified version of the Sorin Pericarbon surgical valve, known for improved transvalvular gradients and increased orifice areas. Perceval S is constructed of a bovine pericardial valve mounted on a self-expanding nitinol frame that is comprised of an inflow ring, which is deployed within the native annulus, and an outflow ring that sits at the level of the sinotubular junction [1]. The delivery system loaded with the compressed stent mounted valve is guided to its correct position by sliding it over three guiding sutures connected to the annulus. The sutures are stitched through the annulus and removed after valve placement [4]. Once the valve is deployed, a balloon is then inserted and expanded for 30 s at a pressure of approximately 3 atm. Mean cross-clamp and CPB times are approximately 40 and 70 min, respectively, with a minimal 2 % incidence of moderate or severe PVL and low post-operative gradients [30, 31].
The second of the SU-AVRs is the Intuity valve. This valve is the combination of the two Carpentier-Edwards valves: the Carpentier-Edwards Perimount and Edwards THV. Intuity consists of a bovine pericardial bioprosthesis, delivery system, and balloon catheter which is used to deploy the valve [32]. Like the Perceval S, the diseased valve is excised and three equidistant guiding sutures are placed through the nadir of the aortic annulus and then placed in the corresponding positions through the sewing ring. The valve and the delivery system are lowered and secured onto the annulus. The balloon catheter is inflated to 3 atm to deploy the stent frame, the delivery system then removed, and the three guiding sutures tied to the new valve. Data from Treatment of Aortic Stenosis with a Next Generation Surgical Aortic Valve (TRITON) study revealed cross-clamp times of 41 min, <1 % moderate or severe PVL, and excellent hemodynamic performance up to 1 year [32].
Advanced Fusion Imaging for Planning and Guidance
The integration of multimodality imaging with fluoroscopy in the catheterization laboratory, fusion imaging, provides an alternative to traditional fluoroscopically guided catheterization. Like other transcatheter interventions, it has the potential for TAVR to improve procedural efficacy and safety, while reducing radiation exposure, contrast volume requirements, and procedural duration. Fusion imaging relies on the utilization of 3 dimensional (3D) data acquisition from computed tomography (CT) and/or transesophageal echocardiography (TEE). This 3D data is merged with live fluoroscopy to generate a 3D cardiac model, while preserving the spatial and temporal resolution essential from fluoroscopy. The fundamental features of fusion imaging for TAVR include the localization of aortic valve anatomy, determination of appropriate THV size, identification of optimal X-ray projections for implantation, and guidance during deployment.
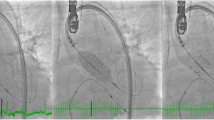
The HeartNavigator system (Philips Healthcare, Best Netherlands) is a proprietary software available for computed tomography-fluoroscopy fusion imaging in TAVR and utilizes the pre-procedural cardiac CT images [33, 34] (Fig. 2a–c). Pre-procedural 2D images are 3D volume-rendered and automatically segmented to identify the aortic root, coronary ostia, the aortic valve, the left ventricle, and the valve plane running through the bottom of the three cusps [35–37]. After segmentation, X-ray projections are planned by positioning a simulated X-ray view based on 3D-rendered images with the same perspective as that of the fluoroscopic c-arm. Views are selected such that the fluoroscopic image is in line with the valve plane. Aortic measurements and overlay of a virtual THV are then performed prior to implantation. Next, the CT images are registered with fluoroscopy and an outline of the cardiac structures with landmarks are subsequently overlayed onto the live fluoroscopic image to guide TAVR implantation.
a Computed tomography (CT)-fluoroscopy fusion imaging (Philips Healthcare, Best Netherlands) utilizes the pre-procedural CT images and volume-renders and automatically segments the aortic valve (green), aortic root/aorta with coronary arteries and bypass grafts (orange), and left ventricle (blue). b Generation of a valve plane running through the bottom of the three cusps is generated (yellow line) and appropriate c-arm angulations for implant determined. A virtual CoreValve is implanted to simulate size, implantation depth, and orientation. c CT overlay onto live fluoroscopy is shown for guidance during transcatheter heart valve implantation. d Transesophageal echocardiography (TEE)-fluoroscopy fusion imaging (Philips Healthcare) registers the TEE field of view with fluorosocopy. Landmarks placed, such as the annular plane (yellow circle) and left coronary artery (purple marker), are overlayed onto live fluoroscopy for additional guidance
Furthermore, the EchoNavigator system (Philips Heathcare, Best Netherlands) is a proprietary software available for echo-fluoroscopy fusion imaging [38] (Fig. 2d). It enables the echocardiographer and interventionalist to merge live 3D TEE data with fluoroscopy. The software automatically registers the TEE field of view in reference to the probe face plate onto fluoroscopy. The free view feature allows the operator to move the echocardiographic image in any direction while keeping track of a virtual fluoroscopic c-arm orientation and, thereby, determine the appropriate implant view. Like the HeartNavigator system, landmarks can be placed to identify the coronary ostia and aortic annular plane. The landmarks are first placed using 2D x-plane image then confirmed in a 3D view. Once accepted, they are subsequently overlayed onto fluoroscopy to guide TAVR implantation.
Conclusion
TAVR technologies have evolved significantly over the last 14 years since the first THV implantation in 2000. Initial balloon-expandable and subsequent self-expandable valve designs have demonstrated efficacy and safety. Significant advances made with newer generation devices suggest decreased complications: reduction in delivery system and sheath size improves the rate of vascular complications, application of skirt/cuffs minimizes the rate of paravalvular leaks, and reduction in outflow tract forces decreases rate of pacemaker implantation. Now, repositionable and retrievable devices are available to ensure appropriate implantation depth and results prior to final release. Alternative mechanisms of deployment have emerged and are being studied along with the hybrid sutureless valves that apply transcatheter technologies to open SAVR. Finally, advancements in fusion imaging have allowed the merging of multiple imaging modalities, CTA and TEE, with fluoroscopy for procedural planning and guidance. These described TAVR technologies, along with others soon to come, will continue to broaden our ability to treat this complex patient population.
References
Kumar R, Latib A, Colombo A, Ruiz CE. Self-expanding prostheses for transcatheter aortic valve replacement. Prog Cardiovasc Dis. 2014;56:596–609.
Stewart BF, Siscovick D, Lind BK, et al. Clinical factors associated with calcific aortic valve disease. Cardiovascular Health Study. J Am Coll Cardiol. 1997;29:630–4.
Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Thorac Cardiovasc Surg. 2014;148:e1–e132.
Flameng W, Herregods MC, Hermans H, et al. Effect of sutureless implantation of the Perceval S aortic valve bioprosthesis on intraoperative and early postoperative outcomes. J Thorac Cardiovasc Surg. 2011;142:1453–7.
Cribier A, Eltchaninoff H, Bash A, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description. Circulation. 2002;106:3006–8.
Cribier A, Eltchaninoff H, Tron C, et al. Early experience with percutaneous transcatheter implantation of heart valve prosthesis for the treatment of end-stage inoperable patients with calcific aortic stenosis. J Am Coll Cardiol. 2004;43:698–703.
Webb JG, Chandavimol M, Thompson CR, et al. Percutaneous aortic valve implantation retrograde from the femoral artery. Circulation. 2006;113:842–50.
Kapadia SR, Tuzcu EM, Makkar RR, et al. Long-term outcomes of inoperable patients with aortic stenosis randomized to transcatheter aortic valve replacement or standard therapy. Circulation. 2014;130:1483–92.
Kodali SK, Williams MR, Smith CR, et al. Two-year outcomes after transcatheter or surgical aortic-valve replacement. New Engl J Med. 2012;366:1686–95.
Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. New Engl J Med. 2011;364:2187–98.
Genereux P, Head SJ, Van Mieghem NM, et al. Clinical outcomes after transcatheter aortic valve replacement using valve academic research consortium definitions: a weighted meta-analysis of 3,519 patients from 16 studies. J Am Coll Cardiol. 2012;59:2317–26.
Mussardo M, Latib A, Chieffo A, et al. Periprocedural and short-term outcomes of transfemoral transcatheter aortic valve implantation with the Sapien XT as compared with the Edwards Sapien valve. JACC Cardiovasc Interv. 2011;4:743–50.
Binder RK, Rodes-Cabau J, Wood DA, Webb JG. Edwards SAPIEN 3 valve. Euro Interv. 2012;8(Suppl Q):Q83–7.
Binder RK, Rodes-Cabau J, Wood DA, et al. Transcatheter aortic valve replacement with the SAPIEN 3: a new balloon-expandable transcatheter heart valve. JACC Cardiovasc Interv. 2013;6:293–300.
Grube E, Laborde JC, Zickmann B, et al. First report on a human percutaneous transluminal implantation of a self-expanding valve prosthesis for interventional treatment of aortic valve stenosis. Catheter Cardiovasc Interv. 2005;66:465–9.
MacDonald I, Pasupati S. Transcatheter aortic valve implantation: know the differences between the currently available technologies. Eur Heart J. 2010;31:1663–5.
Popma JJ, Adams DH, Reardon MJ, et al. Transcatheter aortic valve replacement using a self-expanding bioprosthesis in patients with severe aortic stenosis at extreme risk for surgery. J Am Coll Cardiol. 2014;63:1972–81.
Adams DH, Popma JJ, Reardon MJ, et al. Transcatheter aortic-valve replacement with a self-expanding prosthesis. New Engl J Med. 2014;370:1790–8.
Piazza N, Martucci G, Lachapelle K, et al. First-in-human experience with the Medtronic CoreValve Evolut R. Euro Interv. 2014;9:1260–3.
Sinning JM, Werner N, Nickenig G, Grube E. Medtronic CoreValve Evolut R with EnVeo R. Euro Interv. 2013;9(Suppl):S95–6.
Willson AB, Rodes-Cabau J, Wood DA, et al. Transcatheter aortic valve replacement with the St. Jude Medical Portico valve: first-in-human experience. J Am Coll Cardiol. 2012;60:581–6.
Manoharan G, Spence MS, Rodes-Cabau J, Webb JG. St Jude Medical Portico valve. Euro Interv. 2012;8(Suppl Q):Q97–101.
Meredith Am IT, Walters DL, Dumonteil N, et al. Transcatheter aortic valve replacement for severe symptomatic aortic stenosis using a repositionable valve system: 30-day primary endpoint results from the REPRISE II study. J Am Coll Cardiol. 2014;64:1339–48.
Schofer J, Colombo A, Klugmann S, et al. Prospective multicenter evaluation of the direct flow medical transcatheter aortic valve. J Am Coll Cardiol. 2014;63:763–8.
Flameng WJ, Herijgers P, Szecsi J, Sergeant PT, Daenen WJ, Scheys I. Determinants of early and late results of combined valve operations and coronary artery bypass grafting. Ann Thorac Surg. 1996;61:621–8.
Basel R, Ramchandani M, Reardon M. Surgical approaches to aortic valve replacement and repair—insights and challenges. Interv Cardiol Rev. 2014;9:32–6.
Gaasch W, Brecker S, Aldea G. Transcatheter aortic valve replacement. UpToDate. 6/4/2014 ed: UpToDate, 2014.
Phan K, Tsai YC, Niranjan N, Yan TD, Di Eusanio M. Sutureless aortic valve replacement: a systematic review and meta-analysis. Ann Cardiothorac Surg. 2014. doi:10.3978/j.issn. 2225-319X.2014.06.01.
Brown JM, O'Brien SM, Wu C, Sikora JA, Griffith BP, Gammie JS. Isolated aortic valve replacement in North America comprising 108,687 patients in 10 years: changes in risks, valve types, and outcomes in the Society of Thoracic Surgeons National Database. J Thorac Cardiovasc Surg. 2009;137:82–90.
Miceli A, Santarpino G, Pfeiffer S et al. Minimally invasive aortic valve replacement with Perceval S sutureless valve: Early outcomes and one-year survival from two European centers. J Thorac Cardiovasc Surg 2014
Rubino AS, Santarpino G, De Praetere H, et al. Early and intermediate outcome after aortic valve replacement with a sutureless bioprosthesis: Results of a multicenter study. J Thorac Cardiovasc Surg. 2014;148:865–71.
Kocher AA, Laufer G, Haverich A, et al. One-year outcomes of the Surgical Treatment of Aortic Stenosis With a Next Generation Surgical Aortic Valve (TRITON) trial: a prospective multicenter study of rapid-deployment aortic valve replacement with the EDWARDS INTUITY Valve System. J Thorac Cardiovasc Surg. 2013;145:110–5.
Schrofel H, Bakker N, van der Boomen R. Transcatheter aortic valve implantation in a hybird operating room using HeartNavigator. Medicamundi. 2010;53:2–9.
Kliger C, Jelnin V, Sharma S, et al. CT angiography-fluoroscopy fusion imaging for percutaneous transapical access. JACC Cardiovasc Imaging. 2014;7:169–77.
Waechter I, Kneser R, Korosoglou G, et al. Patient specific models for planning and guidance of minimally invasive aortic valve implantation. Med Image Comput Comput Assist Interv. 2010;13:526–33.
Ecabert O, Peters J, Schramm H, et al. Automatic model-based segmentation of the heart in CT images. IEEE Trans Med Imaging. 2008;27:1189–201.
Peters J, Ecabert O, Meyer C, Kneser R, Weese J. Optimizing boundary detection via Simulated Search with applications to multi-modal heart segmentation. Med Image Anal. 2010;14:70–84.
Sundermann SH, Biaggi P, Grunenfelder J, et al. Safety and feasibility of novel technology fusing echocardiography and fluoroscopy images during MitraClip interventions. Euro Interv. 2014;9:1210–6.
Compliance with Ethics Guidelines
Conflict of Interest
Chad Kliger has received a speaking honorarium from St. Jude Medical, Philips Healthcare. Carlos E. Ruiz is a consultant for Valtech, St. Jude Medical, Sorin Medical, receives research grants from Philips Healthcare, and has financial interest in Vascular Therapies, MitrAssist, Entourage, and BioInspire. Gregory P. Fontana is a consultant for St. Jude Medical and receives research support from Medtronic and honoraria from Sorin Medical and Edwards. Dillon Weiss, Luigi Pirelli, and Vladimir Jelnin declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Coronary Heart Disease
Rights and permissions
About this article
Cite this article
Weiss, D., Ruiz, C.E., Pirelli, L. et al. Available Transcatheter Aortic Valve Replacement Technology. Curr Atheroscler Rep 17, 10 (2015). https://doi.org/10.1007/s11883-015-0488-7
Published:
DOI: https://doi.org/10.1007/s11883-015-0488-7