Abstract
Purpose of Review
Allergen immunotherapy (AIT) has been shown to be safe and effective in children and is a unique treatment strategy that has disease-modifying and preventative effects that are not shared with other treatment options for allergic diseases. This article reviews the present knowledge and relevant updates on AIT in children.
Recent Findings
Although there is no definite lower age limit for starting AIT, clear indications for AIT are established and each case should be considered individually by weighing risks and benefits. Documented short- and long-term benefits of AIT in children with allergic disease include significant improvement of symptoms and quality of life, and decreased use of medications as well as preventing the development of new allergen sensitizations and the progression of allergic rhinitis to asthma.
Summary
This review provides a comprehensive overview of the present knowledge and key updates on AIT in the pediatric population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is a high and increasing prevalence in pediatric allergic diseases such as allergic rhinitis, asthma, and atopic dermatitis (AD) [1]. Treatment strategies for these diseases include education on allergen-specific avoidance precautions, pharmacotherapy, and allergen immunotherapy. Allergen immunotherapy (AIT) has been a treatment for allergic disease for over 110 years and has been shown to be safe, effective, and a disease-modifying treatment for patients [2]. New data continues to emerge on benefits of AIT in young children, particularly on its role in preventing the development of asthma and new allergen sensitizations.
The aim of this article is to summarize the present knowledge and key updates for AIT in the pediatric population. This review is written to serve as a resource for healthcare providers managing allergic diseases in children.
Indications
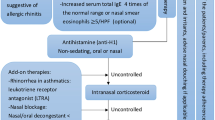
In general, the clinical indications for AIT are similar for adults and children [3]. AIT is indicated in patients with allergic rhinitis with or without conjunctivitis (AR/C), allergen-induced (allergic) asthma, or stinging insect hypersensitivity who demonstrate allergen-specific IgE antibodies diagnosed with skin prick testing or serum specific IgE laboratory testing [4]. A third practice parameter update for AIT was published in 2010 and described new indications for AIT, which includes atopic dermatitis (AD) in subjects with aeroallergen sensitization and for patients who experience recurrent bothersome large local reactions (LLR) to stinging insects [4]. Although immunotherapy for food allergy is available with one new US Food and Drug Administration (FDA)-approved product for peanut allergy (Palforzia, approved January 2020) and for many non-FDA oral immunotherapy protocols for other foods, subcutaneous immunotherapy (SCIT) and sublingual immunotherapy (SLIT) are not indicated for food allergy. For the purpose of this review, we will be discussing allergen immunotherapy regarding SCIT or SLIT.
Contraindications
Contraindications to AIT include inability to communicate and certain medical comorbidities. Severe systemic allergic reactions are a rare but possible risk of AIT [5, 6]. Contraindications to AIT involve considerations that would reduce a patient’s ability to survive a systemic allergic reaction or increase the risk of one [4].
There is no specific upper or lower age limit for initiating immunotherapy if the indications are present; however, the risks and benefits should be assessed carefully in each situation [4]. Patients selected for AIT should be mentally and physically able to communicate clearly any signs and symptoms suggestive of adverse reactions to the medical care team [4]. Age-related ability to communicate must be taken into consideration when weighing risks and benefits of AIT initiation in children. For this reason, there is some debate about initiating AIT in children less than the age of 5 years. Although the preventative effect of AIT on development of new aeroallergen sensitizations and the progressive march to asthma provides a benefit to beginning AIT earlier than age of 5 years, therefore, each case to begin AIT should be evaluated carefully by assessing the severity of disease and benefits/risks ratios [3, 4].
Allergen immunotherapy is not recommended for patients with uncontrolled labile asthma because of increased risk for systemic reactions to AIT injections in this population [4, 7, 8]. Survey studies revealed that mortalities from AIT were more frequent in persons with uncontrolled and/or labile asthma [8]. Therefore, asthma control needs to be achieved prior to initiating immunotherapy.
Other relative contraindications for AIT include medical conditions that reduce the patient’s ability to survive the systemic allergic reaction or the resultant treatment [4]. These medical conditions include heart disease, markedly compromised lung function, and conditions requiring beta-blockers and ACE inhibitors [4]. Although these comorbidities are less prevalent in children than adults, they are present. Caution should be used when considering initiating AIT in this population with a thorough evaluation of benefits and risks of immunotherapy.
Another special consideration that is more relevant to the adult population, but can also apply to pediatric age (< 18 yo), is immunotherapy in pregnancy. The AAAAI/ACAAI practice parameters state “allergen immunotherapy can be continued, but usually is not initiated in the pregnant patient.” The updated practice parameters also suggests that “discontinuation of immunotherapy should be considered if the pregnancy occurs during the buildup phase” as the dose during this phase is unlikely to be therapeutic [4].
Efficacy
Immunotherapy for children has been shown to be effective and well tolerated [3, 4]. Many clinical trials have shown that SCIT and SLIT are beneficial for allergic rhinitis and asthma by decreasing symptoms and medication use [9–11]. One study in children age 5–10 years showed that both SCIT and SLIT when compared to pharmacotherapy demonstrated a significant reduction of total rhinitis and asthma symptoms score, total medical score, and skin reactivity to house dust mite [10]. A randomized, double-blind, placebo-controlled study assessed efficacy of grass pollen immunotherapy in children 3–16 years old with a history of seasonal allergic asthma sensitized to grass pollen and requiring daily inhaled corticosteroid for asthma management [9]. In this study, the use of immunotherapy was associated with significant reduction in asthma symptom-medication score compared with placebo, and significant reductions in cutaneous, conjunctival, and bronchial reactivity to allergen after immunotherapy compared with that after placebo [9]. For atopic dermatitis, a double-blind, placebo-controlled study of 48 pediatric subjects with AD who received treatment to dust mite allergy with SLIT revealed a significant difference from baseline in visual analog scores, SCORAD scores, and pharmacotherapy utilization in the mild-to-moderate group; however, patients with severe AD had minimal benefit [4, 12]. One systematic review of AIT for AD showed significant improvement in symptoms in subjects with AD who received SCIT [13].
A retrospective study analyzing data from 107 children who had taken venom immunotherapy (VIT) from 2002 to 2015 concluded that VIT appeared to be safe and protective against severe reactions after future stings [14]. A 2012 Cochrane Review meta-analysis was performed to evaluate the effectiveness of VIT for preventing allergic reactions to insect stings [15]. The systematic review analyzed 7 randomized controlled trials which included 392 participants (children and adults) involving ant, bee, and wasp immunotherapy with previous systemic or large local reactions to a sting. The study revealed that VIT reduces the chances of having a serious allergic reaction to an insect sting by 90% and significantly improves quality of life of patients who have had serious reactions to insect stings by reducing anxiety and possible limitation of activities caused by fear of stinging insects [15].
Prevention
Preventative effects and disease-modifying treatment are unique characteristics of AIT that other treatment modalities for allergic disease do not possess. AIT might prevent the development of sensitivity to new aeroallergens in mono-sensitized children [16, 17••]. It has also been shown to decrease the possibility for later development of asthma in patients with AR/C [17••, 19••, 20]. Another study in 2017 concluded that AIT given for 3 years significantly decreased the risk of asthma in patients with AR with the greatest effect in children and for pollen AIT [18]. The effect was present up to 2 years after the end of treatment; however, no significant conclusion could be made in regard to a maintained effect over a longer duration [18].
Safety
Systemic Reactions
AIT is considered a safe treatment; however, there are adverse effects associated with AIT such as local and large local reactions (LLRs) and systemic reactions, including in rare cases anaphylaxis [4]. The majority of the severe systemic reactions will happen within 30 min after injection [5, 6]. SLIT has a better safety profile than SCIT because fewer systemic side effects and no deaths have been reported with SLIT [21, 22••]. One prospective study examined the safety of AIT in children less than 5 years of age and found there was one systemic reaction among 6,689 injections in 239 subjects. The authors concluded that specific immunotherapy in children younger than 5 years is a safe treatment [23].
Because almost all severe systemic reactions occur within 30 min after the injection, the practice parameters recommend a 30-min observation period after an injection at the medical clinic [4]. Injections for AIT should also be given in a setting where severe systemic reactions such as anaphylaxis will be quickly recognized and treated by the medical care team [4].
Local Reactions and Large Local Reactions
Local reactions are a common adverse effect of immunotherapy [24]. Seventy-one percent of the subjects in a survey study of 249 patients undergoing AIT reported experiencing a local reaction from their AIT [24]. Of those patients who reported local reactions, 96% stated they would not stop AIT because of the local reactions [24]. Individual local reactions are not predictive of future systemic reactions or having future local reactions [4, 24, 25]. However, some patients with a greater frequency of LLRs might be at an increased risk of future systemic reactions [26]. A retrospective large multicenter study compared the frequency of LLRs (defined as > 25 mm) in subjects who had experienced systemic reactions with age-, sex-, and allergen sensitivity-matched controls who had not had AIT-induced systemic reactions, which revealed that LLRs were increased fourfold in those who experienced a systemic reaction compared to those who had never experienced a systemic reaction [26].
Antihistamine Pretreatment/Epinephrine Prescription
Pretreatment with oral H1-antihistamines may be helpful for the management of AIT and might decrease the frequency of systemic reactions caused by AIT [4, 27]. One randomized controlled study showed that premedication with a second-generation H1-antihistamine leads to a reduction in the occurrence of severe systemic reactions caused by AIT [28]. For rush VIT protocols, pretreatment with H1-antihistamines has been shown to significantly decrease frequency of LLRs and systemic reactions [27, 29, 30].
First-line treatment of severe systemic reactions and anaphylaxis is administration of epinephrine [4]. Although the majority of severe systemic reactions with SCIT occur within 30 min of injection, there are cases that have occurred outside this time frame [6–8, 31••]. Patients and their legal guardians should be counseled on the risk of adverse reactions including severe systemic reactions during the informed consent process prior to initiating immunotherapy and educated on when to seek emergency medical attention. A study published in 2019 surveyed allergists on adverse reactions including systemic reactions of patients on SCIT from 2008 to 2016. This study demonstrated that prescribing epinephrine auto-injectors for SCIT does not appear to improve outcomes, possibly due to low rates of self-administration [31••]. The AAAAI/ACAAI practice parameters state that the decision to prescribe epinephrine auto-injectors to patients receiving SCIT should be at the physician’s discretion [4]. For United States FDA-approved SLIT tablets, auto-injectable epinephrine must be prescribed along with any SLIT tablet [22••]. The AAAAI/ACAAI practice parameters for SLIT recommend epinephrine (either an auto-injector or other form for self-injection) to patients receiving SLIT tablets [32].
Injection Limitations for Kids
Immunotherapy injections can be painful and traumatizing to pediatric patients who have a fear of needles. This may be a reason healthcare providers may attempt to limit the number of injections. There is little data that supports minimizing the quantity of AIT injections for patient comfort or therapy adherence. One study surveyed patients and the legal guardians of pediatric patients on their perceptions concerning the number of AIT injections given per visit [33]. In this study, the majority of pediatric subjects (21/38 [55.3%]) were willing to undergo 3 or more injections and indicated that “patients want to receive all clinically relevant allergens for their immunotherapy despite having to receive potentially more immunotherapy injections” [33]. Therapeutic dosing in polysensitized patients may mean 2–4 shots. Consequently, shared decision-making should be used when considering the number of AIT injections per visit [33].
Dosing/Labeling
The efficacy of SCIT recommended for aeroallergens is dependent on dosage. Specifically, effective SCIT correlates with the administration of an optimal maintenance dose in the range of 5–20 mcg of major allergen for inhalant allergens. Placebo dose SCIT has been delivered in many forms in the USA but best exemplified by Rinkel immunotherapy which was shown to be no more effective than a histamine placebo in influencing the weekly mean symptom, medication, and physical examination scores or lgE antibody levels [34].
For nonstandardized extracts, a suggested maintenance dose is “0.5 mL of a 1:100 or 1:200 wt/vol dilution of manufacturer’s extract” [4]. Effective doses have been defined in the AIT practice parameter [4]. How to practically use the recommended doses in the mixing lab has been proven to be confusing to the practicing allergist such that “math-free” guidelines have been published [35]. These authors have found these to also be cumbersome and offer the 10% rule as a simpler presentation of effective dosing to the practicing allergist.
The 10% rule is based upon four assumptions. First, a 1:20 w/v manufacturer’s vial is utilized as the source vial to create the red 1:1 v/v maintenance vial. Second, a maintenance dose of 0.5 mL of the 1:1 v/v red maintenance vial is injected into the patient. Third, cross-reactivity is taken into consideration such that non-cross-reactive tree, grass, weed, and/or mold mixes are not used. Fourth, cross-reactive allergens would either be in a manufacturer’s mix (e.g., boxelder/maple, sage/mugwort) or a single allergen selected to represent cross-reactive allergens used in skin testing (e.g., Timothy used for all the northern grasses). The 10% rule means that each allergen used in the maintenance vial is 10% of the volume of the maintenance vial.
There are three exceptions to the 10% rule. First, only 5% of the maintenance vial is required for standardized northern grasses (e.g., 0.5 mL of Timothy 100,000 BAU/mL in a 10 mL maintenance 1:1 v/v vial). Second, AP dog should be 15% of the maintenance vial. It is not possible to achieve a therapeutic dose with non-AP dog as it is so weak [36]. Third, standardized cat extract should be 20% of the maintenance vial. In summary, the 10% rule becomes 5–10-15–20 to include the 3 exceptions.
Venom Immunotherapy and Imported Fire Ant Immunotherapy
Immunotherapy is indicated for patients with stinging insect hypersensitivity who exhibit Hymenoptera-specific IgE antibodies [4]. The third update AAAAI/ACAAI practice parameters for immunotherapy state that “VIT might be effective in reducing LLRs that might cause significant morbidity and impair quality of life” [4]. For children who have experienced cutaneous-only reactions to Hymenoptera stings, immunotherapy may not be required. VIT is fundamentally like inhalant allergen immunotherapy, with a few unique features such as no associated increased incidence of systemic reactions with rush VIT compared to inhalant rush immunotherapy. Also, in patients who cannot safely discontinue beta-blockers but who have a history of moderate-to-severe systemic reactions to Hymenoptera insect stings, VIT may be initiated.
Utilizing whole-body extract, placebo dose VIT had unknowingly been used in the USA prior to 1978. The Johns Hopkins group demonstrated venom rather than whole-body extract was effective for the successful treatment of venom allergic patients [37]. In contrast, utilization of whole-body extract for imported fire ant (IFA) immunotherapy is effective using monthly maintenance doses of 0.5 mL of a 1:100 wt/vol concentration [38]. In the case of VIT, the optimal maintenance dose is 100 mcg for each venom [4].
Schedule
Generally, the initial AIT dose is 1,000- to 10,000-fold less than the maintenance dose. This excludes SLIT, where the starting dose is the maintenance dose. Immunotherapy schedules can be divided into two periods—the buildup and maintenance phase. The buildup phase entails administration of gradually increasing doses of a period of approximately 8 to 28 weeks. In conventional schedules, a single dose increase is given on each visit. The visit frequency can vary from 1 to 3 times per week. Utilizing cluster and rush schedules are another way to optimize options to enable the patient to achieve maintenance in fewer visits because these accelerated schedules entail administration of several injections at increasing doses on a single visit.
Dose adjustments may be needed in the event of systemic reactions or gaps in therapy; however, evidenced-based guidelines on dose adjustments during AIT have not been established. In the case of systemic reactions, many providers decrease the dose to one that was formerly tolerated or an even lower dose depending on the severity of the reaction. Careful increase in subsequent doses can be attempted if the patient is able to tolerate the reduced dose. For missed immunotherapy doses during the buildup phase or gaps in therapy, it is customary to reduce the dose of AIT extract [4].
Adherence
Adherence to AIT is affected by many factors such as the inconvenience frequent visits for injections, adverse side effects, and cost which are the foremost reasons for discontinuation [22••, 39]. The AAAAI/ACAAI practice parameters recommend that patients should be assessed every 6 to 12 months while they receive SCIT. We can infer a similar follow-up schedule for patients on SLIT. Considerations should be given for closer follow-up during the buildup phase of AIT with progressively longer intervals from 1-, 2-, 4-, and 6-month follow-up visits, and then routine 6-month follow-up visits [4, 22••]. Evaluation of clinical response to AIT, compliance, and medical history changes since previous visit should be addressed at follow-up visits.
Sublingual Immunotherapy
There are currently 3 FDA-approved SLIT formulations for the treatment of grass and ragweed allergy for pediatric patients (see Table 1) [40,41,42]. SLIT for house dust mite (ODACTRA) is available; however, it is not approved for patients under 18 years of age [43]. Safety and effectiveness of FDA-approved SLIT formulations have not been well-established for children < 5 years of age [40,41,42,43]. The AAAAI/ACAAI practice parameters for SLIT developed in 2017 do not endorse alternative formulations and preparations of SLIT, such as using liquid SCIT extract delivered sublingually or using of specific sublingual drops or other sublingual tablets as these products are currently not FDA-approved [32].
There is no induction/buildup period in North America or Europe for the Timothy grass (GRASTEK) or ragweed (RAGWITEK) SLIT [22••]. Year-round daily SLIT doses are 2800 BAU for Timothy grass and 12 Amb a 1 units for ragweed [22••, 40, 41]. For patients between 5 and 17 years, the induction schedule for the FDA-approved 5-grass SLIT (ORALAIR) is one 100 index of reactivity (IR) dose tablet on day 1, two 100 IR dose tablets on day 2, and one 300 IR dose tablet on day 3 [42]. The daily maintenance dose thereafter is 300 IR, which is equal to 9000 bioequivalent allergy units (BAU) [42].
Costs and Coding
A ten-injection buildup schedule through each vial with a 4-vial set would be 40 visits to maintenance. Achieving this with twice-weekly visits and maintenance injections every 2–6 weeks results in an average of 50 visits in the first year. This would be billed as 50 units of 95,165 for each injection. Though a patient on 4 injections would be 200 units, most insurance carriers limit annual doses to 150–160 units per year. However, in subsequent years 2–5, refills would be under the annual limits with 80 units per year (20 units per shot) assuming a 6-visit buildup after a 50% dose adjustment for a new vial and then another 14 visits over the remainder of the year with maintenance injections every 2–6 weeks. In summary, using effective doses results in excellent medical care with a sound business model.
Utilizing cluster schedules is another way to optimize options to enable the patient to achieve maintenance in fewer visits. As the cost of cluster injection visits (CPT 95,180) is seven times more expensive for the patient than a typical visit (CPT 95,115 and 95,117), insurance typically dictates whether this is an option for the patient. However, many carrier plans cover in a way that there is no additional cost to the patient. This is beneficial to the patient and a beneficial business model. When implementing cluster immunotherapy, offices must pre-check insurance before the initial visit and review treatment and cost with patient when consenting for SCIT. This author routinely offers three injection cluster visits (CPT 95,180 2 units) in the green 1:1,000 v/v vial and two injection cluster visits (CPT 95,180 1 unit) in the blue 1:100 v/v vial. This facilitates the patient getting through the first two vials in eight visits rather than twenty visits.
Special Considerations
Immunotherapy injections can be a challenge to administer due to needle fear in children and pain associated with injections. Strategies used to decrease needle phobia and increase adherence include child life consultants, age-appropriate distractions, and positive reinforcement with a reward system such as stickers and candy after each injection and/or transition to a new vial during buildup. A systematic review of 22 studies evaluated the effectiveness of psychological interventions for reducing vaccination pain and related outcomes in children and adolescents [44]. The review concluded that interventions such as verbal, video, music distraction, and breathing with a toy are effective interventions for reducing pain and pain-related outcomes during vaccine injections in children [44].
Conclusion
Allergen immunotherapy is safe and effective and should be considered in children with allergic disease. There is no specific lower age limit for initiating immunotherapy if indications are present [4]. Indications are AR/C, allergic asthma, and stinging insect hypersensitivity. The updated AAAAI/ACAAI practice parameters for AIT include AD in patients with aeroallergen sensitization and for patients who experience bothersome LLRs with venom stings [4]. Available forms of immunotherapy for children include SCIT and SLIT (not approved for age < 5 yo). Each case should be considered individually by weighing the risks and benefits. A special consideration to initiating immunotherapy at a younger age would be the preventative role AIT has on the development of new allergen sensitizations and development of asthma in patients with allergic rhinitis.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Christiansen ES, Kjaer HF, Eller E, Bindslev-Jensen C, Host A, Mortz CG, et al. The prevalence of atopic diseases and the patterns of sensitization in adolescence. Pediatr Allergy Immunol. 2016;27(8):847–53. https://doi.org/10.1111/pai.12650.
Jutel M, Agache I, Bonini S, Burks AW, Calderon M, Canonica W, et al. International consensus on allergy immunotherapy. J Allergy Clin Immunol. 2015;136(3):556–68. https://doi.org/10.1016/j.jaci.2015.04.047.
Finegold I. Immunotherapy: when to initiate treatment in children. Allergy Asthma Proc. 2007;28(6):698–705. https://doi.org/10.2500/aap.2007.28.3053.
Cox L, Nelson H, Lockey R, Calabria C, Chacko T, Finegold I, et al. Allergen immunotherapy: a practice parameter third update. J Allergy Clin Immunol. 2011;127(1 Suppl):S1-55. https://doi.org/10.1016/j.jaci.2010.09.034.
Cox L, Larenas-Linnemann D, Lockey RF, Passalacqua G. Speaking the same language: The World Allergy Organization Subcutaneous Immunotherapy Systemic Reaction Grading System. J Allergy Clin Immunol. 2010;125(3):569–74, 74 e1–74 e7. https://doi.org/10.1016/j.jaci.2009.10.060.
Tinkelman DG, Cole WQ 3rd, Tunno J. Immunotherapy: a one-year prospective study to evaluate risk factors of systemic reactions. J Allergy Clin Immunol. 1995;95(1 Pt 1):8–14. https://doi.org/10.1016/s0091-6749(95)70146-x.
Lockey RF, Nicoara-Kasti GL, Theodoropoulos DS, Bukantz SC. Systemic reactions and fatalities associated with allergen immunotherapy. Ann Allergy Asthma Immunol. 2001;87(1 Suppl 1):47–55. https://doi.org/10.1016/s1081-1206(10)62195-3.
Bernstein DI, Wanner M, Borish L, Liss GM, Immunotherapy Committee AAoAA, Immunology. Twelve-year survey of fatal reactions to allergen injections and skin testing: 1990–2001. J Allergy Clin Immunol. 2004;113(6):1129–36. https://doi.org/10.1016/j.jaci.2004.02.006.
Roberts G, Hurley C, Turcanu V, Lack G. Grass pollen immunotherapy as an effective therapy for childhood seasonal allergic asthma. J Allergy Clin Immunol. 2006;117(2):263–8. https://doi.org/10.1016/j.jaci.2005.09.054.
Eifan AO, Akkoc T, Yildiz A, Keles S, Ozdemir C, Bahceciler NN, et al. Clinical efficacy and immunological mechanisms of sublingual and subcutaneous immunotherapy in asthmatic/rhinitis children sensitized to house dust mite: an open randomized controlled trial. Clin Exp Allergy. 2010;40(6):922–32. https://doi.org/10.1111/j.1365-2222.2009.03448.x.
Yukselen A, Kendirli SG, Yilmaz M, Altintas DU, Karakoc GB. Effect of one-year subcutaneous and sublingual immunotherapy on clinical and laboratory parameters in children with rhinitis and asthma: a randomized, placebo-controlled, double-blind, double-dummy study. Int Arch Allergy Immunol. 2012;157(3):288–98. https://doi.org/10.1159/000327566.
Novak N. Allergen specific immunotherapy for atopic dermatitis. Curr Opin Allergy Clin Immunol. 2007;7(6):542–6. https://doi.org/10.1097/ACI.0b013e3282f1d66c.
Bussmann C, Bockenhoff A, Henke H, Werfel T, Novak N. Does allergen-specific immunotherapy represent a therapeutic option for patients with atopic dermatitis? J Allergy Clin Immunol. 2006;118(6):1292–8. https://doi.org/10.1016/j.jaci.2006.07.054.
Gur Cetinkaya P, Esenboga S, Uysal Soyer O, Tuncer A, Sekerel BE, Sahiner UM. Subcutaneous venom immunotherapy in children: efficacy and safety. Ann Allergy Asthma Immunol. 2018;120(4):424–8. https://doi.org/10.1016/j.anai.2018.01.015.
Boyle RJ, Elremeli M, Hockenhull J, Cherry MG, Bulsara MK, Daniels M, et al. Venom immunotherapy for preventing allergic reactions to insect stings. Cochrane Database Syst Rev. 2012;10:CD008838. https://doi.org/10.1002/14651858.CD008838.pub2.
Di Bona D, Plaia A, Leto-Barone MS, La Piana S, Macchia L, Di Lorenzo G. Efficacy of allergen immunotherapy in reducing the likelihood of developing new allergen sensitizations: a systematic review. Allergy. 2017;72(5):691–704. https://doi.org/10.1111/all.13104.
•• Gradman J, Halken S. Preventive effect of allergen immunotherapy on asthma and new sensitizations. J Allergy Clin Immunol Pract. 2021;9(5):1813–7. https://doi.org/10.1016/j.jaip.2021.03.010. Excellent overview of the preventative effect of allergen immunotherapy.
Kristiansen M, Dhami S, Netuveli G, Halken S, Muraro A, Roberts G, et al. Allergen immunotherapy for the prevention of allergy: a systematic review and meta-analysis. Pediatr Allergy Immunol. 2017;28(1):18–29. https://doi.org/10.1111/pai.12661.
•• Valovirta E, Petersen TH, Piotrowska T, Laursen MK, Andersen JS, Sorensen HF, et al. Results from the 5-year SQ grass sublingual immunotherapy tablet asthma prevention (GAP) trial in children with grass pollen allergy. J Allergy Clin Immunol. 2018;141(2):529–38 e13. https://doi.org/10.1016/j.jaci.2017.06.014. Study showing that grass immunotherapy reduced risk of asthma symptoms in children with grass pollen allergic rhinoconjunctivitis.
Polosa R, Li Gotti F, Mangano G, Paolino G, Mastruzzo C, Vancheri C, et al. Effect of immunotherapy on asthma progression, BHR and sputum eosinophils in allergic rhinitis. Allergy. 2004;59(11):1224–8. https://doi.org/10.1111/j.1398-9995.2004.00537.x.
Calderon MA, Simons FE, Malling HJ, Lockey RF, Moingeon P, Demoly P. Sublingual allergen immunotherapy: mode of action and its relationship with the safety profile. Allergy. 2012;67(3):302–11. https://doi.org/10.1111/j.1398-9995.2011.02761.x.
•• Tankersley M, Han JK, Nolte H. Clinical aspects of sublingual immunotherapy tablets and drops. Ann Allergy Asthma Immunol. 2020;124(6):573–82. https://doi.org/10.1016/j.anai.2019.12.025. Great overview of SLIT and formulations of SLIT.
Rodríguez Pérez N, Ambriz Moreno Mde J. Safety of immunotherapy and skin tests with allergens in children younger than five years. Rev Alerg Mex. 2006;53(2):47–51.
Coop CA, Tankersley MS. Patient perceptions regarding local reactions from allergen immunotherapy injections. Ann Allergy Asthma Immunol. 2008;101(1):96–100. https://doi.org/10.1016/S1081-1206(10)60841-1.
Calabria CW, Coop CA, Tankersley MS. The LOCAL Study: local reactions do not predict local reactions in allergen immunotherapy. J Allergy Clin Immunol. 2009;124(4):739–44. https://doi.org/10.1016/j.jaci.2009.07.048.
Roy SR, Sigmon JR, Olivier J, Moffitt JE, Brown DA, Marshall GD. Increased frequency of large local reactions among systemic reactors during subcutaneous allergen immunotherapy. Ann Allergy Asthma Immunol. 2007;99(1):82–6. https://doi.org/10.1016/S1081-1206(10)60626-6.
Wang L, Wang C, Lou H, Zhang L. Antihistamine premedication improves safety and efficacy of allergen immunotherapy. Ann Allergy Asthma Immunol. 2021;127(3):363–71 e1. https://doi.org/10.1016/j.anai.2021.05.023.
Ohashi Y, Nakai Y, Murata K. Effect of pretreatment with fexofenadine on the safety of immunotherapy in patients with allergic rhinitis. Ann Allergy Asthma Immunol. 2006;96(4):600–5. https://doi.org/10.1016/s1081-1206(10)63556-9.
Reimers A, Hari Y, Muller U. Reduction of side-effects from ultrarush immunotherapy with honeybee venom by pretreatment with fexofenadine: a double-blind, placebo-controlled trial. Allergy. 2000;55(5):484–8. https://doi.org/10.1034/j.1398-9995.2000.00520.x.
Brockow K, Kiehn M, Riethmuller C, Vieluf D, Berger J, Ring J. Efficacy of antihistamine pretreatment in the prevention of adverse reactions to Hymenoptera immunotherapy: a prospective, randomized, placebo-controlled trial. J Allergy Clin Immunol. 1997;100(4):458–63. https://doi.org/10.1016/s0091-6749(97)70135-0.
•• Epstein TG, Liss GM, Berendts KM, Bernstein DI. AAAAI/ACAAI Subcutaneous Immunotherapy Surveillance Study (2013–2017): Fatalities, Infections, Delayed Reactions, and Use of Epinephrine Autoinjectors. J Allergy Clin Immunol Pract. 2019;7(6):1996–2003 e1. https://doi.org/10.1016/j.jaip.2019.01.058. Study showing that prescribed epinephrine for SCIT does not affect outcomes of delayed systemic reactions.
Greenhawt M, Oppenheimer J, Nelson M, Nelson H, Lockey R, Lieberman P, et al. Sublingual immunotherapy: a focused allergen immunotherapy practice parameter update. Ann Allergy Asthma Immunol. 2017;118(3):276–82 e2. https://doi.org/10.1016/j.anai.2016.12.009.
Coop CA, Yip SK, Tankersley MS. Perceptions regarding injection number and technique. Ann Allergy Asthma Immunol. 2014;113(2):227–8. https://doi.org/10.1016/j.anai.2014.05.008.
Hirsch SR, Kalbfleisch JH, Golbert TM, Josephson BM, McConnell LH, Scanlon R, et al. Rinkel injection therapy: a multicenter controlled study. J Allergy Clin Immunol. 1981;68(2):133–55. https://doi.org/10.1016/0091-6749(81)90172-x.
Grier TJ, Converse LM, Rekkerth DJ, Renahan KE. Math-free guides for glycerin and allergens at variable subcutaneous injection volumes: How’s my dosing? Update Ann Allergy Asthma Immunol. 2016;116(5):455–60. https://doi.org/10.1016/j.anai.2016.02.015.
Nelson HS. Allergy immunotherapy for inhalant allergens: Strategies to improve efficacy. Allergy Asthma Proc. 2020;41(1):26–37. https://doi.org/10.2500/aap.2020.41.190013.
Hunt KJ, Valentine MD, Sobotka AK, Benton AW, Amodio FJ, Lichtenstein LM. A controlled trial of immunotherapy in insect hypersensitivity. N Engl J Med. 1978;299(4):157–61. https://doi.org/10.1056/NEJM197807272990401.
Freeman TM, Hylander R, Ortiz A, Martin ME. Imported fire ant immunotherapy: effectiveness of whole body extracts. J Allergy Clin Immunol. 1992;90(2):210–5. https://doi.org/10.1016/0091-6749(92)90073-b.
Pajno GB, Vita D, Caminiti L, Arrigo T, Lombardo F, Incorvaia C, et al. Children’s compliance with allergen immunotherapy according to administration routes. J Allergy Clin Immunol. 2005;116(6):1380–1. https://doi.org/10.1016/j.jaci.2005.07.034.
Ragwitek (Short Ragweed Pollen Allergen Extract Tablet for Sublingual Use): Full Prescribing Information. 2021. Accessed.
Grastek (Timothy Grass Pollen Allergen Extract Tablet for Sublingual Use): Full Prescribing Information. Whitehouse Station, NJ: Merck Sharp & Dohme Corp; 2021.
Oralair (Sweet Vernal, Orchard, Perennial Rye, Timothy, and Kentucky Blue Grass Mixed Pollens Allergen Extract Tablet for Sublingual Use): Full Prescribing Information. Antony, France: Stallergenes S.A.; 2021.
ODACTRA (House Dust Mite Allergen Extract Tablet for Sublingual Use): Full Prescribing Information. Hørsholm, Denmark: ALK-Abelló A/S; 2021.
Birnie KA, Chambers CT, Taddio A, McMurtry CM, Noel M, Pillai Riddell R, et al. Psychological interventions for vaccine injections in children and adolescents: Systematic review of randomized and quasi-randomized controlled trials. Clin J Pain. 2015;31(10 Suppl):S72-89. https://doi.org/10.1097/AJP.0000000000000265.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Phomakay: None. Dr. Tankersley: ALK (speaker/advisory board), Tankersley Healthcare Consulting (CEO), HollisterStier (advisory board).
Human and Animal Rights and Informed Consent
There were no human or animal subjects studied in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of Topical Collection on Immunotherapy and Immunomodulators
Rights and permissions
About this article
Cite this article
Phomakay, V., Tankersley, M. Allergen Immunotherapy in Young Children. Curr Allergy Asthma Rep 22, 93–99 (2022). https://doi.org/10.1007/s11882-022-01035-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11882-022-01035-0