Abstract
Purpose of Review
To evaluate the impact of allergic rhinitis (AR) on the development of asthma and to update readers on recent literature suggesting that early treatment of allergic subjects with immunotherapy may prevent asthma onset.
Recent Findings
AR is frequently associated with asthma, leading to the concept that these two conditions are different aspects of the same disease. There is increasing evidence that AR precedes the onset of asthmatic symptoms and current treatment strategies are beneficial in symptom control with no impact prevention. There is limited knowledge about the risk factors responsible for the progression of AR to asthma, though recent data supports the notion that it is possible to prevent asthma onset by allergen immunotherapy.
Summary
Despite significant advances in specific immunotherapy (SIT) therapy strengthening its efficacy in AR and possible prevention of progression to asthma, the adoption of this therapeutic strategy is still restricted in comparison to therapies directed towards treatment of AR symptoms. Unlike corticosteroids and other symptomatic therapies, the benefit of SIT treatment in allergic individuals has been shown to prevent the development of allergic conditions. Hence, large well-conducted randomized clinical trials with long-term efficacy of SIT are required to confirm or refute the concept that SIT may abrogate the progression of AR to asthma in patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of allergic rhinitis (AR) is increasing, affecting 10–40% of the global population. AR negatively impacts quality of life, school, and work performance and increases primary care frequency visits [1]. Cardinal symptoms of AR include nasal pruritus, sneezing, rhinorrhea, and nasal congestion, though may also be associated with ocular symptoms, itching of the palate, postnasal drip, and cough [1]. AR is frequently associated with asthma: found in 15–38% of the patients. Conversely nasal symptoms are present in 6–85% patients with asthma [1]. Hence, AR is considered a major risk factor for asthma onset, and uncontrolled moderate-to-severe AR can significantly affect asthma control.
It is known that allergic airway disease affects the mucosal lining and can span from the nose to lungs with a range of symptoms based on the location and its severity [2, 3, 4••, 5, 6]. The upper and lower respiratory tracts share the same anatomical, functional, pathogenic, clinical, and immunological features; with the latter including the same lymphoid network, thus reacting to airborne allergens by activating similar effector cells. These associations have been extensively studied and hence proposed that allergic airway disease represents a disease continuum occurring simultaneously [4••, 5]. Several prospective severe asthma studies have shown that subjects with an upper airway involvement reported more emergency room visits and an increased severity of respiratory symptoms [7, 8]. It seems that the effect of AR on asthma may be further enhanced by the coexistence of allergic eye symptoms (rhinoconjunctivitis) [9]. Therefore, the terms united airway disease, allergic rhinobronchitis, allergic respiratory disease (ARD), and/or combined allergic rhinitis and asthma syndrome (CARAS) have been advocated by various researchers [1, 4••, 5, 10, 11]. From these studies is an emerging evidence proposing that clinical manifestations are heterogeneous, with a clinical profile often related to the individual airborne allergens [10].
Additional data confirming the combined allergic airway paradigm is derived from observation during nasal allergen challenges inducing bronchial inflammation/hyperresponsiveness (BHR) [12, 13] and conversely during segmental bronchial provocation the induction of nasal inflammation in AR subjects without asthma [14]. In a study of non-asthmatic AR subjects, it was noted that > 8% of the 605 subjects enrolled had an attenuated FEV1 and impaired small airway assessment. Moreover two thirds of the cohort had a positive bronchodilator reversibility [15]. In a recent prospective study, Di Cara and colleagues demonstrated that children with moderate-to-severe persistent AR developed new onset asthma at 5 years follow-up; and the development of asthma was noted in a third of the mild AR children, hence reinforcing the notion that the persistence of AR may be linked with progression of AR to asthma. This may be explained by the presence of persistent nasal inflammation which may be associated with the involvement of the lower airways with mucosal infiltration and lung function impairment [16]. Thus, the evidence suggests a strong relationship between allergic nasal disease and asthma with a prevalence that may be as high as 80% [17, 18].
In a study by Cirillo and colleagues [19•] in 200 AR subjects, fractional exhaled nitric oxide (FeNO) was noted to be increased in AR subjects with BHR, probably reflecting the extension of inflammation throughout the airways. This might reveal changes in the physical properties of bronchial mucosa that may be induced by the subclinical lower airway inflammation in AR.
There is a notion that the airways right from the nose to the lower respiratory tract are in continuum, and hence, atopic/allergic conditions may manifest as a result, especially in childhood (“The Allergic March”). Several studies suggest that AR (and/or atopic dermatitis) may predict progression to asthma both in children and in adults [1, 5, 6, 9, 17, 18, 20,21,22].
The Continuum of Rhinitis to Asthma on an Allergy Background
The prevalence of AR is increasing globally and frequently overlaps with asthma [23,24,25,26,27]. There is evidence in the literature that AR shares most of its mechanisms with asthma [28, 29]. In a recent study, a computational analysis of the molecular mechanisms underlying multi-morbidity between asthma, eczema, and rhinitis identified a number of proteins and cellular processes that were common to these atopic conditions [30•]. It was observed that asthma and rhinitis shared a large number of associated proteins that exhibited a significant degree of interconnection through the interaction network. Moreover, they found 15 pathways involved in the multi-morbidity of asthma, eczema, and rhinitis, including the IL4 signaling- and GATA3-related pathways. In particular, the authors observed 196 proteins associated with asthma and 40 with rhinitis (of which only 163 and 32 are associated to functional interaction networks in asthma and AR, respectively). The number of proteins associated with both asthma and rhinitis was 35. Among these proteins, there were a number of members of HLA-DRB and HLA-DQ families, which have roles in T cell activation and in the development of an IgE response. More than 90% of the functional connections belonging to rhinitis associated proteins were shared with asthma, and the topological overlap between proteins common to a combination of asthma and rhinitis was significantly larger than random expectation (z-test, P < 0.01). Moreover, the authors identified individual pathways that may be linked to the multi-morbidity between asthma, eczema, and rhinitis. Assuming that the cellular pathways were significantly perturbed by two or three of the diseases were more likely candidate mechanisms for multi-morbidity, three pathways showed a significant overlap score between asthma and AR: IL 4 signaling pathway, GATA3 participates in activating the Th2 cytokine genes expression, and the 4-IBB-dependent immune response [30•, 31]. The cellular pathways observed to be involved in both the airway diseases can potentially explain the subclinical background inflammation in the lower airways of a number of AR subjects [32], which could represent a prominent risk factor for progression from AR to asthma [6, 33]. These findings may represent the molecular basis of the overlap phenomenon that has been observed in clinical studies, about the nasal provocation challenges resulting in significant BHR despite the absence of asthma symptoms, in particular phenotype clusters of AR patients [20, 30•, 33].
Recent studies have aimed to define clusters of rhinitis in order to differentiate subphenotypes of AR patients. In a prospective cohort study of a general population of school-aged children followed up at 2 and 4 years, the researchers investigated the development of new cases of BHR and asthma symptoms [20]. Four distinct rhinitis clusters were identified by latent class analysis that used demographic, clinical, and environmental variables. Two of these clusters were characterized by high prevalence of atopy with differences in lung function (normal vs. impaired lung function). The other 2 clusters had low or very low prevalence of atopy with normal vs. impaired lung function. The highly atopic cluster with impaired lung function had a significantly higher prevalence of BHR at the time of enrollment and was associated with an increased prevalence of newly developed BHR and asthma symptoms during follow-up at 2 and 4 years, thus indicating that this cluster may represent an allergic march-associated rhinitis phenotype. The underlying pathophysiological mechanism of both AR and BHR involves bidirectional interactions between the nose and the bronchi [6, 20, 34, 35]. In a prior study by Burgess and colleagues, it was reported that the presence of childhood eczema increased the risk of new-onset asthma (OR 4.1), and rhinitis alone predicted the persistence of childhood asthma to topic asthma (OR 2.7) [35]. Similarly, in a 10-year retrospective assessment of 300 Italian subjects, a diagnosis of AR was significantly and independently predictive of developing asthma (OR 7.80) [36]. Of note, there were no differences in the use of topical corticosteroids in the AR subjects developing asthma symptoms compared to those who did not.
Importantly, data from epidemiological studies need to be interpreted with caution as they may have limitations of interpretation bias; this is due to the fact that these epidemiological studies are based on written questionnaires for the diagnoses of AR and asthma. Additionally, some of the treatments for the management of AR may mask the developing symptoms of asthma reducing the accuracy of the diagnosis. Prospective epidemiological studies have substantiated the progression of rhinitis to asthma [37,38,39]. A prospective, open-labeled, multi-center European study of 205 children with grass- and/or birch-induced rhinoconjunctivitis randomized to specific immunotherapy (SIT) or not reported that compared to children receiving SIT, those not on SIT had an OR of 2.68 more symptoms consistent with asthma [37]. Similar observations were noted 2 years later in the same cohort assessed [40].
Predictors for the Progression from Rhinitis to Asthma
Repeated exposure to inhaled antigens with potent allergenic properties may predispose the advancement of the AR towards asthma [41]. House dust mite (HDM) has been implicated in the development of asthma [42,43,44]: probably due to its great diffusion in the environment and its high allergy prevalence [45]. Moreover HDM allergens are able to activate TH2 cells that stimulate the production of specific IgE as well as the recruitment of inflammatory cells leading to structural changes in the lung and nose over time [46]. In a retrospective Italian study, surprisingly HDM sensitization was not markedly predictive of the onset of asthma (OR 1.33), though sensitization to Parietaria judaica was (OR 4.26) [36]. These discrepancies may reflect the inhaled allergen characteristics determined by geographic location where the studies were conducted. Interestingly, the duration of rhinitis did not predict the development of asthma. Female gender and the presence of BHR in rhinitis patients have been observed as risk factors for the onset of asthma [47, 48]. The former may be attributed to hormonal modifications [47]. Except for one retrospective study, the increased predisposition for the development of asthma in female patients with AR (OR 2.83) [36] has not been studied as a relevant factor.
Cigarette smoke exposure is another important factor in the development of asthma, with a strong association of asthma and wheezing in childhood with maternal and household smoking [49,50,51,52]. In a study by Polosa and colleagues, in non-asthmatic subjects with AR, smokers had an enhanced odds (OR 2.98) of developing asthma compared to non-smokers [53]. Additionally, the risk of asthma onset was more marked in individuals with more smoking exposure as assessed by pack years of smoking.
It is known that inflammatory changes may be present in the lower airways of non-asthmatic AR patients [23,24,25], which may ultimately result in the progression to asthma. Persistent exposure to inhaled allergens in addition to cigarette smoke may have a synergistic effect in the inflammatory processes. Cigarette smoke is composed of a complex mixture of solid particles and gases; in vivo studies showed that polyaromatic hydrocarbons in tobacco smoke induce TH2 immune responses, thus promoting allergic inflammation [54, 55], including synthesis of allergen-specific IgE antibodies and IgE-mediated allergic conditions such as AR and asthma in sensitized individuals [56, 57]. Hence, smoking AR patients may even be more likely to progress to asthma. Additionally, BHR is well recognized in asthmatic patients with rhinitis [12, 14, 20] and is also strongly associated with smoking [53]. This may explain the increased incidence of new onset asthma in smoking rhinitis patients.
It has been suggested that patients with AR and BHR are at higher risk of developing asthma. Moreover, some recent studies have highlighted that FeNO in AR subjects is highly correlated with the degree of BHR [58, 59]. These discoveries have raised clinical and scientific interest in FeNO as a biomarker in AR patients with BHR. This emphasizes the close link between upper and lower airways. Hence, increased FeNO in subjects with AR may be a useful indicator of the risk for developing asthma [19•].
Recent studies have focused their research on epigenetic regulation and particularly on the modulation of inflammatory processes by microRNAs (miRNAs). Panganiban and colleagues showed a subset of 10 circulating miRNAs (miR-26b, miR-29, miR-133a, miR-133b, miR-330-5p, miR-144, miR-145, miR-422, miR-1248, and miR-1291) that was similarly deregulated in patients with AR and asthma [60]. As such, this identified subset is indicative of the common pathway involved in AR and asthma. In a more recent study, it was showed that Chinese AR patients with SNP rs2292832 in miR-149 have an increased risk of asthma [61].
Another biomarker of AR that could be very helpful in monitoring immunotherapy efficacy could be miR-146a. An altered expression of this molecule in the PBMCs of AR children was associated with Foxp3 expression and disease severity suggesting that miR-146a may be involved in the insufficiency of Treg cells for AR pathogenesis. Luo and colleagues recently reported that in HDM-sensitized children (n = 24) with persistent AR treated with SIT (both SCIT and SLIT), miR-146a expression level in peripheral blood mononuclear cells increased significantly, in addition to Foxp3 mRNA production (P < 0.01) [62]. It seems that miR-146a exerts an important control on the suppressor function of Treg cells [63]. These studies suggest that miR-146a might play a role in SIT by modulating Treg cells.
Management Strategies for the Prevention of AR to Asthma
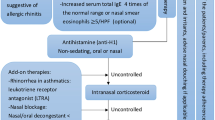
Besides environmental control measures and allergen avoidance, the management of AR consists of pharmacological management and SIT. It is recognized that AR may progress to the onset of asthma; hence, appropriate treatment of the underlying inflammation, although mild, is imperative. A number of approaches are under consideration, as reported by the ARIA guidelines, to manage and reduce symptoms; however, these are limited to a combination of oral and intranasal H1-antihistamines, intranasal corticosteroids, and leukotriene receptor antagonists [1]. The evidence base for these combined pharmacological approaches is strong, but they are intended only to control the symptoms of AR. To date, the only treatment option to abrogate respiratory symptoms and background allergic/immunological features is SIT. By targeting the underlying etiology, SIT can modify the prognosis of allergic conditions, especially AR, hence should be considered a valuable first-line treatment strategy which may prevent the development of asthma as well [64, 65].
In the following sections, we will discuss the postulated mechanism(s) of action of SIT and its specific role with regards to prevention of disease progression from AR to asthma.
Specific Immunotherapy—Mechanism of Action
The mechanism of action of SIT is not fully understood, yet. It is, however, based on the understanding that repeated allergen exposure in allergic individuals results in immune tolerance by attenuating the sensitivity to the offending allergen. It is widely accepted that tolerogenic dendritic cells, processing allergens as small peptides, mediate several modifications of the cellular and humoral immune response during the course of SIT administration [66,67,68,69] (Fig. 1). The immunological manifestations of SIT in long-term desensitization are initiated by functional regulatory T (Treg) cells that shift the TH1/TH2 cell balance in favor of TH1 milieu [66,67,68].
Immunologic responses of specific immunotherapy. Specific immunotherapy (SIT) triggers various mechanisms that work simultaneously to lead to allergen desensitization and suppression of allergic inflammation. The Th1/Th2 cytokine ratio is increased following SIT. Monocytes, macrophages, lymphocytes B, and T increased the production of interleukin-10 (IL-10). SIT induces a shift in the proportion of IL-4-secreting Th2 cells in favor of inducible IL-10-secreting T-regulatory cells (T-reg) that increase in number and function. IL-10, together with transforming growth factor-β (TGFβ), contribute to T-reg function and immunoglobulin class switching to IgA, IgG1, and IgG4. These blocking antibodies compete with IgE for allergen binding and suppress IgE production. In addiction, there are suppressive effect on mast cells, basophils, and eosinophils. Images of cells by Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014.” WikiJournal of Medicine 1 (2). DOI: https://doi.org/10.15347/wjm/2014.010. ISSN 2002-4436
SIT, unlike standard symptomatic therapies, has the potential to regulate underlying allergic mechanisms and may have a relevant role in reducing or preventing the progression of AR to asthma and new sensitizations. Also, SIT in susceptible individuals may halt immune processes to asthma progression rather than dampening the immune response once asthma is established [70, 71].
Clinical Evidence of the Role of SIT in Preventing Progression from AR to Asthma
For more than a decade, retrospective studies have demonstrated that in monosensitized individuals, SIT dramatically attenuates the onset of new sensitizations [72,73,74]. Studies have reported that 75–97% of the SIT-treated AR subjects compared to 35–53% of the AR subjects not treated with SIT had no new sensitizations [75, 76]. The most robust evidence for SIT efficacy in attenuating the onset of asthma stems from the Preventive Allergy Treatment (PAT) study [37, 38, 40]. In this open-labeled, randomized study, subcutaneous SIT was administered in 205 children and followed up to 10 years post-treatment completion. Besides sustained improvements in AR symptoms over the 10-year period, significantly fewer children developed asthma in the SIT-treated group at 3 (OR 2.52), 5 (OR 2.68), and 10 years (OR 2.5) of treatment initiation [37, 38, 40]. Additionally, it was reported that there was a longitudinal treatment effect (adjusting for baseline BHR and asthma) over the 10-year period (p = 0.0075) [38]. Further evidence of the positive effects of SIT in halting AR progression to asthma has been demonstrated in longitudinal and case-control studies [36, 77,78,79].
A prospective randomized controlled trial of 48 children with mild persistent asthma with/without rhinitis, monosensitized to HDM and treated with HDM-SCIT (n = 14), HDM-SLIT (n = 15), and pharmacotherapy alone (n = 14) was followed for 3 years for subjective and objective asthma and AR parameters [80•]. At 3 years, it was noted that there was a significant reduction in asthma symptoms in SIT-treated groups, a marked improvement in rhinitis symptoms and general improvements in total symptom score compared to baseline and controls. Medicine intake (p = 0.01) and skin reactivity to HDM (p < 0.05) were also dramatically attenuated compared to baseline and to the control group. Overall, although a sustained clinical improvement was observed in children treated by SIT (both SCIT and SLIT), only SCIT-treated (and not SLIT) children had a significant increase in HDM-specific IgG4 at 3 years follow-up.
Results from the GRAZAX Asthma Prevention (GAP) study have been recently published [81]. This was a 5-year double-blind, placebo-controlled, parallel-group randomized study in 802 children with grass pollen-induced allergic rhinoconjunctivitis and allergic asthma. The primary objective was to investigate the effect of the grass sublingual immunotherapy tablet (GRAZAX 75,000 SQ-T/2,800 BAU, ALK, Hørsholm, Denmark) compared to the placebo on the risk of developing asthma. SLIT significantly attenuated the risk of asthma onset or the use of asthma medication by the end of trial (OR0.66; p < 0.036), during the 2-year post-treatment follow-up, and during the entire 5-year trial period. Moreover, allergic rhinoconjunctivitis symptoms were markedly reduced (p < 0.005 for all 5 years) and so were the total IgE, grass pollen-specific IgE, and skin prick test reactivity to grass pollen compared to the placebo. Importantly, despite the clinically significant effects shown previously, SLIT did not show an effect on the time of onset of symptoms related to asthma in respect to the placebo group [81].
Although SIT may potentially prevent new sensitizations and the development of asthma in AR subjects, it is important to acknowledge that the overall quality of the current evidence is suboptimal. Well-conducted, large, long-term follow-up double-blind, placebo-controlled randomized studies are necessary. Theoretically, with the availability of more practical SIT formulations (e.g., tablet sublingual SIT, aqueous sublingual SIT, enteric and microencapsulated SIT preparations), which are more practical to administer and randomize, it will be simpler to design and implement such studies.
In recent years, different meta-analysis and systematic reviews have been published to assess the efficacy of SIT in preventing new allergic sensitization and/or asthma onset in allergic subjects [83, 84]. In a recent systematic review of 18 studies (1049 children and 10,057 adults), it was reported that there was low-grade evidence supporting the assumption that SIT prevents the onset of new allergen sensitizations, with 10 of 18 studies reporting a reduction in the onset of new sensitizations in patients treated with SIT compared to the placebo. Of note, small studies and studies with a shorter follow-up have demonstrated the highest benefit of SIT [84].
However, another systematic review and meta-analysis on 32 studies analyzing the safety, clinical and cost-effectiveness, and safety of SIT reported a reduction in the short-term risk of AR subjects undergoing SIT in developing asthma (RR = 0.40); though there was lack of conclusive evidence for longer term benefit for this outcome (RR = 0.62) [85•]. Additionally, SIT seemed to reduce the risk of new sensitizations over the short term; however, the sensitivity analysis remains debatable (RR = 0.72). There was no clear evidence of any longer-term reduction in the risk of sensitization (RR = 0.47). Also, controversially, no conclusive evidence of AIT decreasing the risk of manifesting the first allergic condition in the short or long term was noted [85•].
In a systematic overview of systematic reviews, Nurmatov and colleagues noted moderate-to-strong evidence that SIT administered to appropriately selected allergic rhinoconjunctivitis patients is effective in reducing symptoms and medication use. However, the authors suggested caution in interpreting these data due to the heterogeneity in the populations, allergens, and protocol a (e.g., SCIT vs. SLIT) [83]. An important consideration is the limitation of data/outcomes of meta-analyses. They may be subject to a variety of biases, e.g., incorrect selection of trials, inappropriate use of evaluation parameters for the analysis, and unsuitable analyses [86]. For instance, a meta-analysis of several small studies does not predict the results of a single large study that remains the gold standard to assess the efficacy and safety of a treatment. Therefore, when evaluating the results from meta-analyses, one must keep in mind these limits and observe carefully the selection criteria of individual studies and the statistical models used for the data analysis.
Conclusions
Although there have been significant advances in SIT therapy with clinical trials revealing its efficacy in AR and possible reduction in progression to asthma [87, 88], the adoption of this therapeutic strategy is still restricted in comparison to therapies addressing AR symptoms. This may be explained by lack of awareness of the clinical benefits of SIT, its safety profile, the multiple routes of administration of currently available SIT formulations, a greater experience with conventional symptomatic medications, or due to SIT short-term exorbitant costs. Conversely, evidence suggests that in pre-school children at a high risk for developing asthma, early anti-inflammatory therapy with inhaled corticosteroids has little impact on the natural course of the disease [89,89,91]. Unlike corticosteroids and other symptomatic therapies, in at-risk individuals, the benefit of SIT in the treatment of allergic individuals has been shown to prevent the development of allergic conditions. Hence, taking into consideration that the studies described in the literature presently are largely observational or uncontrolled, large well-conducted randomized clinical trials with long-term efficacy of SIT, irrespective of the route of administration, are required to confirm or refute the concept that SIT may abrogate the progression of AR to asthma in patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bro JL, Bousquet J, Agache I, Agarwal A, Bachert C, Bosnic-Anticevich S, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines—2016 revision. 2017.
Togias A. Mechanisms of nose-lung interaction. Allergy. 1999;54(s57):94–105.
Passalacqua G, Ciprandi G, Canonica GW. The nose-lung interaction in allergic rhinitis and asthma: united airways disease. Curr Opin Allergy Clin Immunol. 2001;1(1):7–13.
•• Giavina-Bianchi P, Aun MV, Takejima P, Kalil J, Agondi RC. United airway disease: current perspectives. J Asthma Allergy. 2016;9:93–100. This paper gathers epidemiologic, pathophysiologic, and clinical evidence for an integrated view of rhinitis and asthma defining them unitarily as “united airway disease.
Jeffery CC, Bhutani M, Vliagoftis H, Wright ED, Seikaly H, Côté DWJ. Association between allergic rhinitis and asthma in a Northern Alberta cohort. J Otolaryngol Head Neck Surg. 2013;42(1):58.
Ciprandi G, Cirillo I. The lower airway pathology of rhinitis. J Allergy Clin Immunol. 2006;118(5):1105–9.
Lin J, Su N, Liu G, Yin K, Zhou X, Shen H, et al. The impact of concomitant allergic rhinitis on asthma control: a cross-sectional nationwide survey in China. J Asthma. 2014;51(1):34–43.
Bousquet J, Hellings PW, Agache I, Bedbrook A, Bachert C, Bergmann KC, et al. ARIA 2016: care pathways implementing emerging technologies for predictive medicine in rhinitis and asthma across the life cycle. Clin Transl Allergy. 2016;6:47.
Cibella F, Ferrante G, Cuttitta G, Bucchieri S, Melis MR, La Grutta S, et al. The burden of rhinitis and rhinoconjunctivitis in adolescents. Allergy Asthma Immunol Res. 2015;7(1):44–50.
Navarro AM, Delgado J, Muñoz-Cano RM, Dordal MT, Valero A, Quirce S, et al. Allergic respiratory disease (ARD), setting forth the basics: proposals of an expert consensus report. Clin Transl Allergy. 2017;7:16.
Ciprandi G, Caimmi D, Miraglia Del Giudice M, La Rosa M, Salpietro C, Marseglia GL. Recent developments in United airways disease. Allergy Asthma Immunol Res. 2012;4(4):171–7.
Bonay M, Neukirch C, Grandsaigne M, Leçon-Malas V, Ravaud P, Dehoux M, et al. Changes in airway inflammation following nasal allergic challenge in patients with seasonal rhinitis. Allergy. 2006;61(1):111–8.
Zhu Z, Xie Y, Guan W, Gao Y, Xia S, Zhong N, et al. FeNO for detecting lower airway involvement in patients with allergic rhinitis. Exp Ther Med. 2016;12(4):2336–40.
Braunstahl G-J, Overbeek SE, Fokkens WJ, Kleinjan A, Mceuen AR, Walls AF, et al. Segmental bronchoprovocation in allergic rhinitis patients affects mast cell and basophil numbers in nasal and bronchial mucosa. Am J Respir Crit Care Med. 2001;164(5):858–65.
Ciprandi G, Signori A, Tosca MA, Cirillo I. Spirometric abnormalities in patients with allergic rhinitis: Indicator of an “asthma march”? Am J Rhinol Allergy. 2011;25(5):181–5.
Lambrecht BN, Hammad H. Asthma: the importance of dysregulated barrier immunity. Eur J Immunol. 2013;43(12):3125–37.
Pawankar R, Bunnag C, Khaltaev N, Bousquet J. Allergic rhinitis and its impact on asthma in Asia Pacific and the ARIA update 2008. World Allergy Organ J. 2012;5(Suppl 3):S212–7.
Linneberg A, Henrik Nielsen N, Frølund L, Madsen F, Dirksen A, Jørgensen T, et al. The link between allergic rhinitis and allergic asthma: a prospective population-based study. The Copenhagen Allergy Study. Allergy. 2002;57(11):1048–52.
• Cirillo I, Ricciardolo FLM, Medusei G, Signori A, Ciprandi G. Exhaled nitric oxide may predict bronchial hyperreactivity in patients with allergic rhinitis. Int Arch Allergy Immunol. 2013;160(3):322–8. This study highlights the relevance of FeNO as a possible predictive marker for BHR in AR patients and underlines the close link between upper and lower airways.
Lee E, Lee SH, Kwon J-W, Kim Y, Cho H-J, Yang S-I, et al. A rhinitis phenotype associated with increased development of bronchial hyperresponsiveness and asthma in children. Ann Allergy Asthma Immunol. 2016;117(1):21–28.e1.
Nickel R, Lau S, Niggemann B, Gruber C, von Mutius E, Illi S, et al. Messages from the German multicentre allergy study. Pediatr Allergy Immunol. 2002;13(s15):7–10.
Spergel J, Paller AS. Atopic dermatitis and the atopic march. J Allergy Clin Immunol. 2003;112(6):S118–27.
Asher MI, Montefort S, Björkstén B, Lai CKW, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet (Lond Engl). 2006;368(9537):733–43.
Björkstén B, Clayton T, Ellwood P, Stewart A, Strachan D. Phase III study groupthe I. Worldwide time trends for symptoms of rhinitis and conjunctivitis: phase III of the International Study of Asthma and Allergies in Childhood. Pediatr Allergy Immunol. 2008;19(2):110–24.
Yoo B, Park Y, Park K, Kim H. A 9-year trend in the prevalence of allergic disease based on national health insurance data. J Prev Med Public Health. 2015;48(6):301–9.
Linneberg A, Dam Petersen K, Hahn-Pedersen J, Hammerby E, Serup-Hansen N, Boxall N. Burden of allergic respiratory disease: a systematic review. Clin Mol Allergy. 2016;14:12.
Sinha B, Vibha, Singla R, Chowdhury R. Allergic rhinitis: a neglected disease—a community based assessment among adults in Delhi. J Postgrad Med. 2015;61(3):169–75.
Bousquet J, Anto JM, Wickman M, Keil T, Valenta R, Haahtela T, et al. Are allergic multimorbidities and IgE polysensitization associated with the persistence or re-occurrence of foetal type 2 signalling? The MeDALL hypothesis. Allergy. 2015;70(9):1062–78.
Liu AH, Babineau DC, Krouse RZ, Zoratti EM, Pongracic JA, O’Connor GT, et al. Pathways through which asthma risk factors contribute to asthma severity in inner-city children. J Allergy Clin Immunol. 2016;138(4):1042–50.
• Aguilar D, Pinart M, Koppelman GH, Saeys Y, Nawijn MC, Postma DS, et al. Computational analysis of multimorbidity between asthma, eczema and rhinitis. PLoS One. 2017;12(6):e0179125. This in silico study highlights the molecular mechanisms overlap among AR and asthma.
BioCarta_Pathways [Internet]. [cited2017Nov 2]. Available from:https://cgap.nci.nih.gov/Pathways/BioCarta_Pathways.
Canonica GW, Compalati E. Minimal persistent inflammation in allergic rhinitis: implications for current treatment strategies. Clin Exp Immunol. 2009;158(3):260–71.
Kurukulaaratchy RJ, Zhang H, Patil V, Raza A, Karmaus W, Ewart S, et al. Identifying the heterogeneity of young adult rhinitis through cluster analysis in the Isle of Wight birth cohort. J Allergy Clin Immunol. 2015;135(1):143–50.
Braunstahl G-J, Fokkens WJ, Overbeek SE, KleinJan A, Hoogsteden HC, Prins J-B. Mucosal and systemic inflammatory changes in allergic rhinitis and asthma: a comparison between upper and lower airways. Clin Exp Allergy. 2003;33(5):579–87.
Burgess JA, Walters EH, Byrnes GB, Matheson MC, Jenkins MA, Wharton CL, et al. Childhood allergic rhinitis predicts asthma incidence and persistence to middle age: a longitudinal study. J Allergy Clin Immunol. 2007;120(4):863–9.
Polosa R, Al-Delaimy WK, Russo C, Piccillo G, Sarvà M. Greater risk of incident asthma cases in adults with allergic rhinitis and effect of allergen immunotherapy: a retrospective cohort study. Respir Res. 2005;6(1):153.
Niggemann B, Jacobsen L, Dreborg S, Ferdousi HA, Halken S, Høst A, et al. Five-year follow-up on the PAT study: specific immunotherapy and long-term prevention of asthma in children. Allergy. 2006;61(7):855–9.
Jacobsen L, Niggemann B, Dreborg S, Ferdousi HA, Halken S, Høst A, et al. Specific immunotherapy has long-term preventive effect of seasonal and perennial asthma: 10-year follow-up on the PAT study. Allergy. 2007;62(8):943–8.
Meadows A, Kaambwa B, Novielli N, Huissoon A, Fry-Smith A, Meads C, et al. A systematic review and economic evaluation of subcutaneous and sublingual allergen immunotherapy in adults and children with seasonal allergic rhinitis. Health Technol Assess. 2013;17(27):vi. xi–xiv, 1-322
Möller C, Dreborg S, Ferdousi HA, Halken S, Høst A, Jacobsen L, et al. Pollen immunotherapy reduces the development of asthma in children with seasonal rhinoconjunctivitis (the PAT-study). J Allergy Clin Immunol. 2002;109(2):251–6.
Halken S, Larenas-Linnemann D, Roberts G, Calderón MA, Angier E, Pfaar O, et al. EAACI guidelines on allergen immunotherapy: prevention of allergy. Pediatr Allergy Immunol. 2017;28:728–45.
Platts-Mills TAE, de Weck AL. Dust mite allergens and asthma—a worldwide problem. J Allergy Clin Immunol. 1989;83(2 Pt 1):416–27.
Sporik R, Holgate ST, Platts-Mills TAE, Cogswell JJ. Exposure to house-dust mite allergen (Der p I) and the development of asthma in childhood. N Engl J Med. 1990;323(8):502–7.
Meng Q, Liu X, Li P, He L, Xie J, Gao X, et al. The influence of house dust mite sublingual immunotherapy on the TSLP-OX40L signaling pathway in patients with allergic rhinitis. Int Forum Allergy Rhinol. 2016;6(8):862–70.
Ulrik CS, Backer V. Markers of impaired growth of pulmonary function in children and adolescents. Am J Respir Crit Care Med. 1999;160(1):40–4.
Huang F-L, Liao E-C, Yu, S-J. House dust mite allergy: its innate immune response and immunotherapy. Immunobiology. 2018;223(3):300–302. https://doi.org/10.1016/j.imbio.2017.10.035.
Venn A, Lewis S, Cooper M, Hill J, Britton J. Questionnaire study of effect of sex and age on the prevalence of wheeze and asthma in adolescence. BMJ. 1998;316(7149):1945–6.
Geier DA, Kern JK, Geier MR. Demographic and neonatal risk factors for childhood asthma in the USA. J Matern Fetal Neonatal Med. 2017:1–5.
O’Connor GT, Lynch SV., Bloomberg GR, Kattan M, Wood RA, Gergen PJ, et al. Early-life home environment and risk of asthma among inner-city children. Allergy Clin Immunol. 2017. https://doi.org/10.1016/j.jaci.2017.06.040.
Ferrini M, Carvalho S, Cho YH, Postma B, Miranda Marques L, Pinkerton K, et al. Prenatal tobacco smoke exposure predisposes offspring mice to exacerbated allergic airway inflammation associated with altered innate effector function. Part Fibre Toxicol. 2017;14(1):30.
Makadia LD, Roper PJ, Andrews JO, Tingen MS. Tobacco use and smoke exposure in children: new trends, harm, and strategies to improve health outcomes. Curr Allergy Asthma Rep. 2017;17(8):55.
Tanaka K, Miyake Y, Furukawa S, Arakawa M. Secondhand smoke exposure and risk of wheeze in early childhood: a prospective pregnancy birth cohort study. Tob Induc Dis. 2017;15(1):30.
Polosa R, Knoke JD, Russo C, Piccillo G, Caponnetto P, Sarvà M, et al. Cigarette smoking is associated with a greater risk of incident asthma in allergic rhinitis. J Allergy Clin Immunol. 2008;121(6):1428–34.
Diaz-Sanchez D, Rumold R, Gong H. Challenge with environmental tobacco smoke exacerbates allergic airway disease in human beings. J Allergy Clin Immunol. 2006;118(2):441–6.
Polosa R, Russo C, Caponnetto P, Bertino G, Sarvà M, Antic T, et al. Greater severity of new onset asthma in allergic subjects who smoke: a 10-year longitudinal study. Respir Res. 2011;12(1):16.
Platts-Mills TAE. The role of immunoglobulin E in allergy and asthma. Am J Respir Crit Care Med. 2001;164(supplement_1):S1–5.
Platts-Mills TAE, Woodfolk JA. Allergens and their role in the allergic immune response. Immunol Rev. 2011;242(1):51–68.
Makinen T, Lehtimäki L, Kinnunen H, Nieminen R, Kankaanranta HME. Bronchial diffusing capacity of nitric oxide is increased in patients with allergic rhinitis. Int Arch Allergy Immunol. 2009;148(2):154–60.
Ciprandi G, Tosca MA, Capasso M. Exhaled nitric oxide in children with allergic rhinitis and/or asthma: a relationship with bronchial hyperreactivity. J Asthma. 2010;47(10):1142–7.
Panganiban RP, Wang Y, Howrylak J, Chinchilli VM, Craig TJ, August A, et al. Circulating microRNAs as biomarkers in patients with allergic rhinitis and assthma. J Allergy Clin Immunol. 2016;137(5):1423–32.
Hu D, Zhang Z, Ke X, Kang H, Hong S. A functional variant of miRNA-149 confers risk for allergic rhinitis and comorbid asthma in Chinese children. Int J Immunogenet. 2017;44(2):62–70.
Luo X, Hong H, Tang J, Wu X, Lin Z, Ma R, et al. Increased expression of miR-146a in children with allergic rhinitis after allergen-specific immunotherapy. Allergy Asthma Immunol Res. 2016;8(2):132–40.
Lu L-F, Boldin MP, Chaudhry A, Lin L-L, Taganov KD, Hanada T, et al. Function of miR-146a in controlling Treg cell-mediated regulation of Th1 responses. Cell. 2010;142(6):914–29.
Wallace D, Dykewicz M, Bernstein D, Blessingmoore J, Cox L, Khan D, et al. The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol. 2008;122(2):S1–84.
Brożek JL, Bousquet J, Baena-Cagnani CE, Bonini S, Canonica GW, Casale TB, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010;126(3):466–76.
Larché M, Akdis CA, Valenta R. Immunological mechanisms of allergen-specific immunotherapy. Nat Rev Immunol. 2006;6(10):761–71.
Holgate ST, Polosa R. Treatment strategies for allergy and asthma. Nat Rev Immunol. 2008;8(3):218–30.
Burks AW, Calderon MA, Casale T, Cox L, Demoly P, Jutel M, et al. Update on allergy immunotherapy: American academy of allergy, asthma & immunology/European academy of allergy and clinical immunology/PRACTALL consensus report. J Allergy Clin Immunol. 2013;131(5):1288–1296.e3.
Şahin E, Bafaqeeh SA, Güven SG, Çetinkaya EA, Muluk NB, Coşkun ZO, et al. Mechanism of action of allergen immunotherapy. Am J Rhinol Allergy. 2016;30(5):1–3.
Polosa R. Can immunotherapy prevent progression to asthma in allergic individuals? J Allergy Clin Immunol. 2002;110(4):672–3.
Baena-Cagnani CE, Larenas-Linnemann D, Teijeiro A, Canonica GW, Passalacqua G. Will sublingual immunotherapy offer benefit for asthma? Curr Allergy Asthma Rep. 2013;13(6):571–9.
Purello-D’Ambrosio F, Gangemi S, Merendino RA, Isola S, Puccinelli P, Parmiani S, et al. Prevention of new sensitizations in monosensitized subjects submitted to specific immunotherapy or not. A retrospective study. Clin Exp Allergy. 2001;31(8):1295–302.
Des Roches A, Paradis L, Menardo JL, Bouges S, Daurés JP, Bousquet J. Immunotherapy with a standardized Dermatophagoides pteronyssinus extract. VI. Specific immunotherapy prevents the onset of new sensitizations in children. J Allergy Clin Immunol. 1997;99(4):450–3.
Pajno GB, Barberio G, De Luca F, Morabito L, Parmiani S. Prevention of new sensitizations in asthmatic children monosensitized to house dust mite by specific immunotherapy. A six-year follow-up study. Clin Exp Allergy. 2001;31(9):1392–7.
Marogna M, Tomassetti D, Bernasconi A, Colombo F, Massolo A, Businco ADR, et al. Preventive effects of sublingual immunotherapy in childhood: an open randomized controlled study. Ann Allergy Asthma Immunol. 2008;101(2):206–11.
Inal A, Altintas DU, Yilmaz M, Karakoc GB, Kendirli SG, Sertdemir Y. Prevention of sew sensitizations by specific immunotherapy in children with rhinitis and/or asthma monosensitized to house dust mite. J Investig Allergol Clin Immunol. 2007;17(2):85–91.
Novembre E, Galli E, Landi F, Caffarelli C, Pifferi M, De Marco E, et al. Coseasonal sublingual immunotherapy reduces the development of asthma in children with allergic rhinoconjunctivitis. J Allergy Clin Immunol. 2004;114(4):851–7.
Polosa R, Li Gotti F, Mangano G, Paolino G, Mastruzzo C, Vancheri C, et al. Effect of immunotherapy on asthma progression, BHR and sputum eosinophils in allergic rhinitis. Allergy. 2004;59(11):1224–8.
Milani M, Pecora S, Burastero S, Group on behalf of EIS. Observational study of sublingual specific immunotherapy in persistent and intermittent allergic rhinitis: the EFESO trial. Curr Med Res Opin. 2008;24(9):2719–24.
• Karakoc-Aydiner E, Eifan A, Baris S, Gunay E, Akturk H, Akkoc T, et al. Long-term effect of sublingual and subcutaneous immunotherapy in dust mite–allergic children with asthma/rhinitis: a 3-year prospective randomized controlled trial. J Investig Allergol Clin Immunol. 2015;25(255):334–42. This Randomized Controlled Trial shows the efficacy and the prevention effect of SIT in Dust Mite allergic children with AR or mild asthma.
Valovirta E, Petersen TH, Piotrowska T, Laursen MK, Andersen JS, Sørensen HF, et al. Results from the 5-year SQ grass sublingual immunotherapy tablet asthma prevention (GAP) trial in children with grass pollen allergy. J Allergy Clin Immunol. 2018;141(2):529-538. https://doi.org/10.1016/j.jaci.2017.06.014.
British Thoracic Society and Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. 2016. Available from: https://www.brit-thoracic.org.uk/document-library/clinical-information/asthma/btssign-asthma-guideline-2016/.
Nurmatov U, Dhami S, Arasi S, Roberts G, Pfaar O, Muraro A, et al. Allergen immunotherapy for allergic rhinoconjunctivitis: a systematic overview of systematic reviews. Clin Transl Allergy. 2017;7:24.
Di Bona D, Plaia A, Leto-Barone MS, La Piana S, Macchia L, Di Lorenzo G. Efficacy of allergen immunotherapy in reducing the likelihood of developing new allergen sensitizations: a systematic review. Allergy. 2017;72(5):691–704.
• Kristiansen M, Dhami S, Netuveli G, Halken S, Muraro A, Roberts G, et al. Allergen immunotherapy for the prevention of allergy: a systematic review and meta-analysis. Pediatr Allergy Immunol. 2017;28(1):18–29. This systematic review provides evidences of a reduced short-term risk of developing asthma in allergic rhinitis subjects treated with SIT.
Ridolo E, Incorvaia C, Gritti BL, Passalacqua G. The current overuse and misuse of meta-analyses on sublingual immunotherapy: the case of grass pollen allergy. Curr Opin Allergy Clin Immunol. 2017;17(1):12–6.
Abramson MJ, Puy RM, Weiner JM. Allergen immunotherapy for asthma. Cochrane Database Syst Rev. 2003;4:CD001186.
Penagos M, Passalacqua G, Compalati E, Baena-Cagnani CE, Orozco S, Pedroza A, et al. Metaanalysis of the efficacy of sublingual immunotherapy in the treatment of allergic asthma in pediatric patients, 3 to 18 years of age. Chest. 2008;133(3):599–609.
Guilbert TW, Morgan WJ, Zeiger RS, Mauger DT, Boehmer SJ, Szefler SJ, et al. Long-term inhaled corticosteroids in preschool children at high risk for asthma. N Engl J Med. 2006;354(19):1985–97.
Bisgaard H, Hermansen MN, Loland L, Halkjaer LB, Buchvald F. Intermittent inhaled corticosteroids in Infants with episodic wheezing. N Engl J Med. 2006;354(19):1998–2005.
Murray CS, Woodcock A, Langley SJ, Morris J, Custovic A, IFWIN study team. Secondary prevention of asthma by the use of Inhaled Fluticasone propionate in Wheezy INfants (IFWIN): double-blind, randomised, controlled study. Lancet (Lond Engl). 2006;368(9537):754–62.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Morjaria reports non-financial support from Boehringer Ingelheim, during the conduct of the study; personal fees and other from Boehringer Ingelehim; Chiesi; AstraZeneca; Novartis; Teva UK Ltd; Pfizer; and GlaxoSmithKline, outside the submitted work. The other authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Rhinitis
Rights and permissions
About this article
Cite this article
Morjaria, J.B., Caruso, M., Emma, R. et al. Treatment of Allergic Rhinitis as a Strategy for Preventing Asthma. Curr Allergy Asthma Rep 18, 23 (2018). https://doi.org/10.1007/s11882-018-0781-y
Published:
DOI: https://doi.org/10.1007/s11882-018-0781-y