Abstract
Over the past several years, taste receptors have emerged as key players in the regulation of innate immune defenses in the mammalian respiratory tract. Several cell types in the airway, including ciliated epithelial cells, solitary chemosensory cells, and bronchial smooth muscle cells, all display chemoresponsive properties that utilize taste receptors. A variety of bitter products secreted by microbes are detected with resultant downstream inflammation, increased mucous clearance, antimicrobial peptide secretion, and direct bacterial killing. Genetic variation of bitter taste receptors also appears to play a role in the susceptibility to infection in respiratory disease states, including that of chronic rhinosinusitis. Ongoing taste receptor research may yield new therapeutics that harness innate immune defenses in the respiratory tract and may offer alternatives to antibiotic treatment. The present review discusses taste receptor-protective responses and analyzes the role these receptors play in mediating airway immune function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Canonically, taste has been thought of as an adaptive sense for organisms that feed on matter in the environment: food that nourishes and provides energy is considered to have a pleasant taste, while poisons and inedible material tend to be far less palatable. Specifically, bitter taste receptors are often tuned to respond to toxic chemicals or organismal products that compromise digestive health. Over the past several years, a growing body of literature supports a much broader role for taste receptors throughout the body, with functions that extend far beyond the sensory capacity of the tongue [1–6]. Both bitter and sweet taste receptors are expressed in the airway, where they appear to play several important roles in innate immune defense [7••, 8••]. In this review, we will explore the function of taste receptors in the sinonasal tract and the implications that these receptors have in the understanding of rhinologic and pulmonary disease.
Taste Receptor Mechanisms
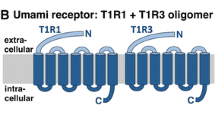
Bitter and sweet taste receptors are G-protein-coupled receptors (GPCRs) that were first identified in taste bud type II cells [9, 10]. Those from taste receptor family 1 subtypes 2 and 3 (T1R2/T1R3) respond to sugars [5, 11] such as glucose, fructose, and sucrose [12]. Bitter taste receptors, from taste receptor family 2 (T2Rs), have a much wider diversity of subtypes, with each tuned to specific bitter compounds [13]. These compounds include the plant sesquiterpene lactones, clerodane, strychnine, and denatonium [14]. Humans are known to have at least 25 T2R subtypes [11, 15], and there are many others that have been discovered in mammalian species [16]. The type II taste cells of the tongue most often express only one taste modality, but some cells do express multiple unique receptors [17–19]. Presently, this capability of a multimodal cell to discriminate between distinct compounds has yet to be fully explained.
The presynaptic mechanisms for taste receptor stimulation and signal transduction are relatively conserved in the tongue and the airway. Briefly, a bitter or sweet ligand binds its respective GPCR, triggering downstream activation of phospholipase C isoform β2 (PLCβ2). PLCβ2 then causes inositol 1,4,5-trisphosphate (IP3) production, activating the IP3 receptor (IP3R) on the endoplasmic reticulum to stimulate the release of calcium (Ca2+) [20]. While this process occurs, the GPCR stimulation also activates phosphodiesterases (PDEs) that cause the reduction of cAMP levels and corresponding protein kinase A (PKA) activity. PKA acts as an inhibitor of the type III IP3R through phosphorylation, so the removal of this inhibitory pathway further enhances calcium release from the endoplasmic reticulum [21–23]. The released calcium activates the TRPM5 channel [24], which depolarizes the cell membrane, activates voltage-gated sodium (Na+) channels, and generates an action potential that causes ATP release through the CALHM1 ion channel [5, 23, 25, 26]. In the tongue, this ATP release activates purinergic receptors on presynaptic taste cells and sensory fibers, transmitting the sensation of taste to the central nervous system [5, 26, 27].
Taste Receptors and Airway Immunity
GPCR taste receptors are expressed in a number of organ systems, including the brain, pancreas, testicles, bladder, and GI tract [1–6]. The present review will focus on taste receptors expressed in the airway: the sinuses, trachea, and bronchi.
Overview of Innate Airway Immunity
Several respiratory immune mechanisms work in concert to achieve lower airway sterility, in spite of the vast number of bacteria, fungi, and viruses that are inhaled into the upper respiratory tract with each breath. The convoluted anatomy of the sinonasal tract, combined with the ciliated surface, traps particulates and organisms in a mucus layer, which is then cleared by beating cilia [28]. During infection or debris inhalation, ciliary beat frequency (CBF) increases to speed up this mucociliary clearance (MCC) [29]. In addition to transporting the mucus to the nasopharynx or oropharynx where it is cleared by swallowing, innate immune products are disseminated on the airway surface [30]. These immune products include directly anti-organismal compounds such as defensins, lactoferrin, cathelicidins, and lysozyme, in addition to reactive oxygen species (ROS) and nitric oxide (NO) that also display potent antimicrobial activity [31]. Several indirect pathways are activated as well, with the release of cytokines and chemokines that recruit the adaptive immune system and begin inflammatory cascades [32].
In order to activate all of these defense mechanisms, recognition of foreign organisms or toxins both immediately and throughout bacterial colonization is paramount. The mechanisms behind this process have not yet been fully elucidated. Toll-like receptors (TLRs) are expressed by airway ciliated cells and recognize pathogen-associated molecular patterns (PAMPs), which are bacterial cell wall components or bacterial products. These include lipoteichoic acid in gram-positive organisms, lipopolysaccharide in gram-negative organisms, and flagellin (a protein involved in organismal motility) [33]. TLR signaling and downstream immune effect take up to 12 hours and work through gene expression, creating a sustained immune response [34]. However, a portion of antimicrobial peptide secretion and changes in MCC in response to pathogens occur almost immediately [35], suggesting the existence of a molecular pathway that can rapidly detect foreign compounds and effect timely responses. Bitter taste receptors may provide a missing link in this pathway as initiators of this rapid defense.
Airway Bitter Taste Receptors
A wide variety of bitter taste receptors are expressed in various parts of both the human and rodent airway (Table 1). Some of the bitter compounds that are detected by these airway receptors include denatonium benzoate, absinthin, salicin, sodium thiocyanate, phenylthiocarbamide (PTC), thujone, parthenolide, acetylthiourea, cycloheximide, and amarogentin [8••, 35, 36•, 37, 38•]. While some bitter taste receptors in the airway are upstream of a nervous system signaling cascade [7••, 39••, 40], others act in a cell-autonomous fashion without any nervous innervation. Thus, response to the bitter products detected is an entirely local phenomenon in these cells. In 2009, bronchial epithelial cells were shown to have Ca2+ increases following bitter compound stimulation, precipitating further downstream responses of increasing CBF and thus accelerating clearance of the toxin or organism producing the bitter compound [38•]. These T2R receptors are located on the motile cilia themselves. In response to PTC stimulation of sinonasal epithelial cell bitter taste receptors, an increase in NO production is also observed, with potent bactericidal consequences [8••]. NO diffuses very quickly into bacteria such as Pseudomonas aeruginosa, where it causes cellular destruction and death [41]. In addition to this direct antimicrobial activity, NO acts as a second messenger to activate protein kinase G (PKG) and guanylyl cyclase to phosphorylate proteins within the cilia and speed up CBF [42]. Other experiments have further investigated this NO pathway and found that both the TRPM5 channel and PLCβ2, two of the components in canonical taste transduction, are necessary for NO production but not the canonical taste G protein gustducin [8••].
Lactones are bitter chemicals that can stimulate T2Rs in the airway [8••, 43], and acyl-homoserine lactones (AHLs) are a subclass of lactones that are produced by many gram-negative bacteria [44, 45]. AHLs serve as biofilm “quorum-sensing molecules” for the bacteria. Once a sufficient concentration of AHLs is produced in a localized environment, bacteria will begin to form a biofilm, which confers increased protection for the bacteria from the immune defenses of the host [46]. It is hypothesized that detection of these AHLs before bacteria reach a density required for biofilm formation is an adaptive mechanism, allowing for an increased immune response before microbial protection occurs in the biofilm formation [7••]. Through the bitter taste receptors, the airway is able to “spy” on the bacterial communication system [45].
Solitary Chemosensory Cells
Ciliated epithelial cells are not the only cells to express bitter taste receptors in the airway. Over a decade ago, a class of cells that is sparsely scattered in rodent respiratory epithelium was shown to be immunoreactive with alpha-gustducin (a component of taste signaling) [47]. These cells were named “solitary chemosensory cells” (SCCs), and they share many similarities with cells found in the taste buds of the tongue [36•]. Approximately one out of every hundred cells in the sinonasal cavity is a SCC, making their isolation experimentally challenging [39••]. The function of these airway taste-like cells was explored further, and it was discovered that they express sweet and bitter taste receptors [35, 48], capable of responding to AHLs and other bitter agonists [7••, 40, 49]. These SCCs show intracellular calcium responses in the presence of AHLs [39••], but they do not activate downstream NO production. Instead, when mouse sinonasal SCCs are stimulated with AHLs or denatonium, the calcium response results in acetylcholine (ACh) release that stimulates trigeminal nerve peptidergic nociceptors, with downstream effects of breath holding and inflammatory mediator release [7••, 39••, 40]. The inflammatory response is intuitively antimicrobial, while the breath holding response may also represent an adaptive reflex to limit toxin or organism aspiration in the host. Calcitonin gene-related peptide (CGRP), substance P, and vasoactive intestinal peptide (VIP) are known substances released in this inflammatory cascade [50, 51], and CBF increases and transient fluid secretion are also possible consequences of this substance generation [52••].
SCCs have been identified in human upper airway tissue as well [35, 53••], along with additional physiological function beyond what has been elucidated in the rodent system (Table 1). T1R1, T1R2, T2R4, T2R10, and T2R47 are all expressed on SCCs in the human nasal cavity [37, 53••]. Denatonium, a bitter compound that shows activity in mouse SCC signaling [36•], also stimulates a Ca2+ response in human SCCs that spreads to neighboring cells via gap junctions [37]. Just as in the NO response seen in ciliated cells, the calcium signaling requires many known components of traditional taste signaling, including gustducin, PLCβ2, the IP3 receptor, and TRPM5 [37]. Gap junction spread of the signal causes immediate release of antimicrobial peptides (AMPs) from the adjacent ciliated cells (Fig. 1) [35]. These AMPs include beta defensin 1 (BD1) and beta defensin 2 (BD2), and the secreted products have potent activity in killing of gram-positive and gram-negative organisms [51], including methicillin-resistant Staphylococcus aureus and P. aeruginosa. This rapid secretion of antimicrobial products contrasts directly with the TLR mechanism of AMP precursor messenger RNA upregulation, causing a sustained response that does not appear until several hours after bacterial stimulation [34]. Preformed stores of AMPs are released in the T2R response, rather than de novo synthesis [51]. Of interest, this SCC response of AMP secretion has not been demonstrated in the mouse and may represent a newer adaptation. Further investigation of the difference in SCC function between species is necessary to adequately explain the adaptive patterns of innate defense.
Function of the solitary chemosensory cell (SCC) in innate immune defense in humans. The presence of infectious bacteria decreases glucose concentration in the airway surface liquid (ASL), decreasing stimulation of the T1R receptor and releasing inhibition of T2R signaling. Additionally, the bacteria secrete bitter compounds that directly stimulate the T2R receptors. This propagates a downstream calcium response that spreads to neighboring ciliated cells that secrete antimicrobial peptides that directly kill the inciting pathogen
T2R38
T2Rs are very genetically diverse, a phenomenon that helps to explain the wide variety of taste preference both within and between cultures [60, 61]. Many individuals find bitter foods such as coffee or herbs to be detestable, while others do not have an aversive response. This genetic variation of T2Rs is not exclusively found in the tongue; T2R receptor variation in the airway appears to also play a key role in respiratory defense. T2R38, a receptor that is localized to motile cilia in humans, responds to at least three AHLs produced by P. aeruginosa, N-butyryl-l-homoserine lactone, C-6-homoserine lactone, and N-3-oxo-dodecanoyl-l-homoserine lactone [8••]. Additionally, PTC and propylthiouracil (PROP) are bitter compounds that also agonize T2R38 in a similar fashion [62]. When T2R38 is stimulated by AHLs, PTC, or PROP, NO is produced to speed up MCC and directly kill pathogens in the human respiratory mucosa (Fig. 2) [37]. However, the genetic locus for T2R38, TAS2R38, has three common polymorphisms that tend to segregate together, yielding a functional receptor (PAV) and a non-functional receptor (AVI) [61]. The polymorphisms are so named with respect to their amino acid sequence differences, with the functional protein containing a proline, alanine, and valine sequence (PAV) and the non-functional protein containing an alanine, valine, and isoleucine (AVI). Individuals who have an AVI/AVI genotype do not taste the bitter compounds PTC or PROP [63••], and epithelial cells from these patients grown at an air-liquid interface (ALI) show significantly lower NO production in response to AHLs when compared to epithelial cells from a PAV/PAV individual. The consequent reductions in MCC and bacterial killing are also significant in the AVI/AVI group [8••].
T2R38 bitter taste receptor regulation of innate immunity in humans. P. aeruginosa produces acyl-homoserine lactone quorum-sensing molecules, which stimulate the T2R38 bitter taste receptor. This precipitates a downstream calcium response with subsequent nitric oxide (NO) production. The NO diffuses into the airway where it is directly bactericidal and additionally activates protein kinase G to increase ciliary beat frequency and mucociliary clearance
The implications of these differences are broad. Patients with chronic rhinosinusitis (CRS) have pathological mucociliary stasis, which harbors bacteria and allows infection to perpetuate [64]. This creates a very stagnant and favorable environment for bacteria to proliferate and for bacterial toxins to continually cause destruction of both cells and cilia [65, 66]. It was previously shown that sinonasal epithelial explants from patients with CRS show an attenuated response to a variety of compounds that stimulate CBF in normal controls [67, 68]. Additionally, further studies demonstrated that there were differences in NO levels in patients with CRS or other airway diseases [69]. However, a review of the nasal NO literature was unable to demonstrate any trends in rhinopathologies with regard to nasal NO measurements [70]. The pathophysiology behind this disparity is not entirely clear, but the T2R38 genotype (or not controlling for T2R38 genotype) may help to explain the conflicted literature. Individuals who have the PAV/PAV genotype are less likely to need surgical intervention for their CRS symptoms than those with the AVI/AVI genotype [63••, 71•]. PAV/PAV patients are additionally less prone to developing gram-negative infection, such as that of P. aeruginosa [63••, 71•, 72••]. In light of this data, it appears that variation in bitter taste receptor function in humans has a phenotypic effect on upper respiratory disease. In the near future, bitter taste testing with PTC or PROP could potentially help to stratify surgical candidates and identify patients who are more likely to benefit from standard sinus procedures as well as those who should receive alternative or more aggressive management [8••]. Further, the bitter compounds themselves could even serve as therapeutic agents, in speeding up MCC and strengthening host responses to counter bacterial proliferation in CRS [73].
Sweet Taste Receptors
The T1R receptors (dimer of isoform 2 and 3) detect sweet compounds and are also found in the respiratory mucosa [36•]. They have been isolated in the human vomeronasal duct [36•] as well as in SCCs in ALI cultures from surgical explants [35]. In the sinuses, the sweet receptors respond to concentrations of glucose and other sugars that are far lower than those detected on the tongue [74]. Normally, individuals have a glucose concentration of approximately 0.5 mM in the airway surface liquid (ASL), and there is a constant leak and reuptake of glucose from the serum that maintain this constant concentration [37]. The T1R2/3 sweet receptors are tonically activated by this low level of glucose and appear to function in an antagonistic role to that of the bitter taste receptors. Depletion of ASL glucose is a harbinger of bacterial infection, as the bacteria consume the sugar rapidly. It is hypothesized that this reduction in glucose deactivates the sweet receptors, which then release their inhibition on the action of the T2R receptors to bitter compounds [37]. While low-level colonization by bacteria is expected in the sinonasal tract, any perturbation in this homeostasis towards glucose depletion (i.e., more than colonization) causes a balance in favor of T2R activation with subsequent mobilization of local defenses against the pathogen, resulting in decreased microbial numbers and restoration of physiologic airway surface glucose concentrations. This cycle is on a “continuing loop” thus maintaining a low level of bacteria, i.e., colonization, with airway surface glucose acting as an indirect measurement of bacterial load.
This hypothesis has been supported by several experiments. The addition of glucose and sucrose (both T1R2/3 agonists) to the ASL of an ALI culture blocks the calcium response of bitter taste receptors to denatonium, while mice that do not express these sweet receptors [75] show a normal response to the compound [37]. Antagonists of the T1R2/3 receptors, such as lactisole [76] and amiloride [37, 77], also can release the inhibition of the denatonium response.
Just as is the case with bitter receptors, there is genetic variation in T1Rs that manifests as individual preference in sweet taste [78–80]. While no single locus has yet been identified, there are allele variations among the TAS1R genes (that encode T1Rs) that show frequency differences of >10 % in 16 loci between patients with CRS and controls [72••]. Patients with CRS also have chronically elevated ASL glucose concentrations [37], and a similar elevation is seen in diabetic patients as well [81]. These findings may help provide a parsimonious explanation for why some diabetics are highly prone to airway infections and why having diabetes correlates with unique nasal microbiologic cultures [82]. Additional studies on sweet receptor inhibition are necessary before the pathophysiology can be leveraged to treat chronic respiratory disease, but T1R2/3 antagonists such as lactisole may prove useful in the future in augmentation of host bitter taste responses.
Additional Functions of Taste Receptors in the Airway
The previous experiments discussed focused on SCCs and ciliated cells that populate the upper airway, and SCCs are unique to that location of the respiratory tract. Bronchial tissue, which contains an abundance of smooth muscle cells, does not demonstrate SCC responses or secretion of AMPs following stimulation [37]. However, the smooth muscle cells do express several T2R receptors, and activation of these receptors causes bronchodilation [36•, 57•]. This phenomenon possibly occurs due to an increase in Ca2+ that modifies potassium currents within the muscle cells that causes them to become hyperpolarized and relax [58]. These cells lack innervation, so this response is similar to that of the NO production within ciliated cells, in that it is a local defense. Interestingly, asthmatics have an upregulation in TAS2R gene expression [83•].
Allele expression studies in patients with CRS show that T2R38 is not the only genetic determinant of disease severity. Several other loci, such as that of TAS2R14 and TAS2R49, show an allele frequency difference of >10 % between CRS patients and controls [72••]. It will be important for future research to determine the full expression pattern of taste receptors throughout the length of the respiratory tract, as well as explore the full complement of bitter products that are secreted by organisms. Preliminary data also shows a role for T2R pathways in fungal [84] and viral detection as well [85].
Conclusions
Airway taste receptors play an important role in innate respiratory defense, and they function in regulating inflammation and antimicrobial activity within the respiratory tract. These responses are quick in onset and are complementary to traditional antimicrobial pathways, such as those involving TLRs. Dysfunction or genetic variation of bitter or sweet taste receptors appears to play a key role in respiratory disease, including CRS and increased susceptibility to infection in diabetes. Conventional management of respiratory diseases often involves antibiotics, but strengthening endogenous defense mechanisms may be possible by using T1R and T2R receptors as novel therapeutic targets.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Laffitte A, Neiers F, Briand L. Functional roles of the sweet taste receptor in oral and extraoral tissues. Curr Opin Clin Nutr Metab Care. 2014;17(4):379–85.
Clark AA, Liggett SB, Munger SD. Extraoral bitter taste receptors as mediators of off-target drug effects. FASEB J. 2012;26(12):4827–31.
Depoortere I. Taste receptors of the gut: emerging roles in health and disease. Gut. 2014;63(1):179–90.
Behrens M, Meyerhof W. Oral and extraoral bitter taste receptors. Results Probl Cell Differ. 2010;52:87–99.
Kinnamon SC. Taste receptor signalling—from tongues to lungs. Acta Physiol (Oxf). 2012;204(2):158–68.
Sternini C, Anselmi L, Rozengurt E. Enteroendocrine cells: a site of ‘taste’ in gastrointestinal chemosensing. Curr Opin Endocrinol Diabetes Obes. 2008;15(1):73–8.
Tizzano M et al. Nasal chemosensory cells use bitter taste signaling to detect irritants and bacterial signals. Proc Natl Acad Sci U S A. 2010;107(7):3210–5. Demonstrated that bitter taste receptors are used to detect bacterial products in the airway.
Lee RJ et al. T2R38 taste receptor polymorphisms underlie susceptibility to upper respiratory infection. J Clin Invest. 2012;122(11):4145–59. Experiment to demonstrate the T2R38 stimulation causes downstream production of NO with subsequent increased MCC and bacterial killing.
Zhang Y et al. Coding of sweet, bitter, and umami tastes: different receptor cells sharing similar signaling pathways. Cell. 2003;112(3):293–301.
Iwata S, Yoshida R, Ninomiya Y. Taste transductions in taste receptor cells: basic tastes and moreover. Curr Pharm Des. 2014;20(16):2684–92.
Margolskee RF. Molecular mechanisms of bitter and sweet taste transduction. J Biol Chem. 2002;277(1):1–4.
Treesukosol Y, Smith KR, Spector AC. The functional role of the T1R family of receptors in sweet taste and feeding. Physiol Behav. 2011;105(1):14–26.
Adler E et al. A novel family of mammalian taste receptors. Cell. 2000;100(6):693–702.
Brockhoff A et al. Broad tuning of the human bitter taste receptor hTAS2R46 to various sesquiterpene lactones, clerodane and labdane diterpenoids, strychnine, and denatonium. J Agric Food Chem. 2007;55(15):6236–43.
Chandrashekar J et al. T2Rs function as bitter taste receptors. Cell. 2000;100(6):703–11.
Wu SV, Chen MC, Rozengurt E. Genomic organization, expression, and function of bitter taste receptors (T2R) in mouse and rat. Physiol Genomics. 2005;22(2):139–49.
Liman ER, Zhang YV, Montell C. Peripheral coding of taste. Neuron. 2014;81(5):984–1000.
Roper SD. Taste buds as peripheral chemosensory processors. Semin Cell Dev Biol. 2013;24(1):71–9.
Meyerhof W et al. The molecular receptive ranges of human TAS2R bitter taste receptors. Chem Senses. 2010;35(2):157–70.
Giovannucci DR et al. Targeted phosphorylation of inositol 1,4,5-trisphosphate receptors selectively inhibits localized Ca2+ release and shapes oscillatory Ca2+ signals. J Biol Chem. 2000;275(43):33704–11.
Voigt A et al. Genetic labeling of Tas1r1 and Tas2r131 taste receptor cells in mice. Chem Senses. 2012;37(9):897–911.
Li F. Taste perception: from the tongue to the testis. Mol Hum Reprod. 2013;19(6):349–60.
Taruno A et al. How do taste cells lacking synapses mediate neurotransmission? CALHM1, a voltage-gated ATP channel. Bioessays. 2013;35(12):1111–8.
Zhang Z et al. The transduction channel TRPM5 is gated by intracellular calcium in taste cells. J Neurosci. 2007;27(21):5777–86.
Miyoshi MA, Abe K, Emori Y. IP(3) receptor type 3 and PLCbeta2 are co-expressed with taste receptors T1R and T2R in rat taste bud cells. Chem Senses. 2001;26(3):259–65.
Taruno A et al. CALHM1 ion channel mediates purinergic neurotransmission of sweet, bitter and umami tastes. Nature. 2013;495(7440):223–6.
Behrens M et al. Immunohistochemical detection of TAS2R38 protein in human taste cells. PLoS One. 2012;7(7), e40304.
Hilding AC. The role of the respiratory mucosa in health and disease. Minn Med. 1967;50(6):915–9.
Shaari J et al. Regional analysis of sinonasal ciliary beat frequency. Am J Rhinol. 2006;20(2):150–4.
Sleigh MA, Blake JR, Liron N. The propulsion of mucus by cilia. Am Rev Respir Dis. 1988;137(3):726–41.
Parker D, Prince A. Innate immunity in the respiratory epithelium. Am J Respir Cell Mol Biol. 2011;45(2):189–201.
Knowles MR, Boucher RC. Mucus clearance as a primary innate defense mechanism for mammalian airways. J Clin Invest. 2002;109(5):571–7.
Ooi EH, Wormald PJ, Tan LW. Innate immunity in the paranasal sinuses: a review of nasal host defenses. Am J Rhinol. 2008;22(1):13–9.
Hume DA et al. Macrophages exposed continuously to lipopolysaccharide and other agonists that act via toll-like receptors exhibit a sustained and additive activation state. BMC Immunol. 2001;2:11.
Barham HP et al. Solitary chemosensory cells and bitter taste receptor signaling in human sinonasal mucosa. Int Forum Allergy Rhinol. 2013;3(6):450–7.
Tizzano M et al. Expression of taste receptors in solitary chemosensory cells of rodent airways. BMC Pulm Med. 2011;11:3. Analyzed the expression pattern of taste receptors in the rodent airway.
Lee RJ et al. Bitter and sweet taste receptors regulate human upper respiratory innate immunity. J Clin Invest. 2014;124(3):1393–405.
Shah AS et al. Motile cilia of human airway epithelia are chemosensory. Science. 2009;325(5944):1131–4. Seminal study demonstrating that cilia can detect chemicals in the sinonasal tract.
Saunders CJ et al. Cholinergic neurotransmission links solitary chemosensory cells to nasal inflammation. Proc Natl Acad Sci U S A. 2014;111(16):6075–80. Experiment to show that the SCC in the mouse transduces bitter taste signals into inflammatory responses.
Gulbransen B, Silver W, Finger TE. Solitary chemoreceptor cell survival is independent of intact trigeminal innervation. J Comp Neurol. 2008;508(1):62–71.
Barraud N et al. Involvement of nitric oxide in biofilm dispersal of Pseudomonas aeruginosa. J Bacteriol. 2006;188(21):7344–53.
Salathe M. Regulation of mammalian ciliary beating. Annu Rev Physiol. 2007;69:401–22.
Chadwick M et al. Sesquiterpenoids lactones: benefits to plants and people. Int J Mol Sci. 2013;14(6):12780–805.
Jimenez PN et al. The multiple signaling systems regulating virulence in Pseudomonas aeruginosa. Microbiol Mol Biol Rev. 2012;76(1):46–65.
Li Z, Nair SK. Quorum sensing: how bacteria can coordinate activity and synchronize their response to external signals? Protein Sci. 2012;21(10):1403–17.
Parsek MR, Greenberg EP. Acyl-homoserine lactone quorum sensing in gram-negative bacteria: a signaling mechanism involved in associations with higher organisms. Proc Natl Acad Sci U S A. 2000;97(16):8789–93.
Zancanaro C et al. Alpha-gustducin expression in the vomeronasal organ of the mouse. Eur J Neurosci. 1999;11(12):4473–5.
Osculati F et al. The solitary chemosensory cells and the diffuse chemosensory system of the airway. Eur J Histochem. 2007;51 Suppl 1:65–72.
Lin W et al. TRPM5-expressing microvillous cells in the main olfactory epithelium. BMC Neurosci. 2008;9:114.
Mendonca JC, Dolci JE. Neuropeptide immunofluorescence in human nasal mucosa: assessment of the technique for vasoactive intestinal peptide (VIP). Braz J Otorhinolaryngol. 2005;71(2):123–31.
Mosimann BL et al. Substance P, calcitonin gene-related peptide, and vasoactive intestinal peptide increase in nasal secretions after allergen challenge in atopic patients. J Allergy Clin Immunol. 1993;92(1 Pt 1):95–104.
Lee RJ et al. Vasoactive intestinal peptide regulates sinonasal mucociliary clearance and synergizes with histamine in stimulating sinonasal fluid secretion. FASEB J. 2013;27(12):5094–103. Experiment to show that the SCC in humans transduces bitter and sweet taste signals and show antimicrobial peptide secretory responses.
Braun T, Mack B, Kramer MF. Solitary chemosensory cells in the respiratory and vomeronasal epithelium of the human nose: a pilot study. Rhinology. 2011;49(5):507–12. Identification of SCCs in the human sinonasal mucosa.
Finger TE et al. Solitary chemoreceptor cells in the nasal cavity serve as sentinels of respiration. Proc Natl Acad Sci U S A. 2003;100(15):8981–6.
Krasteva G et al. Cholinergic chemosensory cells in the trachea regulate breathing. Proc Natl Acad Sci U S A. 2011;108(23):9478–83.
Saunders CJ, Reynolds SD, Finger TE. Chemosensory brush cells of the trachea. A stable population in a dynamic epithelium. Am J Respir Cell Mol Biol. 2013;49(2):190–6.
An SS et al. TAS2R activation promotes airway smooth muscle relaxation despite beta(2)-adrenergic receptor tachyphylaxis. Am J Physiol Lung Cell Mol Physiol. 2012;303(4):L304–11. Bitter taste receptor stimulation causes downstream bronchodilation.
Deshpande DA et al. Bitter taste receptors on airway smooth muscle bronchodilate by localized calcium signaling and reverse obstruction. Nat Med. 2010;16(11):1299–304.
Robinett KS et al. Bitter taste receptor function in asthmatic and nonasthmatic human airway smooth muscle cells. Am J Respir Cell Mol Biol. 2014;50(4):678–83.
Hayes JE et al. Allelic variation in TAS2R bitter receptor genes associates with variation in sensations from and ingestive behaviors toward common bitter beverages in adults. Chem Senses. 2011;36(3):311–9.
Bufe B et al. The molecular basis of individual differences in phenylthiocarbamide and propylthiouracil bitterness perception. Curr Biol. 2005;15(4):322–7.
Kim UK, Drayna D. Genetics of individual differences in bitter taste perception: lessons from the PTC gene. Clin Genet. 2005;67(4):275–80.
Adappa ND et al. The bitter taste receptor T2R38 is an independent risk factor for chronic rhinosinusitis requiring sinus surgery. Int Forum Allergy Rhinol. 2014;4(1):3–7. Prospective study demonstrating the increased need for FESS among AVI/AVI TAS2R38 genotype in CRS patients.
Antunes MB, Gudis DA, Cohen NA. Epithelium, cilia, and mucus: their importance in chronic rhinosinusitis. Immunol Allergy Clin N Am. 2009;29(4):631–43.
Feldman C et al. The effects of pneumolysin and hydrogen peroxide, alone and in combination, on human ciliated epithelium in vitro. Respir Med. 2002;96(8):580–5.
Min YG et al. Effects of staphylococcal enterotoxin on ciliary activity and histology of the sinus mucosa. Acta Otolaryngol. 2006;126(9):941–7.
Chen B et al. Altered sinonasal ciliary dynamics in chronic rhinosinusitis. Am J Rhinol. 2006;20(3):325–9.
Davis SS, Illum L. Absorption enhancers for nasal drug delivery. Clin Pharmacokinet. 2003;42(13):1107–28.
Naraghi M et al. Nitric oxide: a new concept in chronic sinusitis pathogenesis. Am J Otolaryngol. 2007;28(5):334–7.
Phillips PS et al. Nasal nitric oxide and sinonasal disease: a systematic review of published evidence. Otolaryngol Head Neck Surg. 2011;144(2):159–69.
Adappa ND et al. Genetics of the taste receptor T2R38 correlates with chronic rhinosinusitis necessitating surgical intervention. Int Forum Allergy Rhinol. 2013;3(3):184–7. T2R38 genotype determines necessity for surgical intervention in CRS.
Mfuna Endam L et al. Genetic variations in taste receptors are associated with chronic rhinosinusitis: a replication study. Int Forum Allergy Rhinol. 2014;4(3):200–6. Confirmation that T2R38 genotype is associated with CRS.
Lee RJ, Cohen NA. The emerging role of the bitter taste receptor T2R38 in upper respiratory infection and chronic rhinosinusitis. Am J Rhinol Allergy. 2013;27(4):283–6.
Kalsi KK et al. Glucose homeostasis across human airway epithelial cell monolayers: role of diffusion, transport and metabolism. Pflugers Arch. 2009;457(5):1061–70.
Lemon CH, Margolskee RF. Contribution of the T1r3 taste receptor to the response properties of central gustatory neurons. J Neurophysiol. 2009;101(5):2459–71.
Jiang P et al. Lactisole interacts with the transmembrane domains of human T1R3 to inhibit sweet taste. J Biol Chem. 2005;280(15):15238–46.
Imada T et al. Amiloride reduces the sweet taste intensity by inhibiting the human sweet taste receptor. Biochem Biophys Res Commun. 2010;397(2):220–5.
Bachmanov AA et al. Genetics of taste receptors. Curr Pharm Des. 2014;20(16):2669–83.
Fushan AA et al. Allelic polymorphism within the TAS1R3 promoter is associated with human taste sensitivity to sucrose. Curr Biol. 2009;19(15):1288–93.
Mennella JA, Pepino MY, Reed DR. Genetic and environmental determinants of bitter perception and sweet preferences. Pediatrics. 2005;115(2):e216–22.
Pezzulo AA et al. Glucose depletion in the airway surface liquid is essential for sterility of the airways. PLoS One. 2011;6(1), e16166.
Zhang Z et al. The effect of diabetes mellitus on chronic rhinosinusitis and sinus surgery outcome. Int Forum Allergy Rhinol. 2014;4(4):315–20.
Orsmark-Pietras C et al. Transcriptome analysis reveals upregulation of bitter taste receptors in severe asthmatics. Eur Respir J. 2013;42(1):65–78. Asthmatics have an upregulation of bitter taste receptor expression.
Schroeder BO et al. Reduction of disulphide bonds unmasks potent antimicrobial activity of human beta-defensin 1. Nature. 2011;469(7330):419–23.
Wilson SS, Wiens ME, Smith JG. Antiviral mechanisms of human defensins. J Mol Biol. 2013;425(24):4965–80.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Cohen has a patent “Therapy and Diagnostics for Respiratory Infection” 61/697,652 (filed 12/6/12) WO2013112865 pending. Drs. Workman, Palmer, and Adappa declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Rhinosinusitis
Rights and permissions
About this article
Cite this article
Workman, A.D., Palmer, J.N., Adappa, N.D. et al. The Role of Bitter and Sweet Taste Receptors in Upper Airway Immunity. Curr Allergy Asthma Rep 15, 72 (2015). https://doi.org/10.1007/s11882-015-0571-8
Published:
DOI: https://doi.org/10.1007/s11882-015-0571-8