Abstract
Background
Irisin is a precious hormone-like myokine that plays a key role in glucose/energy expenditure and metabolic regulation This paper aimed to determine the irisin levels in patients with type 1 diabetes mellitus and their correlation with insulin therapy and glycaemic control.
Methods
Ninety type 1 diabetes mellitus patients were collected. The patients were subdivided into two groups: group I (37) newly diagnosed type 1 diabetes mellitus and group II (53) T1DM (on insulin injection); for comparison, 30 healthy individuals were included as control. The serum levels of irisin were estimated using ELISA. FSG and lipid profile were measured through spectrophotometrically. Glycated hemoglobin was determined using High-performance liquid chromatography.
Result
Serum levels of irisin were significantly lower (P = 0.01), as compared to the control group. Also irisin level was significantly lower in group I compared to group II. Fasting serum glucose, glycated hemoglobin, and lipid profile were significantly elevated in patient groups compared to the control group. Serum irisin was negatively correlated to fasting serum glucose, and glycated hemoglobin, whereas it positively correlated to serum lipid profile. In multiple stepwise regression, only glycated hemoglobin (β = − 0.600, P = 0.040) was determined as an independent predictor for predicting the irisin levels. The AUC was excellent (AUC = 0.996, P = 0.0001), with high diagnostic accuracy (88.2) in differentiating newly diagnosed type 1 diabetes mellitus from the healthy subject group.
Conclusion
We demonstrated low irisin levels in type 1 diabetes mellitus and the association of the highest irisin amounts to an insulin therapy and a better glycaemic control. Furthermore, the measurement of irisin levels could be useful as laboratory markers to monitor type 1 diabetes mellitus severity and therapy response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is the most common of all endocrine disorders and is one of the foremost public health concerns confronting the world today [1, 2]. The global statistics of diabetes mellitus in the year 2017 indicated about 425 million people had this disease worldwide and this will rise to 629 million in 2045 [3, 4]. T1DM incidence has been globally rising during the past decades by as much as 3% annually; the cause of which is unknown. If these trends will continue, the total prevalence of people with type 1 diabetes will increase in the coming years [5].
Irisin is a recently identified hormone derived from the fibronectin type III domain-containing (FNDC5) gene that is released mainly from skeletal muscle after exercise or exposure to cold [6] and plays a key regulatory role in browning of white adipose tissue [7]. Irisin has a role in glucose/energy expenditure and metabolic regulation [8], which would be of importance for patients with T1DM. Several studies were held out to investigate irisin’s role in glucose metabolism; however, they ended up with controversial results [9, 10]. Whereas irisin has beneficial effects in rodents, data in humans are insufficient so far to evaluate its metabolic effects and association with metabolic disease. Thus, few data suggest that irisin is associated with insulin sensitivity and a new onset of T2DM [9, 11]. To our knowledge, no extensive research on patients with newly diagnosed (without treatment) and irisin levels have been done. It is crucial to figure out if irisin can be utilized as a supplement in the diagnosis and treatment of T1DM. The goal of this study was to clarify the association between serum irisin levels and T1DM by comparing the levels of irisin in patients with newly diagnosed (without treatment), insulin requirement T1 DM patients, and healthy people.
Materials and methods
Inclusion criteria
Diabetic patients
A total of 90 patients were included in this study (43 females, 47 males), age range (18–40 years), and they were seen from Aug 2023 till Dec 2023 at the National Endocrinology and Diabetes Center in, AL-Mustansiriya University; patients were divided into two groups according to there treatment:
-
(A)
Newly diagnosed (T1DM) without treatment patients (GI):
A group of 37 patients ranging from 18 to 35 years mean (21.10 ± 3.74) were 14 females (37.8%) and 23 males (62.2%), were primarily diabetics, and were not receiving treatment of insulin injections.
-
(B)
Insulin requirement (IR) patients (GII):
A group of 53 patients ranging from 18 to 40 years mean (28.33 ± 6.94) were 29 females (54.7%) and 24 males (45.3%), were primarily diabetics, and were treated with insulin injections. The medical history of the patient was of prime consideration in the selection questionnaire. Each patient was defined according to the presence of at least two of the following criteria: (1) significant keton urea, (2) insulin treatment initiated after diagnosis, (3) weight below the ideal weight for the same sex and age.
Healthy control (HC)
A group of 30 subjects matched for age and sex served as healthy control was 13 (43.3%) females and 17 (56.7%) males age range (18–40)years. None of them was diabetic, according to laboratory findings of FSG value < 98 mg/ who were considered as control. All of them had a negative family history of DM and a negative drug history regarding DM.
Exclusion criteria
Pregnant female patients with diabetic complications and patients with mixed treatment (insulin and antidiabetic agents).
Blood collection
Venous blood samples were aspirated following a 12-h fasting into plain tubes and centrifuged to obtain serum for the measurement of serum irisin level in the fasting state as well as other biochemical tests Another blood sample was aspirated into Hebrenized tube for the measurement of HbA1c.
Estimation of irisin
Serum irisin was estimated by quantitative sandwich enzyme immunoassay technique, using the kit supplied by Cusabio, China. The methods depend on pre-coating the microplate with the specific irisin antibody. Complete assay samples and standards were added to the tests and then bounded occurred when irisin was present in the samples by the immobilized antibody. Later on, unbound substances were removed; the specific conjugated antibody for irisin was added to the samples. Horseradish peroxidase was added to the samples after the washing process was performed. The next washing process was applied to remove the unbound enzyme reagent, and the end product color was developed after substrate solution addition. The intensity of the color was determined after stopping color development.
Determination of diabetic‐related parameters
The enzymatic colorimetric method was used for serum glucose determination using the kit supplied by Bio System, Spain. Serum triglyceride was determined using enzymatic colorimetric reaction according to the Fassati and Prencipe method [12], using the kit supplied by Spinreact, Spain. Serum total cholesterol was estimated using the enzymatic colorimetric method [13], utilizing the kit provided by Spinreact, Spain. Serum HDL was determined as well [14]. While HbA1c was determined using Bio-Rad VARIANT Hemoglobin A1c programmer. The principle was similar to that chromatography “ion–exchange high-performance liquid chromatography (HPLC),” sodium phosphate buffer pH 5.9 has been used as elution buffer 1, and pH 5.6 was used as elution buffer 2. The whole blood primer was a human red blood cell hemolysate. The washing solution was deionized distilled water. The hemolysis reagent that was used was citrate solution. For the calibrator, hemoglobin-A1c was used.
Ethical approval
The studies have been approved by the Committee of the University of Diyala College of Science for Women and have been performed in accordance with the ethical standard as laid down in the 1964 Declaration of Helsinki statement and its later corrections or comparable ethical standards, also according to the ministry of Iraqi health protocols. Informed consent was obtained from all individual participants included in the study.
Statistical analysis
A Statistical analysis program (SPSS 25) was utilized for analyzing the results. The normal distribution test was performed for the variables in this study. The General descriptive statistic was used to describe the main findings; the one-way analysis of variance test was used to compare groups. An independent T-test was used also. The correlation was done using Spearman correlation. Multiple regression models were used to study the independent and net effect of a set of independent (explanatory) variables on the response (dependent or outcome) variable. Also, the receiver operating characteristic curve (ROC) analysis was done to identify the cutoff value for the parameters.
Results
Biochemical and anthropometric characteristics of the study population
Biochemical and anthropometric characteristics of the study population are illustrated in (Table 1). Statistically, no significant differences appeared between studying groups for age and BMI, and biochemical parameters showed a significant increase in the newly diagnosed diabetic group as a comparison with the control group except for HDL-C and serum creatinine are non-significance, while TG and VLDL-C show a significant decrease in the newly diagnosed diabetic patient as a compared with the control group. TG, TC, FSG, HbA1c, and LDL-C showed significant differences between patient groups, while blood urea and serum creatinine showed non-significant differences between the two patient groups.
The irisin for the studied groups
Table 2 showed that irisin levels decreased significantly in the two diabetic groups as compared with the control group, while serum irisin levels showed no significant differences in the G II diabetic group as compared with the GI group.
Serum irisin in patients having T1DM divided according to male and female
Table 3 shows the effect of gender on irisin in studied groups. The results show a higher mean value of irisin has been observed in males as compared to females in GI (newly diagnosed DM), but the level of irisin showed no statistically significant differences among both sexes for DM with insulin therapy.
Correlation analysis of parameters associated with serum irisin level in the study subjects
We investigated the relationship between irisin level and various other parameters in the patients’ group (Table 4). Serum irisin was positively correlated with TG, TC, VLDL-C, and LDL-C. Irisin was negatively correlated with FSG and HbA1c (Table 4). We then performed a multiple stepwise regression to determine variables that had independent associations with serum irisin. The results showed that only total HbA1c was an independent predictor of the levels of irisin (Table 4). In the control group, serum irisin was positively correlated with triglyceride and VLDL-C only. We performed a multiple stepwise regression to determine variables that had independent associations with serum irisin. The results showed that triglycerides and VLDL-C were independent predictors of the levels of irisin (Table 4).
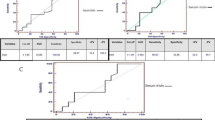
Receiver operator characteristic (ROC) curve analysis
To evaluate the Irisin cutoff value as well as to predict the newly diagnosed DM as diagnostic tests or adjuvant diagnostic tests, receiver operator characteristic (ROC) curve analysis was carried out and the results are shown in Table 5, and Fig 1. The Irisin cutoff value was > 7.02 with sensitivity, specificity, accuracy positive predictive value (PPV), negative predictive value (NPV), and Area under curve of 97.3 %, 96.7 %,88.2% 97.3 %, 96.7% and 0.996 (0.989- 1.000) respectively.
The present results indicate irisin is considered an excellent diagnostic marker. To evaluate the Irisin cutoff value as well as to predict the GII (DM with insulin therapy) as diagnostic tests or adjuvant diagnostic tests, ROC curve analysis was carried out, and the results are shown in Table 6 and Fig. 2. The Irisin cutoff value was > 8.74 with sensitivity, specificity, accuracy, positive predictive value (PPV), negative predictive value (NPV), and area under curve of 94.3%, 96.7%, 83.6%, 98.0%, 90.6%, and 0.809 (0.936–1.000), respectively.
Discussion
The most important finding of our study was that serum irisin levels were decreased in subjects with T1DM in comparison with healthy controls. In addition, among subjects with T1DM, elevated irisin levels are closely related to better insulin therapy and improved glycemic control. Consistently, T1DM patients on insulin injections showed higher irisin levels than patients without treatments. Irisin is a peptide hormone cleaved from FNDC5, which can be released into the circulation [15]. Since its discovery, irisin has been found to be associated with various diseases, including metabolic diseases and cancers [16]. Recently, it has been reported that irisin promoted insulin synthesis as well as glucose-stimulated insulin secretion [17]. In addition, irisin overexpression improved insulin sensitivity in mice while decreasing hyperlipidemia and hyperglycemia [18], suggesting that irisin could have a key role in diabetes management. Some studies evaluated irisin levels between patients with T1DM and healthy individuals and revealed contrasting outcomes as compared to those of our study [19, 20]. According to our findings in all groups, females showed a decrease in irisin levels compared to males. The result found a significant difference in irisin levels between males and females in patients without insulin therapy group. But no significant difference in irisin levels at the two genders in the treatments diabetic patient group. Some studies suggest that sex differences in the adiposity distribution play a role in the different cardiometabolic risks of men and women [21], but an exact role for irisin in this issue would need future studies. Being a product of the skeletal muscle is not strange that serum irisin levels are different between sexes; this may be due to that women have much less skeletal muscle mass [22], and their irisin values are lower than those of men. This means that treatment with insulin injection is more effective in males than in females.
Furthermore, our study revealed that serum irisin levels are inversely linked with HbA1c. Studies conducted with patients with T1DM and metabolic syndrome have not been interpreted these relation. HbA1c is an indirect indicator of hyperglycemia, suggesting that the elevated myokine levels “predicted” a better metabolic control in these patients [19, 23]. Although these data are in contrast with Ates’s results that found a positive correlation between plasma irisin levels with HbA1c, it could be due to the different cohort of T1DM patients tested as well as to the different ELISA kit used to measure the myokine concentration [20]. In the current study, serum irisin levels showed a highly predictive factor for screening type 1 diabetes. Thus, the measurement of irisin serum levels could represent a suitable tool to simultaneously monitor glycaemic in T1DM patients. Furthermore, the measurement of serum irisin levels could also be useful as a laboratory marker to monitor T1DM severity and therapy response.
This study has also some strengths, the first step was to age-match the three groups. Second, newly diagnosed T1DM patients were included, the majority of whom did not have access to insulin injections. Third, patients with T1DM were only given one type of treatment. In addition, the patients were divided into subgroups depending on the duration of the disease. Finally, participants were randomly selected from the general population under normal living conditions. Also, several limitations are as follows: firstly, our sample size was limited patients in one institution, and undoubtedly, our findings will need to be validated in a larger population and multiple institutions. Secondly, we did not correlate serum irisin levels with other T1DM biomarkers such as autoantibodies, due to the lack of availability of these data. Finally, the response of serum irisin to insulin treatment and whether serum irisin-guided therapy can achieve additional benefits for insulin patients are unclear.
Conclusions
Lower irisin levels were determined in T1DM patients compared to the control group. The association of the highest irisin amounts to an insulin therapy and a better glycaemic control. This may suggest that insulin therapy can be effective in the synthesis of irisin. Furthermore, the measurement of serum irisin levels could also be useful as a laboratory marker to monitor T1DM severity and therapy response. Future direction studies on serum irisin-guided therapy can achieve additional benefits for TIDM patients.
Data availability
(ROC) analysis revealed the diagnostic accuracy of using irisin concentrations to distinguish patient groups from healthy control subjects.
Abbreviations
- T1DM:
-
Type 1 diabetes mellitus
- FSG:
-
Fasting blood sugar
- HbA1c:
-
Glycated hemoglobin
- BMI:
-
Body mass index
- HDL:
-
High-density lipoprotein
- LDL:
-
Low density lipoprotein
- ROC:
-
Receiver operating characteristic curve
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- VLDL:
-
Very low-density lipoprotein
References
Jaid HK, Khaleel FM, Salman IN, Abd BA (2023) Estimation of apelin levels in Iraqi patients with Type II diabetic peripheral neuropathy. Baghdad Sci J 20(5):1684–1691
Abed BA, Farhan LO, Dawood AS (2024) Relationship between serum nesfatin-1, adiponectin, resistin concentration, and obesity with type 2 diabetes mellitus. Baghdad Sci J 21(1):0117
Cho NH, Shaw JE, Karuranga S et al (2018) IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract 138:271–281
Shaban A, Abbas SA, Abed BA (2023) Estimation of Tenascin-C Levels in Iraqi patients with diabetic nephropathy. Al-Rafidain J Med Sci 5(1S):S8–13. ISSN 2789-3219
Guariguata L (2011) Estimating the worldwide burden of type 1 diabetes. Diabetes Voice 56(2):6–8
Rana KS, Pararasa C, Afzal I et al (2017) Plasma irisin is elevated in type 2 diabetes and is associated with increased E-selectin levels. Cardiovasc Diabetol 16:147. https://doi.org/10.1186/s12933-017-0627-2
Arhire LI, Mihalache L, Covasa M (2019) Irisin: a hope in understanding and managing obesity and metabolic syndrome. Front Endocrinol (Lausanne) 10:524
Perakakis N, Triantafyllou GA, Fernández-Real JM et al (2017) Physiology and role of irisin in glucose homeostasis. Nat Rev Endocrinol 13(6):324–337. https://doi.org/10.1038/nrendo.2016.221
Alis R, Sanchis Gomar F, Pareja Galeano H et al (2014) Association between irisin and homocysteine in euglycemic and diabetic subjects. Clin Biochem 47(18):333–35
Choi YK, Kim MK, Bae KH et al (2013) Serum irisin levels in new-onset type 2 diabetes. Diabetes Res Clin ract 100(1):96–101
Diabetes A (2012) Association Diagnosis and classification of diabetes mellitus. Diabet Care 36:S67–S74
Fossati P, Prencipe L (1982) Serum triglycerides determined colorimetrically with an enzyme that produces hydrogen peroxide. Clin Chem 28(10):2077–2080
Richmond W (1974) Proceedings in the development of an enzymatic technique for the assay of cholesterol in biological fluids. Clin Sci Mol Med 46(1):6P–7P
Naito HK (1984) High-density lipoprotein (HDL) cholesterol. In: Kaplan A et al. Clin Chem. C.V. Mosby Co., St Louis, pp 1207–1213 and 437
Boström P1, Wu J, Jedrychowski MP et al (2012) A PGC1-alpha-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature 481:463–468
Chen N, Li Q, Liu J, Jia S (2016) Irisin, an exercise-induced myokine as a metabolic regulator: an updated narrative review. Diabetes Metab Res Rev 32:51–59
Natalicchio A, Marrano N, Biondi G et al (2017) The myokine irisin is released in response to saturated fatty acids and promotes pancreatic β-cell survival and insulin secretion. Diabetes 66:2849–2856
Xiong XQ, Chen D, Sun HJ et al (2015) FNDC5 overexpression and irisin ameliorate glucose/lipid metabolic derangements and enhance lipolysis in obesity. Biochim Biophys Acta 1852:1867–1875
Faienza MF, Brunetti G, Sanesi L et al (2018) High irisin levels are associated with better glycemic control and bone health in children with Type 1 diabetes. Diabetes Res Clin Pract 1(141):10–17
Ates I, Arikan MF, Erdogan K et al (2017) Factors associated with increased irisin levels in the type 1 diabetes mellitus. Endocr Regul 51(1):1–7
Yang Y, Xie M, Yuan S et al (2021) Sex differences in the associations between adiposity distribution and cardiometabolic risk factors in overweight or obese individuals: a cross-sectional study. BMC Public Health 21:1232. https://doi.org/10.1186/s12889-021-11316-4
Yang Y, Xie M, Yuan S et al (2021) Sex differences in the associations between adiposity distribution and cardiometabolic risk factors in overweight or obese individuals: a cross-sectional study. BMC Public Health 21(1):1232
Espes D, Lau J, Carlsson PO (2015) Increased levels of irisin in people with long-standing type 1 diabetes. Diabet Med 32:1172–1176
Acknowledgements
We owe our deepest gratitude to the University of Diyala, College of Science.
Author information
Authors and Affiliations
Contributions
Dhifaf A. Abdulabbas: methodology, software, and data curation. Ekhlas Abdallah Hassan: conceptualization, writing—original draft preparation, visualization, investigation, software, validation, writing—reviewing and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlight
• Irisin is a new biomarker candidate in type 1 diabetes mellitus.
• Irisin can be used to differentiate newly diagnosed T1DM from healthy subjects.
• Irisin change depends on the severity of diseases (disease severity depends on increased HbA1c) of T1DM.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abdulabbas, D.A., Hassan, E.A. A case–control study to evaluate irisin levels in patients with type 1 diabetes mellitus. Ir J Med Sci 193, 1275–1282 (2024). https://doi.org/10.1007/s11845-024-03626-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-024-03626-4