Abstract
The diagnosis of central pontine hyperintensities on cranial magnetic resonance imaging has wide-spectrum clinical entities, and the pro-type diagnosis of these is central pontine myelinolysis. The rapid changes in extracellular environment due to an imbalance of electrolytes or metabolic or toxic stress to the myelin sheath can cause demyelination of white matter tracts in pons, which is why this situation could have different etiologies than just rapid sodium changes. Central pontine myelinolysis can be presented with different clinical scenarios from asymptomatic to death. Here, we present eight patients who had central pontine hyperintensities on radiological imaging but showed various clinical symptoms and different etiologies. The etiologies of these cases are hypertriglyceridemia, alcohol consumption, antidepressant usage, immunocompromised situations, uncontrolled diabetes mellitus, liver and kidney failure, electrolyte changes, and adrenal insufficiency. We aimed to take attention with this case series to the fact that not only fast correction of hyponatremia is the cause of central pontine myelinolysis, but also different etiologies could play a role in this situation, and making the central pontine myelinolysis diagnosis considering different diagnosis is very important.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Central pontine myelinolysis (CPM) is a clinical condition in which non-inflammatory myelin sheath degradation within basilar parts of the pons occurs with sudden osmotic changes in extracellular fluids (ECF) [1]. CPM is the most common clinical presentation of osmotic demyelination syndrome (ODS) because the white matter tracts of the pons are vulnerable to extracellular osmotic changes; it is basically a metabolic myelin sheath disorder [2]. Along with the frequent use of magnetic resonance imaging (MRI), asymptomatic CPM can also be detected in clinical practice. These patients usually have comorbidities that make them susceptible to demyelination because of the metabolic stress to the myelin sheath [3], but clinicians also come across the radiological diagnosis of CPM in patients without any symptoms referable to the pons or comorbidities susceptible to CPM [4]. Differential diagnoses such as multiple sclerosis, brainstem posterior reversible encephalopathy syndrome, brainstem infarction, central nervous system (CNS) lymphoma, pontine gliomas, brainstem metastasis, CNS vasculitis, and even CLIPPERS (chronic lymphocytic inflammation with pontine perivascular enhancement syndrome) should be kept in mind in these patients before diagnosis as CPM [1]. Here, we present below our eight symptomatic and asymptomatic different cases showing diverse types of central pontine hyperintensities with a differential diagnosis of CPM syndromes.
Cases and results
Case report 1
A 50-year-old male patient who had a history of hypertension and depression was admitted to our neurology clinic with difficulty concentrating. His habits are drinking alcohol (147 g every other day for 30 years) and smoking. He was using olmesartan and amlodipine for hypertension and paroxetine for depression. The neurological examination was normal. His triglyceride level was 819.2 mg/dL, and his total cholesterol level was 242.5 mg/dL; other blood parameters were normal. MRI revealed T2-weighted and FLAIR (Fluid-Attenuated Inversion Recovery) image hyperintensity in the central part of the pons with a normal periphery (Fig. 1), no enhancement of contrast. The cranial-cervical vascular workup was clear. The cardiac examination showed no pathology. Fibrate and statins were started by internal medicine. Malignity research and the rheumatological investigation were clear. For further examination, a lumbar puncture (LP) was suggested, but he refused. Three months later, his follow-up MRI showed the same image.
Case report 2
A 62-year-old diabetic man presented with dizziness and difficulty remembering recent events for 3 months. He had no history of smoking or alcohol consumption. His medications are acetylsalicylic acid, metformin, and beta-blockers. The neurological examination was normal except for MMSE (mini-mental state examination) 27/30. His triglyceride level was 737.2 mg/dL, HbA1c was 8.41, and the total cholesterol level was 301.9 mg/dL. Other parameters were normal. MRI revealed T2-weighted and FLAIR image trident-shaped hyperintensity in the central part of the pons with normal periphery (Fig. 2), no enhancement of contrast. The cranial-cervical vascular workup was clear. Fibrate and statins were started. The rheumatological, hematological, and oncological workup was normal. For further examination, LP was suggested, but he refused, and no follow-up MRI could be performed either.
Case report 3
A 38-year-old housewife who had a history of hypothyroidism, atypical chronic myeloproliferative disease (CMPD), hyperlipidemia, and depression admitted to a neurology clinic with chronic headache and dizziness. Her current medications were escitalopram and levothyroxine sodium. The neurological examination was normal. On her complete blood count, the white blood cells were 17.1 per microliter (neutrophils: 53.8%, basophils: 0.4%, eosinophils: 2.7%, lymphocytes: 36.6%, monocytes: 6.5%); other parameters were in the normal range. Her JAK-2 V617F mutation was negative, the bone marrow biopsy was normal, and BCR-ABL gene testing for CML was negative. Her other pathological blood chemistry results were TSH level 5.52 mIU/L, LDL cholesterol level 196.26 mg/dL, and total cholesterol level 276.8 mg/dL. The MRI revealed T2-weighted and FLAIR image trident-shaped hyperintensity in the central part of the pons with normal periphery (Fig. 3), no enhancement of contrast. Cranial vascular workup was clear. MR spectroscopy (MRS) was performed for the lesion, and it was more likely CPM. Cerebrospinal fluid (CSF) showed no pathology, including oligoclonal band screening, aquaporin 4, and MOG (myelin oligodendrocyte glycoprotein) antibodies. The rheumatological and oncological workup was clear. Three months later, her follow-up MRI showed the same image.
Case report 4
A 60-year-old female patient known to have migraines admitted to our neurology clinic with a headache that was different from routine migraine attacks. She had been regularly using duloxetine and frovatriptan and smoking for 20 years. She also had type 2 diabetes mellitus (DM) and depression. Her neurological examination was normal. The blood examination was normal except for the pre-prandial glucose level, which was 167 mg/dL. Metformin was started by internal medicine. Her MRI revealed T2-weighted and FLAIR image hyperintensity in the central part of the pons with a normal periphery (Fig. 4), no contrast enhancement. Cranio-cervical vascular workup was normal. MRS did not support the intracranial tumor; it showed a more likely CPM. The rheumatological and oncological workup was clear. For further examination, LP was suggested, but she refused it. After three months, her follow-up MRI showed the same lesion but a pale version.
Case report 5
A 40-year-old female patient presented to a clinic with a headache and blurry vision. The medical history included ankylosing spondylitis (AS), benign intracranial hypertension (BIH), hypothyroidism, and hyperlipidemia. She had been regularly using sulfasalazine for AS but stopped taking acetazolamide for BIH one month ago. After that, her complaints started and showed a slow progression. Her examination showed grade 1 papilledema. She has total cholesterol level of 268.4 mg/dL, LDL cholesterol level of 181.44 mg/dL, a triglyceride level of 169.3 mg/dL, and a TSH level of 5.12 mIU/L. Other parameters were normal, including electrolytes. Her MRI revealed T2-weighted and FLAIR image hyperintensity in the central part of the pons with a normal periphery (Fig. 5), but no enhancement of contrast. The CSF opening pressure was 28 cm/H2O, and all other parameters were normal, including oligoclonal bands, aquaporin 4, and MOG antibodies. Intracranial and extracranial arterial and venous vasculature were normal. The rheumatological, oncological, and hematological investigations were clear. Six months later, her follow-up MRI showed the same image.
Case report 6
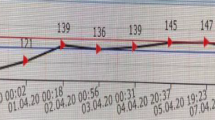
A 30-year-old man was admitted to the emergency department (ED) with complaints of numbness in his hands and feet. He had a history of heavy smoking and had abused alcohol (150–200 g daily) for 10–15 years. The symptoms began three days after quitting alcohol. He was taking paliperidone and escitalopram for depression. Initial neurological examination; confusion, stocking-glove sensory loss; normal general examination. The patient was treated with IV isotonic and 7.5% potassium chloride treatment. One day later, his examination showed more confusion, disorientation, and limitation of cooperation. He followed up intubated in the intensive care unit (ICU) for 6 days. On the sixth day of his admission in the neurological examination, as pathological findings, minimal confusion, 3/5 tetra-paresis, and bilateral extensor plantar response were determined. All laboratory findings are in Table 1. The cranial MRI revealed T2-weighted and FLAIR trident-shaped image hyperintensity in the central part of the pons with a normal periphery (Fig. 6), but no enhancement of contrast. MRS was performed for the lesion, and it was more likely CPM. Physical therapy and rehabilitation were performed, and his motor deficit improved daily. In his 9th month evaluation, repeated MRI showed regression of the CPM (Fig. 6c), and no motor or sensory deficit was left.
Case report 7
An 86-year-old female patient presented to ED with a generalized tonic-clonic seizure. Her comorbidities were controlled diabetes mellitus, hypertension, hyperlipidemia, and hypothyroidism. The detailed medical history: seven months ago, she was followed up in ICU due to an adrenal insufficiency condition secondary to a pituitary adenoma, and she underwent transsphenoidal surgery. She did not have any bad habits. Her vital signs and neurological and general examination were normal. The blood examination showed no pathology. The MRI revealed FLAIR image hyperintensity in the central part of the pons (Fig. 7). A contrast MRI or further examination could not be performed because she refused it. A further examination could not be performed, and a differential diagnosis could not be eliminated; however, due to the trident-shaped image similarity and the adrenal insufficiency history, a preliminary CPM diagnosis was made.
Case report 8
A 69-year-old woman was admitted to a neurology clinic with gait disturbances for 2 years. Medical history had controlled diabetes mellitus, hypertension, and hyperlipidemia. She had no history of smoking or alcohol consumption. Her neurological and general examinations were normal. The blood examination did not show any pathology. MRI revealed T2-weighted and FLAIR image hyperintensity in the central part of the pons with a normal periphery (Fig. 8) and mild cerebellar atrophy, but no enhancement of contrast. Repeated MRIs showed the same lesion. Cranio-cervical vascular workup was normal. For further investigation, MRS was performed, and it was more likely CPM. Rheumatological and oncological investigations were clear. She refused the CSF examination. Three months later, her follow-up MRI showed the same image.
Discussion
The pathophysiology of CPM is complicated, but the main compensatory mechanism of the intracellular environment is being late to rapid changes in extracellular osmotic rise [1, 5, 6]. Sodium is the key electrolyte of ECF, which is why rapid sodium changes are common causes of CPM. But there are other clinical states that are reported with CPM, such as DM, malnutrition, chronic alcoholism, liver transplantation, immunosuppression, renal failure, hypokalemia, adrenal insufficiency, and even depression with antidepression usage [2, 6,7,8,9,10,11,12]. CPM has a wide range of medical conditions from death to asymptomatic [3, 12, 13]. Neuropsychiatric symptoms like depression, apathy, difficulty concentrating, or forgetfulness of recent events can also be seen in patients [6, 11, 12]. The symptoms of our first three cases are difficulty concentrating, forgetfulness, and dizziness; two cases with headaches are asymptomatic regarding pontine lesion; one has an ICU history because of adrenal insufficiency; and one has tetra-paresis and stupor stage. As far as we know, there is no documented relationship between hypertriglyceridemia and CPM. The first two cases have severe hypertriglyceridemia. One case has DM, and the other is a chronic alcoholic. These conditions can induce myelin sheath degradation with apoptosis or fluctuate the extracellular osmotic environment [7, 8]. The first case has hypertriglyceridemia and takes regular paroxetine for depression. CPM cases associated with fluoxetine and clomipramine have been reported, possibly due to myelin toxicity or antidepression-induced syndrome of inappropriate antidiuretic hormone secretion (SIADH) without hyponatremia [10,11,12]. The third and fourth cases are also using escitalopram and duloxetine. In the third case, she is also immunosuppressed due to atypical CMPD. Similarly, the fifth case uses sulfasalazine as an immunosuppressive medication for AS. Acquired immunosuppression created by drugs such as tacrolimus and cyclosporine-induced CPM after liver transplantation without any reason to explain the demyelination is reported; even these could be asymptomatic cases [13, 14]. An immunosuppressive state could be created by chronic alcoholism that also triggers demyelination with or without obvious electrolyte changes [2, 3, 15]. We can also see the combination of etiological factors, and which one is the key factor cannot be decided, like in our sixth case. More than one electrolyte fluctuation can change the extracellular environment and create stress on the myelin sheath, as in cases of adrenal insufficiency syndrome [9].
Conclusion
In the process of time along with the literature, CPM cases without hyponatremia can be seen. Clinicians can even come across asymptomatic cases with different etiologies, while making the diagnosis of CPM different differential diagnosis has similar pontine hyperintensities should be considered and patients should be investigated carefully.
References
Danyalian A, Heller D (2023) Central pontine myelinolysis. In: StatPearls [Internet]. StatPearls Publishing, Treasure Island (FL)
Oke IO, Mughees W, Patel H et al (2021) A case of osmotic demyelination syndrome in a chronic alcoholic with moderate hyponatremia. Cureus 13(5):e15129
Shah SO, Wang A, Mudambi L et al (2012) Asymptomatic central pontine myelinolysis: a case report. Case Rep Neurol 4(3):167–172
Kleinschmidt-DeMasters BK, Anderson CA, Rubinstein D (1997) Asymptomatic pontine lesions found by magnetic resonance imaging: are they central pontine myelinolysis? J Neurol Sci 149(1):27–35
Singh TD, Fugate JE, Rabinstein AA (2014) Central pontine and extrapontinemyelinolysis: a systematic review. Eur J Neurol 21(12):1443–1450. https://doi.org/10.1111/ene.12571
Alsaid HM, Naser AM (2019) Central pontine myelinolysis, osmotic demyelination syndrome due to rapidly decreased fluid intake in a schizophrenic patient with psychogenic polydipsia: a case report and review of the literature. Med Case Rep 5:94
Yadav SK, Ojha R, Parajuli N et al (2022) Occurrence of osmotic demyelination syndrome in diabetes mellitus: a case report and literature review of various etiologies for osmotic demyelination syndrome. SAGE Open Med Case Rep 10:2050313X221135595. https://doi.org/10.1177/2050313X221135595
Shrestha S, Kharel S, Gautam S et al (2023) Pontine and bilateral cerebellar lesion in osmotic demyelination syndrome associated with uncontrolled type II diabetes mellitus: a case report. Ann Med Surg 85(3):515–518
Brunner JE (1985) Central pontine myelinolysis in a patient with adrenal insufficiency. Henry Ford Hosp Med J 33(1):45–47. PMID: 4019226
Liu YC, Yang YK, Chen PS, Chang WH (2021) Central pontine myelinolysis in a normonatremic patient with depression. Clin Psychopharmacol Neurosci 19(3):564–567. https://doi.org/10.9758/cpn.2021.19.3.564
Twardowschy CA, Bertolucci BC, Gracia CM (2007) Pontine and extrapontine osmotic myelinolysis after the syndrome of inappropriate secretion of antidiuretic hormone (SIADH) associated with fluoxetine: case report. Arq Neuropsiquiatr 65(3B):858–864. https://doi.org/10.1590/s0004-282x2007000500027
Lupato A, Fazio P, Fainardi E et al (2010) A case of asymptomatic pontine myelinolysis. Neurol Sci 31(3):361–364. https://doi.org/10.1007/s10072-009-0215-7
Fryer JP, Fortier MV, Metrakos P, Verran DJ et al (1996) Central pontine myelinolysis and cyclosporine neurotoxicity following liver transplantation. Transplantation 61(4):658661. https://doi.org/10.1097/00007890-199602270-00026
Patel K, Menon J, Shanmugam N et al (2022) Tacrolimus-induced central pontine myelinolysis in a pediatric liver transplant recipient. J Clin Exp Hepatol 12(2):714–715. https://doi.org/10.1016/j.jceh.2021.07.011
Tiwari R, Kumari A (2022) Central pontine myelinolysis: a case report. Indian J Crit Care Med 26(9):1049–1051
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The ethics committee approval of this study was received by the Health Sciences University Fatih Sultan Mehmet Training and Research Hospital Clinical Research Ethics Committee.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Erkalaycı, C., Ramazanoğlu, L. & Gözke, E. Symptomatic and asymptomatic pontine hyperintensities: are they central pontine myelinolysis? Case series. Ir J Med Sci 193, 993–997 (2024). https://doi.org/10.1007/s11845-023-03538-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-023-03538-9