Abstract
Background
Smoking continues to cause harm on a huge scale in Ireland. Doctors can help this harm through providing safe, effective and clinically sound stop smoking care, but the needs of Irish doctors in this area are largely uncharted.
Aims
We assessed the knowledge, attitudes and practices of Irish doctors regarding stop smoking care and electronic cigarettes.
Methods
An Internet-based cross-sectional survey was administered to members of the Royal College of Physicians in Ireland and the Irish College of General Practitioners. Descriptive statistics for key parameters were derived and factors associated with more consistent practice of brief intervention, a key component of stop smoking care, were analysed using chi-square testing.
Results
There were 250 responses (58.7% female, 53.0% aged under 45 years, 55.1% graduated in medicine before 2000 and 57.2% worked in general practice). Most (84.9%) reported often or always asking about patient’s smoking behaviour, and most (86.1%) reported often or always advising patients to stop. However, providing or arranging effective stop smoking care was weak and less consistently practised, and while most (91.4%) saw it as a responsibility, few doctors (28.5%) agreed they were sufficiently trained in this area of clinical care. Confidence in the knowledge of e-cigarettes was poor.
Conclusions
While there is a strong reservoir support and areas of good reported practice in stop smoking care among doctors in Ireland, the development of their knowledge and skills in arranging effective care should be supported if doctors are to fulfil their huge potential role in tackling the harm caused by smoking.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite progress in controlling tobacco use, Ireland is continuing to experience an epidemic of smoking-related harm on a staggering scale. Smoking is still the leading cause of preventable ill-health, disability and premature death in Ireland, with the greatest burden borne by the poorest groups [1]. The impact of smoking on health services in Ireland remains substantial, causing over 1,000 hospitalisations each week [2] and costing over €500 million each year [3].
The 2021 Healthy Ireland Survey reported that 18% of Irish adults currently smoke; however, most want to stop, and many report making attempts to stop in the previous year [4]. Ensuring people who smoke have help to stop is a core element of the World Health Organization’s MPOWER model and emphasised in Article 14 of the Framework Convention in Tobacco Control [5, 6].
Despite well-established evidence that accessing help, comprising behavioural support and stop smoking medicines, increases the chance that someone who smokes can successfully stop smoking [7], too many people in Ireland report trying to stop without support. People who smoke are more likely to have ill-health and use health services than people who do not; yet in Ireland, only 40% of people who smoke saw a GP, and 30% who saw a hospital doctor in the past 12 months reported that there was discussion of ways of quitting smoking [8]. The evidence that a doctor simply raising the issue with someone who smokes has a large and significant impact on the likelihood of making an attempt to stop underlines the huge, missed opportunity [9]. This is not unique in Ireland. The Royal College of Physicians in the UK has identified the scale of missed opportunities across the health services to systematically identify and support people who smoke to stop as a quality of care failing “hiding in plain sight” [10]. In the USA, over 50 years on from the landmark surgeon general report on the harms of smoking, the current surgeon general dedicated his 2020 to smoking cessation and noted that a consistent approach to evidence-based stop smoking care across health services could enable half a million people who smoke to stop each year [11]. The first National Stop Smoking Guidelines were formally endorsed by the Irish Nationally Clinical Effectiveness Committee in 2022 and launched by the Minister of Health in 2022. These guidelines do not recommend that healthcare professionals advise people who smoke to use u-cigarettes as a support to stop smoking.
Put simply, the provision of good stop smoking care by doctors is a question of good clinical care.
A key focus within the current national tobacco control policy and the HSE Tobacco Free Ireland Programme Plan is strengthening the approach to stop smoking care nationally as an integral component of safe, good-quality and person-centred care [12, 13]. To better support this focus, in 2022, Ireland’s first national clinical guidelines on helping people to stop smoking were approved by the National Clinical Effectiveness Committee and launched by the Minister for Health [14]. The publication of these national clinical guidelines emphasises the centrality of stop smoking care to good clinical care.
While there have been some national assessments of stop smoking care, including a focus on maternity services [15], mental health services [16], hospital services [17] and HSE staff generally [18], there has been no recent national service evaluation focusing specifically on stop smoking care knowledge, attitudes and practices among Irish doctors. Such a service evaluation would provide a useful baseline and informs actions to support the implementation of recently published national stop smoking guidelines. Electronic cigarettes have recently emerged as a disruptive technology given the surrounding debate on the relative harms, benefits and diverse regulation strategies [19]. There is a particular need to address the gap in understanding how Irish doctors are approaching the dilemmas raised in day-to-day practice. In addition, the emergence of COVID-19 has hugely impacted the delivery of all health services in Ireland [20], and given the relationship between increased risk of severe COVID-19 disease and smoking [21, 22], there is a need to understand how recent issues have affected the delivery of stop smoking care.
Recognising the continuing harm caused by smoking and the central role medical professionals can play in tackling this, the Royal College of Physicians in Ireland established a Policy Group on Tobacco to provide medical leadership, advice and advocacy for action towards a Tobacco Free Ireland [12, 23]. In 2020, it identified a need to evaluate stop smoking care services provided by doctors nationally to better understand the reported practices and view of medical professionals on stop smoking care in general, and specifically on e-cigarettes, so that it could provide leadership in stop smoking service development. The aim of this study is to assess the current practices, beliefs and knowledge of physicians in Ireland regarding tobacco smoking and electronic cigarettes.
Methods
A cross-sectional survey of Irish doctors was conducted by the Tobacco Policy Group of the Royal College of Physicians in Ireland to assess the needs of doctors and inform advice and action it could take to better support doctors in stop smoking care. A questionnaire was developed to assess the knowledge, attitudes and reported practices of Irish doctors regarding stop smoking care, including the issue of electronic cigarettes. The survey was administered using an online platform and was distributed by email to members of the Irish College of General Practitioners and the Royal College of Physicians Ireland in August 2020 (total n = 14,075). The communication to participants included information on the purpose of the survey, why participants were selected, voluntary nature of involvement and how information would be processed and used. Participation in the study was based on consent.
Data were collated and analysed using Excel and JMP, a statistical software programme. Descriptive summary statistics were derived, and some key parameters were compared across participants using chi-square hypothesis testing [24]. Individual responses of “always” or “often” were combined across four key reported practices aligned with the brief intervention “3 A’s” model (“of the patients you saw in the last 12 months”: (1) “how often did you ask them about their smoking behaviour?”; (2) “how often have you advised patients to quit smoking?”; (3) “how often have you referred patients to nationally funded quit services?”; and (4) “how often did you prescribe tobacco cessation therapies?”) to identify respondents who reported more consistently applying these practices (score of 3 or 4 out of a maximum of 4). Responses to other key questions on respondent characteristics and stop smoking care motivation, attitude and self-assessed capability were tested for association with more self-reporting and more consistent application of brief intervention practices. Thematic content analysis was applied to open-ended free text comments [25], using the traditional “long table and scissors” methods and with reference to the capability, opportunity and motivation (COM-B) framework [26].
Results
Overview of respondents
There were 250 doctors who completed the survey (response rate 1.8%). In total, 58.7% were female, 53.0% were aged under 45 years, 55.1% graduated in medicine before 2000, 57.2% reported they worked in general practice, 19.4% worked as consultants across a range of specialties, and the remainder were non-consultant hospital doctors or retired.
Regarding their own smoking behaviour, 65.5% of doctors reported that they never smoked, 33.2% reported previously smoked but were now stopped, and 1.3% reported that they currently smoked. Most respondents reported that they have never tried e-cigarettes (93.2%), 3.8% had tried but were not current users of e-cigarettes, and 3.0% were current users of e-cigarettes.
Reported current practices
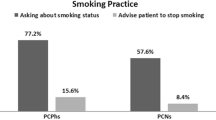
Respondents reported seeing on average 6.3 patients each day who smoked (standard deviation 4.7, range 0–20). Regarding practices in the last 12 months (Fig. 1), most (84.9%) reported often or always asking about patient’s smoking behaviour; while in contrast, only 31.4% often or always asked about e-cigarettes, and 17.0% often or always asked about second-hand smoke exposure. Most (86.1%) reported often or always advising patients to quit smoking. Almost half (52.4%) reported often or always prescribing tobacco cessation therapies. However, only 29.5% reported often or always successfully assisting patients who smoke to quit, and only 27.4% reported often or always referring patients to nationally funded quit services. Most respondents (78.1%) never recommend e-cigarettes to patients.
Capability, opportunity and motivation to help patient stop smoking
Smoking was ranked as the first or second cause of preventable illness by most respondents (93.3%); however, many underestimated the deaths attributable to smoking each week in Ireland (40.5% incorrectly estimated this was less than 80 deaths, 38.6% correctly estimated this was between 80 and 120 deaths [1], and 20.9% over-estimated this figure). While most (84.9%) were aware of the QUIT.ie resource, few respondents (11.2%) had participated in tobacco cessation counselling or brief intervention training in the past year, and few (18.5%) were aware of the HIQA health technology assessment of smoking cessation interventions.
As illustrated in Fig. 2, in general, motivation and attitudes towards helping patients to stop smoking were positive; 91.4% agreed that advising their patients to stop was their responsibility, 70.0% agreed that advice on smoking cessation from a doctor was effective, 77.3% agreed that advice on smoking cessation from a doctor was effective, 89.6% agreed that cessation interventions help decrease tobacco-related diseases, and 80.9% agreed that cessation interventions are cost-effective. However, views on capability were more mixed; only 28.5% agreed they were sufficiently trained in cessation interventions, less than half (45.2%) agreed that they know the best cessation intervention to choose for patients, and only 59.7% agreed they know about what cessation counselling services are available in their service area. There was very strong support for more training on cessation, with 89.9% agreeing this should be taught at the undergraduate level and 90.9% agreeing this should be taught at the postgraduate level.
Respondents reported mixed views on their confidence regarding the provision of smoking cessation care. While most (87.0%) were confident or very confident about their ability to discuss smoking with patients, only half (50.7%) were confident or very confident about their ability to help patients to quit, and 61.3% were confident about their knowledge of cessation therapies.
As demonstrated in Fig. 3, when asked regarding e-cigarettes’ harmfulness, 52.7% agreed these were less harmful than tobacco cigarettes, while 17.3% disagreed with this statement, and 30.0% were neutral. However, 70.5% agreed that e-cigarettes could be a gateway to tobacco cigarette use, and only 15.0% agreed that e-cigarettes should be recommended as a cessation tool, while 53.2% disagreed with this statement and 31.8% were neutral. In total, under a quarter of respondents (23.0%) reported being confident or very confident in their knowledge of e-cigarettes.
In relation to opportunities for smoking cessation care, as illustrated in Fig. 4, over two-thirds of respondents identified at least one barrier: insufficient time (69.5%), patients not taking advice on board (46.5%), and being too busy (41.3%) were the top three reported barriers. Only 16.0% of respondents identified no time to do training as a barrier.
Analysis of comments in free text on potential barriers and enablers identified similar themes (Fig. 4). Patient with low or no intention to quit (theme 1), time required to engage in motivating patients (theme 2) and training for staff (theme 3) were predominant and recurring in comments on barriers, for example: “many patients are not ready or are not contemplating smoking cessation … they have other worries especially in socially deprived areas” (theme 1); “often times the patient has other issues to be dealt with in the consultation and smoking is mentioned at the end” (theme 2); “need training in behavioural interventions and motivational interviewing as we have great trust and knowledge of our patients but lack the experience and tricks of behaviour change theory” (theme 3). Increased supply and access to services (theme 1), including overcoming financial barriers for patients (sub-theme 1.1), training for staff (theme 2) and more supportive policy environment (theme 3) were predominant and recurring in comments on enablers, for example: “more smoking cessation clinics in locality” (theme 1); “it should be free and perhaps pharmacies should be able to dispense like the morning after pill” (sub-theme 1.1); “training. All Drs offered to do a Cert in it” (theme 2); “more laws restricting smoking… continued efforts to make it less acceptable” (theme 3).
COVID-19 and smoking
Most respondents (80.7%) agreed that people who smoke are more likely to suffer severe complications of COVID-19. However, 27.5% reported less patients seeking cessation services during the COVID-19 pandemic and 50% of physicians reported more restricted access to tobacco cessation services during the COVID-19 pandemic compared to before.
Factors associated with reporting more consistent application of brief intervention (BI)
Respondent characteristics and reported motivation, attitude and capability for stop smoking care were compared across respondents grouped into those who reported more consistent application of brief intervention in practice in the last 12 months versus those who did not. In total, 54.7% of respondents reported more consistent application of brief intervention in practice in the last 12 months. As illustrated in Table 1, older respondents (35 years and over), more positive views on stop smoking care, knowledge about stop smoking services and treatments, feeling sufficiently trained and having confidence in the ability to provide stop smoking care were all associated with more consistent application of brief intervention in practice in the last 12 months.
Discussion
This study provides a timely assessment of Irish doctors’ knowledge, attitudes and practices regarding stop smoking care, and for the first time, it delineates Irish doctors’ views on e-cigarettes, a complex and emerging issue in tobacco policy. Overall, the study identifies a strong reservoir of support for good stop smoking care across doctors in Ireland. However, it identifies important gaps in capability and training needs, which, if addressed, could significantly strengthen doctors’ role in delivering a Tobacco Free Ireland [12]. While reported practices regarding e-cigarettes were generally in line with published national clinical guidelines [14], this was an area which doctors have identified both concerns at a policy level regarding the protection of youth as well as concerns regarding their own knowledge needs. The findings will better enable the Royal College of Physician’s Policy Group on Tobacco to provide leadership on this critical clinical care issue.
Most respondents reported strong and positive motivation regarding helping people who smoke to stop, which is encouraging. This is an important foundation upon which to develop the role of doctors in improving the provision of stop smoking care. Care begins with asking about smoking behaviour, the first step in the brief intervention [9], and, in general, doctors report that this is consistently practised. Asking about smoking and documenting the response are fundamental to the recommendations set out in new national stop smoking clinical guidelines and the HSE Making Every Contact Count framework [14, 27]. The scale of the potential impact from this simple clinical intervention cannot be underestimated. Brief advice from a doctor can increase the chance of someone who smokes making an attempt to stop by almost 70% (versus no brief advice, relative risk (RR) 1.66, 95% confidence interval (CI) 1.42 to 1.94) [9]. Linking our findings with the Medical Council of Ireland data on the number of doctors practicing in Ireland, (n = 16,461 in 2021) [28], each day there are over 100,000 interactions between doctors and people who smoke in Ireland. This reflects one in seven of the estimated 717,600 people who currently smoke in Ireland [1].
However, there are some key findings from this study that underline how this potential may not be delivering maximum impact for people who smoke that interact with doctors on a day-to-day basis. Arranging stop smoking care, including behavioural support and pharmacotherapy is, along with asking about smoking and offering advice, integral to effective brief intervention. In this study, few doctors report often or always completing these steps, which is a significant care gap. In contrast, there is good awareness of the HSE “Quit.ie” resource among doctors. There remains room to improve knowledge of local services. The study points to a number of reasons that may explain this care gap. While the motivation to provide good stop smoking care was strong, many doctors underestimated the continuing scale of harm caused by smoking in Ireland and may not fully appreciate its ongoing importance as a public health priority. Doctors’ views on their capability and confidence in providing stop smoking care and interventions were poor, and while there was high support for training at undergraduate and postgraduate levels, few had recently participated in training in this area. The importance of these findings is underscored because of the association with reporting more consistent application of brief intervention to help people who smoke stop. There is robust systematic review-level evidence that training health professionals to provide stop smoking care has a measurable effect on the point prevalence of smoking, continuous smoking abstinence and professional performance of recommended practices [29]. With the publication now of Ireland’s first national clinical guidelines focused on stop smoking care, there is an urgent need to build doctors’ confidence and capability to follow on good practice in asking about smoking with more consistent practice in arranging behavioural support and pharmacotherapy [14]. The HSE Tobacco Free Ireland Programme should work with postgraduate training bodies to raise awareness of current training offerings and resources.
This study explored doctor-reported enablers and barriers to providing good stop smoking care. As illustrated, these aligned well with established evidence-based theory on how capability, opportunity and motivation support behaviour (COM-B framework) [26]. The findings are also consistent with a recent systematic review of clinician-reported barriers to the provision of stop smoking care which found that a lack of knowledge (56% of studies), a lack of time (78%) and a lack of perceived patient motivation to stop smoking (44%) were the commonly identified issues [30].
The HSE Tobacco Free Ireland Programme has recently enabled integration with general practice management systems to stop smoking services across the country for e-referral [31], which should make it quicker and easier for doctors to make referrals. In addition, the roll-out of the new Chronic Disease Management Programme across primary care in Ireland strengthens the opportunities for doctors to address smoking in primary care, and the first report on the programme found that almost half of the enrolled patients who smoke were offered to stop smoking care [32]. Training has the potential to address all of these barriers, since it can help doctors deliver stop smoking care in a time-efficient manner, build an understanding of that this effective and cost-effective use of time and work to build patients’ intrinsic motivation. There is also a need to better communicate to doctors that most patients report high levels of motivation to quit smoking [4]; in fact, recent European studies point out that patient motivation to stop smoking in Ireland was the highest among those surveyed [33], and that arranging effective care can significantly increase the likelihood of success.
While most components of effective stop smoking care are now clearly settled with robust and comprehensive evidence enabling recommendations for clinical practice to be made with confidence [14], e-cigarettes are a complex and disruptive innovation [19], and different countries are adopting different positions in terms of regulation and recommendation on clinical practice [34]. In the UK, for example, where e-cigarettes are recommended for use in clinical practice, a recent survey of doctors found that 71% of respondents would recommend their use for patients with cancer who smoke [35]; however, in the UK, qualitative studies have found that clinicians express concern regarding the safety of e-cigarettes [36]. Reported practices among doctors in the USA regarding e-cigarettes are more conservative [37, 38], in line with advice from the US surgeon general [11]. This is the first assessment of doctor knowledge, attitude and reported practice regarding e-cigarettes in Ireland. Findings underscore a conservative view regarding this new technology among Irish doctors for people who smoke and particular concern regarding risks to youth. While this survey was conducted before the publication of national clinical guidelines, the views are consistent with the Health Research Board evidence review regarding the efficacy of e-cigarettes as a support in stopping smoking and the risk of youth initiation of smoking [39, 40]. Recent national clinical guidelines do not recommend that healthcare professionals in Ireland advise people who smoke to use e-cigarettes as a stop smoking support [14]. For the first time, however, they provide a clear national framework for healthcare professionals facing the increasingly common challenge of e-cigarettes being raised by people who smoke in interactions about stopping. It is important now that this framework is communicated to doctors.
Finally, findings indicate that doctors experienced disruption to stop smoking care during the COVID-19 pandemic. Against a context where smoking prevalence has increased in Ireland over the course of the pandemic and where people report the impact of COVID-19 on a range of health behaviours including smoking [4], there is an urgency now to ensure that doctors are aware that services are resumed and that they can play a key role in increasing demand for the stop smoking services through making referrals.
A key limitation of the study was the response rate. This is disappointing, and it is notable that the study was conducted in a period when many doctors were impacted by COVID-19-related pressures. However, the alignment of key findings with theory and evidence on doctors’ practice of stop smoking care and prior national studies provide some reassurance that the findings offer a reasonably valid national assessment. Practices were self-reported, and, with the publication of national clinical guidelines in the area, there is an opportunity to augment the findings with measurement of actual practice through clinical audit.
In conclusion, with the publication of the first national clinical guidelines focused on stop smoking care, this study provides a timely assessment of current knowledge, attitudes and practices. There is a huge opportunity for population health improvement “hiding in plain sight” to mobilise the strong reservoir of support across doctors in Ireland to improve care for people who smoke. Training, resources, and communication of new recommendations are key actions endorsed by the Policy Group on Tobacco at the Royal College of Physicians, which will take forward these findings to better support doctors and policy makers build a Tobacco Free Ireland.
References
HSE Tobacco Free Ireland Programme (2022) State of tobacco control in Ireland, second report. https://www.hse.ie/eng/about/who/tobaccocontrol/news/state-of-tobacco-control-report-2022.pdf. Accessed 3 Dec 2022
Sheridan A, Quintyne KI, Kavanagh P (2020) Counting the toll of smoking-attributable hospitalisations. Ir Med J 113(1):8
Department of Health, Ireland (2020) An assessment of the economic cost of smoking in Ireland. https://www.gov.ie/en/publication/a7ee00-an-assessment-of-the-economic-cost-of-smoking-in-ireland/. Accessed 3 Dec 2022
Department of Health, Ireland (2021) Healthy Ireland Survey 2021. https://www.gov.ie/en/collection/231c02-healthy-ireland-survey-wave/. Accessed 3 Dec 2022
World Health Organization (2008) MPOWER: a policy package to reverse the tobacco epidemic. Geneva: World Health Organization. https://apps.who.int/iris/handle/10665/43888. Accessed 3 Dec 2022
WHO Framework Convention on Tobacco Control & World Health Organization (2003) WHO Framework Convention on Tobacco Control. Geneva: World Health Organization. https://apps.who.int/iris/handle/10665/42811. Accessed 3 Dec 2022
Stead LF, Koilpillai P, Fanshawe TR et al (2016) Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Database Syst Rev 3:CD008286. Published 2016 Mar 24. https://doi.org/10.1002/14651858.CD008286.pub3
Department of Health, Ireland (2018) Healthy Ireland Survey 2018. https://www.gov.ie/en/collection/231c02-healthy-ireland-survey-wave/. Accessed 3 Dec 2022
Stead LF, Buitrago D, Preciado N et al (2013) Physician advice for smoking cessation. Cochrane Database Syst Rev 2013(5):CD000165. Published 2013 May 31. https://doi.org/10.1002/14651858.CD000165.pub4
Tobacco Advisory Group of the Royal College of Physicians in Ireland (2018) Hiding in plain sight: Treating tobacco dependency in the NHS. https://www.rcplondon.ac.uk/projects/outputs/hiding-plain-sight-treating-tobacco-dependency-nhs. Accessed 3 Dec 2022
United States Public Health Service Office of the Surgeon General; National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health (2020) Smoking cessation: a report of the surgeon general. Washington (DC): US Department of Health and Human Services
Department of Health, Ireland (2019) Tobacco free Ireland, a report by the tobacco policy review. https://www.gov.ie/en/policy-information/5df1e7-tobacco-free-ireland/. Accessed 3 Dec 2022
HSE Tobacco Free Ireland Programme (2022) HSE tobacco free Ireland programme implementation plan, 2022–2025. https://www.hse.ie/eng/about/who/tobaccocontrol/news/tobacco-free-ireland-programme-plan-2022-2025.pdf. Accessed 3 Dec 2022
Department of Health, Ireland (2019) Stop smoking (NCEC National Clinical Guideline No. 28). https://www.gov.ie/en/collection/c9fa9a-national-clinical-guidelines/. Accessed 3 Dec 2022
Reynolds CME, Egan B, Cawley S et al (2017) A national audit of smoking cessation services in Irish maternity units. Ir Med J 110(6):580. Published 2017 Jun 9
Burns A, Lucey JV, Strawbridge J et al (2018) Prospective study of provided smoking cessation care in an inpatient psychiatric setting. J Psychosom Res 115:24–31. https://doi.org/10.1016/j.jpsychores.2018.10.006
Bartels C, Abuhaliga AR, McGee H et al (2012) A survey of the prevalence of smoking and smoking cessation advice received by inpatients in a large teaching hospital in Ireland. Ir J Med Sci 181(3):445–449. https://doi.org/10.1007/s11845-011-0792-3
OhAiseadha C, Killeen M, Howell F et al (2014) An audit of smoking prevalence and awareness of HSE smoking cessation services among HSE staff. Ir Med J 107(4):115–116
Stimson GV, Thom B, Costall P (2014) Disruptive innovations: the rise of the electronic cigarette. Int J Drug Policy 25(4):653–655. https://doi.org/10.1016/j.drugpo.2014.05.003
Marron L, Burke S, Kavanagh P (2022) Changes in the utilisation of acute hospital care in Ireland during the first wave of the COVID-19 pandemic in 2020. HRB Open Res 4:67. Published 2022 Oct 12. https://doi.org/10.12688/hrbopenres.13307.3
Vardavas CI, Nikitara K (2020) COVID-19 and smoking: A systematic review of the evidence. Tob Induc Dis 18:20. Published 2020 Mar 20. https://doi.org/10.18332/tid/119324
Patanavanich R, Glantz SA (2021) Smoking is associated with worse outcomes of COVID-19 particularly among younger adults: a systematic review and meta-analysis. BMC Public Health 21(1):1554. Published 2021 Aug 16. https://doi.org/10.1186/s12889-021-11579-x
Royal College of Physicians in Ireland (2020) Policy group on tobacco. https://www.rcpi.ie/policy-and-advocacy/tobacco/. Accessed 3 Dec 2022
Campbell MJ (2021) Statistics at square one, 12th edn. Wiley-Blackwell
Pope C, Ziebland S, Mays N (2000) Analysing qualitative data. BMJ 320:114. https://doi.org/10.1136/bmj.320.7227.114
Michie S, van Stralen MM, West R (2011) The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 6:42. https://doi.org/10.1186/1748-5908-6-42
Health Service Executive (2022) Making every contact count. https://www.hse.ie/eng/about/who/healthwellbeing/making-every-contact-count/. Accessed 3 Dec 2022
Medical Council of Ireland (2021) Medical workforce intelligence report for 2021. https://www.medicalcouncil.ie/news-and-publications/press-releases/press-release/items/medical-councils-workforce-intelligence-report-2021-launched.html. Accessed 3 Dec 2022
Carson KV, Verbiest MEA, Crone MR et al (2012) Training health professionals in smoking cessation. Cochrane Database Syst Rev (5):CD000214. https://doi.org/10.1002/14651858.CD000214.pub2
Sharpe T, Alsahlanee A, Ward KD et al (2018) Systematic review of clinician-reported barriers to provision of smoking cessation interventions in hospital inpatient settings. J Smok Cessat 13(4):233–243. https://doi.org/10.1017/jsc.2017.25
HSE Tobacco Free Ireland Programme (2023) QUITManager Resources. https://www.hse.ie/eng/about/who/tobaccocontrol/resources/quitmanager-resources.html. Accessed 3 Dec 2022
Health Service Executive (2020) First report of the structured chronic disease management programme in general practice. https://www.hse.ie/eng/services/news/media/pressrel/hse-publishes-first-report-into-the-implementation-of-the-structured-chronic-disease-management-programme-in-general-practice-since-it-began-in-2020.html. Accessed 3 Dec 2022
European Commission, Directorate-General for Communication, Directorate-General for Health and Food Safety (2021) Attitudes of Europeans towards tobacco and electronic cigarettes: report. European Commission. Available via https://doi.org/10.2875/490366. Accessed 3 Dec 2022
Snell LM, Nicksic N, Panteli D et al (2021) Emerging electronic cigarette policies in European member states, Canada, and the United States. Health Policy 125(4):425–435. https://doi.org/10.1016/j.healthpol.2021.02.003
Brett J, Davies EL, Matley F et al (2020) Electronic cigarettes as a smoking cessation aid for patients with cancer: beliefs and behaviours of clinicians in the UK. BMJ Open 10(11):e037637. Published 2020 Nov 19. https://doi.org/10.1136/bmjopen-2020-037637
Albury C, Barnes R, Ferrey A et al (2022) The old and familiar meets the new and unknown: patient and clinician perceptions on e-cigarettes for smoking reduction in UK general practice, a qualitative interview study. Addiction 117(5):1427–1437. https://doi.org/10.1111/add.15760
Nickels AS, Warner DO, Jenkins SM et al (2017) Beliefs, practices, and self-efficacy of US physicians regarding smoking cessation and electronic cigarettes: a national survey. Nicotine Tob Res 19(2):197–207. https://doi.org/10.1093/ntr/ntw194
Delnevo CD, Jeong M, Teotia A et al (2022) Communication between US physicians and patients regarding electronic cigarette use. JAMA Netw Open 5(4):e226692. Published 2022 Apr 1. https://doi.org/10.1001/jamanetworkopen.2022.6692
Quigley JM, Walsh C, Lee C et al (2021) Efficacy and safety of electronic cigarettes as a smoking cessation intervention: a systematic review and network meta-analysis. Tob Prev Cessat 7:69. Published 2021 Nov 22. https://doi.org/10.18332/tpc/143077
O'Brien D, Long J, Quigley J et al (2021) Association between electronic cigarette use and tobacco cigarette smoking initiation in adolescents: a systematic review and meta-analysis. BMC Public Health 21(1):954. Published 2021 Jun 3. https://doi.org/10.1186/s12889-021-10935-1
Acknowledgements
There was no funding or grant provided for this survey. We are grateful to the Postgraduate Training Bodies in Ireland who facilitated the survey by sharing the questionnaire with their members. We also wish to acknowledge the work of Diarmuid O’Sullivan, National University of Ireland, Galway.
Funding
Helen McAvoy and Paul Kavanagh are members of the Royal College of Physicians in Ireland Tobacco Policy Group, which Des Cox chairs. These positions are unpaid. This study was conducted by the Royal College of Physicians in Ireland Tobacco Policy Group to inform its leadership role. Otherwise, the authors have no financial or non-financial interests that are directly or indirectly related to the work submitted for publication to declare.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Aisling Busher, Des Cox and Paul Kavanagh. The first draft of the manuscript was written by Aisling Busher and Paul Kavanagh and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was an evaluation of current services to inform development and improvement and was not researched within the definition of the Health Research Regulations 2018. Research Ethics Committee approval was not sought.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Busher, A., McAvoy, H., Cox, D.W. et al. Knowledge, attitudes and practices of Irish doctors regarding stop smoking care and electronic cigarettes. Ir J Med Sci 193, 783–790 (2024). https://doi.org/10.1007/s11845-023-03507-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-023-03507-2