Abstract
Background
Aromatase inhibitors (AI) are the gold standard treatment option for hormone-sensitive postmenopausal women with breast cancer. Several studies had documented the accelerated bone loss associated with AI.
Aims
In this study, we present real-world data describing the efficacy of implementing a comprehensive bone health program to maintain bone mineral density (BMD) in postmenopausal patients with early-stage breast cancer treated with AI.
Methods
A comprehensive bone health program that includes counseling, exercise, nutritional advice, vitamin D supplements and, when needed, intravenous bisphosphonate infusion was implemented following the initiation of endocrine therapy with AI. Postmenopausal women with hormone-sensitive, early-stage breast cancer treated with endocrine therapy using AI were retrospectively identified. All patients had BMD measurements before and at least 1 year after ET initiation.
Results
A total of 210 patients were included, median (range) age 67 (43–86) years. At baseline, osteoporosis was documented in 38 (18.1%) and osteopenia in 101 (48.1%) patients. Despite the known negative effect of AI, 32 (84.2%) patients with baseline osteoporosis and 69 (68.3%) of those with osteopenia, had a stable or better BMD. On the other hand, 41 (57.7%) of those with normal baseline BMD had a drop in their follow up BMD, p < 0.001. Vertebral fractures were reported in 3 (11.1%) patients with osteoporosis compared to none in patients with normal BMD, p = 0.021.
Conclusions
Despite the known negative effect of ET on bone health of breast cancer patients, implementing a comprehensive bone health program stabilized or improved BMD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, breast cancer is the most common cancer among females and its incidence increases with age [1, 2]. Given the recent advances in early detection, improving access to care and the introduction of more effective anti-cancer medications including endocrine therapy and targeted and immunotherapy, more women are surviving their disease [3]. Women with early-stage breast cancer represent the largest group of cancer survivors. As such, interest is growing to address and deal with late complications of cancer and its therapy.
Majority of patients with breast cancer express hormone receptors; estrogen (ER) and or progesterone receptors (PR), on cancer cells [4]. Consequently, measures that inhibit the synthesis of estrogen and block or destroy its receptors are widely used strategies for therapeutic intervention. In postmenopausal women, estrogen is synthesized peripherally, especially in adipose tissue and muscles by the enzyme aromatase. In such patients, aromatase inhibitors (AI) lead to a relatively rapid decline in circulating estrogens. The third-generation AI (letrozole, anastrozole, and exemestane) had replaced tamoxifen as the preferred treatment for hormone receptor–positive disease in postmenopausal women [5,6,7].
Estrogen deficiency plays a central role in the pathogenesis of osteopenia and osteoporosis in postmenopausal women. Estrogen inhibits bone resorption, so when deficient it may result in increased bone resorption and rapid bone loss. Because of AI’s effect on lowering estrogen level, several studies had documented accelerated bone loss associated with its use [8]. In one study, 197 patients from the monotherapy arms of the ATAC (Arimidex, tamoxifen, alone or in combination) trial were recruited to a bone health substudy. Patients treated with anastrozole had a significant decline in median BMD from baseline to 5 years, in both total hip (−7.24%) and lumbar spine (−6.08%) compared to tamoxifen group (total hip, + 0.74%, lumbar spine, + 2.77%) [9].
Though some of the risk factors for osteoporosis are non-modifiable, like age, gender, genetic predisposition, and ethnic origin, several other risk factors can be modified including smoking, alcohol consumption, sedentary lifestyle, poor dietary habits, and deficient vitamin D level [10].
The use of bone-modifying agents, like bisphosphonates and denosumab, had resulted in a significant improvement in bone mineral density among women treated with AI [11, 12]. Two large randomized trials (Z-FAST and ZO-FAST) addressed the use of bisphosphonates to prevent AI-induced osteopenia and osteoporosis [13,14,15]. In the ZO-FAST trial, a total of 1065 patients treated with adjuvant letrozole were randomized to receive zoledronic acid (4 mg intravenously every 6 months for 5 years) immediately or delayed until the lumbar spine or total hip T-score decreased below 2.0, or when a non-traumatic fracture occurred. Following 12 months of therapy, lumbar spine BMD increased from baseline in the immediate treatment arm, but decreased significantly from baseline in the delayed treatment arm patients [13, 14]. The other trial (Z-FAST) reached similar conclusions, too [15]. Professional societies, like the American Society of Clinical Oncology (ASCO), had issued updated guidelines on the prevention and management of osteoporosis in survivors of adult cancers with nonmetastatic disease [16].
In this study, we present real-world data describing the efficacy of implementing a comprehensive program on bone health of postmenopausal women treated with AI.
Patients and methods
Study population
Patients were postmenopausal with pathologically confirmed, hormone-sensitive, early-stage breast cancer, defined as those with no distant metastasis (M0). All patients were treated with AI (letrozole or anastrozole) and followed at our institution. Information on lifestyle, medical history, and anti-cancer treatment were obtained. Because of the retrospective nature of the study and the lack of personal or clinical details of participants that compromise anonymity, consent was waived and the study was approved by our Institutional Review Board (IRB). The study was conducted at King Hussein Cancer Center in accordance with the local and international guidelines and regulations on human research including the 1964 Helsinki declaration and its later amendments.
Anti-cancer treatment
High-risk patients (n = 103, 49.0%), defined as those with tumor size more than 2.0 cm, node-positive disease, and those with human epidermal growth factor receptor-2 (HER2)–positive disease were treated with 4–6 cycles of anthracycline-based chemotherapy with or without taxanes. Patients with HER2-positive disease were also given 1 year of concomitant trastuzumab. Following the completion of chemotherapy, all patients were treated with endocrine therapy. Patients with low-risk disease (n = 107, 51.0%) were treated with upfront endocrine therapy alone, mostly with aromatase inhibitors, like letrozole or anastrozole.
Exposure assessment
Detailed information on chemotherapy and endocrine therapy regimens were collected. Prior to the initiation of AI, all patients had BMD at total hip (TH) and lumbar spine (LS) just before starting ET and at least a year after. Dual-energy X-ray absorptiometry (DXA) Hologic scan (Discovery-SL) was used for BMD assessment, and T-score, as per World Health Organization guidelines, was used to define bone health status. Osteoporosis was defined as T-score of −2.5 or lower, while osteopenia was defined as scores of −1.0 to −2.49. Vitamin D deficiency was defined as levels < 20.0 ng/mL and insufficiency with level of 20.0–29.9 ng/mL. Patients known to have osteoporosis and on active therapy for osteopenia or osteoporosis were excluded. Additionally, patients who refused to follow the designed bone health program were excluded, too.
Bone health program
A comprehensive bone health program was implemented. The program includes extensive counselling, calcium and vitamin D supplements, increased milk intake, and exercise. Patients with baseline lumbar spine or total hip T-scores ≤ − 2.0 were given short intravenous bisphosphonate infusion every 6 months. Patients with osteoporosis were referred to a specially designed osteoporosis clinic.
Outcome assessment
Osteopenia and osteoporosis diagnoses were confirmed at two points: baseline before the initiation of AI and at 1–2 years of follow-up. Both tests were done using the same machines and interpreted by one of the investigators.
Information on covariates such as age, body mass index (BMI), smoking history, educational level, annual income, bisphosphonate use, and vitamin D supplement use were also collected.
Statistical analysis
Descriptive statistics were performed for all variables. Continuous variables with normal distribution were presented as mean (standard deviation [SD]), and non-normal variables were described as median (interquartile range [IQR]). Categorical variables were expressed as numbers (percentages). A significance level of P ≤ 0.05 was used in the analysis of two sample t-test. Analyses were conducted using Minitab statistical software version 18 (Minitab 18 Statistical Software (2017), State College, PA.
Results
Between 2013 and 2019, a total of 210 patients fulfilled the eligibility criteria and were included in this study. All were female, median (range) age 67 (43–86) years. Low BMI, defined as < 20 kg/m2, a known risk factor for osteoporosis, was encountered in only two patients with osteoporosis and in none among patients with osteopenia. Additionally, active smoking was observed in 16 (7.6%) patients, Table 1. At baseline, and prior to start of AI, osteoporosis was documented in 38 (18.1%) patients (Group I), while 101 (48.1%) others had osteopenia (Group II) and 71 (33.8%) had normal BMD. The median T-scores prior to AI therapy at the hip and lumber spines were −1.0 (range: −3.6, 1.9) and −1.4 (range: −3.9, 2.6), respectively, while the median vitamin D level for 182 patients with known baseline levels was 24.0 (range: 6.6–75.0) ng/mL, with 46 (25.3%) patients had vitamin D deficiency and 74 (40.7%) others had vitamin D insufficiency. None of the patients was on prior active therapy or even aware of their vitamin D or BMD levels (Table 2).
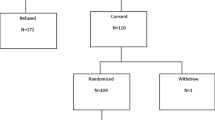
Following at least 12 months of endocrine therapy, 32 (84.2%) patients with prior osteoporosis (Group I) and 69 (68.3%) of those with prior osteopenia (Group II) had a stable or higher BMD. On the other hand, 41 (57.7%) of those with normal baseline BMD (Group III) had a drop in their follow-up BMD (Fig. 1). Thus, following the 12 months of ET, the number of patients with osteoporosis dropped to 27 (12.9%) and those with osteopenia dropped to 96 (45.7%) while those with normal BMD increased to 87 (41.4%) (Fig. 2).
Vertebral fractures, presented with back pain and documented by imaging studies, were reported in 3 (11.1%) patients with osteoporosis compared to none in patients with normal BMD, P = 0.021. Rib fracture and hip fracture were reported in one patient each, and both had normal BMD before and after AI therapy.
Discussion
Osteoporosis and osteopenia are commonly encountered among postmenopausal women [17, 18]. Osteoporotic vertebral and hip fractures are serious, usually require hospitalization and surgery with 1-year mortality rate that can reach 25% [19, 20]. Limited mobility with its potential venous thromboembolism, chronic pain, disfigurement, and deterioration in pulmonary function may complicate vertebral fractures [21]; all may lead to anxiety, depression, and poor quality of life.
Endocrine therapy is increasingly used as a solo therapy for low-risk early-stage breast cancer, and as an additional adjuvant therapy following chemotherapy in high-risk patients. As such, aromatase inhibitors are a standard ET in all postmenopausal patients [5, 6]. Bone pain, arthralgia, and myalgia are commonly encountered with AI and may result in treatment discontinuation in up to 20% of the patients [22, 23]. However, the well-known negative effect on bone health, on already compromised postmenopausal patients, is silent and can go unnoticed until complications happen. Giving its potential serious outcomes, issues related to bone health in breast cancer patients treated with AI are incorporated in major international clinical practice guidelines [24]. Assessment of BMD prior to, and following the treatment with AI, is routinely practiced and can be a key performance indicator (KPI).
Our results clearly show that the existence of osteopenia, or even osteoporosis, should not be a reason to deny women with breast cancer the access to such important drugs. Intense education on modifiable risk factors, along with the use of bone-modifying agents as an active treatment of osteoporosis or prevent progression of osteopenia, worked very well in our patients. The fact that patients with normal BMD at baseline had significant deterioration following AI therapy highlights the importance of such interventions that are not strictly followed by the patients, and not stressed enough by physicians, either.
Our data highlights the fact that almost two-thirds of postmenopausal women are vitamin D deficient or insufficient. Our findings echo results from a recently published meta-analysis in which 67% of patients with breast cancer had a baseline level of 25-hydroxy vitamin D below 30 ng/mL [25].
Given the need for AI in majority of postmenopausal breast cancer patients, and based on our findings, we do recommend that vitamin D level be checked at initial presentation of all women with breast cancer and vitamin D supplements start a lot earlier, during the initial work up and long before the initiation of drugs or interventions that are known to worsen BMD, like AI.
Our study is not without limitations; the inclusion of comparative control group in future studies should empower conclusions. Future studies may consider including premenopausal women treated with tamoxifen or AI plus gonadotropin-releasing hormone agonists (GnRHa); both are known to have negative impact on bone health in this age group.
In conclusion, postmenopausal women with breast cancer are at risk of osteopenia and osteoporosis. Such risk increases significantly with the use of AI. However, early interventions with modifiable risk factors, vitamin D supplements, and use of bone-modifying agents can lower this risk.
Availability of data and material
Data used in this study can be made available upon reasonable request to the corresponding author.
Prior presentation
Data was presented, as a poster, at the annual San Antonio Breast Cancer Symposium held virtually 8–11 Dec 2020.
References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Torre LA, Siegel R, Ward E, Jemal A (2015) Global cancer incidence and mortality rates and trends–an update. Cancer Epidemiol Biomark Prev 25(1):16–27. https://doi.org/10.1158/1055-9965.EPI-15-0578
Berry DA, Cronin KA, Plevritis SK et al (2005) Cancer intervention and surveillance modeling network (CISNET) collaborators. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med 353(17):1784–1792. https://doi.org/10.1056/NEJMoa050518
Howlader N, Altekruse S, Li C et al (2014) US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. JNCI: J Natl Cancer Inst 106(5):dju055. https://doi.org/10.1093/jnci/dju055
Baum M, Buzdar A, Cuzick J et al (2003) Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early-stage breast cancer: Results of the ATAC (Arimidex, Tamoxifen Alone or in Combination) trial efficacy and safety update analyses. Cancer 98:1802–1810. https://doi.org/10.1002/cncr.11745
Breast International Group (BIG) 1–98 Collaborative Group, Thürlimann B, Keshaviah A et al (2005) A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. New Engl J Med 353:2747–2757. https://doi.org/10.1056/NEJMoa052258
Perez E, Josse R, Pritchard K et al (2006) Effect of letrozole versus placebo on bone mineral density in women with primary breast cancer completing 5 or more years of adjuvant tamoxifen: A companion study to NCIC CTG MA.17. J Clin Oncol 24(22):3629–3635. https://doi.org/10.1200/JCO.2005.05.4882
Abdel-Razeq H, Awidi A (2011) Bone health in breast cancer survivors. J Cancer Res Ther 7(3):256–263. https://doi.org/10.4103/0973-1482.87006
Eastell R, Adams J, Coleman R et al (2008) Effect of anastrozole on bone mineral density: 5-year results from the anastrozole, tamoxifen, alone or in combination trial 18233230. J Clin Oncol 26(7):1051–1057. https://doi.org/10.1200/JCO.2007.11.0726
Cosman F, de Beur S, LeBoff M et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381. https://doi.org/10.1007/s00198-014-2794-2
Bouvard B, Chatelais J, Soulié P et al (2018) Osteoporosis treatment and 10 years’ oestrogen receptor+ breast cancer outcome in postmenopausal women treated with aromatase inhibitors. Eur J Cancer 101:87–94. https://doi.org/10.1016/j.ejca.2018.06.028
Langdahl B (2020) Treatment of postmenopausal osteoporosis with bone-forming and antiresorptive treatments: Combined and sequential approaches. Bone 139:115516. https://doi.org/10.1016/j.bone.2020.115516
Bundred N, Campbell I, Davidson N et al (2008) Effective inhibition of aromatase inhibitor-associated bone loss by zoledronic acid in postmenopausal women with early breast cancer receiving adjuvant letrozole. Cancer 112(5):1001–1010. https://doi.org/10.1002/cncr.23259
Coleman R, de Boer R, Eidtmann H et al (2013) Zoledronic acid (zoledronate) for postmenopausal women with early breast cancer receiving adjuvant letrozole (ZO-FAST study): final 60-month results. Ann Oncol 24(2):398–405. https://doi.org/10.1093/annonc/mds277
Brufsky A, Bosserman L, Caradonna R et al (2009) Zoledronic acid effectively prevents aromatase inhibitor–associated bone loss in postmenopausal women with early breast cancer receiving adjuvant letrozole: Z-fast study 36-month follow-up results. Clin Breast Cancer 9(2):77–85. https://doi.org/10.3816/CBC.2009.n.015
Shapiro CL, Van Poznak C, Lacchetti C et al (2019) Management of osteoporosis in survivors of adult cancers with nonmetastatic disease: ASCO clinical practice guideline. J Clin Oncol 37(31):2916–2946. https://doi.org/10.1200/JCO.19.01696
Ahlborg HG, Johnell O, Turner CH et al (2003) Bone loss and bone size after menopause. N Engl J Med 349(4):327–334. https://doi.org/10.1056/NEJMoa022464
Schuit SC, van der Klift M, Weel AE et al (2004) Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study. Bone 34(1):195–202. https://doi.org/10.1016/j.bone.2003.10.001
Ioannidis G, Papaioannou A, Hopman WM et al (2009) Relation between fractures and mortality: results from the Canadian Multicentre Osteoporosis Study. CMAJ 181(5):265–271. https://doi.org/10.1503/cmaj.081720
Magaziner J, Simonsick E, Kashner T et al (1990) Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol 45(3):M101–M107. https://doi.org/10.1093/geronj/45.3.m101
US Department of Health and Human Services (2002) Bone Health and osteoporosis: a report of the surgeon general. Rockville, MD: US Department of Health and Human Services, Office of the Surgeon General 1Y55. Available at: https://www.bones.nih.gov/health-info/bone/SGR/surgeon-generals-report. Accessed on 01 Apr 2021
Tenti S, Correale P, Cheleschi S et al (2020) Aromatase inhibitors-induced musculoskeletal disorders: current knowledge on clinical and molecular aspects. Int J Mol Sci 21(16):5625. https://doi.org/10.3390/ijms21165625
Pineda-Moncusí M, Servitja S, Tusquets I et al (2019) Assessment of early therapy discontinuation and health-related quality of life in breast cancer patients treated with aromatase inhibitors: B-ABLE cohort study. Breast Cancer Res Treat 177(1):53–60. https://doi.org/10.1007/s10549-019-05289-7
NCCN clinical practice guidelines in oncology: Breast Cancer, version 3.2021. Available at: https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 02 Apr 2021
Voutsadakis IA (2021) Vitamin D baseline levels at diagnosis of breast cancer: a systematic review and meta-analysis. Hematol Oncol Stem Cell Ther 14(1):16–26. https://doi.org/10.1016/j.hemonc.2020.08.005
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by King Hussein Cancer Center IRB.
Consent to participate
Consent was waived by King Hussein Cancer Center IRB.
Consent for publication
Not applicable.
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abdel-Razeq, H., Al-Rasheed, U., Mashhadani, N. et al. The efficacy of a comprehensive bone health program in maintaining bone mineral density in postmenopausal women with early-stage breast cancer treated with endocrine therapy: real-world data. Ir J Med Sci 191, 2511–2515 (2022). https://doi.org/10.1007/s11845-021-02897-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-021-02897-5