Abstract
Introduction
Hip fracture prevention is an essential component in elderly patient care. History of prior fracture is a significant risk factor for subsequent hip fracture. There are variable rates of treatment for these groups of patients. The aims of this study were to make an assessment of how many hip fracture patients over a 1 year period had a previous fracture and to assess whether or not these patients were on anti-osteoporotic medication.
Methods
Assessment on whether or not patients had a prior fracture using the national radiology imaging system checking radiology reports for all previous imaging performed. Checking patients bone health status using the hip fracture database for our hospital.
Results
There were 225 hip fractures in 221 patients over a 1-year period. About 42.6% of females and 35.9% of males had a history of previous fracture. Vertebral fractures were the most common type of fracture. We found 7% of patients had a contralateral hip fracture. There were 81% of patients with prior fracture, and 71% of those without prior fracture were on anti-osteoporotic medication.
Discussion
Vertebral fractures were the most common preceding fracture in hip fracture patients. There were many patients with a history of fragility fractures that were not on preventative medication. Overall there were good prescription rates of anti-osteoporotic medication. There were significantly higher rates of prescription amongst females compared with males.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures are a major cause of morbidity and mortality in the elderly. As well the implications of this injury in the patients that sustain a hip fracture, there are also major economic implications for a healthcare system [1]. Most hip fractures are fragility fractures due to underlying osteoporosis. With an increase in life expectancy and an increase of population over the age 70, it is expected for the volume of hip fractures and patients with osteoporosis to increase [2, 3]. Osteoporosis is manifested by fractures at multiple skeletal sites particularly the spine, hip, and wrist. Worldwide, osteoporosis causes > 8.9 million fractures annually, with the greatest number of osteoporotic fractures occurring in Europe (34.8%) [4].
Sustaining a fracture is a well-known risk factor for sustaining future fractures [5,6,7,8,9,10]. It has been reported that vertebral fracture increases the risk of subsequent hip fracture by at least twofold [7, 8]. It was found that history of forearm fracture increases the risk of future hip fracture by around 50% [9, 10]. Because of this high risk, it is important that patients that sustain an osteoporotic fracture are correctly treated to prevent further injury. The use of bone protective medications has been found to almost halve the risk of subsequently developing another fracture [11,12,13]. However, the rate of prescription of osteoporotic protective medications has been in decline in Europe in recent times [14, 15].
The purpose of this study was to assess history of previous fracture in hip fracture patients, what were the most common fracture sites and how much patients were on fracture preventative medication. We also aimed to see how many patients had a previous fracture but were not on preventative medication.
Methods
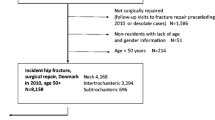
This was a single-centre study, where the aims of the study were to assess the history of previous fracture in hip fracture patients that presented to the hospital over a 1-year period and the rate of fracture preventative medication prescription in these patients. We also used this to audit our own departmental assessment of bone health in hip fracture patients. This was a retrospective study using the orthopaedic department Hip Fracture datasheet over a 12-month period from July 2018 to July 2019.
Assessment of fractures was performed using National Integrated Medical Imaging System (NIMIS), the national radiology imaging software. Patients were searched on this system using name and date of birth. All radiology reports of all imaging on the system for each patient were reviewed, and previous fractures and dates of fracture were recorded. Non hip fractures that occurred at the time of the hip fracture were recorded, and fractures that occurred since their hip fracture were also recorded. Prevalence of dual-energy X-ray absorptiometry (DEXA) scans being performed was also assessed using the national radiology software.
The Hip Fracture datasheet recorded the patient demographics, prescription of fracture prevention medication, admission date, surgery date, discharge date, and type of surgery performed.
Data collection was performed with Microsoft Excel. Statistical analysis was performed using SPSS version 23. Data was analysed by using computing variables, descriptive statistics, independent sample t-tests, and frequency analysis.
Results
There were 225 hip fractures in 221 patients over the 1-year period, with 4 patients sustaining bilateral hip fractures within the study period. The mean age was 77 with a range of 34 to 98. A total of 217 patients (98.1%) were over the age of 50. There was one patient under 40. There were 143 female and 78 male patients. The mean length of stay was 10.1 days (range 1–97). There were 37 patients that had previous DEXA scans performed.
There were 88 patients (39.8%) that had a previous fracture before fracturing their hip. There were 173 fractures in 88 patients, with 32 different types of fractures. Forty-nine patients (22.2%) had 2 or more fractures. There were 110 (63.3%) previous fragility fractures. There was a higher proportion of females that had history of a previous fracture with 42.6%, compared with 35.9% of men (p = 0.33). The mean time from first fracture to hip fracture was 4 years (range 18–24 years). If the image was of an old fracture that was not at the time of injury, the timing of the fracture excluded from analysis. See Table 1 to see full breakdown of fractures. See Table 2 for the breakdown of fragility fractures.
There were 130 patients (58.8%) that underwent bone health assessment. Ninety-eight patients (75.3%) were on anti-osteoporotic medication. Only 52% of males were on anti-osteoporotic medication compared with 84% of females (p = 0.002). Thirty-two patients (24.7%) were not on preventative medication. Anti-osteoporotic medication was commenced on 30 patients, and 2 were referred for DEXA scan. Of the 32 patients that were not on preventative medication, 12 patients (37.5%) had a previous fracture and 8 patients (25%) had 2 or more fractures. Sixty-one of the 88 patients (69.3%) of patients that underwent bone health assessment had a previous fracture. Eleven of these 61 patients (18%) were not on preventative medication. Thirty-five of 49 patients (71.4%) that had 2 or more fractures underwent bone health assessment. Seven of these 35 patients (20%) were not on preventative medication.
Vertebral fractures were the most common type of fracture with 54 vertebral fractures in 35 patients. The breakdown of these vertebral fractures was one cervical fracture, 27 thoracic fractures, and 26 lumbar fractures. Twelve patients with vertebral fractures were single-level fracture and 23 had fractures of multiple levels. Nine of the 35 patients’ vertebral fractures were found incidentally on a CT scan with a different area of concern for the indication for the scan. Thirteen patients with a previous fracture had only vertebral fractures previously. Ten of these patients underwent bone health assessment with 8 patients (80%) being on preventative medication.
Sixteen patients (7.2%) had a previous contralateral hip fracture. Two patients had previous ipsilateral hip fracture. One of these patients had their dynamic hip screw changed to a total hip replacement; the other patient had their short cephalomedullary nail changed to a hemiarthroplasty.
Fifteen patients (6.67%) had another fracture at the time of their hip fracture. Vertebral, olecranon, and distal radius fractures were the most common with three of each (see Table 3).
There were 13 fractures in 12 patients since their hip fracture. Most commonly there were 5 contralateral hip fractures and 4 vertebral fractures (two lumbar, two thoracic). The mean time to fracture was 112 days (range 7–398) (see Table 4).
Cemented bipolar hemiarthroplasty was the most common operation with 109 patients (48.4%) undergoing this procedure, followed by short cephalomedullary nail with 40 patients (17.8%), long cephalomedullary nail with 29 patients (12.8%), and dynamic hip screw with 20 patients (8.8%). Nine patients (4%) were treated nonoperatively. See Table 5 for full breakdown of interventions performed. Ten of 216 patients (4.6%) had their surgery outside the 48 h of admission target of our hospital policy.
Discussion
A history of a fracture is an important predictor of risk in subsequently suffering a hip fracture. Despite this, there are many patients that have sustained a fracture and are not properly assessed for osteoporosis and commenced on preventative medication. This was a single-centre study that looked at the history of previous fracture and the prescription of preventative medication in a hip fracture population over a 1-year period.
We found 39.8% of hip fracture patients in our centre had a previous fracture, with females having a higher incidence of previous fracture with 42.6%, compared with 35.9% of men having a previous fracture. Port et al. [16] performed a similar study in Sydney, Australia, in 2002 which obtained similar results where they found 45% of women with hip fracture had a previous fracture compared with 30% of men having a previous fracture. There were a significant proportion of the fractures (63.6%) in our study that occurred that would be described fragility fractures.
In our study, vertebral fractures were found significantly be the most common fracture, where 54 of a total of 173 (31.2%) fractures were vertebral fractures. There was almost an equal distribution between thoracic and lumbar fracture, being 27 and 26 respectively, and one cervical fracture within this group of patients. The true incidence of vertebral fractures is likely higher than this also, where the true prevalence is several times greater than the number known to patients or that may have been imaged [17]. Vertebral fractures often present as worsening back pain that can often occur without a history of trauma, and therefore may not get imaged. Gehlbach et al. [18] performed a study where they had radiologists review chest X-rays performed in women over 60, where only 50% of vertebral fractures were reported and only 17% a fracture documented in the medical record or discharge summary. Kelly et al. [19] performed a study assessing vertebral fractures in CT pulmonary angiogram in hip fracture patients and the corresponding radiology reports and found that only one in 5 vertebral fractures were reported. Lauritzen and Lund [8] performed a study to assess the risk of subsequent hip fracture in women who had sustained lumbar spine, olecranon, knee, and ankle fractures and found that lumbar spine fracture had the highest relative risk of these injuries with a value of 4.8. Imai et al. [20] performed a study where they obtained lumbar X-rays in all hip fracture patients and compared the 1-year mortality between those that had vertebral fractures and those who did not. They found that 80% of patients had a vertebral fracture and that there was a significant difference in mortality between the groups with a 27% 1-year mortality in those with fractures and 5% mortality in those without.
Fifteen (6.67%) of hip fractures had another fracture at the time of injury with vertebral, olecranon, and distal radius fractures being the most common with three of each occurring in these patients. There was one lumbar and two thoracic fractures that occurred. It has been found that concomitant distal radius and hip fractures result in an increased length of stay, but no effect on mortality [21, 22]. It has been found that patients that sustain simultaneous wrist fractures and hip fractures tend to be fitter and more independent pre-injury [22, 23]. It is hypothesised that these patients sustain wrist fractures because they possess better, intact protective reflexes than the average hip fracture patient [22, 24].
In this study, there were 16 patients (7.2%) that had a previous hip fracture on the contralateral side with 4 of these patients having bilateral hip fractures within the study period. There was one patient that subsequently went on to fracture the contralateral side after the study period. There were 2 patients with previous hip fractures on the ipsilateral side. One patient with previous hip fracture on the same side was converted from a dynamic hip screw to a total hip replacement, and the other was converted from a short cephalomedullary nail to a cemented bipolar hemiarthroplasty. The rate of contralateral hip fracture after previous fracture is quoted to be between 6 and 16% [25,26,27]. Patients with prior hip fracture are at a twofold of further hip fracture [27]. Hughes et al. [28] performed a study comparing rates of contralateral hip fracture in intertrochanteric and pertrochanteric where they found that the dynamic hip screw group had a contralateral fracture rate of 10.7% and short cephalomedullary nail group had a contralateral fracture rate of 7.9% which was not a statistically significant difference. Souder et al. [29] performed a study comparing rates of contralateral fracture in patients that underwent arthroplasty and closed reduction with percutaneous pinning (CRPP) for neck of femur fractures and found that the arthroplasty group had a contralateral fracture rate of 5.57% compared with 10.1% of the CRPP group.
For patients that underwent anti-osteoporotic medication assessment, 75% were already on some form of preventative treatment. Of the patients assessed, 81% of patients that had a history of previous fracture were already on treatment and 71% of patients without a previous fracture were on treatment (p = 0.168). Women had significantly higher rates of prescription of anti-osteoporotic medication with 84% being on preventative medication compared with only 52% of men (p = 0.002). These are very high rates of treatment compared with other similar studies. Maggi et al. [30] found that 25% of their patient were already on preventative treatment prior to fracturing their hip. They also found a difference in prescription rates between those that had previous fractures and those that did not, which were 37.1% and 18.5% respectively. Port et al. [16] found that 26% of women with a previous fracture were on preventative medication and only 10% of women without a previous fracture were on prevention. They also found that there was a significant difference in prescription between genders with only 2% of men on preventative medication in their study.
There were a number of limitations of this study. Some of which include that is was performed as a retrospective study. Fractures that may have occurred in hospitals that do not use the national imaging software would have been missed and fractures that may have occurred prior to the implementation of the national imaging software. Data collected on anti-osteoporotic medication was only collected in 59% of patients and did not go into the detail of which type of medication the patients were on previously or what they were commenced on. This is also a cross-sectional study so we cannot assess a cause-effect association for the risk of hip fracture in patients with previous fracture.
Conclusion
Our study shows high rates of osteoporosis preventative medication prescription in a hip fracture population with higher rates of prescription in patients with a history of previous fracture and females. About 39.8% of patients had a previous fracture, with a higher rate among females in this hip fracture group. Vertebral fractures were the most common type fracture in this group.
References
Haentjens et al (2005) Costs and consequences of hip fracture occurrence in old age: an economic perspective. Disabil Rehabil 27(18–19):1129–1141. https://doi.org/10.1080/09638280500055529
Dodds MK, Codd MB, Looney A, Mulhall KJ (2009) Incidence of hip fracture in the Republic of Ireland and future projections: a population-based study. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 20(12):2105–2110. https://doi.org/10.1007/s00198-009-0922-1
Kelly M, McGowan B, McKenna M, Carey J, Whelan B, Silke C (2018) Emerging trends in hospitalisation for fragility fractures in Ireland. Ir J Med (1971) 187. https://doi.org/10.1007/s11845-018-1743-z
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 17(12):1726–1733. https://doi.org/10.1007/s00198-006-0172-4
Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, Eisman J, Fujiwara S, Garnero P, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35(2):375–382. https://doi.org/10.1016/j.bone.2004.03.024
Van Staa et al (2002) Does a fracture at one site predict later fractures at other sites? A British cohort study Osteoporosis International 13(8):624–629. https://doi.org/10.1007/s001980200084
Kotowicz MA, Melton LJ 3rd, Cooper C, Atkinson EJ, O’Fallon WM, Riggs BL (1994) Risk of hip fracture in women with vertebral fracture. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research 9(5):599–605. https://doi.org/10.1002/jbmr.5650090503
Lauritzen JB, Lund B (1993) Risk of hip fracture after osteoporosis fractures. 451 women with fracture of lumbar spine, olecranon, knee or ankle. Acta Orthop Scand 64(3):297–300. https://doi.org/10.3109/17453679308993629
Mallmin H, Ljunghall S, Persson I, Naessen T, Krusemo UB, Bergstrom R (1993) Fracture of the distal forearm as a forecaster of subsequent hip fracture: a population-based cohort study with 24 years of follow-up. Calcif Tissue Int 52(4):269–272. https://doi.org/10.1007/bf00296650
Cuddihy MT, Gabriel SE, Crowson CS, O’Fallon WM, Melton LJ 3rd (1999) Forearm fractures as predictors of subsequent osteoporotic fractures. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 9(6):469–475. https://doi.org/10.1007/s001980050172
Liberman UA, Weiss SR, Bröll J, Minne HW, Quan H, Bell NH, Rodriguez-Portales J, Downs RW, Jr., Dequeker J, Favus M (1995) Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. The Alendronate Phase III Osteoporosis Treatment Study Group. The New England J Med 333(22):1437–1443. https://doi.org/10.1056/nejm199511303332201
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, Delmas P, Zoog HB, Austin M, Wang A, Kutilek S, Adami S, Zanchetta J, Libanati C, Siddhanti S, Christiansen C (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361(8):756–765. https://doi.org/10.1056/NEJMoa0809493
Chapuy MC, Arlot ME, Duboeuf F, Brun J, Crouzet B, Arnaud S, Delmas PD, Meunier PJ (1992) Vitamin D3 and calcium to prevent hip fractures in elderly women. N Engl J Med 327(23):1637–1642. https://doi.org/10.1056/nejm199212033272305
van der Velde RY, Wyers CE, Teesselink E, Geusens PPMM, van den Bergh JPW, de Vries F, Cooper C, Harvey NC, van Staa TP (2017) Trends in oral anti-osteoporosis drug prescription in the United Kingdom between 1990 and 2012: variation by age, sex, geographic location and ethnicity. Bone 94:50–55. https://doi.org/10.1016/j.bone.2016.10.013
Kanis JA, Cooper C, Rizzoli R, Abrahamsen B, Al-Daghri NM, Brandi ML, Cannata-Andia J, Cortet B, Dimai HP, Ferrari S, Hadji P, Harvey NC, Kraenzlin M, Kurth A, McCloskey E, Minisola S, Thomas T, Reginster JY, for the European Society for C, Economic Aspects of Osteoporosis O, Musculoskeletal D (2017) Identification and management of patients at increased risk of osteoporotic fracture: outcomes of an ESCEO expert consensus meeting. Osteoporos Int 28(7):2023–2034. https://doi.org/10.1007/s00198-017-4009-0
Port L, Center J, Briffa NK, Nguyen T, Cumming R, Eisman J (2003) Osteoporotic fracture: missed opportunity for intervention. Osteoporos Int 14(9):780–784. https://doi.org/10.1007/s00198-003-1452-x
Lane NE (2006) Epidemiology, etiology, and diagnosis of osteoporosis. Am J Obstet Gynecol 194(2):S3–S11. https://doi.org/10.1016/j.ajog.2005.08.047
Gehlbach SH, Bigelow C, Heimisdottir M, May S, Walker M, Kirkwood JR (2000) Recognition of vertebral fracture in a clinical setting. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 11(7):577–582. https://doi.org/10.1007/s001980070078
Kelly MA, McCabe E, Bergin D, Kearns SR, McCabe JP, Armstrong C, Heaney F, Carey JJ (2020) Osteoporotic vertebral fractures are common in hip fracture patients and are under recognised. J Clin Densitom. https://doi.org/10.1016/j.jocd.2020.05.007
Imai N, Endo N, Hoshino T, Suda K, Miyasaka D, Ito T (2016) Mortality after hip fracture with vertebral compression fracture is poor. J Bone Miner Metab 34(1):51–54. https://doi.org/10.1007/s00774-014-0640-4
Uzoigwe CE, Venkatesan M, Johnson N, Lee K, Magaji S, Cutler L (2015) Influence of coincident distal radius fracture in patients with hip fracture: single-centre series and meta-analysis. J Orthop Traumatol 16(2):93–97. https://doi.org/10.1007/s10195-013-0281-8
Robinson PM, Harrison T, Cook A, Parker MJ (2012) Orthopaedic injuries associated with hip fractures in those aged over 60 years: a study of patterns of injury and outcomes for 1971 patients. Injury 43(7):1131–1134. https://doi.org/10.1016/j.injury.2012.03.012
Tow BPB, Chua BSY, Fook-Chong S, Howe TS (2009) Concurrent fractures of the hip and wrist: a matched analysis of elderly patients. Injury 40(4):385–387. https://doi.org/10.1016/j.injury.2008.09.013
Shabat S, Gepstein R, Mann G, Kish B, Stern A, Fredman B, Nyska M (2002) Does the combination of a simultaneous subcapital fracture of humerus and hip fracture in elderly patients carry a prognostic value? Arch Gerontol Geriatr 35(1):71–77. https://doi.org/10.1016/S0167-4943(02)00015-8
Vochteloo AJH, Borger van der Burg BLS, Röling MA, van Leeuwen DH, van den Berg P, Niggebrugge AHP, de Vries MR, Tuinebreijer WE, Bloem RM, Nelissen RGHH, Pilot P (2012) Contralateral hip fractures and other osteoporosis-related fractures in hip fracture patients: incidence and risk factors. An observational cohort study of 1,229 patients. Arch Orthop Trauma Surg 132(8):1191–1197. https://doi.org/10.1007/s00402-012-1520-9
Sawalha S, Parker MJ (2012) Characteristics and outcome in patients sustaining a second contralateral fracture of the hip. J Bone Joint Surg Am Volume 94-B(1):102–106. https://doi.org/10.1302/0301-620X.94B1.27983
Ryg J, Rejnmark L, Overgaard S, Brixen K, Vestergaard P (2009) Hip fracture patients at risk of second hip fracture: a nationwide population-based cohort study of 169,145 cases during 1977–2001. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research 24(7):1299–1307. https://doi.org/10.1359/jbmr.090207
Hughes JD, Bartley JH, Brennan KL, Maldonado YM, Brennan ML, Chaput CD (2017) Rate of contralateral hip fracture after dynamic hip screw vs intramedullary nail for treatment of pertrochanteric hip fractures. Proc (Bayl Univ Med Cent) 30(3):268–272. https://doi.org/10.1080/08998280.2017.11929612
Souder CD, Brennan ML, Brennan KL, Song J, Williams J, Chaput C (2012) The rate of contralateral proximal femoral fracture following closed reduction and percutaneous pinning compared with arthroplasty for the treatment of femoral neck fractures. The J Bone Joint Surg Am 94(5):418–425. https://doi.org/10.2106/jbjs.j.01134
Maggi S, Siviero P, Gonnelli S, Caffarelli C, Gandolini G, Cisari C, Rossini M, Iolascon G, Mauro GL, Nuti R, Crepaldi G (2011) The burden of previous fractures in hip fracture patients. The Break Study. Aging clinical and experimental research 23(3):183–186. https://doi.org/10.1007/bf03324958
Acknowledgements
All authors have participated in (a) conception and design, or analysis and interpretation of the data; (b) drafting the article or revising it critically for important intellectual content; and (c) approval of the final version. The article I have submitted to the journal for review is original, has been written by the stated authors, and has not been published elsewhere. This manuscript has not been submitted to, nor is under review at, another journal or other publishing venue.
Author information
Authors and Affiliations
Contributions
The authors have no affiliation with any organization with a direct or indirect financial interest in the subject matter discussed in the manuscript.
Corresponding author
Ethics declarations
Ethical approval
It was not obtained as it was a retrospective audit of data already obtained for clinical purposes and was compliant with the hospital’s ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
McCarthy, C.J., Kelly, M.A. & Kenny, P.J. Assessment of previous fracture and anti-osteoporotic medication prescription in hip fracture patients. Ir J Med Sci 191, 247–252 (2022). https://doi.org/10.1007/s11845-021-02571-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-021-02571-w