Abstract
Introduction
In laboratory medicine, reference intervals (RIs) are key decision support tools used to guide the clinical interpretation of numerical test results. Best practice suggests each laboratory establishes RIs in the local population prior to introducing an assay into routine clinical practice.
Aim
The aim of this study was to define RIs for frequently requested biochemical/haematological parameters in a healthy adult Irish Caucasian population.
Methods
A cross-sectional study of non-pregnant apparently healthy volunteers was conducted. Baseline demographics, anthropometric and laboratory measurements were recorded. In total, 37 commonly requested biochemical (serum, n = 26) and haematological (venous blood, n = 11) ISO15189:2012 accredited tests were analysed, using the Roche Cobas® Sebia Capillarys 3 Tera and Siemens Advia® 2120i platforms following standard operating procedures. RIs were defined according to the International Federation of Clinical Chemistry (IFCC) recommended method.
Results
Of 208 apparently healthy volunteers, 76 failed to meet the study inclusion criteria. The reference population comprised of 132 participants (males: n = 65, 49.2%) with a median age of 29.7 (18.1–62.2) years. RIs for the majority of biochemical/haematological parameters were broadly in accord with those provided by Pathology Harmony (UK)/Irish RI Harmonisation Project and the manufacturer Roche Diagnostics. However, the established RI defined for HbA1c: 27–37 mmol/mol was markedly different from that quoted nationally, HbA1c: 20–42 mmol/mol.
Conclusion
Normative biological intervals established in a healthy adult Irish population for 37 commonly requested biochemical/haematological parameters will be a valuable aid to result interpretation in clinical laboratories after appropriate verification in accordance with ISO 15189: 2012.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Laboratory tests are requested for several reasons: screening or health checks, to decide on a specific level of risk or probability for the presence of a particular disease, confirmatory tests for a specific condition, action limits and therapeutic targets based on locally agreed protocols or values proposed by expert individuals, committees or organisations [1]. Hence, laboratory medicine data informs a significant proportion of clinical decisions in healthcare and are critical to ensuring evidence-based treatment [2, 3].
The goal of medical testing laboratories is the provision of high quality and competently performed clinical laboratory examinations and interpretative reports that aid patient care. The International Organisation for Standardisation (ISO) 15189:2012 specifies the quality management system requirements for medical laboratories. Certification to ISO 15189:2012 demonstrates that the laboratory is competent to manage all aspects of the work of the medical testing laboratory. This includes organisation and quality management, resources (e.g., state registered staff, equipment), Standard Operating Procedures, and the evaluation and quality assurance (Internal Quality Control, External Quality Assessment) activities required to ensure that the total testing processes (pre-analytical, analytical and post-analytical) meet the needs and requirements of its users.
In laboratory medicine, by convention, health-related population-based reference values are the most commonly used interpretative aid to diagnosis and case finding. The biological reference interval (RI), the interval between and including two reference limits, is commonly established from the central 95% distribution of results acquired from a sample of the reference population [4]. An accepted variation from this RI principle is the use of the 99th percentile of a healthy population for cardiac-specific troponin [5] and clinical decision limits for B-type natriuretic peptide (NT-proBNP) [6], cholesterol [7] and HbA1c [1, 8].
Given the central role that Rls play in laboratory result interpretation, the quality of the RI is as important as the quality of the laboratory result itself [9]. A myriad of factors impact the quality of RIs including the type of primary sample (serum versus heparin plasma (e.g., potassium and protein measurement)), sample handling, time from blood draw to sample processing (e.g., delays result in elevated potassium levels), interferences (e.g., haemolysis has the effect of increasing potassium and deceasing insulin concentrations), assay methodology, assay precision, specificity, detection limits, and the statistical approach used depend on sample size and the distribution of the data e.g., Gaussian or non-Gaussian and the characteristics of the reference population [1, 9]. Furthermore, separate RIs (data partitioning) may be required for different sub-populations or to take account of sex, age (paediatric populations), reproductive status (puberty, pregnancy, menopause), or race [9].
The process of defining the RI starts with the appropriate selection of the reference population which should comprise of individuals in good health that resemble as closely as possible the population where the test(s) will be applied. A major issue is how to define health. The World Health Organization (WHO) defines health as “a state of complete physical, mental and social wellbeing not just merely the absence of disease and infirmity” [10]. The Royal College of Physicians defines a “healthy volunteer” as “an individual who is not known to suffer any significant illness relevant to the proposed study, who should be within the ordinary range of body measurements” [11]. In clinical practice however, reference individuals are usually those deemed “apparently healthy” or at low risk of having disease using defined criteria.
In general, manufacturers provide users with RIs with limited detail on the characteristics of the reference population from which they were derived. Current best practice suggests that each laboratory establish RIs in the local population prior to introducing an assay into routine use [12]. Medical testing laboratories seeking accreditation compliance with ISO 15189:2012 are required to demonstrate that the biological reference intervals communicated to the users of their service are appropriate for the reference population, the patient population served and their analytical methodology [13]. It is also a requirement that laboratories periodically verify the appropriateness of their quoted RIs and in particular, following a change in methodology or the pre-analytical process [13]. This is very challenging and resource intensive. Moreover, in recent times with the emergence of hospital and laboratory networks, cognisance must be given to both national and international (the Irish RI Harmonisation Project (IRIHP) [14, 15], Pathology Harmony (PH) UK [16], Australasian Association for Clinical Biochemistry and Laboratory Medicine (AACB) [17]) efforts to harmonise RIs to reduce unwarranted variation in the work of the clinical laboratory and minimise confusion to service users.
The objective of this study was to define RIs for frequently requested biochemical/haematological parameters in a healthy adult Irish Caucasian population.
Methods
Ethical approval for this study was granted by the research ethics committees at Galway University Hospitals (GUH) and the National University of Ireland Galway (NUIG) (Ref GUH: C.A. 1404; Ref NUIG: 16-July-05). This study was conducted in accordance with the ethical principles as set out by the World Medical Association Declaration of Helsinki. It was part of a larger study which aimed to establish reference intervals for potentially novel biomarkers of renal functional decline [18,19,20]. Written informed consent was obtained from each participant prior to study initiation.
Study design
A cross-sectional study was conducted between March 2016 and December 2018 at GUH and NUIG to recruit healthy participants. Healthy participants were identified using posters displayed at GUH/NUIG and by word of mouth. All participants recruited were fully informed of the nature of the research via an initial briefing meeting and detailed information leaflet. Participants were also required to complete a comprehensive health questionnaire (Supplemental Fig. 1) to identify any medical conditions that could impact on their ability to participate in the study and ultimately the validity of the study.
Reference population
Inclusion criteria
The inclusion criteria were stringent and included signed informed consent, age ≥ 18 years, Caucasian Irish, body mass index (BMI) ≤ 30 kg/m2, systolic blood pressure (SBP) < 140 mmHg, diastolic blood pressure (DBP) < 90 mmHg, non-pregnant (self-reported), C-reactive protein (CRP) < 10 mg/L, haemoglobin (Hb) > 10 g/dL and the estimated glomerular filtration rate (eGFR) ≥ 60 mL/min/1.73 m2 (Fig. 1).
Exclusion criteria
The exclusion criteria included taking prescribed medication (not including contraceptives) or over the counter medications such as nonsteroidal anti-inflammatories (NSAIDs), herbal remedies (e.g., ginseng, ma huang) for a minimum of 2 weeks prior to the study, CRP > 10 mg/L, Hb < 10 g/dL eGFR < 60 mL/min/1.73m2 or previous or new diagnosis at time of enrolment of diabetes, cardiac, thyroid, liver or metabolic bone disease, anaemia or unwell in the previous 2 weeks, non-Caucasian or insufficient sample (Fig. 1).
Data collection
Following informed written consent, eligible participants were required to attend a study site to complete a health questionnaire (Supplemental Fig. 1) and undergo phlebotomy. Volunteers were not required to be fasting, and phlebotomy was performed with study participants seated as per usual practice. At this clinic visit baseline clinical demographics; age, gender ethnicity, BMI, current medication usage, smoking and pregnancy status (self-reported) were recorded. Weight was measured in kilograms using the Tanita® scale and height in metres using a Seca® wall-mounted stadiometer, according to departmental standard operating procedures. SBP and DBP were measured in mmHg using an automated oscillometric device (Omron®), after participants had been seated quietly for 5 min in accordance with the 2013 European Society of Hypertension/Cardiology guidelines [21]. Pulse rate was recorded at the radial artery in the dominant hand as beats per minute.
Sample size
The Clinical Laboratory Standards Institute (CLSI)/International Federation for Clinical Chemistry and Laboratory Medicine (IFCC) recommend the use of nonparametric methods to establish RIs [12]. This mandates 120 individual reference values to define the central 95% distribution of results and enable calculation of the 90% confidence interval (CI) of the lower and upper reference limits.
Sample collection
Each participant had venous whole blood collected into appropriate specimen tubes, one 7.5-mL (Becton Dickinson BD Vacutainer®) plain plastic for biochemical tests and two 3.5-mL BD potassium ethylenediaminetetraacetic acid (EDTA) plasma for measurement of glycated haemoglobin (HbA1c) and haematological parameters respectively.
Biochemical testing included renal profile (sodium (Na+), potassium (K+), chloride (Cl−), urea and creatinine), liver profile (albumin, total protein (T. Prot), bilirubin (T. Bili), alkaline phosphatase (ALP), alanine transaminase (ALT) and gamma-glutamyl transferase (GGT)), lipid profile (total cholesterol (T. Chol), triglycerides (TG), high-density lipoprotein cholesterol (HDL-c)), total calcium (T.Ca2+), inorganic phosphate (iPO4) and intact parathyroid hormone (iPTH)), transferrin, iron, HbA1c, CRP, uric acid (UA), thyroid function tests (free thyroxine (FT4) and thyroid-stimulating hormone (TSH)), N-terminal pro b-type natriuretic peptide (NT-proBNP) and high sensitivity troponin T (hsTnT).
Full blood count (FBC) analysis included white cell count (WCC), red cell count (RBC), Hb, haematocrit (Hct), mean cell volume (MCV), mean cell haemoglobin (MCH), mean cell haemoglobin content (MCHC) and quantitation of neutrophils, lymphocytes, monocytes, eosinophils, basophils, leucocytes and large unstained cells (LUCs).
Laboratory sample processing and analyses
Serum samples were maintained at room temperature (RT) for 30 min to allow clot formation and all specimens transported to the laboratory within 1 h of blood draw. On receipt to the laboratory, serum specimen tubes were labelled and placed on the Roche Cobas® C8100 Modular Pre-Analytical (MPA) automated workflow series. This system centrifuges samples, removes and inserts specimen tube caps as required, applies barcode labels to secondary tubes and prepares aliquots from primary samples. Samples introduced to the MPA are centrifuged at 3000 g for 10 min at RT and separated serum analysed in accordance with the tests requested on the Roche Cobas® modular analyser system. As per our routine practice samples were analysed once. For the period of this study, laboratory turnaround time audits determined that on average 88.9% (range 85.9–99.5) of routine samples received through Monday to Friday were processed and analyses completed within 2 h.
EDTA plasma for HbA1c were analysed within 2 days of sample receipt with haematological analysis performed within 2 h of phlebotomy. The estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease-Epidemiology Collaboration (CKD-EPI) formula [22]. LDL-c was derived using the Friedewald Eq. [23].
Analytical methods and performance specifications
Biochemical parameters
Serum renal, liver, bone and lipid profiles, CRP, UA, thyroid function tests, NT-proBNP and hsTnT were measured by standard laboratory methods on the Roche Cobas® 8000 modular analyser series (Roche Diagnostics Limited, West Sussex, UK). In addition, serum indices (Haemolysis (H), Lipaemia (L) and Icterus (I) that monitor an instrument’s response to detect and flag pre-analytical interference affecting analysis were performed on all samples.
HbA1c was measured using capillary electrophoresis on the Sebia Capillarys 3 automated haemoglobin analysers and the Sebia HbA1c Kit (product number: 2515). Within and between run analytical variation (CVA%) at a mean HbA1C concentration of 36 and 71 mmol/mol was < 1.4%. Analytical bias ranged from − 2.0 to 1.0 mmol/mol (Mean %Bias = 0.24) assessed using external quality assessment samples with IFCC HbA1C targets of 32, 43, 69, 36 and 53 mmol/mol respectively.
Haematological parameters
Haematological parameters including WCC, RBC, Haemoglobin, Hct, (derived MCV, MCH MCHC), platelet, neutrophils, lymphocytes, monocytes, eosinophils, basophils, leucocytes and LUCs were measured using Advia 2120 platforms within 2 h of sample receipt. Within and between run analytical variation (CVA%) were determined using three serum based control materials with low, normal and high) analyte concentrations run twice daily over a period of 5 days. Analytical bias determined by statistically comparing the levels/counts with external quality assessment samples over a 12-month period. Uncertainty of measurements (UoM) were determined from a minimum of 30 controls’ results from which the CV% for that test can be calculated.
Limits of detection (functional sensitivity) for the biochemical parameters were taken from the Roche kit inserts, whereas for the haematological parameters, it was determined by examining 4 specimens with low Hb and low WCC, RCC and platelet counts being serially diluted and analysed in replicates of five.
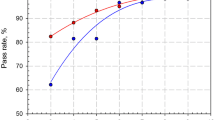
Statistical analyses: Establishing reference intervals
All data (clinical, biochemical/haematological, together with that obtained from the health questionnaires) were recorded using Microsoft® Excel 2016 to create the master database. Statistical analyses were carried out using Minitab® 17.1.0, MedCalc® Statistical Software (Version 18.2.1) and Analyse-it® (Version 17). Reference values within the respective assays’ reportable range were used to establish the reference intervals. For statistical purposes, where results were below an assay’s limit of detection (LoD), an arbitrary figure equal to the respective LoD was assigned. For example, the LoD for hsTroponin T is 3.0 ng/L, where participant results were less than 3.0 ng/L to allow statistical manipulation of the data, the result was recorded as 3.0 ng/L. The Analyse-it® (Version 17) statistical software was used to illustrate the data (histogram and box and whiskers plot), as an example see HbA1c (Fig. 2). The Shapiro-Wilk normality test was used to evaluate normality. The frequency distribution for the various analytes in a healthy Irish population were established and examined visually for apparent outliers (results that do not fit within the majority of reference values) [24]. All potential outliers were reviewed to out rule transcriptional, preanalytical and analytical (haemolysis, lipaemia) errors, or the inclusion of inappropriate reference values. Potential outliers were assessed in accordance with the criteria of Dixon [25] and Reed [26], which is supported by the IFCC working group [12]. In brief, an outlier was removed from the dataset if the difference between it and its nearest value (D) divided by the range of all values including the extremes (R); the D/R ratio [25, 26] was one-third or greater than R as proposed by the IFCC working group [12]. Where multiple outliers were present on the same side of the distribution, the one-third rule was applied to the least extreme outlier. If the rule rejects this outlier, then the more extreme outliers will automatically be rejected. If the rule does not reject this outlier, then all the outliers should be included or an alternative technique that considers all the outliers together should be applied [12]. In this study, in this scenario, the Tukey approach to outliers was used [27]. For each measurand, the data were divided according to gender and then subjected to the Harris and Boyd’s standard deviate test to investigate whether partitioning for gender was required [28]. The IFCC method that does not assume Gaussian type distribution was employed to establish the reference interval. Lower and upper RIs were estimated at the 2.5th and 97.5th percentiles, respectively. Where reference values were less than those required by the nonparametric method, the Robust method[29], which allows for fewer values and does not assume a Gaussian distribution was also used. This enabled calculation of the 90% CI of the respective RIs [12].
Results
Of 208 apparently healthy volunteers, 76 failed to meet the study inclusion criteria (Fig. 1). The reference population comprised of 132 participants of whom 49.2% were men; the median (range) age was 29.7 (18.1–62.2) years (Table 1). The analytical performance characteristics of the common biochemical/haematological parameters assessed over the period of this study (~ 2.8 years) are detailed in supplemental Table 1. Of note, multiple reagent lots for all analytes were used with no results reported without concomitant manufacturer independent IQC being within their respective specified limits. Furthermore, for the years 2016 to 2018 proficiency testing (EQA) for each parameter assessed was acceptable.
RIs for the majority of biochemical parameters assessed were broadly in accord with those provided by Pathology Harmony (PH) [16] and the Irish Reference Interval Harmonisation Project (IRIHP) (Table 2) and literature, alanine transaminase [30] and creatinine [31]. Some minor differences observed included: UA (upper limit), ALP (upper and lower limit), GGT (lower limit), cholesterol and LDL-c (greater than the decision threshold for cardiovascular risk [7], Iron (lower limit) (Table 2). Importantly, the RI defined for HbA1c; 27–37 mmol/mol was markedly different from that quoted nationally, HbA1c; 20–42 mmol/mol [32] and that established for albumin: 42–54 g/L compared with both Pathology Harmony (PH) [16] and the Irish Reference Interval Harmonisation Project (IRIHP) of 35—50 g/L (Table 2). Of note, minor differences were also observed between the locally established biochemical RIs and those provide by the manufacturer Roche Diagnostics.
RIs for the common haematological parameters assessed were generally in agreement with those provided by Bain et al. [33] /RIHP (Table 3). The 90% CI of the lower and upper limits of the established RIs are detailed in Tables 2 and 3. It was found that the lower limits (absolute values) of all the measured markers have considerably narrow 90% CI than the upper limits.
Discussion
Test results provided by medical testing laboratories are critical to clinicians managing patients, to patient safety and the generation of reliable quality data. Although the RI plays a key role in result interpretation, the impact of its quality and validity to the local population is often underappreciated [9]. By and large, RIs provided by the manufacturers offer scant information on the characteristics of the reference population from which they are established. ISO 15189:2012 requires medical testing laboratories to provide evidence that the health-related RIs provided to their service users are appropriate to the population served, their analytical methodology and are periodically verified [13]. The CLSI/IFCC recommends the use of nonparametric methods to establish RIs [12]. This is both onerous and complex, necessitating the selection of a minimum of 120 apparently healthy individuals to provide the requisite reference values to define the central 95% distribution of results with 90%CI.
The observation that the lower limits of all the measured markers have considerably narrow 90% CI than the upper limit highlights that the spread of results is greater at the upper reference limit. The CI is important to calculate as this provides a measure of the “experimental error” of the study due to the statistics and can indicate the need for more data and the significance of a difference between similar studies [9].
Indeed, stringent study criteria are essential to minimise the likelihood of common pathological conditions known to affect the concentration values of the analyte under investigation [1]. For the purpose of a reference interval study, establishing the health of participants is challenging. In this study, we excluded participants who potentially had or who during the study were diagnosed with self-reported illness, hypertension, thyroid dysfunction, anaemia, infection or obesity. Pregnancy was an exclusion criterion as separate trimester specific reference intervals would need to be derived for this population. Medical laboratories are also subject to external pressures such as hospital pathology networks, and in the future, preparedness for the national e-health framework and an electronic health record. These drivers require a prudent mix of good laboratory practice and pragmatism with respect to result reporting and RIs. RIs can only be harmonised for common analytes where reliable calibration and traceability are evident [17]
In this study and in accordance with the IFCC approved methodology, we established normative intervals for 37 routinely requested biochemical (n = 26; calculated: n = 2) and haematological (n = 11; derived: n = 3) parameters in an adult Irish population. The majority of RIs for common analytes were broadly in agreement with IRIHP [14, 15], PH [16] and the AACB [17]. In addition, the RIs for biochemical parameters were mostly in accord with the advice provided by the respective manufacturer (Supplemental Table 2). This likely reflects the European characteristics and age (20–71 years) of the reference population used to derive the RIs and the requirements of the in vitro diagnostic medical devices Directive (EU) 2017/746 [34]. Moreover, it suggests that Roche Diagnostics RIs are applicable to Irish adults.
The HbA1c RI derived in this study (27–37 mmol/mol) is almost identical to that previously established by our research group in healthy non-pregnant Caucasian women (HbA1c: 29–37 mmol/mol) [35] and the IFCC RI (HbA1c: 29–38 mmol/mol) defined in 120 Danish men and women without diabetes with normal glucose tolerance [36]. The nationally quoted RI for HbA1c of 20–42 mmol/mol has its provenance in the Diabetes Control and Complications Trial. This seminal trial determined that a HbA1c of 48–52 mmol/mol was the threshold for detecting an increase in the prevalence of significant diabetic retinopathy in people without a known diagnosis of diabetes and the risk of significant prevalent retinopathy below 42 mmol/mol as negligible [37]. Given that the precise lower cut-off point for risk has yet to be defined (continuum of risk), it is recommended that persons with a HbA1c level between 42 and 48 mmol/mol and at particularly high risk of developing diabetes might be considered for diabetes prevention interventions [38].
The Nationally quoted RI for HbA1c is a direct conversion from the DCCT units of 4% and 6% respectively used pre-standardisation of the HbA1c assay. The findings of this study and others [35, 36] suggest this practice should be reviewed in the light of the global standardisation of HbA1c assays in 2010. It could be argued that establishing RIs for HbA1c or lipid parameters are of little value given that clinical action points are employed for their result interpretation. However, these RI are informative for public health initiatives wishing to target dysglycaemia and dyslipidaemia as modifiable risk factors for diabetes and cardiovascular disease respectively [39].
In 2017, the first report on RIs for the FBC in adults in the Republic of Ireland (ROI) was published [15]. It determined that published literature, specifically a textbook series entitled, “Practical Haematology” [33], was the provenance of the majority of FBC RIs quoted in public haematology laboratories. The report’s authors acknowledged that while this ensured a certain degree of homogeneity, it was not ideal as the RIs used were neither instrument or population specific. The authors’ identified the requirement for up to date RIs for FBC in adults in the ROI to be established using current measurement technology. To our knowledge, the current study is the first to address this need and is the most comprehensive study establishing RIs for both routine biochemical and haematological parameters in a healthy Irish adult Caucasian population. As only healthy adult Caucasian participants were recruited to this study the reference intervals established are not generalisable to the whole Irish population. Strict inclusion and exclusion criteria were used to reduce the potential for confounders to impact the RIs. For all studies establishing reference intervals, the definition of health and the means of excluding disease are challenging and represent potential limitations/confounders. To confirm that participants do not have unknown disease at the time of sampling a period of follow-up would be required. To harmonise the establishment of reference intervals, we advocate the establishment of a uniform definition of health for reference interval studies by expert consensus. The absence of these agreed definitions of health could affect the reproducibility of the study. We acknowledge that this study has a relatively small sample size which impacted on our ability to partition the data for age.
Conclusions
RIs for the majority of biochemical/haematological parameters were broadly in accord with those provided by Pathology Harmony (UK)/Irish RI Harmonisation Project. Minor differences were observed in the RI of biochemical parameters provided by the manufacturer Roche Diagnostic suggesting that the manufacturers’ RIs are applicable to an adult Irish population. The normative biological intervals established in an adult Irish population for 37 commonly requested biochemical and haematological parameters will be a valuable aid to result interpretation in clinical laboratories, medical-decision making and other health related activities after appropriate verification in accordance with ISO 15189: 2012.
Disclaimer
The materials presented, and views expressed are the responsibility of the author(s) only. The EU Commission takes no responsibility for any use made of the information set out.
References
Ceriotti F, Henny J (2008) “Are my laboratory results normal?” Considerations to be made concerning reference intervals and decision limits. EJIFCC 19(2):106–114
Beastall GH (2013) Adding value to laboratory medicine: a professional responsibility. Clin Chem Lab Med 51(1):221–227
Hallworth MJ (2011) The ‘70% claim’: what is the evidence base? Ann Clin Biochem 48(Pt 6):487–488
Solberg HE (1986) Statistical treatment of reference values in laboratory medicine: testing the goodness-of-fit of an observed distribution to the Gaussian distribution. Scand J Clin Lab Invest Suppl 184:125–132
Thygesen K, Alpert JS, Jaffe AS et al (2018) Fourth universal definition of myocardial infarction 2018. Circulation 138(20):e618–e651
Ponikowski P, Voors AA, Anker SD et al (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37(27):2129–2200
Nordestgaard BG, Langsted A, Mora S et al (2016) Fasting is not routinely required for determination of a lipid profile: clinical and laboratory implications including flagging at desirable concentration cut-points-a joint consensus statement from the European Atherosclerosis Society and European Federation of Clinical Chemistry and Laboratory Medicine. Eur Heart J 37(25):1944–1958
Organization WH (2020) World Health Organization. Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus: Abbreviated report of a WHO consultation 2011 (WHO/NMH/CHP/CPM/11.1) [Available from: http://www.who.int/diabetes/publications/diagnosis_diabetes2011/en/. Accessed 30 Sept 2020
Jones G, Barker A (2008) Reference intervals. Clin Biochem Rev 29(Suppl 1):S93–S97
WHO (2020) World Health organization. Constitution of the World Health Organization—Basic documents, Forty-fifth edition, Supplement, October 2006 [cited 20.03.20. Available from: https://www.who.int/governance/eb/who_constitution_en.pdf. Accessed 30 Sept 2020
Research on healthy volunteers (1986) A report of the Royal College of Physicians. J R Coll Physicians Lond 20(4):243–257
CLSI (2008) Clinical and Laboratory Standards Institute EP28-A3c. Defining, establishing, and verifying reference intervals in the clinical laboratory; approved guideline—third edition. Wayne, PA: 2008
ISO15189 (2012) Medical laboratories—requirements for quality and competence. 3 ed. Geneva, Switzerland: International Organization for Standardization
HSE (2020) Health Service Executive. National Clinical Programme for Pathology (NCPP); The Irish Reference Interval Harmonisation Project 2016 [Available from: https://www.hse.ie/eng/services/publications/clinical-strategy-and-programmes/national-laboratory-handbook-volume-1.pdf. Accessed 04 Sept 2020
HSE (2020) Health Sevice Executive. National Clinical Programme for Pathology (NCPP); Survey report on reference intervals for the full blood count in the Republic of Ireland [Available from: https://www.hse.ie/eng/about/who/cspd/ncps/pathology/resources/report-on-reference-intervals-for-the-fbc-in-roi-november-2017.pdf. Accessed 10 Sept 2020
Berg J, Lane V (2011) Pathology harmony; a pragmatic and scientific approach to unfounded variation in the clinical laboratory. Ann Clin Biochem 48(Pt 3):195–197
Koerbin G, Tate JR (2016) Harmonising adult reference intervals in Australia and New Zealand—the continuing story. Clin Biochem Rev 37(3):121–129
Bian X, Griffin TP, Zhu X et al (2019) Senescence marker activin A is increased in human diabetic kidney disease: association with kidney function and potential implications for therapy. BMJ Open Diabetes Res Care 7(1):e000720
Hamon SM, Griffin TP, Islam MN et al (2019) Defining reference intervals for a serum growth differentiation factor-15 (GDF-15) assay in a Caucasian population and its potential utility in diabetic kidney disease (DKD). Clin Chem Lab Med 57(4):510–520
Griffin TP, Islam MN, Wall D et al (2019) Plasma dephosphorylated-uncarboxylated Matrix Gla-Protein (dp-ucMGP): reference intervals in Caucasian adults and diabetic kidney disease biomarker potential. Sci Rep 9(1):18452
Mancia G, Fagard R, Narkiewicz K et al (2013) 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 34(28):2159–2219
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Tremblay AJ, Morrissette H, Gagne JM et al (2004) Validation of the Friedewald formula for the determination of low-density lipoprotein cholesterol compared with beta-quantification in a large population. Clin Biochem 37(9):785–790
Burtis CA, Ashwood ER, Bruns DE et al (2008) TIETZ Fundamentals of Clinical Chemistry. 6 ed: Saunders Elsevier
Dixon W (1953) Processing data for outliers. Biometrics 9:74–89
Reed AH, Henry RJ, Mason WB et al (1971) Influence of statistical method used on the resulting estimate of normal range. Clin Chem 17(4):275–284
Tukey JW (1977) Exploratory Data Analysis. . Reading, Mass. Addison-Wesley Pub. Co., ©1977.
Harris EK, Boyd JC (1990) On dividing reference data into subgroups to produce separate reference ranges. Clin Chem 36(2):265–270
Horn PS, Pesce AJ, Copeland BE et al (1998) A robust approach to reference interval estimation and evaluation. Clin Chem 44(3):622–631
Kwo PY, Cohen SM, Lim JK et al (2017) ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries. Am J Gastroenterol 112(1):18–35
Ceriotti F, Boyd JC, Klein G et al (2008) Reference intervals for serum creatinine concentrations: assessment of available data for global application. Clin Chem 54(3):559–566
HSE (2020) Health Service Executive. Information for Health Care Professionals regarding Diabetes: international change to HbA1c results. 2010 [20.02.20]. Available from: https://www.hse.ie/eng/services/publications/topics/diabetes/hba1c-information-for-health-care-professionals-regarding-diabetes.pdf. Accessed 10 Sept 2020
Bain BJ, Bates I, Laffan MSL et al (2011) Reference ranges and normal values. In: Dacie and Lewis, editor. Practical Haematology 11th ed. London Churchill Livingstone; p. 14–7
HPRA (2020) Health Protection Regulatory Authority: In-Vitro Diagnostic Medical Device Regulations 2017/746 [Available from: https://www.hpra.ie/homepage/medical-devices/regulatory-information/new-eu-device-regulations. Accessed 10 Sept 2020
O’Connor C, O’Shea PM, Owens LA et al (2011) Trimester-specific reference intervals for haemoglobin A1c (HbA1c) in pregnancy. Clin Chem Lab Med 50(5):905–909
Jeppsson JO, Kobold U, Barr J et al (2002) Approved IFCC reference method for the measurement of HbA1c in human blood. Clin Chem Lab Med 40(1):78–89
Diabetes Control Complications Trial Research Group, Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O et al (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 329(14):977–86
WHO (2021) Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes Mellitus: Abbreviated Report of a WHO Consultation. Geneva: World Health Organization; 2011. 2, Glycated haemoglobin (HbA1c) for the diagnosis of diabetes. Available from: https://www.ncbi.nlm.nih.gov/books/NBK304271/. Accessed 20 Jan 2021
Hughes D, Crowley J, O'Shea P (2020) Lipid reference values in an Irish population. Ir J Med Sci
Acknowledgements
We wish to express our gratitude to all volunteers who made this study possible. Special thanks to the scientific, nursing and medical staff at the Centre for Endocrinology, Diabetes and Metabolism and the Departments of Clinical Biochemistry and Haematology at Saolta University Health Care Group (SUHCG), University Hospital Galway.
Funding
TPG is supported by a Hardiman Scholarship from the College of Medicine, Nursing and Health Science, National University of Ireland, Galway, and a bursary from the Irish Endocrine Society/Royal College of Physicians of Ireland. The authors are supported by grants from the European Commission: Horizon 2020 Collaborative Health Project NEPHSTROM (grant number 634086; TPG, NI, MDG), FP7 Collaborative Health Project VISICORT (grant number 602470; MDG), Science Foundation Ireland: REMEDI Strategic Research Cluster (grant number 09/SRC-B1794; MDG), CÚRAM Research Centre (grant number 13/RC/2073; MDG) and by the European Regional Development Fund.
Author information
Authors and Affiliations
Contributions
MNI: Recruitment, consenting and pre-testing preparation of participants, sample collection and processing, data acquisition, assembly, analysis and interpretation; TPG: medical assessment, recruitment, consenting and pre-testing preparation of participants, sample collection and processing, data acquisition and assembly; RW: Recruitment, consenting, and pre-testing preparation of participants and sample collection; SH: sample processing and analytical analyses; LB: quality and accuracy of laboratory methods; DGG: quality and accuracy of laboratory methods and interpretation; MDG: study design, data analysis and interpretation; BC: analytical analyses, quality and accuracy of laboratory methods; JK: quality and accuracy of laboratory methods and interpretation PMOS: conception, study design, quality and accuracy of laboratory methods, data acquisition, assembly, statistical analysis and interpretation. MNI: first draft of manuscript. All authors reviewed, edited and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was granted by the Clinical Research Ethics Committee, Galway University Hospitals (Ref: C.A. 1404) and the National University of Ireland, Galway Research Ethics Committee (Ref: 16-July-05).
Competing interests
The authors declare that they have no conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
11845_2021_2535_MOESM1_ESM.doc
Supplementary file1: Supplemental Table 1: Analytical Performance Specifications of the biochemical/haematological parameters (DOC 267 KB)
11845_2021_2535_MOESM2_ESM.docx
Supplementary file2: Supplemental Table 2: Established reference intervals in Irish adults for commonly requested biochemical tests compared to those provided by Roche Cobas® (DOCX 20 KB)
Rights and permissions
About this article
Cite this article
Islam, M.N., Griffin, T.P., Whiriskey, R. et al. Reference intervals for commonly requested biochemical and haematological parameters in a healthy Irish adult Caucasian population. Ir J Med Sci 191, 301–311 (2022). https://doi.org/10.1007/s11845-021-02535-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-021-02535-0