Abstract
Background
A left ventricular assist device (LVAD) is used to support patients with end-stage heart failure.
Aims
To examine the role of comorbidities and complications in predicting in-hospital mortality since the introduction of continuous flow (CF)-LVAD.
Methods
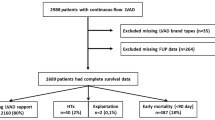
The Nationwide Inpatient Sample was queried from 2010 to 2014 using International Classification of Disease-9 code for LVAD among patients 18 years or older. The sample consisted of 2,359 patients (mean age = 55 ± 13.7 years, 76.8% men, 59.3% Caucasian).
Results
Comparative analysis revealed mortality did not differ from 2010 to 2014 (p = 0.653). Increases in comorbidities of atrial fibrillation, acute kidney injury, mechanical ventilation, body mass index ≥ 25, cerebrovascular disease, and mild liver disease were evidenced over the 5-year period (p values ≤ 0.049). Multivariate analysis showed that significant predictors of mortality were comorbid hemodialysis (AOR = 7.62, 95% CI [4.78, 12.27]), cerebrovascular disease (AOR = 5.38, 95% CI [3.49, 8.26]), mechanical ventilation (AOR = 3.83, 95% CI [2.84, 5.18]), mild liver disease (AOR = 1.96, 95% CI [1.38, 2.76]), and acute kidney injury (AOR = 1.62, 95% CI [1.16, 2.28]). Predictive complications included disseminated intravascular coagulation (AOR = 6.41, 95% CI [2.79, 6.84]), sepsis (AOR = 4.37, 95% CI [2.79, 6.84]), septic shock (AOR = 3.9, 95% CI [2.11, 7.59]), and gastrointestinal bleed (AOR = 1.81, 95% CI [1.11, 2.93]).
Conclusions
CF-LVADs have not reduced mortality, possibly due to utilization in patients with comorbid conditions. Future trials are necessary for improved patient selection and reduced post-procedural complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heart failure (HF) is a growing global pandemic. Currently, the USA has about 5.7 million people who have suffered from HF. A 46% increase in the prevalence of HF is expected by 2030, due to an aging population and increased life expectancy in the population [1]. Heart failure is characterized by two distinct subtypes: heart failure with reduced ejection fraction (i.e., left ventricular ejection fraction rate of < 40% (HFrEF) and heart failure with preserved ejection fraction (HFpEF). The management of HFrEF includes lifestyle modifications, pharmacologic agents, as well as implantation of implantable cardioverter-defibrillator and cardiac resynchronization therapy. Acute decompensations in the clinical condition may require hemodynamic support in the form of an intra-aortic balloon pump (IABP), an axial-flow pump placed in the left ventricle and even extracorporeal membrane oxygenation (ECMO) for short-term support. Some patients’ symptoms continue to progress, and they develop refractoriness to maximally tolerated standard medical therapy, which may necessitate the use of advanced therapies including a more permanent left ventricular assist devices (LVAD) or even heart transplantation [2,3,4]. With the growing prevalence of HF, there has been a shortage of heart donors resulting in increased use of LVADs [2, 4,5,6]. LVADs act as a mechanical pump to support the hemodynamic needs of the body and are now used as a either a bridge to transplantation (BTT) or recovery, a bridge to an appropriate decision or even as destination therapy (DT) [5, 7, 8]. In 2001, the REMATCH trial showed a 48% reduction in the risk of death from any cause in the group that received an LVAD, as compared with the medical therapy group [9].
LVADs are divided into first-, second-, and third-generation categories based on their mechanism of operation. The first generation of ventricular assist devices is pulsatile flow (PF-LVAD) pumps. These devices have limitations including a larger size, limited long-term durability, need for extensive surgical dissection, and higher rates of complications such as infections and device failure [9]. Second-generation (axial flow pumps) and third-generation devices (centrifugal flow pumps) overcome these limitations by using rotary pump technology to provide blood flow with reduced pulsatility [10, 11]. Continuous flow (CF) LVADs are smaller, quieter, and more durable and have improved survival when compared with pulsatile-flow devices [12,13,14]. Given these benefits, the use of continuous flow pumps has increased significantly from the years 2007 to 2013, accompanied by gradual reduction in the use of PF-LVADs [10]. As per the Sixth INTERMACS annual report, CF-LVADs were approved for BTT in 2008 and for DT in 2010 and CF-LVADs accounted for 100% of patients receiving DT since 2010 and more than 95% of all patients receiving LVADs [10, 12].
Although data suggests that newer LVADs are associated with a mortality benefit, those devices are not without complications. The main complications are device thrombosis and its ramifications such as pump failure and stroke along with gastrointestinal bleeding and sepsis [15]. Non-surgical bleeding is a major cause of morbidity and mortality in patients with LVADs [16], and it poses a major challenge to patient utilization of LVADs. We aimed to determine the trends in utilization of LVADs and identify determinants of mortality in patients receiving LVADs following the introduction of newer-generation devices, and we also sought to evaluate if the predicted mortality reduction anticipated with these devices is realized in a real-world setting.
Participants and methods
Data source
The data was obtained for the years 2010 to 2014 from the National Inpatient Sample (NIS) database, which forms part of the Healthcare Cost and Utilization Project (HCUP) [16]. The database was created by the agency for healthcare research and quality and contains data on 5 to 8 million hospital stays from approximately 1,000 hospitals. It was designed to include data from a 20% sample of discharges from all participating hospitals, which reduces the margin of error for estimates and delivers more stable and precise estimations. All states that participate in the HCUP provide data to the NIS, which covers > 95% of the US population. The database includes data from all nonfederal, short-term, general, and other specialty hospitals in the USA (excluding rehabilitation and long-term acute care hospitals) in the form of de-identified patient information containing demographics, discharge diagnoses, comorbidities, procedures, outcomes, and hospitalization costs. Because the NIS database is publicly available and contains de-identified patient information, no approval from the local Institutional Review Board was necessary.
Participant selection and covariates
We used the International Classification of Diseases, 9th Revision procedure code (ICD-9) of 37.66 (Insertion of Implantable Heart Assist System), in any procedure field among patients 18 years or older. We excluded patients with incomplete data for gender and mortality. To reduce the possibility of data duplication, we excluded patients with an indicator of transfer to another acute care facility. Patient baseline characteristics included age, sex, race, insurance, and hospital region. Comorbidities and complications were identified using ICD-9 codes in the diagnosis fields, and procedures were identified using ICD-9 codes in the procedure fields. The Charlson Comorbidity Index Score was categorized as 0, 1, 2, or ≥ 3. Supplementary Table 1 lists the ICD-9-CM and Clinical Classification Software codes used to identify comorbidities and procedures.
Statistical analysis
A series of comparative analyses were computed to identify trends in patient and hospital characteristics, mortality, comorbidities, and complications. Differences between continuous variables were assessed using one-way analysis of variance tests, whereas differences involving categorical variables were tested using the Chi-squared test of independence or Fisher’s exact test. Predictors of in-patient mortality were examined using a hierarchical multivariate binary logistic regression analysis. Patient characteristics (i.e., age, sex, and length of stay) were entered in block 1, while comorbidities and complications were entered in block 2. Because ≤ 0.17% of the total sample were diagnosed with a comorbidity of dementia, human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS), or metastatic solid tumor, each of those variables was omitted from the multivariate analysis. All statistical analyses were performed in R Core Team, 2019 [17, 18], with the type I error rate set to 0.05.
Results
Sample characteristics, descriptive statistics, and comparisons of trends from 2010 to 2014 are reported in Table 1. Our analysis resulted in 2,359 unweighted records representing 20% of the population. The total number of LVADs increases steadily from 380 in 2010 to 548 in 2014. The mean age of the sample was 55 ± 13.7 years, most of which were men (76.8%) and white (59.3%). The highest proportion of patients were in South region (41.4%) and covered by Medicare (45.9%). Over the 5-year period, the mean length of stay was 33.18 ± 26.23 days, and the mean total charges for hospitalization were $772,175.90 ± 498,689.70. Although mean length of stay did not vary over the 5-year period (p = 0.250), there was a significant increase in mean hospital charges (p < 0.001). Overall mortality was 17.1% and did not differ significantly from the year 2010 to 2014 (p = 0.653).
Increases in comorbidities of atrial fibrillation, acute kidney injury, mechanical ventilation, body mass index ≥ 25, cerebrovascular disease, and mild liver disease were evidenced over the 5-year period (all p values ≤ 0.049). The more frequent complications associated with LVAD were sepsis and severe sepsis (11.8%), gastrointestinal bleed (7.5%), septic shock (5.5%), disseminated intravascular coagulation (2.2%), and arterial embolism and thrombosis (1.7%).
The multivariate binary logistic regression analysis (see Table 2) was statistically significant, with model fit improving substantially from block 1 to block 2, ΔNagelkere R2 = 0.47, p < 0.001. On review of comorbidities, hemodialysis (AOR = 7.62, 95% CI [4.78, 12.27]), cerebrovascular disease (AOR = 5.38, 95% CI [3.49, 8.26]), and mechanical ventilation (AOR = 3.83, 95% CI [2.84, 5.18]) showed the strongest association with mortality. Though not as strongly associated, mild liver disease (AOR = 1.96, 95% CI [1.38, 2.76]) and acute kidney injury (AOR = 1.62, 95% CI [1.16, 2.28]) were also significant predictors of mortality. Among complications, disseminated intravascular coagulation (AOR = 6.41, 95% CI [2.79, 6.84]), sepsis and severe sepsis (AOR = 4.37, 95% CI [2.79, 6.84]), septic shock (AOR = 3.9, 95% CI [2.11, 7.59]), and gastrointestinal bleed (AOR = 1.81, 95% CI [1.11, 2.93]) were each associated with an increased likelihood of mortality.
Discussion
In an effort to track the ongoing improvement of increased utilization of LVADs, this study explored trends and examined the role of comorbidities and complications as predictors of in-hospital mortality since the introduction of newer LVADs. The findings of this study indicated that there was an increase in the utilization of LVADs from 2010 to 2014. Although we did not directly compare patients receiving CF-LVADs versus PF-LVADs, prior research has reported improved survival with CF-LVADs compared with PF-LVADs [12]. A reasonable expectation is that there would be an improvement in the survival trends in patients with LVADs over the 5-year period, given improvements in operative techniques, perioperative care, and surgical and institutional experience with CF-LVADs. On the contrary, the findings of this study indicate that in-hospital mortality did not decline from 2010 to 2014. The Sixth INTERMACS annual report also showed that survival has remained unchanged in patients with CF-LVADs from 2008 to 2013 [10].
Using the Charlson Comorbidity Index to compare prevalence of comorbidities [19] from 2010 to 2014, there was evidence of higher comorbidity burden and poorer health in patients with LVADs. There was a 7.2% increase in patients with LVADs who had a Charlson’s score of ≥ 3 between 2010 and 2014, which supports a gradual increase in comorbidities among these patients. This pattern is similar to the trends reported in earlier studies, which have showed an increase in the comorbidity burden over the years in patients with LVADs [12]. There was also evidence of an increase in specific comorbidities over the 5-year period, including atrial fibrillation, acute kidney injury, mechanical ventilation, body mass index ≥ 25, cerebrovascular disease, and mild liver disease. The findings of the study also offer further insight into the role of comorbidities in predicting in-hospital mortality. Specifically, cerebrovascular disease, mechanical ventilation, mild liver disease, and acute kidney injury were found to be independent predictors of in-hospital mortality among patients with LVADs. Poorer patient health, along with insufficient consideration to and treatment of relevant comorbidities, is a possible reason for the sustained mortality rate in patients with these devices. Improving patient selection is one way in which desirable patient outcomes are likely to be achieved.
CF-LVADs have been associated with a lower rate of adverse events, possibly because they are smaller size and have lower thrombotic potential [10, 13, 14, 20]. Although surgical implantation of CF-LVADs is generally less traumatic compared with older generation devices, there was no evidence to suggest that incidence of GI bleed, DIC, and sepsis and severe sepsis in patients with LVADs declined over the 5-year period examined in this study. Consistency in trends of these complications linked to LVADs could explain the stability in mortality rates that were found over this period of time. In line with the Eighth annual INTERMACS report [21], the findings of this study showed that sepsis and severe sepsis, septic shock, and GI bleed are the most frequent adverse events associated with LVADs [15, 21, 22]. Strictly adhering to infection control guidelines [16], meticulous surgical technique for hemostasis, and optimal postoperative surgical site care [18] are some of the ways to mitigate device-related infection and bleeding complications. LVAD placement in patients with active infection should be avoided, given active infection has been identified as an independent predictor of in-hospital mortality [23]. Because LVADs require systemic anticoagulation, careful consideration should also be given to the potential implications of GI bleeding when these devices are used in patients at high risk of peptic ulcer disease and consider more aggressive screening strategies [15, 24]. Blood transfusion in patients with LVADs could predispose them to right heart failure and transfusion-related infections [25,26,27]. Liver and renal disease in the patients with LVADs can also heighten risk of bleeding [28, 29]. Previous studies have found that the risk of bleeding in patients with LVADs is significantly higher compared with the risk of thromboembolic events, indicating that anticoagulation should be used with caution [30,31,32,33]. Another finding in our study is that there was a significant increase in the cost of hospitalization over the 5-year period. To further reduce the rate of mortality and cost of hospitalization among patients with LVADs, it is essential that further emphasis be placed on patient selection, improved screening methods, appropriate management of comorbidities and complications, developing innovative devices, and improving post-implantation care.
Study limitations
Certain limitations of our study must be acknowledged. The NIS is an administrative database, and the accuracy of the data depends highly on the training and expertise of the coders. We were not able to determine the time of onset, duration, type or severity of comorbidities, complications occurring during the recorded hospitalization, temporal relation between LVAD placement, and the time of occurrence of complications [34]. Long-term outcomes could not be estimated, as the available data are cross-sectional. Right ventricular failure [25] is an important complication associated with LVAD use, and it could not be assessed because a separate ICD-9 code was not available. The database is also limited to in-hospital events, and data on the New York Heart Association Functional Class, medications, echocardiography data, preoperative risk, or INTERMACS levels were unavailable [12]. The findings of this study are germane to the LVAD population in the USA and may not be generalized to the LVAD population in other countries.
Conclusion
The findings of this study provide insight into the role of comorbidities and complications linked to LVADs. Considering further mortality reduction has not been achieved since CF-LVADs were initially introduced and the various complications linked to these newer devices, future clinical trials and scoring systems are needed to improve patient selection at the outset and reduce the likelihood of post-implantation complications, which should lead to improved clinical outcomes.
References
Savarese G, Lund LH (2017) Global public health burden of heart failure. Card Fail Rev 3:7. https://doi.org/10.15420/cfr.2016:25:2
Mulloy DP et al (2013) Orthotopic heart transplant versus left ventricular assist device: a national comparison of cost and survival. J Thorac Cardiovasc Surg 145:566–574. https://doi.org/10.1016/j.jtcvs.2012.10.034
Vallabhajosyula S et al (2018) Temporary mechanical circulatory support for refractory cardiogenic shock before left ventricular assist device surgery. J Am Heart Assoc 7:010193. https://doi.org/10.1161/JAHA.118.010193
Stevenson, L.W (2015) Crisis awaiting heart transplantation: sinking the lifeboat. JAMA internal medicine 175:1406-1409. https://doi.org/10.1001/jamainternmed.2015.2203
Miller L et al (2007) Use of a continuous-flow device in patients awaiting heart transplantation. N Engl J Med 357:885–896. https://doi.org/10.1056/NEJMoa067758
Vaidya Y, Dhamoon AS (2019) Left ventricular assist devices (LVAD). StatPearls Publishing
Fang JC (2009) Rise of the machines—left ventricular assist devices as permanent therapy for advanced heart failure. N Engl J Med 361:2282–2285. https://doi.org/10.1056/NEJMe0910394
Hunt SA, Frazier O (1998) Mechanical circulatory support and cardiac transplantation. Circulation 97:2079–2090. https://doi.org/10.1161/01.CIR.97.20.2079
Rose EA et al (2001) Long-term use of a left ventricular assist device for end-stage heart failure. N Engl J Med 345:1435–1443. https://doi.org/10.1056/NEJMoa012175
Kirklin JK et al (2014) Sixth INTERMACS annual report: a 10,000-patient database. J Heart Lung Transplant 33:555–564. https://doi.org/10.1016/j.healun.2014.04.010
Frazier O et al (2007) Initial clinical experience with the HeartMate® II axial-flow left ventricular assist device. Tex Heart Inst J 34:275
Shah N et al (2016) National trends in utilization, mortality, complications, and cost of care after left ventricular assist device implantation from 2005 to 2011. Ann Thorac Surg 101(4):1477–1484. https://doi.org/10.1016/j.athoracsur.2015.09.013
Slaughter MS et al (2010) Clinical management of continuous-flow left ventricular assist devices in advanced heart failure. J Heart Lung Transplant 29:1. https://doi.org/10.1016/j.healun.2010.01.011
Slaughter MS et al (2009) Advanced heart failure treated with continuous-flow left ventricular assist device. N Engl J Med 361:2241–2251. https://doi.org/10.1056/NEJMoa0909938
Joy PS et al (2016) Risk factors and outcomes of gastrointestinal bleeding in left ventricular assist device recipients. Am J Cardiol 117:240–244 https://doi.org/10.1016/j.amjcard.2015.10.041
Suarez J et al (2011) Mechanisms of bleeding and approach to patients with axial-flow left ventricular assist devices. Circ Heart Fail 4:779–784. https://doi.org/10.1161/CIRCHEARTFAILURE.111.962613
Wang, E.S., et al. (2019) Impact of preoperative specialty consults on hospitalist comanagement of hip fracture patients.
R Core Team. (2019) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org/.
Quan H et al (2011) Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 173:676–682. https://doi.org/10.1093/aje/kwq433
Kirklin JK et al (2013) Fifth INTERMACS annual report: risk factor analysis from more than 6,000 mechanical circulatory support patients. J Heart Lung Transplant 32:141–156. https://doi.org/10.1016/j.healun.2012.12.004
Kirklin JK et al (2017) Eighth annual INTERMACS report: special focus on framing the impact of adverse events. J Heart Lung Transplant 36:1080–1086. https://doi.org/10.1016/j.healun.2017.07.005
Chinn R et al (2005) Multicenter experience: prevention and management of left ventricular assist device infections. ASAIO J 51:461–470. https://doi.org/10.1097/01.mat.0000170620.65279.aa
O’Horo JC, et al. (2018) Left ventricular assist device infections: a systematic review. ASAIO journal (American Society for Artificial Internal Organs: 1992) 64:287–294. https://doi.org/10.1097/MAT.0000000000000684
Kreuziger LMB (2015) Management of anticoagulation and antiplatelet therapy in patients with left ventricular assist devices. J Thromb Thrombolysis 39:337–344. https://doi.org/10.1007/s11239-014-1162-6
Matthews JC et al (2008) The right ventricular failure risk score: a pre-operative tool for assessing the risk of right ventricular failure in left ventricular assist device candidates. J Am Coll Cardiol 51:2163–2172. https://doi.org/10.1016/j.jacc.2008.03.009
Fida N et al (2015) Predictors and management of right heart failure after left ventricular assist device implantation. Methodist DeBakey Cardiovasc J 11:18. https://doi.org/10.14797/mdcj-11-1-18
Bihl F et al (2007) Transfusion-transmitted infections. J Transl Med 5:25. https://doi.org/10.1186/1479-5876-5-25
Kujovich, J.L (2015) Coagulopathy in liver disease: a balancing act. Hematology 2014, the American Society of Hematology Education Program Book 243-249. https://doi.org/10.1182/asheducation-2015.1.243
Lutz J et al (2014) Haemostasis in chronic kidney disease. Nephrol Dial Transplant 29:29–40. https://doi.org/10.1093/ndt/gft209
Boyle AJ et al (2009) Low thromboembolism and pump thrombosis with the HeartMate II left ventricular assist device: analysis of outpatient anti-coagulation. J Heart Lung Transplant 28:881–887. https://doi.org/10.1016/j.healun.2009.05.018
John R et al (2008) Low thromboembolic risk for patients with the Heartmate II left ventricular assist device. J Thorac Cardiovasc Surg 136:1318–1323. https://doi.org/10.1016/j.jtcvs.2007.12.077
Strüber M et al (2008) HeartMate II left ventricular assist device; early European experience. Eur J Cardiothorac Surg 34:289–294. https://doi.org/10.1016/j.ejcts.2008.05.011
John R et al (2008) Improved survival and decreasing incidence of adverse events with the HeartMate II left ventricular assist device as bridge-to-transplant therapy. Ann Thorac Surg 86:1227–1235 https://doi.org/10.1016/j.athoracsur.2008.06.030
Wu CP et al (2017) National trends in admission for aspiration pneumonia in the United States, 2002-2012. Ann Am Thorac Soc 14:874–879. https://doi.org/10.1513/AnnalsATS.201611-867OC
Availability of data and material
All data is publicly available.
Code availability
Code available on request.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Karthik Gonuguntla, Shivaraj Patil, Richard Gregory Cowden, Manish Kumar, Chaitanya Rojulpote, and Abhijit Bhattaru. The first draft of the manuscript was written by Karthik Gonuguntla, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 13.7 kb).
Rights and permissions
About this article
Cite this article
Gonuguntla, K., Patil, S., Cowden, R.G. et al. Predictors of in-hospital mortality in patients with left ventricular assist device. Ir J Med Sci 189, 1275–1281 (2020). https://doi.org/10.1007/s11845-020-02246-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-020-02246-y