Abstract
Background
Diabetic foot ulcers (DFU) are associated with an increased risk of lower limb amputation and death. Reported mortality rates for patients with DFU are as high as 50% after 5 years.
Aims
The aim of this retrospective study was to examine the 5-year clinical outcomes of patients with high-risk diabetic foot disease attending a specialist foot clinic in Beaumont Hospital between 2007 and 2010.
Methods
Clinical information was obtained from the CELLMA electronic patient record and laboratory results were extracted from the Beaumont Hospital information system.
Results
In total, data from 98 patients, who attended the foot clinic over the 4-year period, was collected. The 5-year mortality rate was 13.3% with an amputation rate of 28.6%. A significant proportion of patients (33.7%) had recurrent/new DFU after 5 years of follow-up. In this cohort, there was no association between poor glycaemic control, presence of co-existent cardiovascular disease or renal failure, and increased mortality or amputation.
Conclusions
Diabetic foot disease is an important cause of morbidity and mortality in clinical practice. It remains to be seen whether implementation of the national model of foot care in 2011 will improve outcomes for patients with high-risk diabetic foot disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes affects over 6% of the adult Irish population and diabetic foot disease is one of the most common, costly, and debilitating complications of diabetes. In a recent study of over 800 patients with diabetes in the west of Ireland, the proportion of patients at moderate and high risk of future foot ulceration was 25% and 11% respectively [1]. Furthermore, the annual incidence of lower limb ulceration in patients with diabetes in Ireland is 2.2–7% [2].
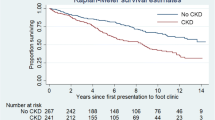
Diabetic foot ulcers (DFUs) are associated with mortality, and patients with DFUs have a greater than two-fold increased risk of death compared to patients with diabetes who do not develop foot ulcers [3, 4]. This is independent of age, smoking history, type and duration of diabetes, treatment regimen and glycaemic control [3]. Similarly, a 5-year prospective study of mortality in patients with lower limb ulceration showed that patients with DFUs had a reduced 5-year survival rate of 43% compared to patients without DFUs (56%) [5].
In addition to the excess mortality related to diabetic foot disease, foot ulcers are also an important cause of morbidity and long-term disability. DFUs are the most common cause of lower limb amputations, which are 22 times more common in patients with diabetes compared to the non-diabetic population [6].
Diabetic foot disease is an eminently preventable disease, with improved outcomes observed following the introduction of screening tools for GPs and dedicated multidisciplinary diabetic foot care clinics. Numerous retrospective studies have shown a reduction in the number of amputations following the implementation of an MDT diabetic foot clinic [7,8,9], whilst Dargis et al., in a prospective study, reported reduced DFU recurrence following introduction of a multidisciplinary approach to diabetic foot care [10]. The national diabetes foot care audit, performed in England between 2014 and 2016, demonstrated that early referral to a specialist diabetes foot service correlated with a higher rate of ulcer resolution at 12 weeks [11]. Of those patients seen in a specialist foot clinic within two weeks of initial presentation, ~ 50% were ulcer-free 12 weeks later, compared to 35% of those patients seen 2 months after initial presentation [11]. Our own hospital has a long tradition of a specialist multidisciplinary foot clinic for patients with active diabetic foot disease and we were keen to determine the 5-year outcomes of patients with diabetic foot ulcers attending our diabetic foot service. The primary outcomes under investigation were rate of ulcer recurrence, amputation and mortality at 5 years.
Methods
A retrospective review of all the patients who attended the Diabetic Foot Clinic in Beaumont Hospital between 2007 and 2010 was conducted. From 2007 until 2010, this clinic was staffed by a consultant endocrinologist with a specialist interest in diabetic foot disease, an endocrine specialist registrar, a diabetes nurse specialist, a podiatrist, an orthotist and a consultant vascular surgeon. Consults could also be sent to a consultant orthopaedic surgeon and to the physiotherapy department when required. Only patients with high-risk diabetic foot disease or an active diabetic foot ulcer were seen in this clinic. Referrals to the diabetic foot clinic came from the general diabetes clinics and diabetes day centre which provides diabetes care for its local catchment area of 300,000 people. Beaumont Hospital diabetes foot MDT acted as a regional service for the people of the north-east region of Ireland and patients with active foot disease were seen as soon as possible by either the podiatry or diabetes department within the hospital.
To ascertain the clinical characteristics of this patient cohort, patient information was obtained from the CELLMA electronic patient database, which is updated during each patient visit to the clinic. Details on the following clinical characteristics were collected: type of diabetes, medications, smoking status and comorbidities including cardiovascular disease, cerebrovascular disease, peripheral vascular disease, peripheral neuropathy, nephropathy and chronic kidney disease.
Laboratory information was obtained from the Beaumont Hospital Patient Information Profile Explorer (P.I.P.E) system, and included glycated haemoglobin (HbA1c), lipid profiles and urine albumin: creatinine ratio and serum creatinine measurement. Laboratory outcomes at presentation and at 5 years were recorded.
Finally, the 5-year outcome for each patient was recorded, thereby stratifying each patient into one of the following outcome groups; resolved ulcerating foot disease, unhealed/recurrent ulcerating foot disease, amputation and death. Of note, no distinction was made between single and multiple ulcers. Specific details on type of amputation (minor/major) were not recorded in the database and therefore not available for the study.
Statistical analysis was performed using SPSS version 22.0. Descriptive statistics was utilised to summarise baseline laboratory data. Data is expressed as mean +/− standard deviation. Odds ratios were calculated to determine associations of clinical variables with 5-year outcomes.
Results
In total, 98 patients attended the clinic over the 4-year period between 2007 and 2010. All patients had a history of a diabetic foot ulcer. In this cohort, 63.3% of patients had type 2 diabetes mellitus (T2DM) and 20.4% of patients had type 1 diabetes mellitus (T1DM). Information on type of diabetes was missing for 16.3% of patients. In terms of medications, 33.7% of patients were on oral hypoglycaemic agents and 50% of patients were on insulin (multiple daily injections/mixed insulin/basal insulin). In this cohort, 49% of patients had co-existent cardiovascular disease (coronary artery disease, stroke or peripheral arterial disease), 61.2% of patients were taking a statin and 67.3% of patients were on aspirin. Only 5.1% of patients in this study were smokers although this is likely underestimated as prior smoking history was not recorded in the database and this information was missing in 40% of cases.
Overall, this cohort of patients with diabetes demonstrated good glycaemic control and a favourable lipid profile. The mean HbA1c for this population of patients on first visit to the foot clinic was 7.53% (+/− 1.90%), with only 43.9% of patients demonstrating an HbA1c level greater than 7%. The mean total cholesterol was 3.96 mmol/l (+/− 1.18); with an LDL cholesterol of 2.02 mmol/l (+/− 0.93 mmol/l). The average ACR (albumin creatinine ratio) was 75.4 mg/mmol, though there was a wide variation of this measurement with a standard deviation of +/− 166 mg/mmol. Similarly, there was a variation in serum creatinine levels in this population, with a mean serum creatinine of 119.6 μmol/l (+/− 79.2 μmol/l).
At 5-year follow-up, the rate of complete recovery from a DFU was 24.5%, while the rate of ulcer recurrence was 33.7%. The proportion of patients who had undergone amputation at 5 years was 28.6%, with a 5-year mortality rate of 13.3% (Table 1).
Odds ratios (OR) were calculated to assess whether type of diabetes, elevated HbA1c, presence of CVD or renal impairment was associated with an increased risk of ulcer recurrence, amputation or mortality at 5 years. In this study, these variables were not associated with an increased risk of poorer outcomes at 5 years (Table 2).
Discussion
This is the first study to assess the outcomes in patients attending a dedicated multi-disciplinary diabetic foot clinic in an Irish population. Such studies have been carried out elsewhere. In a 5-year follow-up study of patients with previous DFUs who attended a foot clinic in Sweden, the rate of ulcer recurrence was 34% at 1 year and 61% at 3 years, with a higher rate of recurrence associated with previous amputations [12]. The rate of amputation in previously healed ulcers was 12% after 5 years, with a higher rate of amputation in patients who had had an amputation for the initial ulcer (48% after 5 years). Similarly, the survival rate at 5 years was lower (27%) in the group that had had amputations at the outset compared to 58% survival at 5 years in the healed-ulcer group [12]. A more recent study on 5-year outcomes in patients with DFUs attending a diabetic foot clinic in Liverpool reported amputation rates for people with DFUs after 5 years varying from 11% (neuropathic ulcers) to 29% (ischaemic ulcers), while reported mortality rates for patients with DFUs after 5 years ranged from 45% (neuropathic ulcers) to 55% (ischaemic ulcers) [13]. A 10-year follow-up population study in Norway reported a mortality rate of 49% in patients with diabetes and a history of a foot ulcer, compared to a mortality rate of only 35% in patients with diabetes and no foot ulcer history [14]. The excess mortality was only partly explained by the increased incidence of older age, male sex, higher A1C, current smoking, insulin use, microalbuminuria, cardiovascular disease and depression in those patients with foot ulcers [14].
Our retrospective review reports better overall outcomes for patients with DFUs attending a specialist foot clinic when compared to the studies cited above. While our study found a similar rate of amputation at 5 years (28.6%), the mortality rate at 5 years was lower (13.3%). There are a number of possible explanations for the improved survival rates of our cohort compared to those reported previously. The study by Apelqvist et al., was conducted in the 1980s prior to the publication of the landmark trials in diabetes which altered glycaemic targets for patients, in order to reduce micro- and macro-vascular complications [12]. Diabetes treatments have also significantly evolved over the past 20 years with an explosion of new classes of oral and injectable anti-hyperglycaemic agents, as well as significant advances in diabetes technology, which have led to improved outcomes for patients. The study by Iverson et al., was conducted more recently but the excess mortality reported by this group (49%) may partly be explained by the poorer glycaemic control in these patients (HbA1c 8.4% vs 7.53%) or the longer duration of follow-up (10 years vs 5 years) [14]. Furthermore, management of DFUs has improved over the timescale with the development of increasingly sophisticated visualisation techniques, debridement methods and wound care protocols. Indeed, we acknowledge the limitation invoked by the small sample size of this study, and the difficulties therein, with making comparisons to much larger studies, such that apparent differences between the studies may not be statistically significant. However, our reported mortality rates are similar to those observed in a large Scottish study published in 2018 [15]. Vadivelo et al., investigated amputation-free survival in over 17,000 patients with diabetes and high-risk feet [15]. In this study, 14% of their cohort had died over the 2-year follow-up period and interestingly, the risk of death was nine times the risk of amputation [15].
Moulik et al., reported increasing age as the only independent factor that affected survival time, while generally reporting ischaemic ulcers secondary to peripheral vascular disease to be associated with an overall shorter survival time compared to neuropathic ulcers [13]. Our study did not differentiate DFUs according to aetiology, and we did not identify a clinical parameter which further increased the risk of mortality in patients with DFUs. In this study, an elevated HbA1c was not associated with an increased risk of adverse outcomes. This result is at variance with previous studies which have demonstrated that poor glycaemic control is a predictor of DFU recurrence [16]. It is worth noting that the HbA1c utilised in our analysis was the first HbA1c measured following attendance at the foot clinic and not the patients’ average HbA1c over the study period. Hence, it is not a true reflection of the patients overall glycaemic control as this may well have varied considerably over the 5 years and this may explain why an association between glycaemic indices and poorer outcomes was not observed in our study.
Although there is a body of evidence to suggest that co-existent CVD and renal failure predict poor outcomes in patients with diabetes, in this cohort, these comorbidities were not associated with an increased risk of mortality, recurrent ulcers or amputations [17, 18]. This conflicting result is likely due to the retrospective design of the study, which by its very nature, is subject to variability and inconsistency in the accurate recording of diagnoses in an electronic patient record. In addition, it is possible that outcome data was not captured for some of the patients and this is the main limitation of the study. Another limitation of this study was the lack of certain data available for some of the patients. Whilst missing data was omitted, the cases were still included in the analysis as the sample size was small but this statistical strategy may have confounded the results.
In conclusion, this study has shown that the outcomes for patients attending a diabetic foot clinic remain suboptimal. Patients with DFUs are at high risk of recurrence and continue to show increased mortality compared to the normal population. Management of DFD is costly; in the USA, it is estimated that the cost of inpatient admissions for DFUs was $1.38 billion per year [19], whilst in the UK, NICE estimated that £650 million is spent on foot ulcers and amputations per year [20]. Therefore, further investment in specialist foot clinics and more intensive follow-up in the community and the hospital are required to achieve improved ulcer healing rates. This would be cost effective given the financial burden of diabetic foot disease.
Although the mortality rate in this cohort was lower than that reported in other studies, it still remains high at a rate of approximately 1 in 5 patients at 5 years. Whilst optimum management of all diabetes complications is key to improving survival outcomes, it is hoped that the implementation of the National Model of Care for the Diabetic Foot in Ireland will improve the rate of healing and lower the rate of amputation and disability in patients with diabetic foot disease. However, an Irish national diabetes foot care audit is now warranted, to examine our current clinical outcomes and to identify areas for further improvements.
References
Hurley L, Kelly L, Garrow AP, Glynn LG, McIntosh C, Alvarez-Iglesias A, Avalos G, Dinneen SF (2013) A prospective study of risk factors for foot ulceration: the West of Ireland Diabetes Foot Study. QJM 106(12):1103–1110
Health Service Executive (2011) Model of care for the diabetic foot. National Diabetes Programme Working Group. Dublin: HSE
Boyko E, Ahroni J, Smith D, Davignon D (1996) Increased mortality associated with diabetic foot ulcer. Diabet Med 13:967–972
Ramsey S, Newton K, Blough D, McCulloch D, Sandhu N, Reiber G, Wagner D (1999) Incidence, outcomes and cost of foot ulcers in patients with diabetes. Diabetes Care 22:382–387
Nelzén O, Bergqvist D, Lindhagen A (1997) Long-term prognosis for patients with chronic leg ulcers: a prospective cohort study. Eur J Vasc Endovasc Surg 13:500–508
Buckley CM, O’Farrell A, Canavan RJ, Lynch AD, Davida V, Bradley CP, Perry IJ (2012) Trends in the incidence of lower extremity amputations in people with and without diabetes over a five-year period in the Republic of Ireland. PLoS One 7(7):e41492
Larsson J, Apelqvist J, Adardh CD, Strenstrom A (1995) Decreasing incidence of major amputation in diabetic patients: a consequence of a multidisciplinary foot care team approach? Diabet Med 12:770–776
Armstrong D, Harkless B (1998) Outcomes of preventative care in a diabetic foot specialty clinic. J Foot Ankle Surg 37:460–466
Aydin K, Isildak M, Karakaya J, Gurlek A (2010) Change in amputation predictors in diabetic foot disease: effect of multidisciplinary approach. Endocrine 38:87–92
Dargis V, Pantelejeva O, Jonushaite A, Vileikyte L, Boulton A (1999) Benefits of a multidisciplinary approach in the management of recurrent diabetic foot ulceration in Lithuania: a prospective study. Diabetes Care 22:1428–1431
Apelquist J, Larsson J, Agardh C (1993) Long-term prognosis for diabetic patients with foot ulcers. J Intern Med 233:485–491
Moulik P, Mtonga R, Gill G (2003) Amputation and mortality in new-onset diabetic foot ulcers stratified by etiology. Diabetes Care 26:491–494
Iversen M, Tell G, Riise T, Hanestad B, Ostbye T, Graue M, Midthjell K (2009) History of foot ulcer increases mortality among individuals with diabetes. Diabetes Care 32:2193–2199
Vadiveloo T, Jeffcoate W, Donnan PT, Colhoun HC, McGurnaghan S, Wild S, McCrimmon R, Leese GP, and Scottish Diabetes Research Network Epidemiology Group (2018) Amputation-free survival in 17,353 people at high risk for foot ulceration in diabetes: a national observational study. Diabetologia 61(12):2590–2597
Dubský M, Jirkovská A, Bem R, Fejfarová V, Skibová J, Schaper NC, Lipsky BA (2013) Risk factors for recurrence of diabetic foot ulcers: prospective follow-up analysis in the Eurodiale subgroup. Int Wound J 10:555–561
Crawford F, Inkster M, Kleijnen J, Fahey T (2007) Predicting foot ulcers in patients with diabetes: a systematic review and meta-analysis. J Assoc Physicians 100(2):65–86
Margolis DJ, Hofstad O, Feldman HI (2008) Association between renal failure and foot ulcer or lower-extremity amputation in patients with diabetes. Diabetes Care 31(7):1331–1336
Hicks C, Selvarajah S, Mathioudakis N, Sherman R, Hines K, Black H, Abularrage C (2016) Burden of infected diabetic foot ulcers on hospital admissions and costs. Ann Vasc Surg 33:149–158
NICE Guidelines: diabetic foot problems: prevention and management; 2015.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
No ethical approval was deemed necessary, as the study involved auditing the treatment of patients as per routine best practice standard of care. No additional interventions were performed in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
H. Forde and S. Wrigley are co-first authors.
Rights and permissions
About this article
Cite this article
Forde, H., Wrigley, S., O’Murchadha, L. et al. Five-year outcomes of patients attending a diabetic foot clinic in a tertiary referral centre. Ir J Med Sci 189, 511–515 (2020). https://doi.org/10.1007/s11845-019-02108-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-019-02108-2