Abstract
Introduction
A growing body of evidence indicates the benefits of early diagnosis of rheumatoid arthritis (RA) and prompt treatment with disease-modifying anti-rheumatic drugs (DMARDS) in terms of relieving symptoms, improving prognosis, and reducing long-term complications. There is however some controversy over the most beneficial method of imaging in providing accurate early diagnosis. Though current practice favours clinical and radiological assessment, this is increasingly supplemented by ultrasound techniques (and, to a lesser extent, CT and MRI scanning). While EULAR and ESSR favour the use of ultrasonography (US) as the first-line investigation in cases of suspected RA, a recent NICE review upholds the traditional place of plain film radiographs of hands and feet to detect erosions as early signs of synovitis. This review considers the evidence for US in the early diagnosis of RA and the case for it becoming the primary assessment modality in rheumatology clinics.
Aims
This paper aims to assess the current literature on the efficacy of ultrasonography in diagnosing early RA, by comparing US with alternative imaging modalities. The goal is to propose the most appropriate method of diagnosis to improve early initiation of DMARD treatment for optimum disease outcomes.
Methods
Searches for related studies and review articles were carried out using electronic databases and hand searches. Additional references were gleaned from the bibliographies of included papers. Related articles and pop-outs from PubMed were also used. The search was refined in PubMed, by only using reviews which were written in English and published in past 10 years and had full free text available.
Results
This review confirms that US has a high level of sensitivity in diagnosing RA (and hence a low risk of missing cases of RA which might benefit from early treatment with DMARDs). It also has a high level of specificity (and hence a low risk of falsely diagnosing somebody with RA who may suffer adverse effects of DMARD therapy). US is already widely available and well accepted by clinicians and patients. It does not involve exposure to radiation and can be readily delivered by appropriately trained staff.
Conclusion
This review of relevant studies indicates that US should become accepted as the investigation with the most favourable balance of benefits to risks in the early diagnosis of RA. Given the continuing controversy surrounding studies of different imaging techniques in RA, further research into the diagnostic role of US in RA is indicated.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
‘detecting subclinical arthritis ……. will ultimately improve the quality of life of patients suffering from rheumatoid arthritis’
Introduction
This review focuses on recent literature regarding role of modern imaging in the diagnosis of rheumatoid arthritis. Early detection is essential in rheumatoid synovitis to avoid disease progression [4, 19, 48].
In 2012, the ESSR (European Society for Musculoskeletal Radiology) considered ultrasound the leading method in peripheral synovitis imaging, irrespective of the disease entity. A growing body of literature demonstrates increasing use of US in rheumatological clinical practice and links US to the diagnostic and therapeutic decision-making process of RA [13]. Some clinicians and researchers claim superiority of US when compared with physical examination, plain radiography, and MRI in rheumatic diseases [30]. Despite the available evidence and the diagnostic potential of US findings, many rheumatologists do not utilise this modality to influence their clinical decision-making.
Zhang [86] argues that detecting subclinical arthritis, to assist in improving medical treatment and successfully halt bone erosion, will ultimately improve the quality of life of patients suffering from RA.
Rheumatoid arthritis
RA is a systemic inflammatory polyarthropathy, characterised by chronic inflammation in the synovium, cartilage degradation, and juxta-articular bone erosions [43, 57]. The debilitating disease affects 1% of the population worldwide [27]. Symptoms include pain, stiffness, swelling, and decreased range of motion [11]. RA is also associated with immune cell activation [85] and non-articular complications such as osteoporosis, accelerated atherosclerosis, and increase risk of malignancy and heart disease [9]. The classification criteria of RA are outlined by the American College of Rheumatology (ACR) and European League Against Rheumatoid Arthritis (EULAR).
In Ireland, general practitioners can refer patients to fast access rheumatology clinics if the small joints of the hands or feet are affected symmetrically or other relevant criteria are met. The key stage in the diagnostic process occurs when the patient attends a specialist rheumatology clinic. Traditionally, X-ray of the hands and feet, to identity bony erosions, was the modality of choice to assess severity of inflammation. Presently, US is increasingly utilised, together with clinical assessment and inflammatory biomarkers, due to its improved diagnostic accuracy and assessment of RA.
Ultrasonography as a diagnostic tool for early rheumatoid arthritis
EULAR 2013 recommendations state that diagnostic certainty in RA is improved by imaging in comparison with clinical examination, in addition to accurate assessment of joint inflammation, joint erosion, prediction of treatment response, and disease activity monitoring [10].
The Swiss Sonography in Arthritis and Rheumatism (SONAR) group believe there is rationale for including US assessment for patients with RA in the daily clinical practice of rheumatologists [88] and have developed the SONAR scoring system.
In the initial stages of rheumatoid synovitis, plain film radiographs may not detect preliminary synovial changes, and patients may only experience non-specific musculoskeletal symptoms [87]. Ultrasonography allows direct visualisation of joint structures, with high sensitivity in detecting pathology, lending it a suitable modality for evaluating RA. The ESSR Arthritis Subcommittee recommend a 4-grade scoring system [53, 74] which has proven high reproducibility among rheumatologists and radiologists [62].
For decades, plain film radiograph has been the diagnostic modality of choice in rheumatology. However, in recent years, US is increasingly selected as diagnostic rheumatoid imaging, revealing subclinical inflammation and predicting progression of joint damage [22].
From their findings of US procedures, Zhang and colleagues claim that US is easy to use and interpret, efficient, economical, and reliable for diagnosis of early synovitis [58, 87]. US can directly visualise the inflamed synovium and synovial sheath, including damaged joints and tendons affected by RA [77]. Gutierrez [28] believes that acquiring US skills for specified targets such as spotting bone erosion is simple, using scanning protocols.
Technique
Ultrasound is best suited to assess many different joints for inflammation, relatively quickly [81]. Naredo found that for routine diagnostic and treatment response purposes, 12-joint power Doppler US (PDUS) assessment of synovitis is valid, reliable, sensitive to change, and feasible for therapy monitoring in RA [50]. They argued it is sufficient to assess the anterior and posterior recess of the elbow, the dorsal carpal recess of the wrist, the second and third MCPJ dorsally and palmar, the suprapatellar recess and the lateral parapatellar recess of the knee, the anterior tibiotalar recess of the ankle, and the medial and lateral tendon sheaths in the ankle area. Spencer recommended more concentration on the wrist and MCPJs for examination [72], while Filer found that scanning MCPs, wrist and MTP joints were most likely to demonstrate specificity for RA [20].
Grey-scale ultrasound
Grey-scale ultrasound (GSUS) provides clear grey-scale images of the musculoskeletal system. Zhang et al. [87] reported grey-scale US is precise, valid, inexpensive, and a readily available method for diagnosis of early rheumatoid synovitis of the wrist and finger joints, as supported by the findings in their cross-sectional study. This study showed that GSUS was more effective at detecting early synovitis compared with clinical laboratory investigations (p = 0.00015) than plain film radiographs (p = 0.0002). While plain film radiography of patients provided precise information of joint erosions, less information was revealed for synovitis. GSUS was more effective at detecting early rheumatoid synovitis and quantified the synovial changes, when compared with X-ray and clinical investigations. GSUS is helpful to differentiate synovial hypertrophy and tendon pathologies, in addition to bony erosions and joint space narrowing.
Power Doppler ultrasound
PDUS uses the change in the frequency of a sound wave by the movement of its source or receiver. PDUS and colour Doppler are valid techniques to illustrate the level of vascularisation, to accurately assess inflammation and monitor treatment response in joints and soft tissues. PDUS provides clear visible evidence of acute inflammation. Iagnocco et al. [29] argue that US is a reliable and sensitive method for continuous monitoring of disease activity in RA. PDUS can be used to measure blood flow through small vessels to evaluate the extent of inflammation [8, 77]. Naredo et al. [50] claim that PDUS is a relatively low cost, non-invasive, bedside imaging technique that facilitates the visualisation of all peripheral joints at the real-time of consultation, numerous times as required.
Filer et al. claimed that PDUS had a uniquely high specificity and sensitivity for RA [20]. PDUS provides info on synovial and tendon sheath vascularity [3]. PDUS correlates with vascular endothelial growth factor (VEGF), providing evidence of a central role for VEGF in synovial neo-angiogenesis [38]. This study evaluated GSUS and PDUS in asymptomatic synovial joints of patients, comprising relevant joints in a RA assessment. A positive correlation between PDUS and serum cytokines involved in synovial inflammation pathogenesis was reported, proving serum VEGF levels are a potential biomarker for synovial vascularity. Ji et al. [31] concluded that PDUS could independently assist the 2010 ACR/EULAR classification criteria in the early diagnosis of RA in those patients who are negative for anti-CCP antibody.
Methods
Inclusion criteria
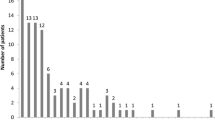
The structured systematic literature search for related studies was carried out using electronic databases—PubMed, Elsevier, Cochrane library, Wiley online library, and Science Direct using MeSH. Searches included specific syntax such as (Rheumatology OR Rheumatic Disease OR Rheumatoid Arthritis OR Arthropathies OR Inflammatory Arthritis OR Rheuma*) AND (Imaging OR Image OR Images OR Radiology OR Radiological OR Ultrasonography OR Ultrasound OR US OR Ultraso*). Additional references were gleaned from the bibliographies and references of included papers. Related articles and pop-outs appearing in PubMed were also used. All journals had a high impact factor and cited numerous times previously. A total of 88 papers are included in this review, including 20 clinical trials and over 60 reviews, research papers, guidelines, recommendations, and 1 meta-analysis.
Other electronic resources included Glucksman Library E-resources, JSTOR, Thieme, and internet sites including Radiopaedia.org, Rheumatology.org, NICE.org.uk, and arthritisireland.ie. Printed sources included Journal of Rheumatology, European Journal of Rheumatology, Radiology, and Clinical Radiology. Grey literature included ResearchGate, British Society for Rheumatology, and Arthritis Research and Therapy. The search was not limited in Cochrane or Science Direct. Additional articles were found in the British Medical Journal, the Irish Medical Journal, ResearchGate, JSTOR, Thieme and reports from the Annals of Rheumatic Diseases, and EULAR. The abstracts of each peer-reviewed paper were evaluated to determine if they addressed ultrasonography, diagnosis, or detection of early rheumatoid arthritis. Clinical trials included in this review will be presented in a chronological order. Conclusions drawn from these studies and reviews are compared to determine an appropriate imaging modality for the early diagnosis of RA.
Exclusion criteria
Search terms yielded numerous results, and many were rejected due to irrelevance or non-specific to early rheumatoid arthritis diagnosis and ultrasonography. Any related conditions including juvenile arthritis, gout, SLE, osteoarthritis, polymyalgia rheumatica, and spondyloarthritis were excluded. The search was refined in PubMed by only using reviews which were written in English and published in past 10 years, solely human studies, and had full free text available. Searches for keywords were limited to the title/abstract to maximise relevant data.
Results
Earlier diagnosis and initiation of DMARDS
NICE guidelines recommend early detection of persistent synovitis and prompt commencement of DMARDS. Earlier detection of joint damage and earlier diagnosis of rheumatoid arthritis is now possible, through imaging modalities such as ultrasound and MRI, allowing repair and halting disease progression by novel therapeutic agents. The accessibility of biologics and DMARDS has prompted earlier initiation of therapy, enabling control of RA and joint preservation [81].
Kelly et al. [37] found that routine US in newly referred patients was associated with significantly earlier diagnosis and initiation of DMARD treatment. Ninety-two percent of their patients later clinically diagnosed with RA fulfilled the ACR/EULAR 2010 criteria at 12 months. A window of opportunity for remission occurs in the earliest stages of RA [82]. It is argued that US improves diagnostic certainty in new patients presenting with seronegative early arthritis [24, 31, 44]. This differs to the Pratt et al., (2013) study; they found that US as routine assessment in an early arthritis clinic did not add substantial discriminatory value for predicting RA.
Evaluation of RA and quickly starting DMARD therapy has advantageous long-term clinical outcomes and socioeconomic benefits. Disease progression can be halted, with improved long-term functional and radiological outcomes. In addition to reduced clinical signs and symptoms of RA, early diagnosis improves long-term outcomes such as pain, structural damage, and disability [54].
Sensitivity and specificity
Studies that compare US and clinical examination have established a higher sensitivity and specificity of RA diagnosis using US [63]. Nakagomi [47] found that US assessment was more sensitive for detecting synovitis than clinical joint examination, (78% sensitivity for GSUS detected synovitis vs 58.5% sensitivity for clinically detected synovitis) thereby minimizing false-negative results and reducing missed diagnosis and loss of benefit of early DMARD treatment. Their study of 41 patients also provided a very specific assessment of synovitis (93.7% specificity for PDUS assessment vs 79.4% specificity for clinically detected synovitis), which is important to eliminate the risk of initiating DMARD therapy, with considerable adverse effects on patients who do not have RA. The NICE report quotes a requirement of sensitivity of > 90% for determining the diagnostic accuracy of US in addition to clinical assessment in diagnosing RA [52] (Table 1).
Main findings of ultrasound in rheumatoid arthritis
The working group in ultrasonography, OMERACTFootnote 1, developed outcome measures in rheumatology, including detectable pathologies for synovial hypertrophy, effusion, rheumatoid erosion, enthesopathy, and tenosynovitis [84].
Synovial pathology determined by US correlates with arthroscopic and MRI synovial hypertrophy. Doppler signal correlates with vascularity and histological features of inflammation in biopsies. Keen et al. [36] discovered that US is reliable in detecting synovitis, effusions, tension lesions, tenosynovitis, and erosions. US can predict patients likely to develop radiographic progression, patients most likely to respond to therapy and patients with low levels of disease activity, likely to flare [36].
Bone erosions
Synovitis
Angiogenesis
Adipose tissue
Metacarpal cartilage thickness [3]
Bone erosions
A large percentage of patients with RA present with bone erosions. High-frequency transducers detect minute erosions, as revealed by micro-CT analysis [23]. Bone erosions signify joint involvement in RA, and its detection reveals diagnosis, persistence, and severity of disease [39, 57]. In their study, Tamas et al. [76] found a high percentage of patients with RA in the early stage of disease with bone erosions, most frequently located in the fifth metatarsal head, and lateral aspects.
Funck-Brentano et al. [25] claimed that US erosions and PDUS synovitis have prognostic value to predict future radiographic damage and evaluate the potential severity of early arthritis. According to Gutierrez, the ulnar and fifth metatarsal heads are highly reproducible and frequently involve bone erosion in RA, whereas erosions at the volar aspects are less reliable due to technical, anatomical, and pathological issues [28]. Bone erosions are the hallmark of joint damage in RA. The detection of erosive bone damage and increase in quantity or extent indicates poor consequences [70]. Sheane et al. [71] identified that targeted US is a quick and convenient tool in detecting erosions in early RA, providing a better indication of disease severity and prognosis, compared with laboratory tests, in the absence of definite diagnosis.
Numerous studies have demonstrated that US is more sensitive than conventional radiography in the detection of joint damage. US may provide less detail in comparison with MRI; however, it demonstrates articular and peri-articular pathology, assisting treatment provision [34]. US assessment of all affected joints could prove to be quite time-consuming in the clinic; therefore, specific joints most likely to yield diagnosis, such as the 5th MTP, could benefit early therapeutic decision-making [71, 75].
Koevoets et al. [39] demonstrated that bone erosions, more than joint space narrowing in the wrist, are associated with impaired physical functioning in patients with early RA with limited overall damage.
Synovitis
Numerous studies have recognised the association between subclinical synovitis and radiographic progression of joint degradation [22]. Kane et al. [32] claimed that high-resolution US is superior to clinical assessment in detecting and localizing joint and bursal effusion and synovitis, spotting minute amount of fluids in joints of asymptomatic patients. Filer et al. [20] established a diagnostic benefit of the increased sensitivity of US in an early synovitis population. In their longitudinal study, US joint evaluation significantly increased detection of joint involvement, providing minimal US findings to improve clinical outcomes for RA.
Najm et al. [46] found US in large joints, including the knee, a reliable tool. A positive correlation was realised between the PDUS grade of synovitis, histological inflammation score, and vascularisation score in actively inflamed knee joints (r = 0.63; p = 0.02). They demonstrated that US examination with both B-mode and power Doppler reflects accurately histological inflammation and vascularisation. They argued that US findings are a useful biomarker for disease activity when compared with synovial histology.
Sahbudin et al. [68] concluded that US of digit flexor tenosynovitis provides independent predictive data for persistent RA development in patients with early arthritis. Filer et al. [20] reported that digit flexor tenosynovitis, determined by MRI (with gadolinium), predicts RA independently; however, US is perceived as a more accessible clinical imaging tool than MRI. They maintained synovitis demarcated by US improves outcomes in RA is superior than serological and clinical variables in early arthritis.
Angiogenesis
Increased synovial vascularity in cartilage, due to angiogenesis, is observed by PDUS and colour Doppler. Blood vessels are not present in healthy cartilage [57]. Despite clinical remission, subclinical inflammatory activity persists in sheaths or joint cavities, causing disease to progress. Increased blood flow in the synovium, detected by PDUS, is a notable risk factor [63].
Adipose tissue
Extra or intra-articular adipose tissue is associated with cartilage and bone erosion [73]. Adipose tissue is infiltrated by inflammatory cells, adipokines, and may be associated with all connective tissue components. Abnormal fat tissue echogenicity is visible in US [57].
Cartilage thickness
Directly measuring cartilage thickness on US in MCPJs and PIPJs is correlated with joint space narrowing in X-ray findings [45]. In their study, Filippucci et al. [21] demonstrated moderate to good interobserver reproducibility of a cartilage damage scoring system, based on morphological changes at MCP joints of patients with RA.
Discussions
Ultrasonography
Ultrasonography (US) uses the physics of sound waves, by converting electrical energy to high-frequency sound via a transducer containing piezoelectrical elements. The transducer directs the sound waves through matter towards the anatomy in question. The waves are affected by both tissue density and frequency of sound waves [36]. The US probe has been likened to the rheumatologist’s stethoscope [8]. US in RA can be used to assess structural damage assessment, monitor RA disease activity, and remission [3]. US bears the ability to differentiate between arthralgia and arthritis, to display erosions in early RA which cannot be viewed on X-ray, to scan tendons in enthesopathies, and to image blood vessels [7]. US permits early detection and detailed characterisation of bone erosion, playing a significant role in diagnostic procedures [70].
Advantages of ultrasound for diagnosis of early RA
US presents numerous advantages over other imaging techniques including the following:
Lack of radiation
Relatively inexpensive
Non-invasive
Acceptable mode of imaging by patients
Allows assessment of multiple regions easily and readily [8]
Alter specific sites, allowing dynamic scans and comparison of bilateral sides
Valid, reproducible, responsive
Given its validity, reproducibility, and responsiveness, US seems a particularly appropriate imaging modality in the early diagnosis RA. It is much more sensitive than clinical examination for detection of inflammation, optimising diagnosis, directing therapy through accurate assessment of disease activity, and understanding the optimal selection of joints for feasible disease monitoring [36]. Due to the excellent soft tissue contrast, US can depict RA at a very early stage.
In patients with RA, US is painless, enables multijoint scanning, offering contralateral and additional anatomic locations, and allows dynamic images immediately and spontaneously [30]. Naredo and others reported US as a useful tool when available as a service in rheumatology clinic [1, 49].
US has demonstrated its success over conventional clinical and serological assessment when evaluating patients with early inflammatory joint disease symptoms. Technological advances in US in recent years have led to advances in the imaging quality of GSUS and the development of progressive forms, including 3D and Doppler US. These enhancements have improved the validity of US diagnosis, as well as the monitoring of pathology and disease progression. They have also facilitated interventional therapies in rheumatic diseases [18]. PDUS improves the sensitivity and specificity of RA diagnosis, as has been recognised by 2010 ACR/EULAR classification criteria [24].
Kawashiri et al. [35] have shown that US can play a central role in the early diagnosis of RA according to the 2010 classification criteria. US is an easily accessible modality for assessing small joints of the hands for bone erosion, joint effusion, synovial proliferation, and synovitis. Bursae, larger joints, and entheses can be readily examined. US is associated with more rapid diagnosis of synovitis and earlier initiation of DMARDS, and its importance has been recognised by NICE, the UK’s National Audit office and Dept. of Health [37].
Disadvantages of ultrasonography for diagnosis or early RA
-
Operator dependent
-
Variances in interpretation of results
-
Significant learning process and period of training
-
Scanning times vary—lack of consensus regarding number of joints to be scanned
As US is the most operator-dependent imaging modality, there may be variances in the interpretation of results by individual operators. US has advanced significantly in terms of probes, scanning techniques, and machines. Differences in US positioning can influence findings, and this obviously affects findings in the research and clinical setting. Scanning times can vary and have ranged from 5 to 15 min depending on joints involved in the research setting [16].
There is a significant learning process to master the skills of US, and a substantial period of training before reaching competency [70]. US is carried out in the clinic, and while US equipment is relatively cheap, Durcan et al. [16] claimed that time and training costs can be considerable.
Some studies have questioned the superiority of US. Dale and colleagues in a RCT published in 2016 investigated whether US assessment could improve an intensive early treatment strategy in patients with RA [12]. They found that, while regular assessment of RA disease activity involved a greater intensity of DMARD therapy, the study demonstrated that this was not associated with superior clinical, functional, health-related quality of life or imaging outcomes. This review, contradicting the growing consensus in favour of wider use of US, confirms the need for further studies in this area.
Other authorities have pointed to the lack of consensus regarding the optimal number of joints that should be routinely assessed using US [37]. Meanwhile, OMERACT has published definitions of common pathological lesions in RA, which have been widely accepted, including bone erosion, synovitis, and synovial hypertrophy [84].
US vs conventional radiography
In Ireland, US is a less accessible modality than plain film radiographs. However, studies show that US is superior to X-ray as it facilitates earlier diagnosis and therefore earlier intervention. With the correct technique and focused assessment, US is feasible in clinical practice, with few contraindications.
X-ray images are two-dimensional representations of three-dimensional pathologies; superimposition of normal and abnormal features reduces the diagnostic integrity [55, 59]. X-ray continues to be a common investigative tool due its availability, universal acceptability (despite the risk of background radiation exposure), cost, performance speed, and diagnostic yield [16]. Plain film radiograph is continually utilised for detecting and scoring erosive damage in routine clinical practice, despite its low sensitivity, in comparison with CT, MRI, and US [70]. Pearman et al. [59] advocate for the importance of utilising well-established, routinely practiced conventional radiography and have demonstrated a novel radiographic position for visualizing bones and joint spaces of hands and wrists, with the aim to improve the ability of radiologists and rheumatologists to identify bony lesions. The primary radiographic features for assessment of RA are bony erosions and joint space narrowing [39].
X-rays include a record of cumulative joint damage triggered by rheumatic disease [10]. While X-ray can detect bone erosions, juxta-articular osteoporosis, joint space narrowing, and new bone formation, it cannot portray inflammatory changes [54]. The key limitation of X-ray is its lack of sensitivity in detecting structural changes in joints of patients with early RA assessment [77]. Wakefield, using US, detected up to seven times more erosions than plain radiography in early RA [83].
US vs computerised tomography
In detecting bone erosions, CT is superior to MRI and US [61]; however, it is limited due to the high radiation doses imparted to the patient [40] (Table 2). There is minimal use of peripheral CT in clinical practice due to its inability to visualise soft tissue changes. CT visualises calcified tissue with high resolution. It is seldom used, unless radiography is unclear and MRI unavailable [54]. CT allows visualisation of osteoporosis and new bone formation, in the form of syndesmophytes ligamentous ossification using multiplanar imaging without superimposition of overlying structures [54]. Its usefulness lies in its ability to depict and delineate new bone formation and erosions in rheumatic disease [14, 15].
US vs magnetic resonance imaging
MRI uses multiplanar tomographic imaging with soft tissue contrast, providing a means to assess all associated structures in RA. MRI can directly and sensitively visualise synovitis (via effusion), synovial hypertrophy, tenosynovitis, tendon rupture, cartilage thickness, periarticular inflammation, bone oedema, bone erosion, and bone proliferation [56]. Synovitis is often present in clinically inactive joints; hence, the presence of subclinical disease activity can be determined using highly sensitive MRI [26]. Bone oedema, a sign of histologic osteitis, is exclusively visualised by MRI and is a strong predictor of structural damage progression [6]. Ionizing radiation is not used and captured images can be filed and analysed centrally [78].
US cannot image bone marrow, to eliminate other pathologies. In suspected cases of bone marrow oedema due to injury or osteoporosis, MRI is modality of choice [5, 6]. In their study of an early RA cohort, Navalho et al. [51] found MRI to have a significantly higher diagnostic capability. Synovitis in flexor tendons and carpal joints revealed by MRI was more powerful than US in predicting progression toward RA.
Ostergaard [54] considered MRI to be the optimum method for detecting inflammation in the spine and sacroiliac joints in early spondylarthritis, but not in RA. In comparison with US, MRI bears higher operation costs. The excessively high costs of MRI and restricted access have contributed to increase in US imaging [66]. Technically, interpreting MRI can be problematic, as similar lesions to bone erosions can be detected in healthy individuals [42]. MRI also carries risk of claustrophobia, and contraindications in metal implantations and in renal failure due to potential exposure to gadolinium-containing contrast agents [78].
In their meta-analysis for the detection of bone erosions, Baillet et al. [2] derived there was no statistically significant difference between MRI and US.Footnote 2
However, in detecting the presence of inflammation in soft tissue, synovitis or tenosynovitis when clinical examination is inconclusive, PDUS is superior to MRI, as it can sense increased blood flow [40, 64].
EULAR and role of imaging
Following the development of DMARDS, the ACR/EULAR revised the diagnostic criteria for RA, assessing joint involvement, blood parameters, and symptom duration. However, imaging was not integrated as part of the primary assessment. Imaging is indicated whereby initial tests deem inconclusive and fail to fulfill the diagnostic criteria [81]. Nineteen experts appointed by EULAR prepared recommendations regarding imaging in RA, to improve diagnosis in patients showing signs of inflammation, detect structural erosions, and forecast the disease course and treatment response.
NICE guidelines
Evidence review A: ultrasound for diagnosis [52]
In July 2018, NICE published guidelines on the role of US in the diagnosis and management of RA [52]. This review concluded that ‘No evidence was identified for any of the clinical effectiveness outcomes’, of using US as a diagnostic tool for RA. In the view of the NICE committee, the evidence for the diagnostic accuracy of US was inconsistent within studies, dependent on how ultrasound was integrated into the diagnostic process.Footnote 3 In contrast to this literature review, which looked at 20 RCTs, only 4 studies satisfied their highly rigorous inclusion criteria. Overall, NICE considered that the limited evidence from their studies was of insufficient qualityFootnote 4 to support any recommendation regarding the use of US in diagnosis of RA. NICE excluded 43 studies in their report.
However, NICE have acknowledged that US may improve patient outcomes in the event the patient is reluctant to accept their diagnosis of RA and commence treatment. US here can enable clinicians to illustrate objective evidence of joint inflammation and thereby encourage commencement of therapy.
NICE also clarified that further research should help clarify the circumstances where US assessment may be clinically and cost effective in diagnosing RA. They have also agreed to develop recommendations to establish the value of US in diagnosing RA where there is uncertainty following clinical assessment, i.e. symptoms of RA without clinically definite synovitis (Table 3).
Conclusion
US has become an integral element of the diagnostic process in RA by identifying and assessing inflammatory changes in joint cavities, sheaths, and bursae. The ESSR considered US the modality of choice for imaging peripheral synovitis [63]. ACR/EULAR, in their RA classification criteria, emphasise the role of US in detection of articular inflammatory changes, which may be ambiguous in the clinical situation initially. These criteria can be applied when clinical synovitis, in the form of oedema and tenderness, is identified in at least one joint.
ACR/EULAR state that US can support diagnosis of arthritis, as well as detecting inflammatory activity in subclinical synovitis and predicting progression of inflammatory arthritis to erosional RA. US is more sensitive in detecting rheumatoid erosions than plain film radiographs. Wakefield et al. [83] established that US detects rheumatoid erosions up to seven times more often than X-ray. US is inexpensive, non-invasive, and can be used conveniently by the bedside, with results evaluated immediately. Both Karim et al. [33] and Agrawal et al. [1] support the use of US for diagnostic evaluation in routine clinical practice.
Despite recommendations from ESSR, EULAR, ACR, SONAR, and Baillet et al. in their systematic review and meta-analysis that US should be integrated into routine RA management, especially at disease onset, NICE have published their evidence-based guidelines stating the contrary. However, McAlindon and colleagues, in their evidence-based review of US for the ACR, found it reasonable to use US to assess inflammatory disease activity in undiagnosed patients with RA or other inflammatory arthritis, as US can detect erosions not evident on plain radiographs [41] (Evidence level B).
Recommendations
US allows for an accurate and non-invasive radiological assessment at multiple joints. To orientate US to a specific target or joint, knowledge of the most sites which frequently involve bone erosion is necessary. In agreement with Tamas et al. [76], a systematic approach, aimed at revealing site-specific bone erosion, is efficient and effective, saving time in the clinical setting.
Gutierrez found in their study that following a 4-week focused training programme, a rheumatologist, without prior experience in US, can detect and score bone erosions in joints of hands and feet in patients with RA [28]. Competency in utilising US for RA diagnosis is an important aspect of training. Higher levels of competence can result in better-quality care and lower cost utilisation.
As per Tins and Butler [81], by working closely together, radiologists and rheumatologists can fulfill their duty to utilise imaging modalities in a cost effective manner to provide diagnosis, prognosis, and continuous assessment with minimal risk and inconvenience to the patient.
Due to its relatively low cost and its inherent safe use, US has been widely adopted in rheumatology clinics for the diagnosis of RA. Assessing all these rival claims, as beneficial outcomes with US are frequently observed in everyday clinical practice, this imaging modality should continue to be used as part of the diagnostic process for RA.
Considering the recent NICE guidelines, it is also evident that further research of the role of US in diagnosing RA should help clarify the circumstances where US assessment may be clinically and cost effective in diagnosing RA.
Notes
OMERACT, Outcome Measures in Rheumatology, is an international, informally organised network initiated in 1992 aimed at improving outcome measurement in rheumatology
MRI spotted more erosions than US in MCP (3+4), MTP (), and shoulder joints, whereas US distinguished more erosions in MCP 5, MTP (1+5), and PIP (). US was superior in early RA, while MRI was better in established RA.
The NICE committee found the studies to be highly diverse, with different populations, study designs and reporting data with some conflicting results. Where longer term follow-up (18 months) was not implemented, NICE committee deemed the study low quality and unreliable, regardless of sensitivity and specificity data of the study.
The major defect of the studies found was that patients had established synovitis in most of the RCTs; hence, the studies could not capture the potential benefit of initial US diagnosis before clinical assessment.
References
Agrawal S, Bhagat SS, Dasgupta B (2009) Improvement in diagnosis and management of musculoskeletal conditions with one-stop clinic-based ultrasonography. Mod Rheumatol 19(1):53–56
Baillet A, Gaujoux-Viala C, Mouterde G, Pham T, Tebib J, Saraux A, Fautrel B, Cantagrel A, Le Loet X, Gaudin P (2011) Comparison of the efficacy of sonography, magnetic resonance imaging and conventional radiography for the detection of bone erosions in rheumatoid arthritis patients: a systematic review and meta-analysis. Rheumatology (Oxford) 50(6):1137–1147
Baker JF, Tan YK, Conaghan PG (2015) Monitoring in established RA: role of imaging and soluble biomarkers. Best Pract Res Clin Rheumatol 29(4-5):566–579
Barhamain AS, Magliah RF, Shaheen MH, Munassar SF, Falemban AM, Alshareef MM, Almoallim HM (2017) The journey of rheumatoid arthritis patients: a review of reported lag times from the onset of symptoms. Open Access Rheumatol 9:139–150
Bloem JL, Reijnierse M, Huizinga TWJ, van der Helm-van Mil AHM (2018) MR signal intensity: staying on the bright side in MR image interpretation. RMD Open 4(1):e000728
Boyesen P, Haavardsholm EA, Ostergaard M, van der Heijde D, Sesseng S, Kvien TK (2011) MRI in early rheumatoid arthritis: synovitis and bone marrow oedema are independent predictors of subsequent radiographic progression. Ann Rheum Dis 70(3):428–433
Chaturvedi V (2014) Musculo-skeletal ultrasound in rheumatology practice. J Assoc Physicians India 62(10):36–40
Chen H-H (2017) The third eye of the rheumatologist: applications of musculoskeletal ultrasound in rheumatic diseases. Journal of Medical Ultrasound 25(1):4–8
Cojocaru M (2010) Extra-articular manifestations in rheumatoid arthritis’. Maedica (Buchar) (4):5, 286–291
Colebatch AN, Edwards CJ, Ostergaard M, van der Heijde D, Balint PV, D’Agostino MA, Forslind K, Grassi W, Haavardsholm EA, Haugeberg G, Jurik AG, Landewe RB, Naredo E, O’Connor PJ, Ostendorf B, Potocki K, Schmidt WA, Smolen JS, Sokolovic S, Watt I, Conaghan PG (2013) EULAR recommendations for the use of imaging of the joints in the clinical management of rheumatoid arthritis. Ann Rheum Dis 72(6):804–814
D’Agostino MA, Haavardsholm EA, van der Laken CJ (2016) Diagnosis and management of rheumatoid arthritis; What is the current role of established and new imaging techniques in clinical practice? Best Pract Res Clin Rheumatol 30(4):586–607
Dale J, Stirling A, Zhang R, Purves D, Foley J, Sambrook M, Conaghan PG, van der Heijde D, McConnachie A, McInnes IB, Porter D (2016) Targeting ultrasound remission in early rheumatoid arthritis: the results of the TaSER study, a randomised clinical trial. Ann Rheum Dis 75(6):1043–1050
de Miguel E, Andreu JL, Naredo E, Moller I (2014) Ultrasound in rheumatology: where are we and where are we going? Reumatol Clin 10(1):6–9
Dohn UM, Ejbjerg BJ, Court-Payen M, Hasselquist M, Narvestad E, Szkudlarek M, Moller JM, Thomsen HS, Ostergaard M (2006) Are bone erosions detected by magnetic resonance imaging and ultrasonography true erosions? A comparison with computed tomography in rheumatoid arthritis metacarpophalangeal joints. Arthritis Res Ther 8(4):R110
Dohn UM, Ejbjerg B, Boonen A, Hetland ML, Hansen MS, Knudsen LS, Hansen A, Madsen OR, Hasselquist M, Moller JM, Ostergaard M (2011) No overall progression and occasional repair of erosions despite persistent inflammation in adalimumab-treated rheumatoid arthritis patients: results from a longitudinal comparative MRI, ultrasonography, CT and radiography study. Ann Rheum Dis 70(2):252–258
Durcan L, Grainger R, Keen HI, Taylor WJ, Dalbeth N (2016) Imaging as a potential outcome measure in gout studies: a systematic literature review. Semin Arthritis Rheum 45(5):570–579
Ellegaard K, Christensen R, Torp-Pedersen S, Terslev L, Holm CC, Konig MJ, Jensen PS, Danneskiold-Samsoe B, Bliddal H (2011) Ultrasound Doppler measurements predict success of treatment with anti-TNF-α drug in patients with rheumatoid arthritis: a prospective cohort study. Rheumatology (Oxford) 50(3):506–512
Epis O, Giacomelli L, Bruschi E (2013) Imaging in rheumatology: ultrasafe + ultrasure = ultrasound. Rheumatol Int 33(7):1901–1903
Evans J, Negoescu A (2017) Early referral improves long-term outcomes in rheumatoid arthritis. Practitioner 261(1804):21–25
Filer A, de Pablo P, Allen G, Nightingale P, Jordan A, Jobanputra P, Bowman S, Buckley CD, Raza K (2011) Utility of ultrasound joint counts in the prediction of rheumatoid arthritis in patients with very early synovitis. Ann Rheum Dis 70(3):500–507
Filippucci E, da Luz KR, Di Geso L, Salaffi F, Tardella M, Carotti M, Natour J, Grassi W (2010) Interobserver reliability of ultrasonography in the assessment of cartilage damage in rheumatoid arthritis. Ann Rheum Dis 69(10):1845–1848
Filippucci E, Di Geso L, Grassi W (2014) Progress in imaging in rheumatology. Nat Rev Rheumatol 10(10):628–634
Finzel S, Ohrndorf S, Englbrecht M, Stach C, Messerschmidt J, Schett G, Backhaus M (2011) A detailed comparative study of high-resolution ultrasound and micro-computed tomography for detection of arthritic bone erosions. Arthritis Rheum 63(5):1231–1236
Freeston JE, Wakefield RJ, Conaghan PG, Hensor EM, Stewart SP, Emery P (2010) A diagnostic algorithm for persistence of very early inflammatory arthritis: the utility of power Doppler ultrasound when added to conventional assessment tools. Ann Rheum Dis 69(2):417–419
Funck-Brentano T, Gandjbakhch F, Etchepare F, Jousse-Joulin S, Miquel A, Cyteval C, Lukas C, Tobon GJ, Saraux A, Boumier P, Goupille P, Bourgeois P, Fautrel B (2013) Prediction of radiographic damage in early arthritis by sonographic erosions and power Doppler signal: a longitudinal observational study. Arthritis Care Res 65(6):896–902
Gandjbakhch F, Conaghan PG, Ejbjerg B, Haavardsholm EA, Foltz V, Brown AK, Moller Dohn U, Lassere M, Freeston J, Boyesen P, Bird P, Fautrel B, Hetland ML, Emery P, Bourgeois P, Horslev-Petersen K, Kvien TK, McQueen F, Ostergaard M (2011) Synovitis and osteitis are very frequent in rheumatoid arthritis clinical remission: results from an MRI study of 294 patients in clinical remission or low disease activity state. J Rheumatol 38(9):2039–2044
Gibofsky A (2014) Epidemiology, pathophysiology, and diagnosis of rheumatoid arthritis: A Synopsis. Am J Manag Care 20(7 Suppl):S128–S135
Gutierrez M, Filippucci E, Ruta S, Salaffi F, Blasetti P, Di Geso L, Grassi W (2011) Inter-observer reliability of high-resolution ultrasonography in the assessment of bone erosions in patients with rheumatoid arthritis: experience of an intensive dedicated training programme. Rheumatology (Oxford) 50(2):373–380
Iagnocco A, Epis O, Delle Sedie A, Meenagh G, Filippucci E, Riente L, Scire CA, Montecucco C, Bombardieri S, Grassi W, Valesini G (2008) Ultrasound imaging for the rheumatologist. XVII. Role of colour Doppler and power Doppler. Clin Exp Rheumatol 26(5):759–762
Jain M, Samuels J (2010) Musculoskeletal ultrasound in the diagnosis of rheumatic disease. Bull NYU Hosp Jt Dis 68(3):183–190
Ji L, Deng X, Geng Y, Song Z, Zhang Z (2017) The additional benefit of ultrasonography to 2010 ACR/EULAR classification criteria when diagnosing rheumatoid arthritis in the absence of anti-cyclic citrullinated peptide antibodies. Clin Rheumatol 36(2):261–267
Kane D, Grassi W, Sturrock R, Balint PV (2004) Musculoskeletal ultrasound--a state of the art review in rheumatology. Part 2: Clinical indications for musculoskeletal ultrasound in rheumatology. Rheumatology (Oxford) 43(7):829–838
Karim Z, Wakefield RJ, Conaghan PG, Lawson CA, Goh E, Quinn MA, Astin P, O’Connor P, Gibbon WW, Emery P (2001) The impact of ultrasonography on diagnosis and management of patients with musculoskeletal conditions. Arthritis Rheum 44(12):2932–2933
Karim Z, Quinn MA, Wakefield RJ, Brown AK, Green MJ, Hensor EM, Conaghan PG, Emery P (2007) Response to intramuscular methyl prednisolone in inflammatory hand pain: evidence for a targeted clinical, ultrasonographic and therapeutic approach. Ann Rheum Dis 66(5):690–692
Kawashiri SY, Suzuki T, Okada A, Yamasaki S, Tamai M, Nakamura H, Origuchi T, Mizokami A, Uetani M, Aoyagi K, Eguchi K, Kawakami A (2013) Musculoskeletal ultrasonography assists the diagnostic performance of the 2010 classification criteria for rheumatoid arthritis. Mod Rheumatol 23(1):36–43
Keen HI, Wakefield R, Conaghan PG (2014) Optimising ultrasonography in rheumatology. Clin Exp Rheumatol 32(5 Suppl 85):S-13–S-16
Kelly S, Davidson B, Keidel S, Gadola S, Gorman C, Meenagh G, Reynolds P (2017) The impact of rheumatologist-performed ultrasound on diagnosis and management of inflammatory arthritis in routine clinical practice. BMC Musculoskelet Disord 18(1):487
Kitchen J, Kane D (2015) Greyscale and power Doppler ultrasonographic evaluation of normal synovial joints: correlation with pro- and anti-inflammatory cytokines and angiogenic factors. Rheumatology (Oxford) 54(3):458–462
Koevoets R, Dirven L, Klarenbeek NB, van Krugten MV, Ronday HK, van der Heijde DM, Huizinga TW, Kerstens PS, Lems WF, Allaart CF (2013) Insights in the relationship of joint space narrowing versus erosive joint damage and physical functioning of patients with RA. Ann Rheum Dis 72(6):870–874
Kumar A (2014) How to investigate new-onset polyarthritis. Best Pract Res Clin Rheumatol 28(6):844–859
McAlindon T, Kissin E, Nazarian L, Ranganath V, Prakash S, Taylor M, Bannuru RR, Srinivasan S, Gogia M, McMahon MA, Grossman J, Kafaja S, FitzGerald J (2012) American College of Rheumatology report on reasonable use of musculoskeletal ultrasonography in rheumatology clinical practice. Arthritis Care Res 64(11):1625–1640
McGonagle D (2010) The history of erosions in rheumatoid arthritis: are erosions history? Arthritis Rheum 62(2):312–315
McInnes IB, Schett G (2011) The pathogenesis of rheumatoid arthritis. N Engl J Med 365(23):2205–2219
Minowa K, Ogasawara M, Murayama G, Gorai M, Yamada Y, Nemoto T, Matsuki Y, Sugisaki N, Ando S, Kon T, Tada K, Matsushita M, Yamaji K, Tamura N, Takasaki Y (2016) Predictive grade of ultrasound synovitis for diagnosing rheumatoid arthritis in clinical practice and the possible difference between patients with and without seropositivity. Mod Rheumatol 26(2):188–193
Moller B, Bonel H, Rotzetter M, Villiger PM, Ziswiler HR (2009) Measuring finger joint cartilage by ultrasound as a promising alternative to conventional radiograph imaging. Arthritis Rheum 61(4):435–441
Najm A, Orr C, Gallagher L, Biniecka M, Gaigneux E, Le Goff B, Fearon U, Veale DJ (2018) Knee joint synovitis: study of correlations and diagnostic performances of ultrasonography compared with histopathology. RMD Open 4(1):e000616
Nakagomi D, Ikeda K, Okubo A, Iwamoto T, Sanayama Y, Takahashi K, Yamagata M, Takatori H, Suzuki K, Takabayashi K, Nakajima H (2013) Ultrasound can improve the accuracy of the 2010 American College of Rheumatology/European League against rheumatism classification criteria for rheumatoid arthritis to predict the requirement for methotrexate treatment. Arthritis Rheum 65(4):890–898
Nam JL, D’Agostino MA (2017) Role of ultrasound imaging in individuals at risk of RA. Best Pract Res Clin Rheumatol 31(1):71–79
Naredo E, Iagnocco A (2012) Why use ultrasound in rheumatology? A valuable tool for diagnosis and research. Rheumatology (Oxford) 51:vii1
Naredo E, Rodriguez M, Campos C, Rodriguez-Heredia JM, Medina JA, Giner E, Martinez O, Toyos FJ, Ruiz T, Ros I, Pujol M, Miquel X, Garcia L, Aznar JJ, Chamizo E, Paez M, Morales P, Rueda A, Tuneu R, Corominas H, de Agustin JJ, Moragues C, Minguez D, Willisch A, Gonzalez-Cruz I, Aragon A, Iglesias G, Armas C, Pablo Valdazo J, Vargas C, Calvo-Alen J, Juan-Mas A, Salvador G, Puigdollers A, Galindez E, Garrido N, Salaberri J, Raya E, Salles M, Diaz C, Cuadra JL, Garrido J (2008) Validity, reproducibility, and responsiveness of a twelve-joint simplified power doppler ultrasonographic assessment of joint inflammation in rheumatoid arthritis. Arthritis Rheum 59(4):515–522
Navalho M, Resende C, Rodrigues AM, Pereira da Silva JA, Fonseca JE, Campos J, Canhao H (2013) Bilateral evaluation of the hand and wrist in untreated early inflammatory arthritis: a comparative study of ultrasonography and magnetic resonance imaging. J Rheumatol 40(8):1282–1292
NICE (2018) Rheumatoid arthritis in adults: diagnosis and management Evidence review a ultrasound for diagnosis, England. Available at: https://www.nice.org.uk/guidance/ng100/evidence/evidence-review-a-ultrasound-for-diagnosis-pdf-4903172318 (Accessed: 7th Aug 2018).
Ohrndorf S, Backhaus M (2013) Advances in sonographic scoring of rheumatoid arthritis. Ann Rheum Dis 72(Suppl 2):ii69–ii75
Ostergaard M (2012) Can imaging be used for inflammatory arthritis screening? Semin Musculoskelet Radiol 16(5):401–409
Ostergaard M, Ejbjerg B, Szkudlarek M (2005) Imaging in early rheumatoid arthritis: roles of magnetic resonance imaging, ultrasonography, conventional radiography and computed tomography. Best Pract Res Clin Rheumatol 19(1):91–116
Ostergaard M, McQueen F, Wiell C, Bird P, Boyesen P, Ejbjerg B, Peterfy C, Gandjbakhch F, Duer-Jensen A, Coates L, Haavardsholm EA, Hermann KG, Lassere M, O’Connor P, Emery P, Genant H, Conaghan PG (2009) The OMERACT psoriatic arthritis magnetic resonance imaging scoring system (PsAMRIS): definitions of key pathologies, suggested MRI sequences, and preliminary scoring system for PsA Hands. J Rheumatol 36(8):1816–1824
Ostrowska M, Maslinski W, Prochorec-Sobieszek M, Nieciecki M, Sudol-Szopinska I (2018) Cartilage and bone damage in rheumatoid arthritis. Reumatologia 56(2):111–120
Ozgul A, Yasar E, Arslan N, Balaban B, Taskaynatan MA, Tezel K, Baklaci K, Ozguven MA, Kalyon TA (2009) The comparison of ultrasonographic and scintigraphic findings of early arthritis in revealing rheumatoid arthritis according to criteria of American College of Rheumatology. Rheumatol Int 29(7):765–768
Pearman L, Last J, Fitzgerald O, Veale D, Joyce M, Rainford L, McEntee M, McNulty J, Thomas E, Ryan J, McGee A, Toomey R, D’Helft C, Lowe J, Brennan PC (2009) Rheumatoid arthritis: a novel radiographic projection for hand assessment. Br J Radiol 82(979):554–560
Peluso G, Michelutti A, Bosello S, Gremese E, Tolusso B, Ferraccioli G (2011) Clinical and ultrasonographic remission determines different chances of relapse in early and long standing rheumatoid arthritis. Ann Rheum Dis 70(1):172–175
Perry D, Stewart N, Benton N, Robinson E, Yeoman S, Crabbe J, McQueen F (2005) Detection of erosions in the rheumatoid hand; a comparative study of multidetector computerized tomography versus magnetic resonance scanning. J Rheumatol 32(2):256–267
Plagou A, Teh J, Grainger AJ, Schueller-Weidekamm C, Sudol-Szopinska I, Rennie W, Astrom G, Feydy A, Giraudo C, Guerini H, Guglielmi G, Isaac A, Jans L, Jurik AG, Kainberger F, Maas M, Martinoli C, Mascarenhas VV, Miese F, O’Connor P, Oei EH, Ostergaard M, Peetrons P, Platzgummer H, Reijnierse M, Robinson P, Rupreht M, Simoni P, Wick MC, Zejden A, Klauser AS (2016) Recommendations of the ESSR arthritis subcommittee on ultrasonography in inflammatory joint disease. Semin Musculoskelet Radiol 20(5):496–506
Plaza M, Nowakowska-Plaza A, Pracon G, Sudol-Szopinska I (2016) Role of ultrasonography in the diagnosis of rheumatic diseases in light of ACR/EULAR guidelines. J Ultrason 16(64):55–64
Porta F, Radunovic G, Vlad V, Micu MC, Nestorova R, Petranova T, Iagnocco A (2012) The role of Doppler ultrasound in rheumatic diseases. Rheumatology (Oxford) 51(6):976–982
Pratt AG, Lorenzi AR, Wilson G, Platt PN, Isaacs JD (2013) Predicting persistent inflammatory arthritis amongst early arthritis clinic patients in the UK: is musculoskeletal ultrasound required? Arthritis Res Ther 15(5):R118
Rahimi H, Bell R, Bouta EM, Wood RW, Xing L, Ritchlin CT, Schwarz EM (2016) Lymphatic imaging to assess rheumatoid flare: mechanistic insights and biomarker potential. Arthritis Res Ther 18:194
Rezaei H, Torp-Pedersen S, af Klint E, Backheden M, Kisten Y, Gyori N, van Vollenhoven RF (2014) Diagnostic utility of musculoskeletal ultrasound in patients with suspected arthritis--a probabilistic approach’. Arthritis Res Ther 16(5):448
Sahbudin I, Pickup L, Nightingale P, Allen G, Cader Z, Singh R, de Pablo P, Buckley CD, Raza K and Filer A (2018) ‘The role of ultrasound-defined tenosynovitis and synovitis in the prediction of rheumatoid arthritis development’, Rheumatology (Oxford).
Salaffi F, Ciapetti A, Gasparini S, Carotti M, Filippucci E, Grassi W (2010) A clinical prediction rule combining routine assessment and power Doppler ultrasonography for predicting progression to rheumatoid arthritis from early-onset undifferentiated arthritis. Clin Exp Rheumatol 28(5):686–694
Salaffi F, Gutierrez M, Carotti M (2014) Ultrasound versus conventional radiography in the assessment of bone erosions in rheumatoid arthritis. Clin Exp Rheumatol 32(1 Suppl 80):S85–S90
Sheane BJ, Beddy P, O’Connor M, Miller S, Cunnane G (2009) Targeted ultrasound of the fifth metatarsophalangeal joint in an early inflammatory arthritis cohort. Arthritis Rheum 61(7):1004–1008
Spencer SP, Ganeshalingam S, Kelly S, Ahmad M (2012) The role of ultrasound in the diagnosis and follow-up of early inflammatory arthritis. Clin Radiol 67(1):15–23
Sudoł-Szopińska I (2013) ‘Role of inflammatory factors and adipose tissue in pathogenesis of rheumatoid arthritis and osteoarthritis. Part I: Rheumatoid Adipose Tissue’ 53:192–201
Szkudlarek M, Court-Payen M, Jacobsen S, Klarlund M, Thomsen HS, Ostergaard M (2003) Interobserver agreement in ultrasonography of the finger and toe joints in rheumatoid arthritis. Arthritis Rheum 48(4):955–962
Szkudlarek M, Narvestad E, Klarlund M, Court-Payen M, Thomsen HS, Ostergaard M (2004) Ultrasonography of the metatarsophalangeal joints in rheumatoid arthritis: comparison with magnetic resonance imaging, conventional radiography, and clinical examination. Arthritis Rheum 50(7):2103–2112
Tamas MM, Filippucci E, Becciolini A, Gutierrez M, Di Geso L, Bonfiglioli K, Voulgari PV, Salaffi F, Grassi W (2014) Bone erosions in rheumatoid arthritis: ultrasound findings in the early stage of the disease. Rheumatology (Oxford) 53(6):1100–1107
Tan YK, Conaghan PG (2011) Imaging in rheumatoid arthritis. Best Pract Res Clin Rheumatol 25(4):569–584
Tan YK, Ostergaard M, Conaghan PG (2012) Imaging tools in rheumatoid arthritis: ultrasound vs magnetic resonance imaging. Rheumatology (Oxford) 51(Suppl 7):vii36–vii42
Ten Cate DF, Luime JJ, Swen N, Gerards AH, De Jager MH, Basoski NM, Hazes JM, Haagsma CJ, Jacobs JW (2013) Role of ultrasonography in diagnosing early rheumatoid arthritis and remission of rheumatoid arthritis--a systematic review of the literature. Arthritis Res Ther 15(1):R4
Terslev L, von der Recke P, Torp-Pedersen S, Koenig MJ, Bliddal H (2008) Diagnostic sensitivity and specificity of Doppler ultrasound in rheumatoid arthritis. J Rheumatol 35(1):49–53
Tins BJ, Butler R (2013) Imaging in rheumatology: reconciling radiology and rheumatology. Insights Imaging 4(6):799–810
van Aken J, Lard L, le Cessie S, Hazes J, Breedveld F, Huizinga T (2004) Radiological outcome after four years of early versus delayed treatment strategy in patients with recent onset rheumatoid arthritis. Ann Rheum Dis 63(3):274–279
Wakefield RJ, Gibbon WW, Conaghan PG, O’Connor P, McGonagle D, Pease C, Green MJ, Veale DJ, Isaacs JD, Emery P (2000) The value of sonography in the detection of bone erosions in patients with rheumatoid arthritis: a comparison with conventional radiography. Arthritis Rheum 43(12):2762–2770
Wakefield RJ, Balint PV, Szkudlarek M, Filippucci E, Backhaus M, D’Agostino MA, Sanchez EN, Iagnocco A, Schmidt WA, Bruyn GA, Kane D, O’Connor PJ, Manger B, Joshua F, Koski J, Grassi W, Lassere MN, Swen N, Kainberger F, Klauser A, Ostergaard M, Brown AK, Machold KP, Conaghan PG (2005) Musculoskeletal ultrasound including definitions for ultrasonographic pathology. J Rheumatol 32(12):2485–2487
Yue J, Wu D, Tam LS (2018) The role of imaging in early diagnosis and prevention of joint damage in inflammatory arthritis. Expert Rev Clin Immunol 14(6):499–511
Zhang H, Xu H, Chen S, Mao X (2018a) The application value of MRI in the diagnosis of subclinical inflammation in patients with rheumatoid arthritis in remission. J Orthop Surg Res 13(1):164
Zhang YH, Li K, Xiao J, Zhang HD, Zhang XY (2018b) Comparison of ultrasound, radiography, and clinical investigations in the diagnosis of early rheumatoid synovitis in patients with nonspecific musculoskeletal symptoms: a multicenter cross-sectional study. Med Sci Monit 24:4372–4378
Zufferey P, Tamborrini G, Gabay C, Krebs A, Kyburz D, Michel B, Moser U, Villiger PM, So A, Ziswiler HR (2013) Recommendations for the use of ultrasound in rheumatoid arthritis: literature review and SONAR score experience. Swiss Med Wkly 143:w13861
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that she has no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Boylan, M. Should ultrasound be used routinely in the diagnosis of rheumatoid arthritis?. Ir J Med Sci 189, 735–748 (2020). https://doi.org/10.1007/s11845-019-02096-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-019-02096-3