Abstract
Background
Burnout is an occupational syndrome frequently encountered within the healthcare profession. It is characterised by emotional exhaustion (EE), depersonalisation (DP) and a low sense of personal accomplishment (PA). Its negative impact extends to the physician, patient and overall service provision.
Aims
The aim of this study was to evaluate work patterns, the prevalence of burnout and its associations in medical oncology consultants and specialist registrars (SpRs) in Ireland.
Methods
Participants were invited to partake in an anonymised online survey. Burnout domains were measured using the validated Maslach Burnout Inventory. Associations between variables were evaluated using the Mann-Whitney U and Kruskal-Wallis tests (continuous), and chi-square and Fisher’s exact testing (categorical).
Results
Seventy-four physicians were contacted to participate, 44 (59%) completed the survey. The majority (71%) work ≥ 50 h a week, with 57% having additional on-call commitments of ≥ 5 days/month. Burnout is defined by a high score in EE combined with a high DP and/or low PA was identified in 45% of consultants and 20% of SpRs. Longer working hours (≥ 60 h/ week) were found to be associated with both high EE (p = 0.049) and DP (p = 0.019). Higher EE scores were demonstrated in those ≥ 40 years (p = 0.04). The majority (86%) reported they would become an oncologist again.
Conclusion
One or more of the symptoms of burnout is highly prevalent in medical oncologists in Ireland. With increasing pressure on resources, burnout is expected to increase. Attention to strategies for prevention needs to be prioritised within our healthcare system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Burnout is an occupational syndrome characterised by emotional exhaustion (EE), depersonalisation (DP; an impersonal response towards patients) and lack of personal accomplishment (PA; feelings of reduced competence and success within ones work) [1]. As a construct, its symptoms overlap with depression, and there is debate as to whether it is a distinct pathological entity [2, 3]. Regardless, it has been frequently encountered in healthcare professionals [4, 5]. The aetiology of burnout is often multifactorial. Personal and professional characteristics may contribute to, or protect one, from its development.
A career in oncology is highly rewarding for a number of reasons. It provides the opportunity to be involved in a specialty that is at the forefront of scientific advances within healthcare. Oncologists are in a position to develop meaningful relationships with their patients and provide compassion and assistance to them at their most vulnerable. However, frequent exposure to death, difficult decisions about the administration of toxic therapies and managing their effects on the patient, and working within a highly emotive environment may have the effect of increasing the stress and emotional burden on the oncologist [6].
Consequences of burnout not only extend to the personal and professional health of the physician, but to the health of the patient and the health system as a whole [7, 8]. In the era of increasing workload secondary to technological and medical advances, coupled with the resultant growing constraints on resources, the issue of burnout is brought to the forefront.
Our study aims to evaluate the presence of burnout in medical oncologists in Ireland. In addition, we sought to identify factors associated with the syndrome in order to inform strategies to reduce its prevalence and improve outcomes for the physician, patient and healthcare system.
Methods
Participation
All medical oncology consultants and specialist registrars (SpRs) in Ireland were invited to participate in this study. Medical oncology consultants were identified and contacted via a database accessible to all consultants and maintained by an organisational committee. Specialist registrars were identified and contacted via the Royal College of Physicians of Ireland Higher Specialist Training department. Consultants and SpRs were contacted via email and the purpose of the study outlined. The email contained a link to an online survey, facilitated through the online platform Survey Monkey. Participation was voluntary, and this was an anonymised survey. Authors were not aware as to whether an invited participant had responded to the survey. The survey included a measurement of burnout and questions regarding their personal and professional characteristics. Personal and professional characteristics were collected in categories (e.g. age 30–39, 40–49, etc.) and as a result individuals were not identifiable by these results.
Measures
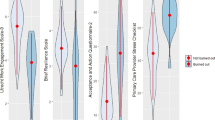
As part of this study, professional characteristics such as working hours, on-call hours and patient numbers in clinic were collected. Participants were asked to select an answer that fell into a range that best represented the average number for each characteristic. (See results table for ranges.)
The survey utilised the validated Maslach Burnout Inventory (MBI), an internationally accepted standard for the measurement of burnout [1]. The MBI is a 22-itemed questionnaire that measures the three domains of burnout (EE, DP and PA), using a 7-point Likert scale for responses. Respondents rate each job-related feeling based on how often they encounter it. Each domain has an individual score and is classified as high, moderate or low. As per the MBI 3rd edition manual, a high score in EE (≥ 27) or DP (≥ 10), or a low score in PA (≤ 33) indicate higher degrees of burnout in the occupational subgroup of medicine. The MBI cautions that there is no definitive score that proves the presence of burnout. For the purpose of our study, we have outlined the results for each domain as categorised as either high, moderate or low. In addition, we have utilised previously accepted measures of burnout as those with a high score in EE accompanied by either a high DP or low PA or both [9].
The internal consistency of results as measured by Cronbach’s alpha was satisfactory for all subscales of the MBI (0.82–0.89).
Statistical analysis
All fully completed surveys were included in the statistical analysis. Associations between categorical variables were tested using chi-square testing or Fisher’s exact testing as appropriate. Associations between continuous variables were tested using Mann-Whitney U and Kruskal-Wallis tests as appropriate. Associations between means were tested using the student’s t test. All tests were two sided with a type I error set at 0.05. Statistical analyses were performed with SPSS version 24.
Results
Seventy-four oncologists were contacted to participate in the study, and 44 (59%) completed the survey in full. Twenty-nine were consultants and 15 SpRs. Demographics of respondents are outlined in Table 1.
Work patterns
The majority of oncologists work over 50 h a week—76% of consultants and 60% of specialist registrars. A significantly greater number of consultants work more than 60 h a week, not including on-call commitments, compared with SpRs (41.4% vs. 6.7%, p = 0.034) (Fig. 1). Notably this included 5 consultants who work in a public only post.
More than half of consultants and SpRs spend greater than 10 h a week on administrative tasks in work (51.7% and 73.4%, respectively). Administrative work at home is also common with those dedicating 5 or more hours a week to these tasks comprising 44.8% of consultants and 60% of SpRs (Fig. 2). SpRs spend more time on professional development at home than consultants with the majority spending greater than 5 h a week on professional development (60% SpRs vs. 27.6% consultants, p = 0.029) (Table 2).
Burnout
Burnout was identified in 45% of consultants and 20% of SpRs. Results are outlined in Table 3. The mean and median scores for each domain of burnout were calculated for all respondents and for professional grade. The mean score for EE, DP and PA in all respondents fall within the moderate score category. There was no statistically significant difference between consultants and SpRs.
Characteristics associated with burnout
Associations between professional characteristics and likelihood of burnout were examined. Higher EE scores were demonstrated in those over the age of 40 years compared with those under the age of 40 (mean rank of 26.26 vs 18.38, respectively; U = 155, p = 0.042). Those working 60 or more hours a week were more likely to have a high EE score (mean rank of 28.38 vs. 20.03 respectively; U = 125, p = 0.049). Working greater than 60 h a week was also associated with a higher DP score than those working less than 60 h (mean rank of 29.5 vs 19.56, respectively; U = 110.5, p = 0.019).
Career choice
The majority of respondents would pursue a career in medicine again—83% of consultants and 87% of SpRs. All of those that would pursue a career in medicine again responded that they would become an oncologist again. Of the 5 consultants, 4 who would not pursue a career in medicine again were classified as suffering from burnout.
Discussion
This is the first national study of work patterns and prevalence of burnout in medical oncologists in Ireland. These results demonstrate that burnout is experienced by over a third of medical oncologists in Ireland.
International and interdisciplinary comparison of burnout prevalence
There are a number of large studies examining the rates of burnout in oncology internationally. Shanafelt et al. undertook a survey of nearly 3000 medical oncologists (not including trainees) in the USA and demonstrated a rate of burnout of 44.7%. This is comparable to the rate seen in oncology consultants in our group. Their definition of burnout was less restrictive however, defining burnout as a high score in either DP and/or EE [10]. In Europe, the European Society for Medical Oncology (ESMO) young oncologists committee demonstrated a burnout rate of 62% in oncologists aged 40 and under, across 41 countries, using the same definition as the Shanafelt study [11]. Using the definition as per the ESMO and Shanafelt studies would inflate the prevalence in our population. It is worth noting that at least one symptom of burnout (high EE/DP or low PA) was identified in 20 (69%) consultants and 8 (53%) SpRs in our study, although this is not enough to qualify respondents as ‘burnt-out’.
Nationally, comparisons can be made to a study by Hayes et al. [12] from the Royal College of Physicians of Ireland (RCPI), who undertook a survey of 1749 hospital trainees and consultants, using the same definition for burnout as our study. The prevalence of burnout in the total group was similar to our study at 30.7%. However, the rates were lower in consultants than SpRs (24.4% vs 38% respectively), which would be more in line with international literature.
Career stage and prevalence of burnout
Burnout was found in a higher percentage of consultants than SpRs in our study. This did not reach statistical significance in our sample size but the absolute figures do diverge noticeably. This finding is at odds with published data which typically demonstrates higher rates of burnout in trainees and younger doctors [13, 14]. A higher rate of burnout in trainees is also demonstrable nationally, as seen in the aforementioned RCPI study [12] and additionally within Irish interns by Hannan et al. [15], whom demonstrated rates of DP and EE exceeding 50% in this group.
There may be a number of reasons why burnout is higher in our consultant group. We have identified that our consultants work longer hours and have greater on-call commitments than SpRs. This has been demonstrated to be associated with higher rates of burnout in oncologists [10]. Additionally, our consultant group comprise mostly of respondents under the age of 50 (76% of respondents) as opposed to 50 or over. The higher proportion of younger consultant respondents may explain the higher rates of burnout in this group comparative to other studies.
Aetiology of burnout
Within our study, we assessed associations between burnout and job characteristics. This has been previously well established with job demands (e.g. workload, role conflict) and lack of resources associated with burnout [16, 17]. Our study demonstrates that long working hours are associated with higher scores in the EE and DP domains of the MBI. Shanafelt et al. [10] identified a similar pattern with greater number of hours seeing patients each week being associated with higher rates of burnout. They reported that an additional hour spent seeing patients each week increased the risk of burnout by approximately 2% to 4%. In their study, each additional hour per week spent on work-related tasks while at home also increased the risk of burnout by approximately 2%.
It is important to highlight this association between hours worked and rates of burnout. The incidence of cancer in Ireland is increasing. The National Cancer Strategy 2017–2026 outlines an expected doubling in cancer incidence by 2040 compared with 2010, largely secondary to an ageing population and increased life expectancy [18]. With this increasing incidence of cancer and the remarkable advancements in treatments, the workload of medical oncologists will increase exponentially. As outlined, this has the potential to increase the levels of physician burnout if adequate resources and staffing are not addressed. Of course, this increasing workload does not exclusively apply to medical oncology and can be expected across all disciplines in healthcare in Ireland.
Personal characteristics and their association with burnout were also examined. Irish oncologists are also more likely to develop burnout with increasing age (40 or over), although as previously mentioned, we note the majority of respondents in our group were under the age of 50. Shanafelt’s group was at odds to our study with younger age independently associated with burnout in their findings. This is likely secondary to the differing work patterns of oncologists in the USA and Ireland.
Consequences of burnout
The consequences of burnout on the healthcare system are legion, affecting the physician, the department and the patient. The relationship between burnout and the health of the physician has been studied demonstrating an association between burnout and a number of physical health issues including cardiovascular and musculoskeletal disorders [19]. Associations between substance abuse disorders, personal relationship conflict and depression have also been established [20, 21].
Physician professionalism is affected by burnout and has negative effects on the patient. Burnout is associated with reduced physician empathy [8, 22]. Ensuing lack of confidence in one’s treatment and lack of compliance to prescribed treatments is a concern. A relationship between burnout and medical error is clearly documented in the literature. One large systematic review performed by Hall et al. [23] revealed that an increased number of medical errors is significantly associated with physician burnout.
Additionally, burnout may have a consequence on staffing. Initial thoughts about burnout predicted that it would be associated with a desire to quit one’s job and this has been demonstrated in early and more recent research [17, 24]. Jourdain and Chenevert [25] demonstrated a significant relationship between EE and DP with the intention to leave one’s profession. We did not explore the intention to quit within our study. The majority of oncologists in Ireland report that they would become a doctor and an oncologist again. However, within the consultant group, 4 of the 13 (31%) respondents suffering from burnout would not pursue a career in medicine again. We should be careful to take heed of the association between burnout and intention to quit and prevent a situation where this is its consequence.
Addressing and treating burnout
Encouragingly, we know that burnout is reversible and this has been documented in a number of prospective studies with rates of reversibility between 21 and 27% [20, 26]. Both individual-focused and organisational solutions to burnout have been tested.
Individual-based strategies to address burnout include techniques and training such as stress management, self-care training, mindfulness training and communication skills training [27]. Qualitative studies have demonstrated that individuals who place a greater emphasis on finding a meaning to their work, adopt a philosophy of work/life balance and maintain a focus on what is important in life have demonstrated lower rates of burnout [28, 29]. The concept of resilience has become more widely recognised in recent years as a strategy to prevent the development, or reverse the presence, of burnout. Resilience is a theory defined by positive adaptation in the setting of adversity or stressors [30]. It involves the ability to activate resources or attitudes to facilitate coping strategies despite a stressful work environment. Many of these individual-based strategies to prevent or treat burnout involve developing the individual’s resilience to burnout.
Although much of the focus of addressing burnout has been at an individual level, the healthcare organisation plays an important role in addressing work-related factors that contribute to burnout [31, 32]. These interventions are not just limited to reducing working hours but improving the work environment by improving team dynamics, prioritising efficient use of physician time, adequate staffing, etc. Improvement in working conditions also allows for development of physician resilience [30].
A systematic review and meta-analysis sought to identify studies of interventions to prevent and reduce physician burnout [33]. They included randomised controlled trials and cohort studies. Interventions included structural interventions within the work environment, (e.g. shortened attending rotation length, various modifications to clinical work processes, shortened resident shifts) and individual-focused interventions (e.g. small group stress management and self-care training, mindfulness training, communication skills training). They demonstrated a significant reduction in overall burnout scores, EE and DP scores with intervention. For overall burnout scores, structural interventions were associated with a greater reduction in incidence of overall burnout compared with individual interventions (p = 0.03).
Due to the negative impact outlined, organisations and training bodies have a vested interest in reducing the rates of burnout to preserve competent, healthy and productive staff. The onset of burnout as early as university should direct our attention to instituting interventions from this stage onwards. Within Ireland, many of the training bodies have developed wellbeing programmes or resources for their trainees and consultants. Organisational-based interventions at a more local level require more attention.
Limitations
There are a number of limitations to our study. We would consider the response rate of 59% satisfactory as it is in line or higher than reported physician survey rates. A form of participation bias is a possibility however, where those who are more affected by this issue of burnout are more likely to respond. We also recognise that our sample size is small which may have limited the ability to draw statistically significant conclusions for some of the tested associations. Due to the self-reporting nature of the survey, recall bias may affect some responses.
Conclusion
Burnout is experienced by over a third of Irish oncologists, with preponderance in consultants. Despite this, the majority report that they would pursue a career in medicine again. As work demands increase and resources become more stretched, burnout can be predicted to increase. Strategies to reduce the incidence of burnout and prevent the development of its consequences on an overextended healthcare system need to be prioritised.
References
Maslach C, Jackson S, Leiter M et al (2016). Maslach burnout inventory, fourth edn. Mind Garden, Inc., California.
Bianchi R, Schonfeld IS, Laurent E (2019) The trouble with burnout: an update on burnout-depression overlap. Am J Psychiatry 176(1):79. https://doi.org/10.1176/appi.ajp.2018.18091026
Schonfeld IS, Verkuilen J, Bianchi R (2019) Inquiry into the correlation between burnout and depression. J Occup Health Psychol. https://doi.org/10.1037/ocp0000151
Ramirez AJ, Graham J, Richards MA, Gregory WM, Cull A (1996) Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet 347(9003):724–728
Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, West CP, Sloan J, Oreskovich MR (2012) Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med 172(18):1377–1385. https://doi.org/10.1001/archinternmed.2012.3199
Shanafelt T, Dyrbye L (2012) Oncologist burnout: causes, consequences, and responses. J Clin Oncol 30(11):1235–1241. https://doi.org/10.1200/JCO.2011.39.7380
Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, Collicott P, Novotny PJ, Sloan J, Freischlag J (2010) Burnout and medical errors among American surgeons. Ann Surg 251(6):995–1000. https://doi.org/10.1097/SLA.0b013e3181bfdab3
Shanafelt TD, Bradley KA, Wipf JE, Back AL (2002) Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med 136(5):358–367
Brenninkmeijer V, VanYperen N (2003) How to conduct research on burnout: advantages and disadvantages of a unidimensional approach in burnout research. Occup Environ Med 60(Suppl 1):i16–i20. https://doi.org/10.1136/oem.60.suppl_1.i16
Shanafelt TD, Gradishar WJ, Kosty M, Satele D, Chew H, Horn L, Clark B, Hanley AE, Chu Q, Pippen J, Sloan J, Raymond M (2014) Burnout and career satisfaction among US oncologists. J Clin Oncol 32(7):678–686. https://doi.org/10.1200/JCO.2013.51.8480
Banerjee S, Califano R, Corral J, de Azambuja E, de Mattos-Arruda L, Guarneri V, Hutka M, Jordan K, Martinelli E, Mountzios G, Ozturk MA, Petrova M, Postel-Vinay S, Preusser M, Qvortrup C, Volkov MNM, Tabernero J, Olmos D, Strijbos MH (2017) Professional burnout in European young oncologists: results of the European Society for Medical Oncology (ESMO) Young Oncologists Committee Burnout Survey. Ann Oncol 28(7):1590–1596. https://doi.org/10.1093/annonc/mdx196
Hayes B, Prihodova L, Walsh G, Doyle F, Doherty S (2019) Doctors don't do-little: a national cross-sectional study of workplace well-being of hospital doctors in Ireland. BMJ Open 9(3):e025433. https://doi.org/10.1136/bmjopen-2018-025433
Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, Shanafelt TD (2014) Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med 89(3):443–451. https://doi.org/10.1097/ACM.0000000000000134
Amoafo E, Hanbali N, Patel A, Singh P (2015) What are the significant factors associated with burnout in doctors? Occup Med 65(2):117–121. https://doi.org/10.1093/occmed/kqu144
Hannan E, Breslin N, Doherty E, McGreal M, Moneley D, Offiah G (2018) Burnout and stress amongst interns in Irish hospitals: contributing factors and potential solutions. Ir J Med Sci 187(2):301–307. https://doi.org/10.1007/s11845-017-1688-7
Demerouti E, Bakker AB, Nachreiner F et al (2001) The job demands-resources model of burnout. J Appl Psychol 86(3):499–512
Alarcon GM (2011) A meta-analysis of burnout with job demands, resources, and attitudes. J Vocat Behav 79(2):549–562
Department of Health (2017). National Cancer Strategy 2017- 2026. https://health.gov.ie/wp-content/uploads/2017/07/National-Cancer-Strategy-2017-2026.pdf. Accessed 22 October 2018.
Honkonen T, Ahola K, Pertovaara M, Isometsä E, Kalimo R, Nykyri E, Aromaa A, Lönnqvist J (2006) The association between burnout and physical illness in the general population--results from the Finnish Health 2000 Study. J Psychosom Res 61(1):59–66. https://doi.org/10.1016/j.jpsychores.2005.10.002
Dyrbye LN, Thomas MR, Massie FS, Power DV, Eacker A, Harper W, Durning S, Moutier C, Szydlo DW, Novotny PJ, Sloan JA, Shanafelt TD (2008) Burnout and suicidal ideation among U.S. medical students. Ann Intern Med 149(5):334–341
Oreskovich MR, Kaups KL, Balch CM et al (2012) Prevalence of alcohol use disorders among American surgeons. Arch Surg 147(2):168–174. https://doi.org/10.1001/archsurg.2011.1481
Bellini LM, Shea JA (2005) Mood change and empathy decline persist during three years of internal medicine training. Acad Med 80(2):164–167
Hall LH, Johnson J, Watt I, Tsipa A, O’Connor DB (2016) Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS One 11(7):e0159015. https://doi.org/10.1371/journal.pone.0159015
Maslach CJ, S. E. (1984) Patterns of burnout among a national sample of public contact workers. J Health Hum Resour Adm 7:189–212
Jourdain G, Chenevert D (2010) Job demands-resources, burnout and intention to leave the nursing profession: a questionnaire survey. Int J Nurs Stud 47(6):709–722. https://doi.org/10.1016/j.ijnurstu.2009.11.007
Campbell J, Prochazka AV, Yamashita T, Gopal R (2010) Predictors of persistent burnout in internal medicine residents: a prospective cohort study. Acad Med 85(10):1630–1634. https://doi.org/10.1097/ACM.0b013e3181f0c4e7
Krasner MS, Epstein RM, Beckman H et al (2009) Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. Jama 302(12):1284–1293. https://doi.org/10.1001/jama.2009.1384
Shanafelt TD, Oreskovich MR, Dyrbye LN, Satele DV, Hanks JB, Sloan JA, Balch CM (2012) Avoiding burnout: the personal health habits and wellness practices of US surgeons. Ann Surg 255(4):625–633. https://doi.org/10.1097/SLA.0b013e31824b2fa0
Shanafelt TD, Novotny P, Johnson ME, Zhao X, Steensma DP, Lacy MQ, Rubin J, Sloan J (2005) The well-being and personal wellness promotion strategies of medical oncologists in the North Central Cancer Treatment Group. Oncology 68(1):23–32. https://doi.org/10.1159/000084519
Hlubocky FJ, Rose M, Epstein RM (2017) Mastering resilience in oncology: learn to thrive in the face of burnout. Am Soc Clin Oncol Educ Book 37:771–781. https://doi.org/10.14694/EDBK_173874
Dunn PM, Arnetz BB, Christensen JF, Homer L (2007) Meeting the imperative to improve physician well-being: assessment of an innovative program. J Gen Intern Med 22(11):1544–1552. https://doi.org/10.1007/s11606-007-0363-5
Linzer M, Poplau S, Grossman E, Varkey A, Yale S, Williams E, Hicks L, Brown RL, Wallock J, Kohnhorst D, Barbouche M (2015) A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: results from the healthy work place (HWP) study. J Gen Intern Med 30(8):1105–1111. https://doi.org/10.1007/s11606-015-3235-4
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD (2016) Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 388(10057):2272–2281. https://doi.org/10.1016/S0140-6736(16)31279-X
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Corrigan, L., O’Leary, C., Kroes, J. et al. Professional burnout, work patterns and career satisfaction in medical oncologists in Ireland. Ir J Med Sci 189, 711–718 (2020). https://doi.org/10.1007/s11845-019-02088-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-019-02088-3