Abstract
Pulsed radiofrequency treatment adjacent to the cervical dorsal root ganglion is used to treat persistent cervical radicular pain that has not responded to conservative therapies. This technique has gained popularity in years for both cervical and lumbosacral radicular pain. The evidence to support its use is still evolving.
Methods
We performed a retrospective review of outcomes in 59 patients who underwent this therapy over a 3-year period in our institution. We evaluated a reduction in pain, duration of pain relief, reduction in use of analgesics and progression to surgery.
Results
Our results demonstrated 49 patients experienced some relief. Forty patients of the 59 experienced an improvement in pain of 50% or more. The mean duration of relief in this group was 37 weeks. Seven patients experienced complete resolution of their pain. In this group, the mean duration of relief was 39 weeks. Regarding the 53 patients who were taking medication for pain prior to the procedure, 37 patients reduced or discontinued their usage after the procedure.
Conclusion
Despite the limitations of a retrospective study, we feel our study adds to the growing evidence base that pulsed radiofrequency treatment adjacent to the cervical dorsal root ganglion has a role in the treatment of chronic cervical radicular pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical radicular pain is defined as pain perceived as arising in the upper limb secondary to ectopic activation of nociceptive afferent fibres in a spinal nerve or its roots. Chronic cervical radicular pain while less common than its lumbosacral counterpart with an incidence of 83 per 100,000 can cause significant debilitation [1]. The aetiology in 25% of cases is a herniated intervertebral disc [1]. Chronic degenerative changes at the zygapophyseal joints with osteophyte formation are another common cause [2]. Trauma is only implicated in approximately 15% of patients [1]. The natural history of cervical radicular pain dictates that most will improve or resolve without intervention. However, for those patients whose symptoms persist, the pain can cause significant physical and psychological impairment with potential disability and reduced capacity to remain employed [3, 4]. If conservative management medications like nonsteroidal anti-inflammatory drugs (NSAIDs), anticonvulsants and antidepressants along with standard physiotherapy fail to alleviate such pain, interventional techniques may be considered a less invasive alternative to surgery. Traditionally, both transforaminal and interlaminar epidural steroids were used to treat persistent symptoms with a moderate and temporary effect [5]. A selective nerve root block (SNRB) using local anaesthetic has a good diagnostic value to confirm the nerve root and the dermatome involved but has very little therapeutic benefit. Pulsed radiofrequency (PRF) applied to the dorsal root ganglion (DRG) is a minimally invasive day-care treatment, which is gaining significant clinical acceptance in a select group of patients with lumbar and cervical radicular pain [6, 7]. The likely appeal of this technique stems from the non-destructive nature of the procedure as compared with the destructive heat lesion that occurs with a continuous radiofrequency (CRF) treatment [8]. Apart from treating chronic radicular pain, this technique is also used for other persistent pain conditions including chronic knee pain, occipital neuralgia and isolated peripheral neuropathies but the evidence is still evolving [9,10,11]. In this retrospective study, we analysed the outcomes of PRF adjacent to the cervical dorsal root ganglion in patients with chronic cervical radicular pain.
Methods
Patients
The study was conducted at St. James’s Hospital, Dublin. All the patients included in this study had been referred to the pain clinic for evaluation and management of cervical radicular pain by their general practitioner (GP) or a hospital consultant. Diagnosis of radicular pain was made based on history, examination and magnetic resonance imaging (MRI) scan. Eighty-three charts were reviewed. Attempts were made to contact all 83 patients; however, only 59 completed the phone follow-up. These 59 patients who underwent cervical dorsal root ganglion pulsed radiofrequency treatment during the period from November 2011 to December 2016 were included. The inclusion criterion was a patient who had received pulsed radiofrequency treatment adjacent the dorsal root ganglion at a cervical level in the day surgery theatre during the time period from November 2011 and December 2016. Ethical approval was granted locally to review theatre logs, patient’s records and to contact patients via telephone with an approved scripted questionnaire. The medical records containing the procedure note for each patient were reviewed to note the level at which the procedure was carried out and the technique including needle used, medications administered and radiofrequency settings. Patients were then contacted by phone call and if the patient consented, then, the scripted questions were asked. If there was no answer from the patient, a maximum of 4 attempts were made to contact the patient. The outcomes assessed in the questionnaire included extent of pain relief after the procedure, an improvement of 50% or more in pain after the procedure, complete resolution of pain after the procedure, duration of pain relief (in weeks), cross over to surgery and any reduction in pain-relieving medication after the procedure if applicable. Although the duration of symptoms prior to the intervention was not recorded, all patients had chronic cervical radicular pain of three months or more.
Intervention technique
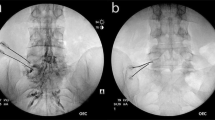
After obtaining informed written consent, patients were brought to theatre for the procedure. Patients were positioned supine and they remained awake, without sedation during the intervention to facilitate accurate sensory testing. Standard monitoring included heart rate, oxygen saturation and blood pressure. An intravenous cannula was sited in each patient. Under aseptic conditions and following skin preparation, Lignocaine 1% was used to provide local anaesthesia. A 22-gauge RF needle with 5-mm exposed tip was then inserted and advanced under fluoroscopic guidance. A Neurotherm model NT2000 PRF generator was used for the procedure. When the anatomical position of the RF needle was optimized (Tip in the dorso-caudal quadrant of the foramen) (Fig. 1), sensory stimulation (frequency 50 Hz; pulsed width 1 millisecond) was performed. A positive sensory response in the painful area was elicited at a voltage ≤ 0.3 V. Motor testing was done (frequency 2 Hz; pulsed width 1 millisecond; voltage up to 1.2 V) to ensure correct placement of the needle on the DRG. One millilitre of omnipaque contrast was administered in the final AP view to confirm the epidural spread and exclude any intravascular placement (Fig. 2). After negative aspiration, 1 ml of 2% lidocaine with 6.6 mg of dexamethasone was injected. PRF was performed with a pulse width of 20 ms, 42°C at 2 Hz frequency for 2 min. On completion of the procedure, patients were observed in the day surgical unit (DSU) for 2 h. They were discharged home once they had achieved standard discharge criteria for the DSU.
Follow-up
Patients were reviewed in the pain consultant’s outpatient clinic at 6 months and 1 year following the treatment. They were discharged back to their GP’s care at 1 year if pain had not recurred. Pain relief, analgesic consumption and adverse events including infection, nerve injury or unplanned hospital admission following the procedure were enquired about as is standard procedure in the post procedure clinic follow-up review.
Results
Patients who had DRG PRF procedure for cervical radicular pain were included in the audit. Retrospective analysis was completed in 59 patients up to 1-year post procedure. Of the 83 patients recorded in the theatre log as having the procedure, only 59 were contactable by phone despite four attempts to make contact using their hospital-registered details. Demographic data is shown in Table 1. Of the 59 patients, 34 were female and 25 were male. The mean age was 56.6 with a range from 26 to 81. The cervical levels at which the procedure was performed are shown in Table 2. The majority of the patients (93%) had the procedure carried out at C5, C6 and C7 levels.
Of the 59 patients, 49 (83%) experienced some improvement in pain after the intervention and 10 did not (17%). Forty patients of the 59 (67%) experienced a reduction of 50% or more (Fig. 3). Of these 40 patients, 24 had sustained relief of 50% or more at 1 year. This represents 40% of the total patient numbers. The mean duration of pain relief in this group who had a reduction of pain of 50% or more was 37 weeks. Seven out of the 59 patients (11%) had complete resolution of the pain after the intervention with a mean duration of relief of 39 weeks (Fig. 3).
Nine out of 59 patients (15%) had insignificant pain relief of less than 50% following the procedure and continued to rely on other pain medications and were not offered repeat intervention on follow-up in the clinic. Thirty-seven of the 53 (69%) patients who were taking analgesics in the form of anti-inflammatories, anti-convulsants, anti-depressants and opioids prior to the intervention decreased or discontinued analgesic consumption after the intervention. Complications were not specifically sought during the questionnaire but if present were noted from the post procedure clinic review. One patient had a temporary flare up of pain after the procedure which resolved within 2 weeks with simple analgesia. Four patients who failed to respond to the procedure had surgery for the same complaint with an overall crossover rate of 6%.
Discussion
In our study, 67% of patients with chronic cervical radicular pain experienced a clinically significant and meaningful reduction in pain of 50% or more. These results are quite similar to Van Zundert’s initial clinical audit [12] which was followed by a RCT of 42 patients receiving either PRF or sham treatment for chronic cervical radicular pain [13]. In the context of avoiding surgery which is associated with higher morbidity [14] and higher healthcare cost [15, 16], it is possible that PRF adjacent the dorsal root ganglion for chronic cervical radicular pain offers a very viable option to a select group of patients.
The use of epidural dexamethasone would not account for the duration of relief in our study. We used dexamethasone as an adjunct to the PRF treatment. When studied as separate treatments for cervical radicular pain, PRF has consistently given a longer duration of relief than steroids [17, 18]. Combining the treatments could possibly maximize benefit from the treatment but this would require appropriate investigation.
Overuse of strong analgesics has been widely described as problematic on both at societal level and indeed in terms of the individual patients own health risks [19, 20]. Ideally, interventional pain treatments would negate or at least reduce the need for prescription analgesics. In our study out of 53 patients who were taking pain medications prior to the procedure, 37 reduced or discontinued the medications. While we did not note the doses of analgesics each patient was taking, there is an association with reduction of potentially harmful medications in a large portion of the patients included in this study.
The 1-year follow-up time gives reassurance that the symptom reduction associated with this procedure is not just short term. A recent meta-analysis of the effectiveness of pulsed radiofrequency treatment on cervical radicular pain included 4 studies including one RCT, two prospective observational studies and one retrospective study included a total of 67 patients compared with our 59 patients [21]. The evaluation time points in the meta-analysis were up to 6 months. The findings concurred with those of our study that PRF treatment at the DRG for chronic cervical radicular pain was an effective intervention. Of the studies published to date, only one had follow-up at 1 year [18].
Our study of course has limitations. It is a retrospective study with adjuvant active drug and no control group. Also, the exact causative pathology for each patient was not specifically noted for the study.
While the clinical evidence for the effectiveness of DRG PRF treatment continues to build [22], the basic science understanding of potential mechanisms is also expanding. In the treatment of chronic radicular pain, the evidence evolves to imply that the DRG may have a more complex role in persistent pain, rather than simply the compressive effect of a herniated disc or an osteophyte complex on the exiting nerve root [23]. Most of the studies to date are on PRF at the lumbar DRG. The mechanism by which this treatment works is complex and multifactorial. Certainly, there is evidence that an immunomodulatory mechanism of action is at least in part involved [24, 25]. There is a need in the future to simultaneously investigate the mechanism of action of cervical DRG PRF treatment while also ascertaining the clinical benefit in patients with defined cervical pathology.
Conclusion
Our study supports the continued use of pulsed radiofrequency treatment adjacent to the dorsal root ganglion for chronic cervical radicular pain. However, a randomised controlled trial with sham pulsed radiofrequency treatment where both patients and physician are blinded is required. Ideally, this would be a three-group RCT whereby the combination of PRF and adjuvant steroid could be compared against sham PRF and steroid and PRF alone. This, moving forward, would help define the interventional treatment for chronic cervical radicular pain that may yield the greatest benefit.
References
Radhakrishnan K, Litchy WJ, O'Fallon WM, Kurland LT (1994) Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 117 ( Pt 2:325–335
Rhee JM, Yoon T, Riew KD (2007) Cervical radiculopathy. J Am Acad Orthop Surg 15(8):486–494
Côté P, Kristman V, Vidmar M, Van Eerd D, Hogg-Johnson S, Beaton D et al (2008) The prevalence and incidence of work absenteeism involving neck pain. Eur Spine J 17(1):192–198
Côté P, Cassidy JD, Carroll L (1998) The Saskatchewan health and back pain survey: the prevalence of neck pain and related disability in Saskatchewan adults. Spine. 23(15):1689–1698
Manchikanti L, Nampiaparampil DE, Candido KD, Bakshi S, Grider JS, Falco FJ, Sehgal N, Hirsch JA (2015) Do cervical epidural injections provide long-term relief in neck and upper extremity pain? A systematic review. Pain Physician 18(1):39–60
Chao S-C, Lee H-T, Kao T-H, Yang M-Y, Tsuei Y-S, Shen C-C, Tsou HK (2008) Percutaneous pulsed radiofrequency in the treatment of cervical and lumbar radicular pain. Surg Neurol 70(1):59–65
Van Boxem K, de Meij N, Kessels A, Van Kleef M, Van Zundert J (2015) Pulsed radiofrequency for chronic intractable lumbosacral radicular pain: a six-month cohort study. Pain Med 16(6):1155–1162
Munglani R (1999) The longer term effect of pulsed radiofrequency for neuropathic pain. Pain. 80(1–2):437–439
Akbas M, Luleci N, Dere K, Luleci E, Ozdemir U, Toman H (2011) Efficacy of pulsed radiofrequency treatment on the saphenous nerve in patients with chronic knee pain. J Back Musculoskelet Rehabil 24(2):77–82
Manolitsis N, Elahi F (2014) Pulsed radiofrequency for occipital neuralgia. Pain Physician 17(6):E709–E717
Philip CN, Candido KD, Joseph NJ, Crystal GJ (2009) Successful treatment of meralgia paresthetica with pulsed radiofrequency of the lateral femoral cutaneous nerve. Pain Physician 12(5):881–885
Van Zundert J, Lamé IE, de Louw A, Jansen J, Kessels F, Patijn J et al (2003) Percutaneous pulsed radiofrequency treatment of the cervical dorsal root ganglion in the treatment of chronic cervical pain syndromes: a clinical audit. Neuromodulation. 6(1):6–14
Van Zundert J, Patijn J, Kessels A, Lamé I, van Suijlekom H, van Kleef M (2007) Pulsed radiofrequency adjacent to the cervical dorsal root ganglion in chronic cervical radicular pain: a double blind sham controlled randomized clinical trial. Pain. 127(1–2):173–182
Wang MC, Chan L, Maiman DJ, Kreuter W, Deyo RA (2007) Complications and mortality associated with cervical spine surgery for degenerative disease in the United States. Spine. 32(3):342–347
Patil PG, Turner DA, Pietrobon R (2005) National trends in surgical procedures for degenerative cervical spine disease: 1990–2000. Neurosurgery. 57(4):753–758
Salahadin Abdi M, Sukdeb Datta M, Andrea MT (2007) Epidural steroids in the management of chronic spinal pain: a systematic review. Pain Physician 10:185–212
Anderberg L, Annertz M, Persson L, Brandt L, Säveland H (2007) Transforaminal steroid injections for the treatment of cervical radiculopathy: a prospective and randomised study. Eur Spine J 16(3):321–328
Choi GS, Ahn SH, Cho YW, Lee DG (2012) Long-term effect of pulsed radiofrequency on chronic cervical radicular pain refractory to repeated transforaminal epidural steroid injections. Pain Med 13(3):368–375
Nelson LS, Juurlink DN, Perrone J (2015) Addressing the opioid epidemic. JAMA. 314(14):1453–1454
Ray WA, Chung CP, Murray KT, Hall K, Stein CM (2016) Prescription of long-acting opioids and mortality in patients with chronic noncancer pain. JAMA. 315(22):2415–2423
Kwak SG, Lee DG, Chang MC (2018) Effectiveness of pulsed radiofrequency treatment on cervical radicular pain: a meta-analysis. Medicine (Baltimore) 97(31):e11761
Facchini G, Spinnato P, Guglielmi G, Albisinni U, Bazzocchi A (2017) A comprehensive review of pulsed radiofrequency in the treatment of pain associated with different spinal conditions. Br J Radiol 90(1073):20150406
Van Boxem K, Huntoon M, Van Zundert J, Patijn J, van Kleef M, Joosten EA (2014) Pulsed radiofrequency: a review of the basic science as applied to the pathophysiology of radicular pain: a call for clinical translation. Reg Anesth Pain Med 39(2):149–159
Das B, Conroy M, Moore D, Lysaght J, McCrory C (2018) Human dorsal root ganglion pulsed radiofrequency treatment modulates cerebrospinal fluid lymphocytes and neuroinflammatory markers in chronic radicular pain. Brain Behav Immun 70:157–165
Cho HK, Cho YW, Kim EH, Sluijter ME, Hwang SJ, Ahn SH (2013) Changes in pain behavior and glial activation in the spinal dorsal horn after pulsed radiofrequency current administration to the dorsal root ganglion in a rat model of lumbar disc herniation: laboratory investigation. J Neurosurg Spine 19(2):256–263
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Ethical approval for this study was granted by the SJH/AMNCH Joint Research and Ethics Committee which operates in compliance with the European Communities Regulations 2004 and ICH GCP guidelines. (Ref: 2017-11-Chairman’s Action [12]).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
O’Gara, A., Leahy, A., McCrory, C. et al. Dorsal root ganglion pulsed radiofrequency treatment for chronic cervical radicular pain: a retrospective review of outcomes in fifty-nine cases. Ir J Med Sci 189, 299–303 (2020). https://doi.org/10.1007/s11845-019-02087-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-019-02087-4