Abstract
Introduction
Emergency laparotomy (EL) is a commonly performed operation with increased morbidity and mortality. Currently, there is a lack of published outcomes following emergency laparotomy within an Irish population. The aim of this study was to assess our outcomes and compare these to predefined outcomes from NELA.
Methods
A review of a prospectively maintained database of all patients who underwent an emergency laparotomy between January 1st 2015 and October 31st 2016 was performed. Patient demographics, operative indication and procedures, preoperative lactate, time of surgery, admission to high dependency unit (HDU) and mortality (30- and 90-day mortality) were included. Statistical analysis was performed using Minitab V18 with p < 0.05 considered significant.
Results
One hundred twenty-four emergency operations were performed on 120 patients. The median age was 60 years. Indications for surgery included the following (%): peritonitis (32.45%), obstruction (22.5%), complicated hernia (19.1%), mesenteric ischaemia (15%), trauma (4.1%), and acute haemorrhage (3.3%). A consultant surgeon and consultant anaesthetist were present at 79 and 78% of EL carried out, respectively. Reported 30- and 90-day mortality were 6.66 and 11.6%, respectively. Thirty-day mortality was 20% in octogenarians. Index lactate did not correlate with mortality (p = 0.43). A significant proportion of mortalities had procedures carried out between 6 pm and midnight with the highest mortality rate in patients with mesenteric ischaemia (p < 0.05).
Conclusion
EL is associated with high mortality rates. Our mortality figures compare favourably with the NELA data. We support the development of a national database to facilitate improvements in the quality of care delivered to this high-risk cohort.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The acute abdomen remains the most frequent indication for acute surgical admission in the nontrauma patient [1]. Emergency laparotomy (EL) describes an exploratory procedure where the clinical presentation, pathology and perioperative management vary considerably. Over 30,000 EL are performed in the UK per annum [2]. Despite this large number, there is an unsatisfactory standard of care for this cohort of patients [1]. In Ireland, over a 3-year period between 2011 and December 2013, there were 19,000 emergency laparotomies performed [3]. There has been limited focus upon introducing and establishing surgical care pathways to improve outcomes in this cohort of critically ill patients with high predicted morbidity and mortality rates. In 2007, the Association of Surgeons in Great Britain and Ireland (ASGBI) identified unsatisfactory outcomes and prepared a strategic document for improvement of provision of care and services in this subset of patients [1]. The National Emergency laparotomy Audit (NELA) was commissioned in 2011 and aimed to highlight the interhospital variations in outcomes and to standardise the perioperative and postoperative management of these patients [4].
According to the 2016 population census, Ireland like many European countries has an ageing population [5]. 19.1% of the population are now over the age of 65 years [3]. While the term ‘elderly’ has not been universally defined, specialists in medicine for the elderly in Ireland generally consider those aged over 70 as elderly. This is also reflected in the NELA project guidelines [4]. Poor outcomes in octogenarians following emergency surgery are well documented. In 2010, the National Confidential Enquiry into Patient Outcomes and Death (NCEPOD) reported 30-day mortality was 31.2% for octogenarians undergoing abdominal surgery; 83.4% of cases were emergencies [6]. The severity of coexisting comorbidities inherently adds to the complexity of both the perioperative and postoperative care leaving them vulnerable to significant postoperative morbidity. Elderly patients account for 43% of emergency surgeries in hospitals and the associated poor outcomes need to be addressed [7]. Recently, some of the recommendations outlined in the NELA report have been investigated in prospective studies [8, 9]. Perioperative initiatives (care bundles) have reduced mortality in this group of patients [8, 9].
The aim of the current study was to compare our institutional EL data with the NELA datapoints, including key recommendations from the first published report and international published data.
Methods
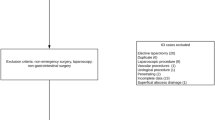
A prospectively maintained emergency laparotomy database was created in December 2014 in conjunction with establishing an emergency surgery signout document. This study included all patients who underwent an EL between the 1st of January 2015 and the 31st of October 2016 in Tallaght Hospital (a university teaching hospital which admits approximately 2500 acute surgical patients annually within a network model of care); analysis was then performed. To ensure all patients were captured in the database during the study period, a further search was performed using the hospital inpatient enquiry (HIPE) and the inpatient manager system (IPM) using the search term ‘exploratory lap*’ and ‘emergency lap*’ to generate a report. This group was then cross-referenced with the database, electronic general surgical theatre log books to validate our records. All manual theatre logbooks were interrogated separately.
Inclusion criteria:
-
Patients older than 18 years
-
Patients who underwent an expedited, urgent or emergency abdominal procedure involving the gastrointestinal tract (GIT)
-
All open, laparoscopic or laparoscopically assisted procedures
-
Procedures involving the stomach, small or large bowel or rectum
-
Procedures were grouped into categories: obstruction, peritonitis (defined as peritonitis due to a perforated viscus), mesenteric ischaemia, etc.
-
Patients who underwent an emergency abdominal surgery for trauma
The list of procedures included was cross-referenced against the scope of the NELA inclusion criteria.
Exclusion criteria:
-
Patients younger than 18
-
Elective abdominal procedures
-
Any procedures involving the oesophagus, the biliary tree, the kidneys, and pancreas
-
Abdominal aortic aneurysm rupture
Demographic features including age and sex were recorded. Operative indication and procedure were recorded and then subdivided into predefined categories. Preoperative or perioperative lactate and preoperative imaging were recorded. Specific documentation of time of admission, time booked on emergency list and of induction of anaesthesia was recorded. Patients admitted to a high-dependency unit (HDU) bed postoperatively, and mortality rates were also included. Seniority of staff present at an operation was recorded from the inpatient manager databases and cross-referenced with theatre logbooks. An electronically circulated ‘surgical signout’, a typed document that is emailed at 7 am to all members of the general surgical teams, including all consultant general surgeons, was also interrogated [10].
Timing of surgery was defined as the logged time of induction of anaesthesia using the centricity software. Patients were recorded as being admitted to HDU if they went to the intensive care unit (ICU) or the postoperative acute care unit (PACU); otherwise, they were recorded as a general surgery ward admission. All patients admitted to HDU had acute physiology and chronic health evaluation II (APACHE II) scores recorded. APACHE II is designed to measure the severity of disease in patients admitted to the ICU. Total mortality in the cohort within the study period, 30-day mortality and 90-day mortality as well as cause of death were also recorded. This was retrieved from medical notes and also by interrogation of the register of deaths within the hospital.
Statistical analysis was performed using Microsoft Excel program and Minitab-V18 with a p value of less than 0.05 (p < 0.05) considered significant. Comparison of outcomes between two groups was performed using paired t test and one-way ANOVA was used to analyse the means of three or more factors within the study. Finally, univariate and multivariate analysis was performed to examine the impact of one or multiple factors on outcome.
Results
The study consisted of 124 operations on 120 patients. These included 63 males and 57 females, with median age 60 years (18–87, Table 1a). The most common operative indications included the following (%): peritonitis (32.5%), obstruction (22.5%), complicated hernia (19.1%), ischaemia (15%), trauma (4.1%), bleeding (3.3%) and missing data 3.3% (Table 1b).
Over half of the patients (55.8%) had preoperative computed tomography (CT) within 24 h of undergoing their operative procedure. Twenty-eight percent were within 6 h of surgery and on the day of admission to hospital. A further 17% of those who did not have a CT had a plain film X-ray displaying evidence of acute abdominal pathology. Most procedures took place between 7 am and 6 pm (54%). A significant number of mortalities underwent operative procedures carried out between 6 pm and midnight (p < 0.05). Preoperative or perioperative lactate was available in 109 patients (Table 2). Sixty-six percent of patients had an elevated lactate; however, index serum lactate measured on admission did not correlate with mortality (p = 0.43). Patients admitted to a HDU bed postoperatively all had Apache II scores on admission. The mean Apache II score for ICU admissions was 20.3 [range 7–29] and HDU admissions 13.59 [4–26].
Consultant surgeon and anaesthetic presence was 79 and 71%, respectively (Table 3). The presence of both consultant surgeon and consultant anaesthetist was highest from 08:00 to 23:59. Attendance was less after 00:00; however, this did not impact on overall 30-day mortality. One patient who was operated on after 00.00 during the study period died within 90 days. The consultant surgeon was present for this operation.
Factors associated with mortality were examined. Patient sex, age, index lactate and seniority presence were not associated with overall patient mortality (p = 0.37, p = 0.54, p = 0.43, p = 0.12, respectively). Patients that underwent laparotomy between 18:00 and 23:59 and those diagnosed with acute mesenteric ischaemia (AMI) as the primary indication had significantly higher 30-day mortality rates (p < 0.05, Table 4).
Equal numbers of patients were managed in an ICU/ HDU and ward setting postoperatively.
Thirty-day mortality was 6.66% (n = 8) and 90-day mortality was 11.6%. Ischaemia was the most common indication (50%) for surgery in the 30-day mortality group, and the level of operator was not statistically significant (p = 0.12). Eighty-three percent of the 90-day mortality operations were performed by a consultant surgeon. Fifty percent were performed during the daytime. Octogenarians had an overall 30-day mortality of 20%. Fifty percent of mortalities were managed in HDU postoperatively. Fifty percent of the 30-day mortality group were already being managed in ICU preoperatively, and all had Apache II scores above 22 which is associated with mortality as high as 40%.
Discussion
Internationally, there are poor reported outcomes in emergency abdominal surgery [2].
In 2007, the ASGBI acknowledged that standards of care for emergency surgical admissions were often unsatisfactory and needed to be addressed [1]. The NELA was one of the first prospective studies examining directly the variations in outcomes across the UK in an attempt to improve and achieve a common ‘gold’ standard. The factors influencing poor outcomes are diverse and can be divided into patient factors and system factors. The cohort of patients admitted acutely and requiring an emergency operation varies in age, comorbidities and diagnosis. The framework to deliver acute surgical care can often be limited by infrastructure, resources, senior clinical input and leadership within it [3]. In Ireland, we have begun to address the framework within which we deliver acute surgical care. In 2013, we began addressing the Irish framework with a comprehensive document ‘Model of care for acute surgery’ [3]. More recently, in 2016, a critical surgical abdomen consensus conference published a paper addressing performance quality and outcomes for acute surgical care [11]. Key performance indicators (KPI) were identified to allow continued evaluation of existing policies and resources to ensure optimal care of the emergency surgical patient going forward.
However, in Ireland, there is currently no ongoing audit analysing mortality after EL; furthermore, very few single centres are reporting their EL mortality data. Given this, the aim of this study was to audit the outcomes, specifically mortality in the EL cohort of patients in a single Irish general surgical centre with the knowledge that this is a diverse cohort undergoing emergent and individually specified procedures that carry higher mortality than elective operations [13].
As described in the first report by the NELA, the umbrella term ‘EL’ can include over 400 operations, contributing to the difficulty in identifying and capturing all procedures in our centre for analysis [1]. Data collated for this study was recorded by cross referencing hospital inpatient enquiry (HIPE) databases, theatre online data portals coding for ‘EL’ and handwritten general surgical theatre logbooks. The ‘surgical signout’ as previously described was invaluable to ensure all EL’s were captured [10]. Ideally, a national database similar to NELA should be in place and run through the National Office of Clinical Audit [12].
Early identification of acute intra-abdominal sepsis and early implementation of care bundles are recommended by NELA [1]. The arterial blood lactate level is an indicator of circulatory and cellular oxygen metabolism and is used as diagnostic criterion of sepsis for evaluating the level of tissue perfusion. While studies in critical care patients have shown lactate to be an independent risk factor for mortality, in the emergency laparotomy cohort, specifically AMI [13], it did not correlate with the severity of ischaemia or mortality [14,15,16,17]. Furthermore, a systematic review examining lactate as a predictor of in-hospital mortality concluded that while lactate is useful for risk assessment of acutely ill patients admitted to hospital, there may be more value in serial measurements or prolonged time to normalise lactate for predicting mortality [15].
In the current study, preoperative or perioperative lactate did not correlate with overall mortality. While higher lactates have been reported as independent factors in surgical decision-making [16], it is not specific to all acute abdomen diagnoses as evidenced by the fact that 45.8% of our patients had a normal lactate.
The 2011 NCEPOD report found delays in 20% of nonelective procedures getting to the operating theatre [18]. Fifty-four percent of EL in our centre occurred during daytime hours and following CT imaging. A significant proportion of mortalities had procedures between 6 pm and midnight (p < 0.05). This reflects data showing poorer outcomes for patients operated on after normal working hours [20]. The indication for surgery, patient comorbidities and time for resuscitation may influence the risk of operative delay and adverse outcomes. Furthermore, due to many confounders, it is challenging to ascertain if a delay in some aspect of care has occurred or influenced outcome. An observational study looking at this found that delayed access to operating rooms for emergency surgery was associated with increased mortality risk and longer length of stay [18]. We acknowledge that we have not ascertained all the confounders that may have been involved namely due to difficulty in accurately collecting this data. The NCEPOD has continuously recommended that emergency surgical patients should have prompt access to radiology, theatres, critical care facilities and senior level trained staff [19,20,21]. It is consistently felt that the entire bundle of components is essential rather than one aspect carrying disproportionate value. High-risk patients anaesthetised or operated on outside normal working hours by nonconsultant trainees have a poorer outcome [21], however, the level of operator did not result in higher mortality in this study.
The NELA recommendations included admission of ‘high-risk’ patients to a HDU postoperatively. Fifty percent of our 30-day mortality patients were managed in either ICU or HDU. Documentation of risk of mortality is important to ensure high-risk patients are prioritised in admission to a HDU bed. Elderly patients and patients with a preoperative mortality risk of over 10% should be managed in HDU [1]. We did not see percentage quantification of perioperative mortality risk documented within the audit period in our institution. Our cohort is a heterogeneous group of patients of varying age, complexity and sickness-severity, similar to the NELA group. Our overall 30-day mortality figures are favourable at 6.66% when compared with the 14.9% overall mortality in the NELA study [2]. Mortality among octogenarians was unsurprisingly higher at 20% and confirms the challenge surgeons face to achieve better outcomes in the elderly with multiple medical comorbidities, reduced physiological reserve that tolerate anaesthetic/surgical insult poorly. It has been estimated that up to 15% of people over the age of 80 are ‘frail’. Frailty can be suspected in those with an obvious lack of reserve, unintentional weight loss, exhaustion, slow walking and low daily physical activity [22]. It is paramount that this cohort also received input early from medicine for the elderly to avoid morbidities and mortalities following surgery. The recently published third NELA report figures remain low for the involvement of geriatricians within this cohort [23]; in our institution involvement was 0% and needs to be addressed. Age has been shown to be an independent predictor of mortality [24].
Although the adherence to use of goal-directed fluid therapy (GDFT) and early antibiotic administration was not directly reviewed within the scope of this study due to limitations in accurately collecting this data, the sepsis six care bundle is in widespread use within our institution with high rates of observed compliance. There are limitations to this single centre study. Firstly, our cohort number is small but acceptable for the study period. Secondly, we acknowledge that there are many confounders that make it difficult to ascertain where true delays occurred in timing of surgery, and the necessity for improvements in documentation has been highlighted. To our knowledge, it is the first EL data reported from Ireland.
We hope this study highlights the need for an Irish prospective emergency laparotomy database and the importance of prospective risk assessments for individual patients requiring EL.
Conclusion
Emergency laparotomy is associated with high mortality rates. Our figures are favourable when compared to the international standards; however, as proposed by the NELA study, the introduction of a care bundle may further improve early and late mortality rates. We feel that it has been an important step in prioritising higher levels of care for these surgical patients and identifying areas for future improvement and collaboration of departments to achieve a higher standard in our institution. Our overall 6.66% 30-day mortality is a snapshot of EL procedures carried out in one Irish institution. We would advocate for implementation of an EL care bundle to include dedicated CT scanning, perioperative checklist for triaging abdominal sepsis (early warning score/GDFT/antibiotics), and introduction of a dedicated emergency theatre to avoid operative delays. We also advocate for a national EL database to address mortality after EL.
References
Association of Surgeons of Great Britain and Ireland (2007) Emergency general surgery: the future—a consensus statement. ASGBI, London
Saunders DI, Murray D, Pichel AC, Varley S, Peden CJ (2012) Variations in mortality after emergency laparotomy: the first report of the UK Emergency Laparotomy Network. Br J Anaesth (England) 109(3):368–375. https://doi.org/10.1093/bja/aes165
Model of care for acute surgery 2013, National Clinical Programme in Surgery. Joint leads Professor Frank Keane, Mr. Ken Mealy. Published 2013
NELA (2015) The first patient report of the national emergency laparotomy audit. Royal College of Anaesthetists, London
Central Statistics Office (CSO) (2016) Census of population 2016—profile 3 an age profile of Ireland http://www.cso.ie/en/release and publications/ep/p-cp3oy/cp3: CSO
National Confidential Enquiry into Patient Outcome and Death (NCEPOD) (2010) An age old problem: a review of the care received by elderly patients undergoing surgery. www.nce pod.org.uk/2010report3/downloads/EESE_fullReport.pdf: NCE- POD; 2010
Sharrock AE, McLachlan J, Chambers R, Bailey IS, Kirkby-Bott J (2017) Emergency abdominal surgery in the elderly: can we predict mortality? World J Surg 41(2):402–409. https://doi.org/10.1007/s00268-016-3751-3
Quiney N, Huddart S, Peden C, Dickinson M (2015 Jun) Use of a care bundle to reduce mortality following emergency laparotomy. Br J Hosp Med (Lond) 76(6):358–362. https://doi.org/10.12968/hmed.2015.76.6.358
Huddart S1, Peden CJ, Swart M, McCormick B, Dickinson M, Mohammed MA, Quiney N, ELPQuiC Collaborator Group, ELPQuiC Collaborator Group (2015) Use of a pathway quality improvement care bundle to reduce mortality after emergency laparotomy. Br J Surg 102(1):57–66
Gibbons JP, Nugent E, Tierney S, Kavanagh D (2016 Feb) Implementation of a surgical handover tool in a busy tertiary referral centre: a complete audit cycle. Ir J Med Sci 185(1):225–229. https://doi.org/10.1007/s11845-015-1278-5
Emergency surgery performance and quality outcome consensus summit, Donegal Ireland 2016, Sugrue M, Maier R
National office of clinical audit. www.NOCA.ie . 2015
Studer P, Vaucher A, Candinas D, Schnüriger B (2015) The value of serial serum lactate measurements in predicting the extent of ischemic bowel and outcome of patients suffering acute mesenteric ischemia. J Gastrointest Surg 19(4):751–755. https://doi.org/10.1007/s11605-015-2752-0
Demir IE, Ceyhan GO, Friess H (2012) Beyond lactate: is there a role for serum lactate measurement in diagnosing acute mesenteric ischemia. Dig Surg 29(3):226–235. https://doi.org/10.1159/000338086
Kruse O, Grunnet N, Barfod C (2011) Blood lactate as a predictor for in-hospital mortality in patients admitted acutely to hospital: a systematic review. Scand J Trauma Resusc Emerg Med 19:74
Verma I, Kaur S, Goyal S, Goyal S, Multani JS, Narang APS (2014 Jul) Diagnostic value of lactate levels in acute abdomen disorders. Indian J Clin Biochem 29(3):382–385
Buck N, Devlin HB, Lunn JN (1988) Report by the national confidential enquiry into perioperative deaths. Nuffield Provincial Hospitals Trust, London
McIsaac DI, Abdulla K, Yang H, Sundaresan S, Doering P, Vaswani SG, Thavorn K, Forster AJ (2017 Jul 10) Association of delay of urgent or emergency surgery with mortality and use of health care resources: a propensity score-matched observational cohort study. CMAJ 189(27):E905–E912. https://doi.org/10.1503/cmaj.160576
Campling EA, Devlin HB, Lunn JN. The report of the National Confidential Enquiry into Perioperative Deaths 1989. NCEPOD, London 1990 (see: www.ncepod.org.uk/)
Campling EA et al. The report of the National Confidential Enquiry into Perioperative Deaths 1992/1993. NCEPOD, London 1995 (see: www.ncepod.org.uk/)
Buck N, Devlin HB, Lunn JN (1988) Report by the National Confidential Enquiry into Perioperative Deaths. Nuffield Provincial Hospitals Trust, London
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56(3):M146–M156. https://doi.org/10.1093/gerona/56.3.M146
The third patient report of the national emergency laparotomy audit October 2017. http://www.nela.org.uk/reports
Cook TM, Day CJE (1998) Hospital mortality after urgent and emergency laparotomy in patients aged 65 and over. Risk and prediction of risk using multiple logistical regression analysis. Br J Anaesth 80(6):776–781. https://doi.org/10.1093/bja/80.6.776
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kiernan, A.C., Waters, P.S., Tierney, S. et al. Mortality rates of patients undergoing emergency laparotomy in an Irish university teaching hospital. Ir J Med Sci 187, 1039–1044 (2018). https://doi.org/10.1007/s11845-018-1759-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-018-1759-4