Abstract
Background
With concerns that blind registration in Ireland due to diabetic retinopathy is continuing to rise, a structured retinopathy screening service is in the process of being rolled out nationally.
Aims
To report on the validation process for creating a register of diabetics in the Mid-West of Ireland, and findings following retinopathy screening of a representative sample.
Methods
National primary care databases were employed in generating provisional lists of diabetic patients in the Health Service Executive (HSE) Mid-West area. Subsequent engagement with the corresponding general practices over a three year period between 2010 and 2013 facilitated the validation of these lists. A summary of the retinopathy screening outcomes of 1,434 patients and pre-existing screening patterns is reported.
Results
The number of patients on the Mid-West diabetes register to date is 11,126. Of the 1,434 patients screened, 288 (20.1 %) had background retinopathy, while 117 (8.2 %) had sight-threatening retinopathy. Seventeen (19.8 %) of the 86 patients identified with maculopathy required treatment with intravitreal injections. Of the 610 patients questioned about previous screening events, 389 (63.8 %) said they had undergone an ocular examination within the previous 12 months.
Conclusions
The HSE Mid-West has over 11,000 patients on its database ready to be screened by the national programme, with the treatment of maculopathy expected to have the largest impact on resources. Although the majority of patients are already undergoing screening in the community in an ad hoc fashion, the rates of sight-threatening retinopathy encountered highlight the timeliness of the full implementation of the national programme.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetes is a chronic multisystem disease associated with microvasculature complications such as diabetic retinopathy (DR), where there is microangiopathy of the retinal circulation. It has been estimated that there are 382 million people worldwide with diabetes [1], over 90 million of whom have DR [2]. In Ireland, between 1996 and 2003, there was a 120 % increase in blind registration due to DR from 147 to 323 cases, and it is a leading cause of blindness in the 16–65 age group [3]. As this trend is expected to continue, its impact on individuals, particularly those of working age, is likely to increase over the coming years from both an economic and quality of life perspective. The direct financial cost of vision impairment and blindness to the health care system in Ireland has been estimated to be €117 million in 2010, with indirect costs to the state and society estimated at €269 million [4]. The cost-effectiveness and benefits of a structured screening programme are well documented, as laser treatment can significantly reduce the risk of blindness [5].
One of the key initial steps in facilitating a structured screening programme is accurate case identification and collection onto a database, which also provides useful epidemiological data to help inform health policy planning, management and funding of public health programmes. This is especially important in the context of expected increases in diabetes prevalence rates from the current worldwide estimate of 8.2 % of adults, and the corresponding impact on global health expenditure which was at least USD 548 billion in 2013 [1]. It has been estimated that, by 2015, the number of adults with diabetes in Ireland will reach approximately 193,000, equating to 5.2 % of the adult population [6]. There is a lack of worldwide data on the prevalence of DR [1], and published epidemiological data regarding DR may be outdated, with changes in therapeutic options available for managing diabetes possibly reducing complication rates [7]. Consequently, accurate data on the prevalence of DR in the Irish population rather than extrapolation of data from other countries is desirable.
In 2010, as part of the framework for the development of a national service [8], the Health Service Executive (HSE) set up the Mid-West Diabetic Retinopathy Screening Programme (MWDRS). The main objectives were to create a database registering the area’s diabetic population, and to offer local retinopathy screening clinics throughout the Mid-West. Subsequently, the National Screening Service (NSS) was tasked with the development of a comprehensive diabetes register for Ireland with a view to implementing the national, quality assured retinopathy screening service, ‘Diabetic RetinaScreen’. In this paper, we report on the processes and issues surrounding the setting up of the Mid-West database, the pre-existing system of screening in the region, the rates of diabetes and retinopathy in the area, and the resultant treatment workload.
Materials and methods
To generate the initial diabetic client list, a pilot study was undertaken to identify possible clients through a combination of Primary Care Re-imbursement Service (PCRS) sources [Medical Card Prescriptions (MCP) and Long Term Illness (LTI) Scheme], Hospital In-Patient Enquiry (HIPE) scheme, Patient Administration System (PAS), and Laboratory Information System (LIS) sources. A composite list for a sample of general practitioners (GPs) was then cross-referenced with the GPs’ own information systems to confirm the diabetic status of each patient on the list, and was found to be approximately 60 % accurate. It was concluded that the most comprehensive and accurate lists were generated through MCP and LTI sources. These lists were transferred to a specially commissioned secure electronic database which could be updated with the relevant demographic and clinical data, and was used in the larger study involving the remaining GPs with practices in the HSE Mid-West.
Over a three-year period commencing January 2010, 139 practices in the Mid-West with GPs holding General Medical Services (GMS) contracts were contacted to partake in the database process. This entailed a visit to each practice, so that every patient on the provisional list could be validated in terms of their diabetes status (patients under the age of 12 or who had gestational diabetes were excluded). Private practices were also contacted in a similar process. Any additional patients not on the provisional list that were identified through the practices’ clinical software were added. Registration forms were left in each practice, so that patients (including newly diagnosed diabetic patients) could be added to the database prospectively.
Using these validated lists, retinopathy screening clinics were set up in a number of health centres throughout the Mid-West, with appointments offered to a cohort which reflected a wide geographic spread, and included a mixture of urban and rural areas, namely: County Limerick, Limerick City, County Clare, and Tipperary North. All 1,434 patients who attended screening underwent a dilated ocular examination performed by a single ophthalmologist (MJ) primarily with slit lamp biomicroscopy, or indirect and direct ophthalmoscopy in cases of poor patient mobility. No patient was screened with retinal photography. Every patient who attended screening gave informed consent for recording of their clinical details for research and teaching purposes, and the study adhered to the tenets of the Declaration of Helsinki. In a prospective study, the results of all screening outcomes over a 2 year period from June 2010 to June 2012 were collated.
Data was prospectively entered onto the Mid-West diabetes database. This included demographic details such as age, gender, type and duration of diabetes, as well as ocular data such as visual acuity, presence of non-diabetic ocular pathology, and retinopathy grade. The grading classification of the national screening programme in England and Wales was adopted, where patients are given a retinopathy (R0-3) and maculopathy (M0-1) grade; patients with pre-proliferative (R2), proliferative (R3), or maculopathy (M1) grades were classed as having sight-threatening DR [9]. To investigate the pre-existing screening patterns which were in place prior to the setting up of our community clinics, a proportion of the study patients with a diagnosis of diabetes of at least 12 months were also asked when and with whom their last ophthalmic exam took place. The data were analysed using a statistical software package (Stata, StataCorp, College Station, TX).
Results
Of the 139 general practices located in the HSE Mid-West area within the GMS scheme, 132 (95 %) agreed to be involved in the validation process. Seven (5 %) practices were either unwilling or unable to partake. Of the 24 exclusively private GPs registered in the area, 16 (66.7 %) were included in the validation process. As of February 2014, the total number of diabetics attending practices within the HSE Mid-West which have been entered onto the diabetes database from these validated lists is 11,126, of whom 11,006 were aged 20 years and over, accounting for 4 % of the local adult population. Up to 40 % of these clients were identified outside PCRS sources following additions from GPs either on the day the practices were visited to validate the list, or subsequently though the use of referral forms. Demographic data of all known diabetic patients in the HSE Mid-West area are shown in Table 1.
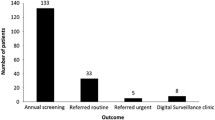
Of the 1,943 patients who were offered screening during the study period, 1,434 (73.8 %) attended, with demographic data summarized in Table 2. Variables associated with poorer attendance rates at screening clinics which were highly statistically significant (p < 0.01) included age less than 35 years and clients from Limerick City (p < 0.0001) and County Clare (p < 0.005). Of those who attended, 14 (1.0 %) were deemed ungradable due to media opacity obscuring the fundal view, 1,015 (70.9 %) had no retinopathy (R0M0), 288 (20.1 %) had background retinopathy only (R1M0), while 117 (8.2 %) had sight-threatening retinopathy (Table 3). There was a statistically significant association between type of diabetes and grade of retinopathy (p < 0.0001), with 32 (28.3 %) of type I diabetics having sight-threatening retinopathy versus 85 (6.4 %) of type II diabetics (Fig. 1). Type II diabetics requiring insulin were also more likely to have more severe grades of retinopathy compared to non-insulin dependent diabetics (24.3 % versus 4.8 %, p < 0.0001). There was no statistically significant difference in grade of retinopathy between the different areas.
Twenty-eight (2 %) patients were identified with proliferative diabetic retinopathy, of whom 25 (89.3 %) had already undergone panretinal photocoagulation therapy in the past (Fig. 2). Nine (36 %) of those previously treated were deemed to have unstable disease, and were listed for further treatment. Of all patients screened, there were only three (0.2 %) patients who were newly diagnosed with proliferative diabetic retinopathy. Eighty-six (6 %) patients were diagnosed with diabetic maculopathy; of these, 35 (40.7 %) had already been treated with laser in the past, while 32 (37.2 %) were deemed to have clinically significant macular oedema requiring treatment (Fig. 2). In total, 17 (19.8 %) of those with maculopathy required treatment with intravitreal therapy, 16 (94.1 %) of whom received anti-vascular endothelial growth factor (VEGF) injections either on their own or combined with laser, while one (5.9 %) patient was treated with intravitreal steroid. Excluding diabetic retinopathy, newly diagnosed ocular pathology requiring further management was identified in 42 (2.9 %) of those screened, the details of which are shown in Table 4.
Management outcomes of those screened who were graded as having sight-threatening diabetic retinopathy. R0 no retinopathy, R1 background retinopathy, R2 pre-proliferative retinopathy, R3 proliferative retinopathy, M0 no maculopathy, M1 maculopathy, CSMO clinically significant macular oedema, PRP panretinal photocoagulation, VEGF vascular endothelial growth factor
Data from 610 patients who were questioned regarding their previous screening experience are outlined in Table 5. Overall, the mean (±SD) age of those questioned was 64.7 (±13.2) years, with no statistically significant differences with respect to location of the screening clinics. The median (interquartile range) duration since their last ocular examination was 1 (0.5–2) year. This was with an ophthalmologist in 266 (43.6 %) cases, and an optometrist or optician in 332 (54.4 %). Twelve (2 %) denied having attended an eye specialist since their diabetes diagnosis. There were 384 (63 %) who had undergone an ocular examination within the previous 12 months, and 530 (86.9 %) within the previous 2 years. There were six (1 %) patients who said it had been more than 5 years since their last visit to an eye specialist. There was a significantly greater proportion of clients from urban areas screened within 12 months compared to rural clinics (68 % versus 60 % respectively, p = 0.043), and in particular, those from County Limerick were significantly less likely to be screened within this timeframe compared to County Clare (55.9 versus 75.4 % respectively, p = 0.005). Patients aged 65 years or over were more likely to have been screened within the preceding 12 months than those in the 50–64 age group (p = 0.032), while there were no statistically significant differences found between the other age groups.
Discussion
Although it has been estimated that, by 2015, diabetes will affect 5.2 % of the adult population in the Republic of Ireland [6], this prevalence rate is lower than the most recent figure of 6.47 % quoted for Ireland from the International Diabetes Federation [1]. However, this 6.47 % estimate was based on extrapolation of rates from similar countries, thus highlighting the importance of developing a diabetes database from which accurate prevalence rates can be calculated. The 11,006 individuals aged 20 years and over on the Mid-West diabetes database (4 % of the adult population in the region) is an underestimate due to under-ascertainment with significant numbers remaining undiagnosed or unregistered. With this caveat in mind, information arising from the database is still useful in terms of health service resource planning and assisting GPs managing their own diabetic lists; we found only one practice in the Mid-West which had a pre-existing complete list of diabetic patients which we could not add to through the validation process. Additionally, the completion of the Mid-West diabetes register is an important step in enabling the ‘Diabetic RetinaScreen’ programme achieve its aims of offering screening to 100 % of the known diabetic population of Ireland by the end of 2014.
Data linked to PCRS generated large numbers of potential clients for our database and were generally accurate. Numbers arising from HIPE data were small, and LIS data containing HbA1c levels were particularly inaccurate at identifying true diabetics, hampered by the lack of unique patient identifier numbers, and therefore not recommended for populating lists. Data from MCP and LTI together with a validation process involving GPs may be able to generate a database which identifies 83 % of true diabetics [10]. Further addition of newly diagnosed patients via GP referrals and patients not on health-related schemes should help towards identifying 90 % of all diabetics which is the minimum required for a database to be considered complete [8]. The national database will be populated using similar methods to that employed in this study, and, therefore, will also need the engagement of GPs to ensure accuracy and completeness of the register. However, the time and resources required to visit individual GPs as was done during this study would not be practical on a national level, necessitating the use of other methods such as patient and GP education through media campaigns.
The overall prevalence of any DR in our study of 28.3 % is within the range expected from published global prevalence estimates [2, 11], and similar to the 25.6 and 28 % rates found in primary care-based screening initiatives in Ireland and the United Kingdom (UK) respectively [12, 13]. Higher retinopathy rates have been reported in other population based studies in the UK, but this is likely due to differences in the study populations, either in terms of a greater proportion of patients who are insulin-dependent or of Asian ethnicity [14, 15]. The overall prevalence of potentially sight-threatening eye disease in our cohort was similar to retinopathy screening studies in Cork, Liverpool, Scotland, and London (8.2 versus 6.5, 7.1, 7, and 7.1 % respectively) [12, 13, 16, 17]. In keeping with the findings of similar studies elsewhere, the majority of referable retinopathy cases we encountered had maculopathy [13, 17]. With the increasing use of anti-VEGF therapy in the management of these cases, each receiving, on average, seven injections during the first year of treatment [18], maculopathy will undoubtedly place the heaviest burden on hospital eye services. However, just under 20 % of those with maculopathy in our study underwent intravitreal therapy, the remainder requiring either laser therapy or close monitoring. It is also likely that, in the absence of a structured screening programme, these maculopathy cases would have eventually presented to the treatment centres anyway, but at a more advanced and symptomatic stage, with an increased likelihood of requiring anti-VEGF therapy rather than focal laser.
There were only three new cases of proliferative DR identified during our screening process, with the other 25 proliferative cases having already received treatment in the past. This suggests that the majority of patients in the HSE Mid-West with sight-threatening disease may already have been identified and treated by local ophthalmology services, despite the absence of a structured screening service in the region to date. From a workload perspective, it is also reassuring to note that these rates of referable retinopathy are for the first screening round of a new programme, and are likely to decline over time as there should be a trend toward lower rates by the second and subsequent rounds of screening [17]. However, while the rates of referrals requiring laser treatment may eventually decline [19], this effect may be countered by the ever increasing number of diabetic patients in the community requiring screening [20]. It is hoped that a structured retinal screening programme will at least allow for more appropriate use of hospital-based ophthalmology resources [21], with improved access for those with referable retinopathy facilitated by the freeing up of hospital clinic space through the discharge of the majority of patients with no or background retinopathy to screening in the community [22]. Out of the 1,434 patients involved in the MWDRS, 36 underwent treatment for retinopathy associated with a high risk of severe visual loss, and are now unlikely to go blind.
Newly diagnosed ocular pathology (i.e. not already being managed by ophthalmology services) other than DR which warranted further work-up was identified in approximately 3 % of patients attending screening. This rate indicates the additional workload the general eye clinics of treatment centres may expect to receive from their screening programme clinics. It is hoped that the transfer of routine retinopathy screening cases out of these general clinics to the national screening programme will allow for timely assessment of those newly diagnosed with ocular pathology, but resources dedicated to the management of referrals from the national programme are still vital.
In 2010, the financial cost of vision impairment in Ireland was estimated to be €386 million incurred by 224,832 people. With an expected increase in visual impairment rates of 20 % over the following decade, this cost is expected to rise to €449 million by 2020 [4]. The impact of a screening programme on the diabetic population who are identified with sight-threatening disease requiring treatment is that 6 % of them will be prevented from going blind within a year of treatment and 34 % within 10 years of treatment [5]. Besides the obvious dramatic effect this has in terms of maintaining quality of life for patients, it also eases the considerable financial burden associated with diabetes-related blindness, and such screening programmes are far more cost-effective than those of other commonly provided medical interventions [23].
Our screening attendance rate of 73.8 % of eligible persons is just above the proposed minimum standard of 70 % [8]. There are a number of predictors of poor attendance at screening events such as social deprivation, young age, poor risk factor control, and long duration of diabetes [24]. Attendance rates in our clinics were poorer for those less than 35 years of age, in keeping with other studies showing lower rates of eye care utilization among younger patients [25–27]. Those over 65 years of age were more likely to have been screened within the preceding 12 months than those in the 50–64 age group, which may be due to an increased rate of ocular complaints in an older population. With only 63 % of those asked indicating that they had undergone an ocular exam within the previous 12 months suggesting inadequate screening regimes, it may be that longer screening intervals are being offered as part of routine clinical practice. It has been suggested that appointment intervals may be safely extended to two or even 3 years for type II diabetic patients who have not yet developed retinopathy [28, 29]. However, we would caution against extending the screening intervals of type II diabetic patients who are on insulin, as we found a five-fold rate of sight-threatening retinopathy in these cases compared to those who did not require insulin, in keeping with other studies [13, 17].
Variations in attendance rates and opportunistic screening intervals may also be due to historical local funding and policy issues with respect to access to community or hospital eye services [30], reflecting the ad hoc nature of screening to date, or individual variations in how actively GPs engage with their patients in emphasizing the importance of screening for diabetic complications [25, 31]. We found significantly higher rates of non-attendance in urban environments compared to more rural locations. The higher rate of non-attendance in our County Clare clinics may reflect how more patients are already receiving regular screening locally through pre-existing ophthalmic services, as this was the only area to achieve the minimum standard of over 70 % being screened within 12 months [8]. In support of this, the areas with the best clinic attendance rates were also those where patients were less likely to have been screened within the previous year.
In the first round of a new screening service, duplication of screening is unavoidable, with nearly two-thirds of those questioned in our study indicating that they had already attended an eye specialist within the last 12 months. However, a number of the sight-threatening cases identified during our study were in instances where patients had already been screened elsewhere within the previous year. Furthermore, we found a number of patients who had already undergone treatment for both maculopathy and proliferative retinopathy in the past, but were deemed unstable and in need of further intervention. This demonstrates the benefits of a structured screening programme even in cases where patients already get their eyes routinely checked or have been previously managed within the hospital eye services.
The extent of the MWDRS was limited by the absence of a digital retinal photography service, which has not only been shown to be a highly sensitive screening tool [32], but also a cost-effective one [33]. On the other hand, it is worth noting that only 44 of the 117 patients we graded as having sight-threatening retinopathy required referral for hospital-based laser therapy or intravitreal injections, the remainder being suitable for ophthalmology review in the community, whereas all 117 would have required referral if they were screened by photography. Similarly, only 1 % of patients screened in our study were deemed ungradable through the use of slit-lamp biomicroscopy compared to the expected rate of between 5 and 10 % with retinal photography [8, 12], dramatically reducing the numbers needing referral due to ungradable image sets. This should be borne in mind when extrapolating the above figures regarding the likely impact of the national programme on hospital workloads where there is pre-existing ophthalmologist-led screening in the community.
There are a number of caveats worth noting with respect to the data collected in our study. The validation process employed may be subject to errors retrieving data from GP clinical software packages, and limited by the accuracy of recall by GPs regarding the diabetic status of individual patients. The determination of type I versus type II diabetes status can be inaccurate from both referral forms and patient inquiry. Our study is also missing data from a number of private GP practices. However, it is likely that many of these private patients are also on the systems of the GPs with GMS contracts, as private and public practices are often connected and share files on the practice software. Care should be taken when referencing the retinopathy data, as this was from a portion of the diabetic population, the results of which could be skewed by the sampling process. There may be recall bias of patients regarding their last screening appointment, as the frequency of eye examinations may be falsely elevated in self-reported data [34], and just refraction, rather than a dilated fundal exam may have taken place. Thus we may be presenting an overly optimistic picture as to the pre-existing retinal screening uptake in terms of both timing and quality.
In summary, we recommend that the use of MCP and LTI sources provide a useful basis with which to populate a diabetes register, but engagement with GPs is essential to ensure its accuracy and completeness. It is clear that macular oedema cases requiring anti-VEGF therapy will be responsible for a significant initial impact on the workload and budget of treatment centres following the commencement of the national programme. Referrals for non-diabetic ocular abnormalities will also add to hospital workloads, but this can be offset against the large numbers of diabetic clients with non-referable retinopathy who could be safely discharged to receive screening in the community. The MWDRS has over 11,000 patients on its database, and if the rates of sight-threatening retinopathy in this study are representative of the total diabetic population in the Mid-West, structured screening may help prevent up to 280 patients from going blind locally. This emphasizes the timeliness of the full implementation of the national programme, and it is hoped that this will improve the standard of care delivered to all patients living with diabetes in Ireland, even those who already undergo routine eye checks or have been previously managed within the hospital eye services.
References
International Diabetes Federation (2013) IDF Diabetes Atlas, 6th edn. International Diabetes Federation, Brussels
Yau JW, Rogers SL, Kawasaki R et al (2012) Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care 35:556–564
Kelliher C, Kenny D, O’ Brien C (2006) Trends in blind registration in the adult population of the Republic of Ireland 1996–2003. Br J Ophthalmol 90:367–371
National Council for the Blind of Ireland (2011) The cost of sight loss: the economic impact of vision impairment and blindness in the Republic of Ireland. NCBI Publications, Dublin
Bachmann MO, Nelson SJ (1998) Impact of diabetic retinopathy screening on a British district population: case detection and blindness prevention in an evidence-based model. J Epidemiol Community Health 52:45–52
Balanda KP, Barron S, Fahy L (2010) Making chronic conditions count: hypertension, coronary heart disease, stroke, diabetes. A systematic approach to estimating and forecasting population prevalence on the island of Ireland. Executive summary. Institute of Public Health in Ireland, Dublin
Delcourt C, Massin P, Rosilio M (2009) Epidemiology of diabetic retinopathy: expected vs reported prevalence of cases in the French population. Diabet metab 35:431–438
Health Service Executive Expert Advisory Group National Retinopathy Screening Committee (2008) Framework for the development of a diabetic retinopathy screening programme for Ireland. Health Service Executive, Kildare
Harding S, Greenwood R, Aldington S et al (2003) Grading and disease management in national screening for diabetic retinopathy in England and Wales. Diabet Med 20:965–971
Cooke M, Leane G, Mannix M et al (2010) Development of a diabetes register in Ireland: feasibility study—recommendations for the establishment of a register. Health Service Executive, Kildare
Williams R, Airey M, Baxter H et al (2004) Epidemiology of diabetic retinopathy and macular oedema: a systematic review. Eye 18:963–983
Mc Hugh S, Buckley C, Murphy K et al (2013) Quality-assured screening for diabetic retinopathy delivered in primary care in Ireland: an observational study. Br J Gen Pract 63:85–86
Younis N, Broadbent DM, Harding SP et al (2002) Prevalence of diabetic eye disease in patients entering a systematic primary care-based eye screening programme. Diabet Med 19:1014–1021
Broadbent DM, Scott JA, Vora JP et al (1999) Prevalence of diabetic eye disease in an inner city population: the Liverpool Diabetic Eye Study. Eye 13:160–165
Raymond NT, Varadhan L, Reynold DR et al (2009) Higher prevalence of retinopathy in diabetic patients of South Asian ethnicity compared with white Europeans in the community: a cross-sectional study. Diabetes Care 32:410–415
Forster AS, Forbes A, Dodhia H et al (2013) Changes in detection of retinopathy in type 2 diabetes in the first 4 years of a population-based diabetic eye screening program: retrospective cohort study. Diabetes Care 36:2663–2669
Looker HC, Nyangoma SO, Cromie DT et al (2014) Rates of referable eye disease in the Scottish National Diabetic Retinopathy Screening Programme. Br J Ophthalmol 98:790–795
Mitchell P, Bandello F, Schmidt-Erfurth U et al (2011) The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology 118:615–625
Scanlon PH, Carter S, Foy C et al (2005) An evaluation of the change in activity and workload arising from diabetic ophthalmology referrals following the introduction of a community based digital retinal photographic screening programme. Br J Ophthalmol 89:971–975
Cugati S, Kifley A, Mitchell P et al (2006) Temporal trends in the age-specific prevalence of diabetes and diabetic retinopathy in older persons: population-based survey findings. Diabetes Res Clin Pract 74:301–308
Leese GP, Morris AD, Swaminathan K et al (2005) Implementation of national diabetes retinal screening programme is associated with a lower proportion of patients referred to ophthalmology. Diabet Med 22:1112–1115
James M, Heng TH, Minasyan D (2014) A quantitative analysis of diabetic retinopathy screening in a regional treatment centre. Ir Med J 107:321–323
Javitt JC, Aiello LP (1996) Cost-effectiveness of detecting and treating diabetic retinopathy. Ann Intern Med 124:164–169
Leese GP, Boyle P, Feng Z et al (2008) Screening uptake in a well-established diabetic retinopathy screening program. Diabetes Care 31:2131–2135
Schoenfeld ER, Greene JM, Wu SY et al (2001) Patterns of adherence to diabetes vision care guidelines: baseline findings from the diabetic retinopathy awareness program. Ophthalmol 108:563–571
MacLellan PA, McGwin G, Heckemeyer C et al (2014) Eye care use among a high-risk diabetic population seen in a public hospital’s clinics. JAMA Ophthalmol 132:162–167
Mukamel DB, Bresnick GH, Wang Q et al (1999) Barriers to compliance with screening guidelines for diabetic retinopathy. Ophthalmic Epidemiol 6:61–72
Chalk D, Pitt M, Vaidya B et al (2012) Can the retinal screening interval be safely increased to 2 years for Type 2 diabetic patients without retinopathy? Diabetes Care 35:1663–1668
Agardh E, Tababat-Khani P (2011) Adopting 3-year screening intervals for sight-threatening retinal vascular lesions in type 2 diabetic subjects without retinopathy. Diabetes Care 34:1318–1319
Bagga P, Verma D, Walton C et al (1998) Survey of diabetic retinopathy screening services in England and Wales. Diabet Med 15:780–782
Dervan E, Lillis D, Flynn L et al (2008) The factors that influence the patient uptake of diabetic retinopathy screening. Ir J Med Sci 177:303–308
Hutchinson A, McIntosh A, Peters J et al (2000) Effectiveness of screening and monitoring tests for diabetic retinopathy—a systematic review. Diabet Med 17:495–506
James M, Turner DA, Broadbent DM et al (2000) Cost effectiveness analysis of screening for sight threatening diabetic eye disease. Br Med J 320:1627–1631
Harwell TS, Moore K, Madison M et al (2001) Comparing self-reported measures of diabetes care with similar measures from a chart audit in a well-defined population. Am J Med Qual 16:3–8
Acknowledgments
We wish to thank Patricia Brewitt (Mid-West Database Co-ordinator, Primary, Continuing and Community Care, HSE West) for her effort and dedication in helping set up the Mid-West diabetes database, including the scheduling of practice visits, the validation of provisional lists, entry and updating of client details into the database, and organizing clinics to screen clients from this database. We would also like to thank Patrice James (Researcher, Oral Health Services Research Centre, University College Cork) for her considerable contribution on the statistical analysis and editing of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
James, M., Goodchild, C., Bashir, S. et al. Report on the creation of a diabetes register and retinopathy screening outcomes in the Mid-West of Ireland. Ir J Med Sci 185, 151–159 (2016). https://doi.org/10.1007/s11845-015-1248-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-015-1248-y