Abstract
Background
Fracture and dislocation of the thoracic spine without neurological deficits are rare. Most of these cases are managed by non-operative methods or a posterior approach surgery.
Aim
To report three cases of fracture and lateral dislocation of the thoracic spine without neurological deficits and review the literature on the management strategy.
Methods
Three patients who suffered thoracic spinal fracture and lateral dislocation without spinal cord injury underwent anterior decompression, reduction and internal fixation. The case series describe their management, surgical intervention and their follow-up.
Results
Reduction was satisfactory, none of the patients had any postoperative neurological deficits. Fusion was successful, and vertebral column alignment was maintained at the last follow-up.
Conclusion
An anterior approach facilitated adequate decompression, reduction and stabilization through instrumentation in this series of injury without neurological deficits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past few years, the incidence of spinal cord injuries has increased dramatically [1–3]. This has been attributed to an increase in the number of traffic accidents as well as work place-related injuries [4, 5]. Thoracic injuries, especially those involving dislocations, are severe injuries that affect the spinal column and can cause spinal cord injury (SCI). It is extremely rare that fracture-dislocations of the thoracic spine do not result in SCI. We present three cases of fracture and lateral dislocation of the thoracic spine without any neurologic deficits. In addition, the surgical treatment employed in the management of these cases is discussed.
Case reports
Case 1
A 50-year-old woman fell from a height of 10 m and injured her back. She was admitted to our hospital immediately following the fall. On admission, the patient was drowsy and complained of severe head, chest and mid-back pain. She was tachycardia with a heart rate of 128 per min and hypotensive with a blood pressure of 75/52 mmHg. Local examination revealed severe tenderness and crepitation in the mid-thoracic region. Her cranial nerves, motor power, sensory examination, reflexes and sphincter tone were normal.
Initial radiographs and CT showed a complete lateral displacement of T5/T6. The body of T6 was displaced laterally to the right of the body of T5 (Fig. 1a). CT also demonstrated bilateral pulmonary contusions, hemothorax, and fractures of the 5th and 6th ribs and the right scapula. Subsequently, a MRI revealed that although the thecal sac was stretched at the level of T5/T6, there was no significant compromise of the neural canal (Fig. 1b, c).
a CT demonstrating the lateral displacement of the sixth thoracic vertebra over the fifth thoracic vertebra. b, c Coronal MRI demonstrating the nature of disruption of the spinal column with translation and overlap of the fifth and sixth thoracic vertebrae. Also noted is the stretched thecal sac without any significant narrowing of the neural canal. d Postoperative anteroposterior roentgenogram showing the reduced lateral dislocation and fixation. e, f A follow-up roentgenogram demonstrates a healed fracture and good alignment in both AP and lateral radiographs
The patient was admitted to the intensive care unit because of unstable vital signs. Bilateral chest tubes were inserted immediately to manage the hemothorax. After fluid resuscitation and blood transfusions, her vital signs became stable.
The patient underwent surgical intervention 25 days after admission. Under general anesthesia, the patient was placed in the right lateral decubitus position. The spine was approached through a left thoracotomy incision, removing the 5th and 6th ribs, the body of T6, the left section of T5, and the discs of T4/5, T5/6 and T6/7. The dural sac was fully exposed. With the cord under direct vision, sufficient distraction was performed to reduce the dislocation. The resected ribs were used as bone-graft struts to implant the area of the partial corpectomy. Then, internal fixation with an anterior lateral plate and screws from T4–7 was completed. The wound was irrigated and closed with a chest tube placed on the left side.
The patient had an uneventful postoperative course. Her neurological function remained intact. The patient was discharged after 2 weeks, and mobile in a brace postoperative. Roentgenographically, an anatomic alignment was obtained and maintained at discharge as well as at subsequent follow-up appointments (Fig. 1d–f). At the last follow-up, approximately 5 years after admission, the patient did not complain of any back pain and has maintained a good quality of life.
Case 2
A 35-year-old man was involved in a motorcycle accident. He was admitted to our hospital 2 days later. On admission, the patient was fully conscious and his vital signs were stable. He complained of severe mid-back pain. Palpation of the area revealed a marked separation of the spinous processes at the middle thoracic level. He had normal sphincter control, and neurologic examination of extremities revealed normal muscle power, sensation and reflexes.
Radiographs revealed fracture and lateral displacement at T6/7 with right scoliosis and kyphosis (Fig. 2a, b). CT showed a severely comminuted fracture of the body of T7 with fractures of the 6th and 7th pedicles on the left side and 6th, 7th and 8th transverse processes on the right side. The volume of the spinal canal was increased at the T7 level (Fig. 2c, d). MRI confirmed that the spinal cord had angulated; however, there were no signal changes inside the spinal cord (Fig. 2e).
a, b Anteroposterior and lateral roentgenogram showing the fracture and lateral displacement at T6/7 with a right scoliosis and kyphosis. c, d CT demonstrating comminuted fracture and lateral displacement of T7. The transverse diameter of the spinal canal was increased resulting in an increase in the space available for the spinal cord. e MRI demonstrating the angulated spinal cord without changes in the signal intensity. f Postoperative anteroposterior roentgenogram showing the reduced lateral dislocation and internal fixation with a titanium mesh and anterior lateral plate. g Follow-up CT showing a wide neural canal and that the space for the spinal cord is well maintained
Under general anesthesia, the patient was placed in the left lateral position because of right thoracic scoliosis and hemothorax. After removal of the 6th and 7th ribs, the body and transverse process of the fractured T7 was excised to expose the spinal cord. A titanium mesh filled with bone graft was inserted into the space between T6 and T8, which was distracted and reduced with lamina spreaders. An anterolateral plate was fixed to restore the anatomical relationship. The wound was closed in layers and a chest tube was placed.
Postoperative examination confirmed the patient’s intact neurological status. After the chest tube was removed, a plastic-moulded brace was applied for 3 months. On last follow-up at 4 years, he was asymptomatic, with pain-free thoracic movements and unimpaired neurological status. Radiographs showed an excellent fusion mass (Fig. 2f). Follow-up CT at 15 months after surgery showed healing of the fractures with no significant stenosis at any level (Fig. 2g).
Case 3
A 56-year-old man was involved in an automobile accident, 5 days later, he was transferred to our hospital. On examination, the patient was stable with normal vital signs and complained of pain in the back and left chest. His sphincter control, sensations, muscle power and reflexes were intact, except the tenderness and ecchymosis over the middle back and left chest.
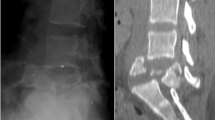
CT scan showed a fracture with lateral displacement of the T7/8 vertebrae (Fig. 3a, b). MRI demonstrated an increase in the spinal diameter at the dislocation level without any signal changes of the spinal cord (Fig. 3c).
a, b CT demonstrating a comminuted fracture and lateral displacement of T8. The transverse diameter of the spinal canal was increased. c MRI demonstrating a normal signal intensity of the spinal cord indicating that there was no damage to the spinal cord. d Postoperative CT showing that reduction and anatomic alignment was obtained. e, f Follow-up roentgenogram demonstrating a maintained spinal cord alignment on subsequent follow-ups
For the purpose of the surgery, the patient was positioned in the right lateral decubitus position through left thoracic approach. After the 7th and 8th ribs were resected, the T8 vertebral body was partially removed. This exposed the central and left lateral aspects of the spinal canal. Reduction via gradual distraction was performed under direct visualization. A titanium mesh was implanted to the area of the partial corpectomy, and a lateral plate was fixed at T7–T9 for stabilization.
The patient had no postoperative neurological deficits. He was discharged after 2 weeks with VAS score was 2. For 3 months, he walked freely wearing a plastic custom-made body jacket. The postoperative CT demonstrated satisfactory realignment of the surgical segment (Fig. 3d). In addition, follow-up spinal radiographs after 2 years revealed adequate vertebrae alignment and spinal fusion (Fig. 3e, f).
Discussion
Fracture-dislocations of the thoracic spine frequently result in complete paraplegia due to narrowing of the thoracic canal and the precarious blood supply of the spinal cord in this region. Incidence of severe thoracic fracture and dislocation without neurological damage is extremely rare. To our knowledge, only 16 cases have been reported in the English language literature [6–16]. Traffic trauma [7–15, 17] and injury secondary to falls from a height [7, 16] are common etiological factors. Biomechanical studies have shown that the spine is very vulnerable to shear and rotational forces and that the hyperflexion or hyperextension forces alone can seldom cause a fracture-dislocation. However, when these forces are combined with rotational force, mechanical failure is more likely to occur [18]. McAfee et al. [19] defined fracture-dislocations as translational injuries due to shear forces, while Magerl et al. [20] classified fracture-dislocations as rotational injuries resulting from torsional forces. According to the AO’s comprehensive spinal injury classification, the injuries could be classified as C1.2.4, in which the vertebral body separates and the spinal canal may be widened at the level of trauma/lesion [20]. There are two different patterns of dislocation that occur depending on the direction of force experienced by the spinal column. One is anterior–posterior [6–10] and the other is lateral or rotational dislocation [7, 11–16]. In this series, the dislocation in the first case was secondary to a lateral shear and flexion force. In contrast, the dislocations in cases 2 and 3 were due to forced flexion combined with rotation.
In this series of cases, we believe that SCI did not occur because of “spontaneous decompression” [13, 21–23]. This was perhaps due to complete disruption of the rigid bony envelopment around the neural structures. Consequently, the middle and posterior columns were widely separated and resulted in marked widening of the spinal canal. The cord maintained its correct relationship to the posterior elements and was, therefore, not compromised. The ribcage helps maintain the stability of an injured thoracic spine, decreasing the risk of neurological injury [13, 21].
Currently, there are no clear-cut guidelines for the treatment of thoracic fracture-dislocations without any neurological deficits. Several case studies have treated these patients with halo-femoral traction and bed rest followed by rigid casting [7, 8, 10, 11, 14]. Closed reduction by means of traction is not only impossible, but also carries the danger of a neurological lesion due to narrowing of the spinal canal during traction [24]. Conservative treatment is the first choice in older patients and in those with underlying diseases or serious complications [10, 21].
The optimum treatment for thoracolumbar fracture-dislocation lesions is reduction and internal fixation if the patient’s condition is suitable for surgery [21]. A major challenge in surgical management is achieving reduction and preserving the neurologic function after stabilization [16]. In all our cases, reduction of the fracture and dislocation was considered necessary to produce a more biomechanically stable spine, to enhance the possibility of fusion, and to prevent delayed neurologic deterioration [24]. However, reduction entails highly significant risks, especially in neurologically uncompromised individuals with severe thoracic displacement [13].
The most optimal surgical approach for decompression and stabilization is controversial. The majority of studies prefer posterior reduction, internal fixation and posterolateral fusion [6, 7, 15–17]. Posterior reduction and stabilization without anterior fusion increases the risk of loss of reduction, instrumentation failure, and non-union in long-term follow-up [25–27]. In addition, attempting to reconstruct the anterior and middle columns through a posterior approach entails a great risk especially in the patient who is neurologically intact. Another method that has been described includes a combined anterior–posterior approach with corpectomy, anterior intervertebral fusion, and subsequent posterior instrumentation. This technique usually involves longer operating times and has a greater risk of surgical complications. Furthermore, it commonly requires two surgical teams and longer postoperative hospital stays and has higher postoperative morbidity [29]. All the three cases suffered concomitant severe thoracic trauma, such as pulmonary contusions and hemothorax. These serious injuries precluded use of extensive surgeries specifically the single stage combined anterior and posterior approaches surgery. In this case, we decided to perform anterior surgery first, and followed the cases vigilantly. Since there was good bone fusion and no loss of reduction was found on subsequent follow-ups, the posterior operation as second stage procedure seemed unnecessary. As for unstable thoracolumbar burst fractures, some studies have advocated that anterior decompression and reconstructions must be performed to avoid delayed loss of sagittal and coronal balance [28, 29]. From our own experience, following partial corpectomy and resection of the pedicles and transverse processes, an anterior approach achieves adequate exposure to prevent cord contusion, root entrapment, dural tears, and disc or bony fragment displacement. Reduction can be performed under direct visualization of the spinal cord, minimizing the risk of SCI. Meanwhile, lateral dislocation can be corrected easily by distraction and internal fixation. Also, the anterior and middle column can be reconstructed and fused simultaneously. Anterior instrumentation devices combined with a structural graft allow for a stable construct that may obviate a posterior procedure [30]. With the support of the ribcage, sternum and a plaster cast or brace, a long period of bed rest can be avoided and possible urinary and respiratory complications can be reduced [6].
The three cases described in this report are unique due to the absence of neurological symptoms following a lateral fracture-dislocation of the thoracic spine. This study describes the successful use of an anterior approach, reduction maneuvers and instrumentation to achieve an optimal result in managing these cases. We believe that this treatment strategy may be suitable for managing lateral fracture-dislocations of the middle thoracic spine without SCI, meanwhile, it is equally important to follow-up until a sound bone fusion occurs and radiologically no loss of reduction is seen.
References
Langlois JA, Rutland-Brown W, Wald MM (2006) The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil 21(5):375–378
McCammon JR, Ethans K (2011) Spinal cord injury in Manitoba: a provincial epidemiological study. J Spinal Cord Med 34(1):6
Tator C, Bray G, Morin D (2007) The CBANCH report—the burden of neurological diseases, disorders, and injuries in Canada. Can J Neurol Sci 34(3):268–269
Sekhon LH, Fehlings MG (2001) Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine 26(24S):S2–S12
Jackson AB, Dijkers M, DeVivo MJ, Poczatek RB (2004) A demographic profile of new traumatic spinal cord injuries: change and stability over 30 years. Arch Phys Med Rehabil 85(11):1740–1748
Sasson A, Mozes G (1987) Complete fracture-dislocation of the thoracic spine without neurologic deficit: a case report. Spine 12(1):67–70
Simpson A, Williamson D, Golding S, Houghton G (1990) Thoracic spine translocation without cord injury. J Bone Joint Surg Br 72(1):80–83
Voronovich I, Dulub O, Nikolayev V, Selkov J (1990) A variant of severe deformation of the thoracic spine with favorable neurologic outcome. Spine 15(8):833–834
Yang SC, Yu SW, Chen YJ, Chen WJ (2003) Surgical treatment for thoracic spine fracture-dislocation without neurological deficit. J Formos Med Assoc 102(8):581–585
Miyasaka Y, Satomi K, Sugihara S, Tahara Y, Hayashi T, Ishii Y (1993) Posterior fracture-dislocation of the thoracic spine without neurologic deficit: a case report and short literature review. Spine 18(15):2351–2354
Gertzbein S, Offierski C (1979) Complete fracture-dislocation of the thoracic spine without spinal cord injury. A case report. J Bone Joint Surg Am 61(3):449
Weber SC, Sutherland GH (1986) An unusual rotational fracture-dislocation of the thoracic spine without neurologic sequelae internally fixed with a combined anterior and posterior approach. J Trauma 26(5):474–479
Harryman DT (1986) Complete fracture-dislocation of the thoracic spine associated with spontaneous neurologic decompression: a case report. Clin Orthop Relat Res 207:64–69
Uriarte E, Elguezabal B, Tovio R (1987) Fracture-dislocation of the thoracic spine without neurologic lesion. Clin Orthop Relat Res 217:261–265
Korovessis P, Sidiropoulos P, Dimas A (1994) Complete fracture-dislocation of the thoracic spine without neurologic deficit: case report. Spine 36(1):122–124
Alobaid A, Arlet V, Ouellet J, Reindl R (2006) Surgical technique: technical notes on reduction of thoracic spine fracture dislocation. Can J Surg 49(2):131
Liljenqvist U, Halm H, Castro W, Mommsen U (1995) Thoracic fracture-dislocations without spinal cord injury: a case report and literature review. Eur Spine J 4(4):252–256
Roaf R (1960) A study of the mechanics of spinal injuries. J Bone Joint Surg Br 42(4):810–823
McAfee PC, Yuan H, Fredrickson B, Lubicky J (1983) The value of computed tomography in thoracolumbar fractures. J Bone Joint Surg Am 65(4):461–473
Magerl F, Aebi M, Gertzbein S, Harms J, Nazarian S (1994) A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 3(4):184–201
Akay KM, Baysefer A, Kayali H, Beduk A, Timurkaynak E (2003) Fracture and lateral dislocation of the T12-L1 vertebrae without neurological deficit. Neurol Med Chir 43(5):267–270
Hsieh CT, Chen GJ, Wu CC, Su YH (2008) Complete fracture-dislocation of the thoracolumbar spine without paraplegia. Am J Emerg Med 26(5):633.e5–633.e7
Jackson RH, Quisling RG, Day AL (1979) Fracture and complete dislocation of the thoracic or lumbosacral spine: report of three cases. Neurosurgery 5(2):250–253
Abdel-Fattah H, Rizk AH (1990) Complete fracture-dislocation of the lower lumbar spine with spontaneous neurologic decompression. Clin Orthop Relat Res 251:140–143
Obeid I, Guérin P, Gille O, Gangnet N, Aurouer N, Pointillart V et al (2011) Total vertebrectomy and spine shortening in the management of acute thoracic spine fracture dislocation: technical note and report of 3 cases. J Spinal Disord Tech 24(5):340–345
McCormack T, Karaikovic E, Gaines RW (1994) The load sharing classification of spine fractures. Spine 19(15):1741–1744
Sasso RC, Cotler HB (1993) Posterior instrumentation and fusion for unstable fractures and fracture-dislocations of the thoracic and lumbar spine: a comparative study of three fixation devices in 70 patients. Spine 18(4):450–460
Kirkpatrick JS (2003) Thoracolumbar fracture management: anterior approach. J Am Acad Orthop Surg 11(5):355–363
Otani K, Higuchi M, Watanabe T, Nakai S, Fujimura Y, Manzoku S et al (1984) The surgical reconstruction of fractures and fracture dislocations of the thoraco-lumbar spine. Int Orthop 8(1):29–36
McDonough PW, Davis R, Tribus C, Zdeblick TA (2004) The management of acute thoracolumbar burst fractures with anterior corpectomy and Z-plate fixation. Spine 29(17):1901–1908
Acknowledgements
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Conflict of interest
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tong, J., Zhou, R., Liu, S. et al. Management of fracture and lateral dislocation of the thoracic spine without any neurological deficits: three case reports and review of the literature. Ir J Med Sci 185, 949–954 (2016). https://doi.org/10.1007/s11845-014-1237-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-014-1237-6