Abstract
Purpose
Patient-reported outcomes (PROs) are essential for assessing potential late effects experienced by young adult cancer survivors (YACS), but stigma and social desirability bias may limit their effectiveness for assessing sensitive topics (e.g., suicidal ideation, sexual health). This study compared two methods of item administration to determine the optimal method for obtaining sensitive information in YACS.
Methods
Two hundred forty-four YACS (ages 18–40) were randomized to complete measures of suicidal ideation and sexual health (i.e., sensitive items) by paper survey or by telephone automated computer assisted structured interview (TACASI). Participants also provided information on acceptability of administration mode and sensitive items.
Results
The proportion of participants reporting symptoms did not significantly vary between paper and TACASI administration: respectively, 10% vs. 12% reported suicidal ideation and 55% vs. 58% reported sexual health concerns. The majority (≥ 78%) of participants reported feeling comfortable answering sensitive items on paper and TACASI and there were no significant differences in acceptability based on administration mode. Although participants endorsing sensitive symptoms were significantly more likely to feel upset answering sensitive items, the majority (93%) of participants experiencing symptoms still felt they were important to ask.
Conclusions
Despite their potentially sensitive nature, questions about suicidal ideation and sexual health were highly acceptable to YACS across administration modes. Moreover, YACS almost universally endorse the importance of providers asking about these topics.
Implications for Cancer Survivors
Findings should bolster provider confidence that screening for suicidal ideation and sexual health concerns can and should be integrated into clinical care for YACS using paper or technology-assisted methods.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Young adult cancer survivors (YACS) are at risk for a wide range of late effects of cancer treatment. Indeed, current clinical care guidelines include screening recommendations for more than 120 potential late effects [1, 2]. Patient-reported outcomes (PROs) are important tools for assessing survivors’ health and well-being after cancer and are particularly critical for assessment of symptoms involving subjective experience such as depression, anxiety, quality-of-life, pain, and fatigue [3,4,5]. Despite their utility, clinical information reported on PROs can be limited if patients feel uncomfortable disclosing sensitive symptoms (e.g., suicidal ideation, sexual health) due to stigma or a fear of consequences (e.g., hospitalization due to suicide risk) [6,7,8]. Additionally, patient report of sensitive symptoms may be influenced by social desirability bias, in which patients under-endorse socially undesirable activities and over-endorse socially desirable ones [9]. YACS may be particularly prone to reporting bias; research suggests that YACS underreport negative symptoms and overreport positive traits, possibly in an effort to be seen more positively by themselves and others [10].
Method of administration is a crucial factor in determining the accuracy and completeness of responses [9]. Specifically, self-administered assessments have been shown to increase reporting of concerns and reduce social desirability bias on sexual health and other sensitive topics. One form of self-administered assessment is a telephone automated computer assisted structured interview (TACASI) [9, 11,12,13,14]. TACASIs allow a computer to administer an interview and record responses with no human interviewer involved, potentially facilitating disclosure of sensitive symptoms [11,12,13,14]. For example, participants are more likely to report sexual behaviors [14] and symptoms of sexually transmitted diseases (STDs) [15] on an assessment using TACASI compared to a human interviewer. One study found this relationship to be strongest for younger participants [15], suggesting that TACASI may be particularly appropriate for YACS. Despite its potential to provide quick, low-cost screening in cancer survivors, to our knowledge no studies have reported on the use of TACASI in a population of YACS.
To evaluate the utility of TACASI for gathering sensitive information from YACS, this study compared the prevalence of suicidal ideation and sexual health concerns reported by YACS randomly assigned to paper-and-pencil or TACASI administration. Participants’ reports of acceptability of these two modes of sensitive item administration and differences in acceptability between participants who did and did not endorse sensitive symptoms were also evaluated. Because the TACASI assessment process eliminates direct human interaction [11,12,13,14], we hypothesized participants assigned to TACASI administration would be more likely to report sensitive symptoms and higher acceptability of sensitive items compared to participants assigned to paper administration. Additionally, we hypothesized that acceptability of sensitive items would be lower for participants reporting sensitive symptoms regardless of administration mode [6,7,8].
Methods
Participants and procedure
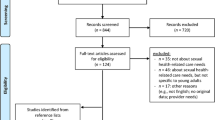
Participants were 250 young adult cancer survivors (YACS) enrolled in E-Quest, a study of self-report measures of anxiety and depression in YACS [16,17,18,19]. Participants were recruited from specialty clinics (e.g., breast cancer) within a single cancer center. To be eligible for E-Quest, survivors needed to be age 18–40, at least 3 years from their first cancer diagnosis, at least 2 years from treatment completion (excluding chemoprevention), and able to complete self-report measures in English. Selective recruitment was used in an effort to enroll equal numbers of survivors diagnosed before and after age 21, with equal numbers of males and females in each of these groups. During the study period, 349 eligible survivors were approached and 250 (71.6%) consented and enrolled. Of these 250 participants, 248 (98%) completed all measures to study standards and were included in analyses; six were omitted from analysis due to incomplete data.
As part of the E-Quest study, all participants completed anxiety and depression measures administered using both paper-and-pencil and TACASI (these data not reported on here) [11,12,13,14]. In the TACASI administration, participants listened to a recording of each item over the telephone and provided their answer by pressing a telephone button. Additionally, each participant was randomized to complete the sensitive items inquiring about suicidal ideation and sexual health either using paper-and-pencil or TACASI. Finally, all participants completed an exit survey on paper to assess acceptability of sensitive items and administration mode. Study procedures were approved by the cancer center’s institutional review board and all measures were completed during a single study visit.
Measures
Demographic and treatment information
Participants reported their demographic (e.g., age, race, ethnicity) and medical (e.g., cancer diagnosis) information on a study questionnaire.
Suicidal ideation
Participants completed six items on suicidal ideation under the survey heading of “hopelessness and emotional distress.” Specifically, items asked participants if in the last 12 months they had (1) felt life was not worth living, (2) thought they would be better off dead, (3) had thoughts of ending their life, (4) seriously thought about committing suicide, (5) made a plan for committing suicide, and (6) attempted suicide. Participants were coded as expressing suicidal ideation if they responded “Yes” to one or more of these items. Items were previously adapted from established mental health measures and employed in a study of suicidal ideation in prostate cancer survivors [20]. Participants were also asked if they had completed any treatment (e.g., hospitalization, medication) for a psychiatric or emotional problem in the past 12 months.
Sexual health
Participants completed nine items on sexual health under the survey heading of “sexual health and functioning.” Items asked about sexual interest, sexual activity, sexual pain, sexual dysfunction (e.g., erectile dysfunction, vaginal dryness), and sexual satisfaction in the last 30 days. As seen in Supplemental Table 1, these items were adapted from the Patient-Reported Outcomes Measurement Information System (PROMIS) Network sexual health item bank [21]. Adaptations were made for clarity and brevity (e.g., by reducing the number of response categories). Participants were classified as having a sexual health concern if they endorsed erectile dysfunction, vaginal dryness, or pain with sexual activity, or if they reported that they were “Not at all” or “A little” satisfied with their sex life (as opposed to “Somewhat,” “Quite a bit,” or “Very much” satisfied). Participants were also asked if they had spoken with a medical provider about sexual health concerns in the past 12 months.
Exit survey
The exit survey is a questionnaire developed for this study to ascertain respondents’ subjective appraisal of the paper and TACASI administration modes and the acceptability the sensitive items used in this study. Specifically, participants were asked if items were easy to complete, easy to understand, upsetting, frustrating, “too personal,” and important for providers to ask. Participants were also asked if they felt comfortable answering items and whether items should only be asked if the patient initiates the subject. Participants responded using a 4-point scale: “Agree strongly,” “Agree somewhat,” “Disagree somewhat,” and “Disagree strongly.” Participants were categorized as agreeing with the statement if they selected “Agree strongly” or “Agree somewhat.” Participants completed this measure on paper independently after responding to all sensitive items.
Statistical analysis
Descriptive statistics were used to summarize demographic, medical, sensitive item, and acceptability variables. Chi-square analyses were used to compare prevalence of sensitive symptoms and acceptability variables by sex (i.e., male, female); except where noted below, findings were not statistically significant. Chi-square analyses and Fisher’s exact tests were used to compare the two administration groups (paper vs. TACASI) on prevalence of sensitive symptoms reported and acceptability of sensitive items. To examine how the presence of sensitive symptoms affected participants acceptability ratings, participants with and without sensitive symptoms were compared on acceptability variables using Fisher’s exact tests; as there were no significant differences in acceptability based on administration mode (Table 1), the paper and TACASI groups were collapsed for these analyses (Table 2). Results were considered statistically significant if associated probabilities were < 0.05.
Results
Sample description
Participants were 122 males (60 diagnosed < age 21) and 122 females (61 diagnosed age < 21), the majority of whom were Non-Hispanic and White (84%). Mean age at study participation was 29.5 years (SD = 7.35, range 18–40). Age of first cancer diagnosis ranged from birth to 37 years (M = 20.56 years, SD = 9.74). The most common cancer diagnoses were Hodgkin’s lymphoma (21%), leukemia (17%), and sarcoma (7%).
Suicidal ideation
Twenty-seven participants (11%) endorsed experiencing at least one symptom of suicidal ideation in the last 12 months. Specifically, 19 participants (8%) reported feeling that life was not worth living, 14 (6%) reported feeling it would be better if they were dead, 12 (5%) reported having thoughts about ending their life, 3 (1%) reported having seriously considered committing suicide, and 1 (0.4%) reported making a suicide plan. No participants endorsed attempting suicide in the past 12 months. Of participants reporting suicidal ideation, 18 (67%) reported mental health treatment in the last 12 months such as appointment with a mental health provider (n = 17, 63%), psychiatric medication (n = 14, 52%), and hospitalization (n = 1, 4%).
Sexual health
Over half of participants (n = 135, 55%) reported at least one sexual health concern in the last 30 days. Specifically, 24 (19%) male participants reported difficulty getting or sustaining an erection and 15 (12%) reported using prescription medication to get an erection. Thirty-three (28%) female participants reported vaginal dryness affecting their sex life and 41 (35%) reported using personal lubricants or vaginal moisturizers. A significantly higher proportion of female participants reported pain with sexual activity (n = 22, 18%) than male participants (n = 9, 7%; X2 = 6.38, p = 0.01). Ninety-eight (40%) participants reported feeling dissatisfied with their sex life (i.e., “Not at all” or “A little” satisfied). Sixty (25%) participants reported no sexual activity with another person in the last month despite wanting sexual activity during this time. Of those reporting at least one sexual health concern, less than a quarter (24%) reported speaking with their provider about sexual health problems in the last year.
Effect of administration mode on symptom prevalence and acceptability
Suicidal ideation
There was no significant difference in proportion of participants reporting suicidal ideation using paper (10%) vs. TACASI (12%, X2 = 0.38, p = 0.54). Similarly, no significant differences in acceptability of suicidal ideation items were found between paper and TACASI groups (Table 1). Of note, the majority of participants reported that, given the choice, they would prefer to answer these items on paper (paper, 51%; TACASI, 9%; no preference, 39%). In both paper and TACASI groups, the overwhelming majority (≥ 92%) reported feeling comfortable answering suicidal ideation items and felt items were easy to complete, clear and easy to understand, important to ask, and will help providers understand patient health (Table 1). However, a minority (≤ 6%) of participants felt suicidal ideation items were upsetting, frustrating, or “too personal” and approximately 13% felt they should only be asked if the patient initiates the subject (Table 1).
Sexual health
The proportion of participants reporting sexual health concerns did not significantly differ between paper (55%) vs. TACASI groups (58%, X2 = 0.30, p = 0.59), and no significant differences in acceptability of sexual health items were found between the two administration groups (Table 1). Consistent with analysis of suicidal ideation items, the majority of all participants reported that, given the choice, they would prefer to answer sexual health items on paper (paper, 55%; TACASI, 11%; no preference, 34%). For both paper and TACASI, the majority (≥ 77%) of participants reported feeling comfortable answering sexual health items and felt items were easy to complete, clear and easy to understand, important to ask, and will help providers understand patient health (Table 1). However, a minority (≤ 9%) of participants felt sexual health items were upsetting, frustrating, or “too personal” and approximately 25% felt they should only be asked if the patient initiates the subject (Table 1). Of note, although not statistically significant, twice as many participants reported feeling upset completing sexual health items on TACASI (n = 10, 8%) vs. paper (n = 5, 4%).
Effect of symptom report on acceptability
Suicidal ideation
Compared to those who reported no suicidal ideation, participants endorsing suicidal ideation reported significantly lower rates of acceptability on two of the nine acceptability items. Specifically, they were significantly less likely to report feeling comfortable answering suicidal ideation items (82% vs. 95%) and significantly more likely to report feeling upset by suicidal ideation items (15% vs. 2%; Table 2). Nonetheless, the majority of participants experiencing suicidal ideation felt that suicidal ideation items were important to ask (93%). There were no other statistically significant differences in acceptability between participants who endorsed suicidal ideation and those who did not (Table 2).
Sexual health
Participants endorsing sexual health concerns were significantly more likely to report feeling upset completing sexual health items compared to participants who did not endorse sexual health concerns (9% vs. 2%; Table 2). However, the majority of participants experiencing sexual health concerns felt that sexual health items were important to ask (93%). There were no other statistically significant differences in acceptability between participants who endorsed sexual health concerns and those who did not (Table 2).
Discussion
Based on prior research using automated interviews [11,12,13,14,15], we expected TACASI to facilitate survivors’ disclosure of suicidal ideation and sexual dysfunction, two distressing and sensitive potential late effects in YACS. However, contrary to our hypotheses and previous findings, participants in the current study were equally likely to report symptoms on paper surveys or using TACASI. Similarly, although the majority of participants reported preferring paper surveys, we found no significant differences in acceptability of sensitive items across modes of administration. These unexpected findings may be due to the fact that studies demonstrating participants report more sensitive symptoms on TACASI compared TACASI to a clinical interview with a human interviewer [14, 15]. In our study, the limited human interaction involved in both paper surveys and TACASI may reduce social desirability bias and reluctance to endorse sensitive symptoms as compared clinical interviews. These results suggest that paper surveys and automated interviews are both well-suited for assessing sensitive items in YACS.
More generally, findings support the use of PROs for sensitive items in YACS. Almost all participants felt that the sensitive items were easy to complete, important to ask, and would help providers understand their health. Additionally, the majority of participants felt comfortable answering sensitive items. Even among participants experiencing sensitive symptoms, feeling upset or frustrated completing these items was uncommon. Nonetheless, that YACS with these symptoms were more likely to report this kind of discomfort suggests there is a burden for some YACS when reporting suicidal ideation and sexual health concerns. Fortunately, this burden seems to affect a small group of survivors, and seems to occur in those who, because of their symptoms are most likely to directly benefit directly from assessment of these sensitive issues. Moreover, even among YACS endorsing these symptoms, the overwhelming majority feel they are important to ask about, underscoring their openness to being asked about sensitive areas of health despite potential discomfort.
This research also reinforces and extends descriptive research available on suicidal ideation and sexual health in YACS. Several studies of YACS have highlighted the increased risk of suicidal ideation in this population [22, 23], including a large multicenter cohort that compared rates in YACS (8%) to their peers (5%) [24]. Although not designed or powered to determine prevalence of suicidal ideation in YACS, prevalence of suicidal ideation in the current study (10%) suggests that the sample is not atypical and underscores the importance of screening in this area. Research reporting rates of sexual dysfunction in YACS is more limited, but our results are consistent with findings that approximately half of YACS report at least one sexual health concern [25]. The current study adds to these prior findings by reporting sexual health concerns that may be particularly relevant to YACS (e.g., sexual dissatisfaction, lack of sexual activity despite interest) in addition to the physical symptoms (e.g., vaginal dryness) that are traditionally assessed [21, 25]. Findings also highlight gaps in evaluation of sexual health in YACS, as less than a quarter of those experiencing sexual health concerns had spoken with a provider about them in the last year. Additional research is needed to continue expanding inquiry and treatment of sexual health that is tailored to the YACS population. For example, development of items assessing concerns related to psychosexual milestones (e.g., delays in first sexual experience) and other aspects of YACS’s experience that may not be captured by existing measures is necessary.
Although findings provide important information on screening of sensitive items in YACS, limitations must be taken into consideration. First, participants were recruited from a moderate size YACS sample from a single cancer center and may not represent the range of demographics, suicidal ideation, and sexual health in the YACS population at large. Furthermore, as YACS who agreed to enroll in a research survey, study participants may have been more open and accepting of study items compared to YACS seen outside a research setting. Second, acceptability of sensitive items was assessed using a written exit survey; acceptability may have been different if assessed using TACASI or qualitative exit interviews. Similarly, interviews or items on social desirability bias may have provided information on how revealing participants were in their symptom report and why. Finally, sexual health items were adapted from items in previous studies (i.e., PROMIS sexual health items) to fit YACS and thus cannot be directly compared with other samples.
Despite these limitations, the current study provides important support and guidance in the use of PROs for assessing sensitive symptoms in YACS. First, as there was no difference in symptom report between paper and TACASI and both modes of administration were found to be highly acceptable, findings support the use of either option. Additionally, although only TACASI was examined here, high acceptability of this novel approach supports research into other automated data collection. For example, there is increasing support for the use of electronic PRO (ePRO) data collection (e.g., application-based, web-based portal), particularly when data can be automatically collected and integrated into electronic medical or research records [26]. Future research should examine whether ePRO applications may facilitate YACS’s reports of sensitive symptoms and increase acceptability of assessment. Similarly, given the overall preference of YACS for paper assessments in our sample, it would be important to learn whether familiarity or some other aspect of this approach is driving their choice.
In addition, the findings demonstrate that YACS appreciate medical providers asking them about sensitive health topics regardless of administration mode. Contrary to concerns raised by some medical providers [8, 27], YACS believe these topics are important to their healthcare and the majority feel comfortable being asked about these sensitive symptoms using paper or TACASI. Accurate assessment of sensitive topics is particularly important as stigma and discomfort may prevent discussion of these topics during medical visits, particularly for YACS. No formalized procedure for suicidal ideation or sexual health screening exists across survivorship despite increased risk of these late effects in YACS [22, 23, 25]. Findings from the current study represent a clear call to action from survivors to address this gap in care; YACS want and expect providers to ask about suicidal ideation and sexual health. These results should bolster provider confidence that screening for suicidal ideation and sexual health concerns can and should be integrated into clinical care for YACS and that either paper or automated telephone interviews are acceptable methods.
References
American Academy of Pediatrics Section on Hematology/Oncology Children’s Oncology, G. Long-term follow-up care for pediatric cancer survivors. Pediatrics. 2009;123(3):906–15.
Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. Children’s Oncology Group. Published October 2018. Accessed March 2022. http://www.survivorshipguidelines.org/pdf/2018/COG_LTFU_Guidelines_v5.pdf.
Jefford M, et al. Patient-reported outcomes in cancer survivors: a population-wide cross-sectional study. Support Care Cancer. 2017;25(10):3171–9.
Ferreira A, et al. Differential impact of endocrine therapy and chemotherapy on quality of life of breast cancer survivors: a prospective patient-reported outcomes analysis. Ann Oncol. 2019;30(11):1784–95.
Doward LC, McKenna SP. Defining patient-reported outcomes. Value Health. 2004;7:S4–8.
Sudak H, Maxim K, Carpenter M. Suicide and stigma: a review of the literature and personal reflections. Acad Psychiatry. 2008;32(2):136–42.
Blanchard M, Farber BA. “It is never okay to talk about suicide”: patients’ reasons for concealing suicidal ideation in psychotherapy. Psychother Res. 2020;30(1):124–36.
Frederick NN, et al. Barriers and facilitators to sexual and reproductive health communication between pediatric oncology clinicians and adolescent and young adult patients: the clinician perspective. Pediatr Blood Cancer. 2018;65(8):e27087.
Krumpal I. Determinants of social desirability bias in sensitive surveys: a literature review. Qual Quant. 2013;47(4):2025–47.
O’Leary TE, Diller L, Recklitis CJ. The effects of response bias on self-reported quality of life among childhood cancer survivors. Qual Life Res. 2007;16(7):1211–20.
Kobak KA, et al. A computer-administered telephone interview to identify mental disorders. JAMA. 1997;278(11):905–10.
Kobak KA, et al. Computerized assessment of depression and anxiety over the telephone using interactive voice response. MD Comput. 1999;16(3):64–8.
Greist JH, Mundt JC, Kobak K. Factors contributing to failed trials of new agents: can technology prevent some problems? J Clin Psychiatry. 2002;63(Suppl 2):8–13.
Turner CF, et al. Improving epidemiological surveys of sexual behaviour conducted by telephone. Int J Epidemiol. 2009;38(4):1118–27.
Villarroel MA, et al. T-ACASI reduces bias in STD measurements: the national STD and behavior measurement experiment. Sex Transm Dis. 2008;35(5):499–506.
Recklitis CJ, Blackmon JE, Chang G. Screening young adult cancer survivors for distress with the distress thermometer: comparisons with a structured clinical diagnostic interview. Cancer. 2016;122(2):296–303.
Recklitis CJ, Blackmon JE, Chang G. Validity of the Brief SymptomInventory-18(BSI-18)for identifying depression and anxiety in youngadult cancer survivors: comparison with a structured clinical diagnosticinterview. Psychol Assess. 2017;29:1189.
Recklitis CJ, Blackmon JE, Chang G. Screening young adult cancersurvivors with the PROMIS Depression Short Form (PROMIS-D-SF):comparison with a structured clinical diagnostic interview. Cancer. 2020;126:1568–75.
Recklitis CJ, et al. Validating the patient-reported outcomes measurement information system short form v1. 0–anxiety 8a in a sample of young adult cancer survivors: comparison with a structured clinical diagnostic interview. Cancer. 2021;127(19):3691–7.
Zhou ES, et al. Identifying suicidal symptoms in prostate cancer survivors using brief self-report. J Cancer Surviv. 2015;9(1):59–67.
Flynn KE, et al. Development of the NIH PROMIS® sexual function and satisfaction measures in patients with cancer. J Sex Med. 2013;10(Supplement 1):43–52.
Brinkman TM, et al. Suicide ideation and associated mortality in adult survivors of childhood cancer. Cancer. 2014;120(2):271–7.
Gunnes MW, et al. Suicide and violent deaths in survivors of cancer in childhood, adolescence and young adulthood-a national cohort study. Int J Cancer. 2017;140(3):575–80.
Recklitis CJ, et al. Suicide ideation in adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2010;28(4):655–61.
Cherven B, et al. Sexual health among adolescent and young adult cancer survivors: a scoping review from the Children’s Oncology Group Adolescent and Young Adult Oncology Discipline Committee. CA Cancer J Clin. 2021;71(3):250–63.
Coons SJ, et al. Capturing patient-reported outcome (PRO) data electronically: the past, present, and promise of ePRO measurement in clinical trials. Patient-Patient-Centered Outcome Res. 2015;8(4):301–9.
Bajaj P, et al. Screening for suicidal thoughts in primary care: the views of patients and general practitioners. Ment Health Fam Med. 2008;5(4):229.
Funding
This research was supported by the National Cancer Institute (R21CA161315; Recklitis). In addition, Dr. Chevalier’s effort was supported by Swim Across America.
Author information
Authors and Affiliations
Contributions
Lydia L. Chevalier: formal analysis, writing—original draft, writing—review and editing, visualization. Jaime E. Blackmon: formal analysis, data curation, writing—original draft, writing—review and editing, visualization. Sharon L. Bober: conceptualization, methodology, writing—original draft, writing—review and editing, visualization. Anthony Roman: methodology, resources, data collection, program coding and development, data management. Grace Chang: conceptualization, methodology, investigation, writing—review and editing, visualization. Christopher J. Recklitis: conceptualization, methodology, formal analysis, investigation, resources, writing—original draft, writing—review and editing, visualization, supervision, project administration, and funding acquisition.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chevalier, L.L., Blackmon, J.E., Bober, S.L. et al. Evaluating sensitive symptoms in young adult cancer survivors: acceptability of suicidal ideation and sexual health items across administration modes. J Cancer Surviv 18, 450–456 (2024). https://doi.org/10.1007/s11764-022-01237-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-022-01237-5