Abstract
Purpose
The aim of the study was to investigate overall patterns in labour market affiliation, risk for permanently reduced work ability and prevalence of long-term sickness absence among women diagnosed with gynaecological cancer.
Methods
We followed 8451 women diagnosed with ovarian, endometrial or cervical cancer, and 72,311 women with no history of cancer in nationwide registers for up to 19 years (mean 7.5 years). We computed hazards ratios for permanently reduced working ability and annual proportions of long-term sick leave.
Results
Patterns of labour market affiliation varied by cancer diagnosis and stage. The hazard of permanently reduced working ability was increased for survivors of all three cancers but most pronounced for women diagnosed with advanced ovarian cancer. The highest hazard ratios were found 2–5 years after diagnosis, and they persisted for years in all groups and throughout the follow-up period of 19 years in women diagnosed with advanced cervical cancer. In the subgroups of women who continued to be potentially active on the labour market, long-term sick leave was more prevalent among cancer survivors than women with no history of cancer up to 10 years after diagnosis.
Conclusions
Women diagnosed with localised as well as advanced gynaecological cancer are at prolonged risk for permanently reduced working ability and long-term sick leave.
Implications for Cancer Survivors
Gynaecological cancer can have long-term as well as permanent consequences for working ability, and survivors who remain active on the labour market might have to take more sick leave even years after cancer diagnosis than other women at their age.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately half of women with gynaecological cancer are of working age at the time of diagnosis [1]. Almost all are treated surgically, some more extensively (ovarian cancer) than others (endometrial cancer). Patients with advanced disease also undergo adjuvant chemo- and/or radiotherapy. The duration of treatment varies widely from relatively minor surgical procedures as for example conisation (localised cervical cancer) to surgery followed by adjuvant treatment over several months or palliative treatment until end of life [2,3,4], leading to varying expected duration of sick leave in relation to treatment. However, all treatment modalities may cause late effects that are likely to interfere with their daily and working lives on a long-term basis. A recently published review of 55 studies on late effects following gynaecological cancer showed that the women might struggle with menopausal symptoms, bowel and urinary tract complications, lymphedema, pelvic pain and fear of recurrence. These complications are experienced in a time span from shortly after treatment to decades later [5]. Furthermore, we have published a register-based study among 16,833 women diagnosed with gynaecological cancers between 1998 and 2013, and 138,888 reference women showing increased risk for use of antidepressants up to 19 years after the cancer diagnosis [6].
Several large register-based cohort studies that have investigated work-related outcomes among cancer patients have shown that women diagnosed with a gynaecological cancer are at increased risk of disability pension [7, 8], long-term sick leave [9, 10], unemployment [11] or reduced earnings [12]. However, in these studies, women diagnosed with gynaecological cancer represented only small subgroups of the study population.
Most previous studies on women with gynaecological cancer were cross-sectional [13, 14], did not include a reference cohort or had small samples and short follow-up [15]. A recent Swedish population-based cohort study of 1971 cervical cancer patients showed an increased risk of lost workdays due to sick leave and disability pension up to 8 years after diagnosis [16]. To our knowledge, no similar study has been published on women diagnosed with endometrial or ovarian cancer, and no studies have been published in which localised and advanced disease were distinguished, although the treatment and prognoses in these groups differ. Consequently, still little is known about the long-term working ability of women who have had gynaecological cancer. Such knowledge is important for health professionals who provide care, support and work-related guidance to women diagnosed with gynaecological cancer.
The aim of this nationwide, register-based study was to investigate overall patterns of labour market affiliation, risk for permanently reduced working ability and the prevalence of long-term sick leave among women diagnosed with gynaecological cancer.
Methods
We performed a nationwide register-based cohort study with up to 19 years of follow-up. This was possible, since all residents of Denmark are assigned a unique personal identification number (CPR number). Individual information is kept under this identification number in all Danish national registries, which enables linkage of information between the registers at the level of the individual [17].
Study population
We used the Danish Cancer Register to establish a population of all women resident in Denmark aged 30–61 years, in whom ovarian cancer (ICD10: C56, C570-C574), endometrial cancer (ICD10: C54-C55, C58) or cervical cancer (ICD10: C53) had been diagnosed between 1998 and 2014, and who had no previous history of cancer (except for non-melanoma skin cancer). These age limitations were chosen since we wanted to focus on individuals who had completed their education, and further, the women should potentially have some years left on the labour market. This national Register contains almost complete data on all cancer cases in the Danish population since 1943, providing data on stage of disease, previous cancer history and new incident cancers during follow-up for all the women [18].
Women on disability pension or in wage-subsidised employment at the time of cancer diagnosis were excluded, leaving all women who were potentially active members of the labour market for inclusion. Each woman was individually matched on month and year of birth to 10 women with no history of cancer. The unexposed women were sampled randomly from the Danish Civil Registration System and assigned the same entry date (“index date”) as the date of diagnosis of cancer in the exposed woman to whom they were matched. From this register, we also obtained information on emigration and death [19].
All women were followed until they had permanently reduced working ability or one of the following censoring events: new diagnosis of primary cancer, emigration, death, permanent withdrawal from the labour market due to age or 31 December 2016, whichever occurred first.
Comorbidity and socioeconomics
Information on pre-existing diseases was obtained from the National Patient Register, which holds information on diagnoses at all hospital contacts in Denmark since 1978 [20]. Based on these data, we calculated the Charlson Comorbidity Index (CCI) that includes 19 different medical conditions, each weighted according to its potential to impact on mortality. The index is the sum of these weights (from 0 to 6). A higher CCI score indicates an increased severity of comorbid condition [21, 22]. We applied data on use of at least one prescription for antidepressant medication (group N06A of the Anatomical Therapeutic Chemical (ATC) classification system) in the 3 years before cancer diagnosis as a proxy for psychological comorbidity. This information was obtained from the National Prescription Register, which contains high quality individual-level information on all prescription drugs sold in Danish pharmacies since 1994 [23].
Statistics Denmark provided data on cohabitation status and educational level [24].
Labour market affiliation
Denmark has a high level of social security that covers all citizens. Individuals that are permanently unable to work due to physical or mental disability are supported financially through public transfer payments. Further, the entire population is included in the public sickness absence benefit programme, which covers both work-related and non-work-related reasons for sickness absence [25, 26]. The country is divided into 98 municipalities. These municipalities function as local authorities, and they administer all public transfer payments.
Information on labour market affiliation was obtained from the Danish Register for Evaluation of Marginalisation (DREAM), which contains unique information on all public transfer payments to Danish citizens on a weekly basis [27, 28].
The primary outcome of this study was permanently reduced working ability, which we defined as being granted either wage-subsidised employment (flex job) or a disability pension. To be granted wage-subsidised employment in Denmark, working ability must be permanently reduced to a level that prevents the individual from working in an ordinary job, by means that there is a permanent requirement for reduced working hours and tailored job tasks. Wage-subsidised employment is granted by the municipal authorities. It is initially granted for 5 years after which it becomes a permanent solution if needed [29]. Disability pension is granted by the municipal authorities if working ability is reduced permanently to an extent that prevents return to work. All the options available for improving the individual’s participation in the labour market, through rehabilitation, treatment or wage-subsidised employment, must have been considered before a disability pension is granted [26]. The acts on wage-subsidised employment and disability pension were reformed 1 January 2013 with the aim of maintaining people with reduced work ability on the labour market. This lead to a decrease in the number of individuals being granted disability pension and an increase in number of individuals being granted wage-subsidised employment [30].
The secondary outcome was long-term sick leave among women who were still potentially active in the labour market. This was defined as more than 4 consecutive weeks of part- or full-time sick leave, as the first 30 days of sick leave are usually paid by the employer, and therefore not consistently registered in DREAM [25].
During the study period (1998–2016), all Danish residents were eligible for old age pension from the age of 65 years [26], and further, if they fulfilled specific criteria, they were able to retire already at 60–61 years of age [31].
Statistical analysis
All analyses were carried out separately for data on women diagnosed with localised or advanced ovarian, endometrial or cervical cancer. Information on education or stage of disease was missing for some women. All analyses were conducted as complete case analyses, resulting in different numbers of individuals in the tables and figures.
To illustrate timewise differences in labour market participation, status proportion plots were computed from 1 year before cancer diagnosis or index date to 5 years after.
Using a competing risk approach, we also examined the primary reasons for leaving the labour market (permanently reduced working ability, old age pension or death). A survival model incorporating the three outcomes simultaneously was fitted, and the cumulative incidence function for each cause was calculated.
We used the Cox proportional hazards regression analyses to compare the hazard of permanently reduced working ability among exposed and unexposed women. Overall analyses were performed for the entire follow-up period and separate estimates by time since diagnosis. The analyses were stratified by age, calendar period and amount of sick leave the year before cancer diagnosis, and were further adjusted for educational level and physical comorbidity. As death is an important competing event to work-related outcomes, we also calculated hazard ratios for death as an outcome.
The Cox proportional hazards regression was used to investigate risk factors for permanently reduced working ability among exposed women. All covariates in the model were mutually adjusted (age, cohabitation status, educational level, physical and psychological comorbidity, stage of disease), and further stratified by calendar period and amount of long-term sick leave the year before cancer diagnosis. The proportional hazards assumption was evaluated by tests based on the Schoenfeld residuals and by assessing log-minus-log survivor curves.
We calculated the annual prevalence of long-term sick leave by using the number of weeks in which the women were potentially active in the labour market (not dead, emigrated or permanently withdrawn from working life due to age or disability) as the denominator and the number of weeks on long-term sick leave (> 4 weeks) as the numerator.
Results
We included 8451 exposed women with ovarian (N = 2536), endometrial (N = 2522) and cervical cancer (N = 3393), and 72,311 age-matched unexposed women potentially affiliated to the labour market (Fig. 1 and Table 1).
Figure 2 shows a descriptive overview of the weekly proportional distributions of labour market affiliation and death from 1 year before until 5 years after diagnosis. Overall, the patterns are similar for women with localised and advanced disease in the three cancer subgroups, with a high proportion of long-term sick leave at the time of diagnosis, decreasing strongly during the first 2 years after diagnosis and less strongly during the next 3 years. The proportions of women with permanently reduced working ability appeared to increase more rapidly in all six exposure groups than among the unexposed women in the years after diagnosis (Fig. 2).
Status proportion plots visualising proportions of different labour market affiliations according to years since diagnosis (index date for unexposed women) for 7774 women diagnosed with localised or advanced ovarian, endometrial or cervical cancer and 72,311 age-matched unexposed women (individuals for whom information on stage of disease was missing were not included)
Permanently reduced working ability
The risk of leaving the regular labour market due to permanently reduced working ability, old age pension or death differed widely by cancer diagnosis and stage of disease (Fig. 3). Fifteen years after diagnosis, 94% of women who had been diagnosed with advanced ovarian cancer had left the labour market, mostly due to death but 38% due to permanently reduced working ability; the respective proportions were 74% and 22% of women diagnosed withlocalised ovarian cancer. Of the women diagnosed with advanced endometrial cancer, 90% had left the labour market 15 years after diagnosis, mostly due to death or old age pension but 20% due to permanently reduced working ability; the respective proportions were 88% and 12% in women who have had localised endometrial cancer. Of the women who had been diagnosed with advanced cervical cancer, 80% had left the labour market 15 years after diagnosis, 34% due to permanently reduced working ability and the respective proportions were 41% and 19% for women who have had localised cervical cancer (Fig. 3).
Probability of exit (time to first event) from the labour market due to permanently reduced work ability, age pension or death by stage of disease among 7774 women diagnosed with localised or advanced ovarian, endometrial or cervical cancer and 72,311 age-matched unexposed women (individuals for whom information on stage of disease were missing were not included)
In multivariate analyses, women with localised as well as advanced disease in all three diagnostic groups had an overall significantly increased hazard of permanently reduced working ability compared with the unexposed women (Table 2). The hazard ratios were higher among women with advanced disease than among those with localised disease. Women with ovarian cancer constituted the group with the highest risk. Two to 5 years after diagnosis, they had an almost 19 times higher hazard of permanently reduced working ability than the unexposed women (HR 18.72, 95% CI 16.04–21.84). The hazard was seven times higher (HR 7.23, 95% CI 4.75–11.01) among women with advanced endometrial cancer and nearly ten times higher (HR 9.51, 95% CI 7.53–12.02) among women with advanced cervical cancer than the unexposed women. The increased hazard of permanently reduced working ability decreased slightly during subsequent years but persisted throughout the follow-up period of 19 years among women who had been diagnosed with advanced cervical cancer, 10 years among women diagnosed with localised as well as advanced ovarian cancer and 5 years for women who had been diagnosed with all stages of endometrial cancer or localised cervical cancer (Table 2).
These analyses were also conducted for wage-subsidised employment and disability pension separately and showed similar patterns (Supplementary Table 1).
Factors associated with permanently reduced working ability
A diagnosis of advanced disease was the factor most strongly associated with permanently reduced working ability. In all three groups, we found a stepwise higher hazard of permanently reduced working ability with lower level of education. Older age, living alone and physical or psychological comorbidity were also associated with an increased hazard of permanently reduced working ability (Supplementary Table 2).
Long-term sick leave
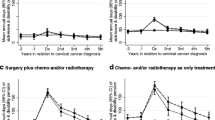
The annual prevalence of long-term sick leave was calculated only for the subgroups of women who were potentially active on the labour market at some time during the year in question. Long-term sick leave was most prevalent in the first year after cancer diagnosis and decreased subsequently (Fig. 4). In the subgroups of women who were potentially active on the labour market during the 10th year, however, those who have had localised ovarian cancer (N = 145) or advanced cervical cancer (N = 310) still had significantly more long-term sick leave than the unexposed women. Thus, of the women who have had localised ovarian cancer, 13% had long-term sick leave at some time during the 10th year, whereas the proportion was 9% among unexposed women. For advanced cervical cancer, the proportion was 15%, while for the unexposed women, it was 10% (Fig. 4).
Annual percentages of women who had long-term sick leave (> 4 weeks) at some time each year (2 years before and up to 10 years after the date of cancer diagnosis or study entry) among those who were potentially active on the labour market. The patterned areas of the columns illustrate the proportions among unexposed women. The years in which the proportions differed significantly between exposed and unexposed women are marked with red stars. Numbers of women who were potentially active on the labour market at some time during the year (and included in this Figure): Year 1, localised ovarian cancer, n = 1073 (100%); advanced ovarian cancer, n = 1257 (100%); localised endometrial cancer, n = 1979 (100%); advanced endometrial cancer, n = 296 (100%); localised cervical cancer, n = 2459 (100%); advanced cervical cancer, n = 703 (100%). Year 3, localised ovarian cancer, n = 849 (79%); advanced ovarian cancer, n = 684 (54%); localised endometrial cancer, n = 1700 (86%); advanced endometrial cancer, n = 184 (55%); localised cervical cancer, n = 2272 (92%); advanced cervical cancer, n = 436 (62%). Year 5, localised ovarian cancer, n = 635 (59%); advanced ovarian cancer, n = 332 (26%); localised endometrial cancer, n = 1308 (66%); advanced endometrial cancer, n = 109 (36%); localised cervical cancer, n = 1942 (79%); advanced cervical cancer, n = 310 (44%). Year 10, localised ovarian cancer, n = 285 (27%); advanced ovarian cancer, n = 145 (11%); localised endometrial cancer, n = 435 (22%); advanced endometrial cancer, n = 46 (15%); localised cervical cancer, n = 1112 (45%); advanced cervical cancer, n = 149 (21%)
Discussion
This first comprehensive, long-term overview of the labour market affiliation of women diagnosed with gynaecological cancer shows that they are at long-term increased risk for permanently reduced working ability and long-term sick leave. The magnitude of the effect differed widely by cancer and stage of disease but was most pronounced for women who had been diagnosed with advanced ovarian or cervical cancer. Nevertheless, localised as well as advanced gynaecological cancer had long-term consequences for working ability.
Previous studies on the risk for permanently reduced working ability addressed only disability pension. A large Danish register-based cohort study with up to 21 years of follow-up showed an overall increased risk for receiving a disability pension for women diagnosed with ovarian (RR 2.47, 95 % CI 2.2–2.7) or cervical cancer (RR 1.27, 95 % CI 1.2–1.4) and not for women with endometrial cancer, as compared with cancer-free controls [7]. Like us, they found that the risk for disability pension was higher 1–3 years after diagnosis than during the first year; however, their risk estimates were lower than ours, perhaps due to methodological differences, as we had access to weekly information on labour market affiliations, whereas the previous study only had annual information [7].
We were able to investigate risk for reduced working ability in women diagnosed with both localised and advanced gynaecological cancer. This is an important feature, as stage of disease is strongly correlated with treatment and prognosis. Previous studies on other cancer types have found both poor prognosis and treatment with chemotherapy to be associated with not returning to work [32, 33]. Further, a recently published Swedish population-based cohort study of 1971 cervical cancer patients provided results according to treatment type. Like us, they found that women treated for a higher stage of disease had a higher risk of receiving disability pension than cancer-free women. Those who underwent conisation or trachelectomy did not have increased risk, whereas women treated by hysterectomy had a slightly increased risk, and those treated with adjuvant therapy had the highest risk of receiving a disability pension [16]. The mechanisms behind stage of disease and adjuvant treatment as important risk factors of reduced work ability may to some extent be explained by the burden of late effects. Qualitative as well as quantitative studies have documented that physical and psychological late effects following cancer are some of the most important barriers for returning to work and for functioning at work [34,35,36].
Although we found increased risk for permanently reduced work ability among women who had been diagnosed with a gynaecological cancer, a considerable proportion of these women, particularly those who have had localised cervical cancer, had a good chance of remaining active on the labour market. Nevertheless, they still experienced significantly more long-term sick leave 5 years after their diagnosis than the age-matched unexposed women. A Norwegian study of 244 women diagnosed with gynaecological cancer also found an increased risk of sick leave 5 years after the diagnosis; however, this was found only for women with endometrial cancer and not for those with cervical or ovarian cancer [10]. The difference from our results might be due to different definitions of sick leave. In the Norwegian study, sick leave was defined as more than 16 days (part- or full-time absence), whereas we defined it as more than 4 consecutive weeks of part- or full-time sick leave. The combination of the results of the two studies might imply that women diagnosed with cervical or ovarian cancer are at increased risk of long-term sick leave, whereas women diagnosed with endometrial cancer are at higher risk of shorter periods of sick leave than other women at same age.
The reasons for work-related consequences of gynaecological cancer have not been investigated extensively. The main causes are suggested to be symptoms and late effects of treatment. A cross-sectional study of 104 gynaecological cancer survivors in the USA showed that those who had received radiotherapy were more likely to experience limitations in physical work-related activities after treatment, while women who had received chemotherapy more often reported challenges in psychological job tasks, such as concentration [13]. In line with this, we found that having had advanced disease was the factor most strongly associated with permanently reduced working ability. A qualitative study of 55 women with gynaecological cancer showed that they had unrealistic expectations of returning to full employment shortly after treatment [37]. This indicates that gynaecological cancer survivors should be supported in adjusting and managing their expectations of return to work.
Strengths and limitations
One of the major strengths of this study is the use of high quality data from registers established independently of the study hypothesis, with continuous weekly updates on outcome and censoring variables throughout the study period. This allowed us to obtain unique results on the long-term working ability of women diagnosed with gynaecological cancer.
The limitations of the study include lack of detailed information on cancer treatment, which is probably associated with the risks for both long-term sick leave and permanently reduced working ability. However, as stage of disease and treatment are closely related, we assume that any effect of treatment would be included in the association found between stage of disease and working status. Furthermore, we had no access to data on disease status (complete remission or recurrence), which would probably also affect labour market affiliation. We were not able to include patient-reported information. It could have been relevant to include information on reasons for leaving the labour market, or motivations to stay at work (for example, concerns about the ability to provide for the family). Unfortunately, we had missing values on stage of disease in 7–10 % of the patients (depending on cancer cite). These patients were not included in the analyses, and since we do not know if this information was missing at random, it may have biased the absolute estimates. Through the follow-up period, different labour market policy reforms have been carried out, which means that terms for different public transfer payments have varied. Further, treatment guidelines have chances over time. We took this into account by stratifying our analyses on calendar time, meaning that individuals are only compared within the same period of time. Finally, it is a limitation that the study did not capture short-term sick leave of 4 weeks or less.
Conclusion
Women diagnosed with localised as well as advanced gynaecological cancer are at prolonged risk for permanently reduced working ability and long-term sick leave. The work-related consequences are most pronounced among women diagnosed with advanced ovarian or cervical cancer.
The results of our study could inform health professionals and social workers about the work-related challenges faced by women who have had a gynaecological cancer. The results may also contribute to the formulation of employer policies to improve communication and to accommodate return to work for these women.
References
Engholm G, Ferlay J, Christensen N, Bray F, Gjerstorff ML, Klint A, et al. NORDCAN – a Nordic tool for cancer information, planning, quality control and research. Acta Oncol. 2010;49(5):725–36. https://doi.org/10.3109/02841861003782017.
The Danish Health Authority. Pakkeforløb for kraeft i aeggestokkene (in Danish) (National Ovarian Cancer Pathway). 2019. https://www.sst.dk/-/media/Udgivelser/2019/Pakkeforloeb-kraeft-2015-2019/AEggestokkene-2019/Pakkeforloeb-for-kraeft-i-aeggestokkene.ashx?la=da&hash=90133A54680DD62EA2A6200B187C51774444DBFD. Accessed 14 April 2020
The Danish Health Authority. Pakkeforløb for livmoderhalskraeft (in Danish) (National Cervical Cancer Pathway). 2019. https://www.sst.dk/-/media/Udgivelser/2019/Pakkeforloeb-kraeft-2015-2019/Livmoderhalskraeft-2019/Pakkeforloeb-for-livmoderhalskraeft.ashx?la=da&hash=5D85BB09AAC54123E5013B552B22E0920C9CF7D8. Accessed 14 April 2020
The Danish Health Authority. Pakkeforløb for kraeft i livmoderen (in Danish (National Endometrial Cancer Pathway). 2018. https://www.sst.dk/-/media/Udgivelser/2019/Pakkeforloeb-kraeft-2015-2019/Livmoderen-2019/Pakkeforloeb-for-kraeft-i-livmoderen.ashx?la=da&hash=7C7966715635AF6270F8ADE26FAD0F80D83062AA. Accessed 14 April 2020
Sekse RJT, Dunberger G, Olesen ML, Osterbye M, Seibaek L. Lived experiences and quality of life after gynaecological cancer-an integrative review. J Clin Nurs. 2019;28(9-10):1393–421. https://doi.org/10.1111/jocn.14721.
Horsboel TA, Kjaer SK, Johansen C, Suppli NP, Ammitzboll G, Froding LP, et al. Increased risk for depression persists for years among women treated for gynecological cancers - a register-based cohort study with up to 19 years of follow-up. Gynecol Oncol. 2019;153(3):625–32. https://doi.org/10.1016/j.ygyno.2019.03.259.
Carlsen K, Oksbjerg Dalton S, Frederiksen K, Diderichsen F, Johansen C. Cancer and the risk for taking early retirement pension: a Danish cohort study. Scand J Public Health. 2008;36(2):117–25. https://doi.org/10.1177/1403494807085192.
Taskila-Abrandt T, Pukkala E, Martikainen R, Karjalainen A, Hietanen P. Employment status of Finnish cancer patients in 1997. Psycho-oncology. 2005;14(3):221–6. https://doi.org/10.1002/pon.838.
Gudbergsson SB, Torp S, Flotten T, Fossa SD, Nielsen R, Dahl AA. A comparative study of cancer patients with short and long sick-leave after primary treatment. Acta Oncol. 2011;50(3):381–9. https://doi.org/10.3109/0284186X.2010.500298.
Torp S, Nielsen RA, Gudbergsson SB, Fossa SD, Dahl AA. Sick leave patterns among 5-year cancer survivors: a registry-based retrospective cohort study. J Cancer Surviv. 2012;6(3):315–23. https://doi.org/10.1007/s11764-012-0228-8.
Carlsen K, Dalton SO, Diderichsen F, Johansen C. Risk for unemployment of cancer survivors: a Danish cohort study. Eur J Cancer. 2008;44(13):1866–74. https://doi.org/10.1016/j.ejca.2008.05.020.
Syse A, Tretli S, Kravdal O. Cancer's impact on employment and earnings--a population-based study from Norway. J Cancer Surviv. 2008;2(3):149–58. https://doi.org/10.1007/s11764-008-0053-2.
Nachreiner NM, Shanley R, Ghebre RG. Cancer and treatment effects on job task performance for gynecological cancer survivors. Work. 2013;46(4):433–8. https://doi.org/10.3233/wor-131752.
Nakamura K, Masuyama H, Nishida T, Haraga J, Ida N, Saijo M, et al. Return to work after cancer treatment of gynecologic cancer in Japan. BMC Cancer. 2016;16:558. https://doi.org/10.1186/s12885-016-2627-0.
Nachreiner NM, Ghebre RG, Virnig BA, Shanley R. Early work patterns for gynaecological cancer survivors in the USA. Occup Med (Oxf). 2012;62(1):23–8. https://doi.org/10.1093/occmed/kqr177.
Everhov AH, Ekberg S, Hirschberg AL, Bergmark K, Radestad AF, Glimelius I, et al. Lost workdays in uterine cervical cancer survivors compared to the general population: impact of treatment and relapse. J Cancer Surviv. 2016;10(3):514–23. https://doi.org/10.1007/s11764-015-0496-1.
Erlangsen A, Fedyszyn I. Danish nationwide registers for public health and health-related research. Scand J Public Health. 2015;43(4):333–9. https://doi.org/10.1177/1403494815575193.
Gjerstorff ML. The Danish Cancer Registry. Scand J Public Health. 2011;39(7 Suppl):42–5. https://doi.org/10.1177/1403494810393562.
Pedersen CB. The Danish Civil Registration System. Scand J Public Health. 2011;39(7 Suppl):22–5. https://doi.org/10.1177/1403494810387965.
Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39(7 Suppl):30–3. https://doi.org/10.1177/1403494811401482.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. https://doi.org/10.1016/0021-9681(87)90171-8.
de Groot V, Beckerman H, Lankhorst GJ, Bouter LM. How to measure comorbidity. A critical review of available methods. J Clin Epidemiol. 2003;56(3):221–9. https://doi.org/10.1016/s0895-4356(02)00585-1.
Kildemoes HW, Sorensen HT, Hallas J. The Danish National Prescription Registry. Scand J Public Health. 2011;39(7 Suppl):38–41. https://doi.org/10.1177/1403494810394717.
Jensen VM, Rasmussen AW. Danish Education Registers. Scand J Public Health. 2011;39(7 Suppl):91–4. https://doi.org/10.1177/1403494810394715.
The Ministry of Employment. Bekendtgørelse af lov om sygedagpenge (in Danish) (Act on sickness absence benefits). 2019. https://www.retsinformation.dk/pdfPrint.aspx?id=206429. Accessed 14 April 2020.
The Ministry of Employment. Bekendtgørelse af lov om social pension (in Danish) (Act on social pensions). 2017. https://www.retsinformation.dk/pdfPrint.aspx?id=194457. Accessed 14 April 2020.
Hjollund NH, Larsen FB, Andersen JH. Register-based follow-up of social benefits and other transfer payments: accuracy and degree of completeness in a Danish interdepartmental administrative database compared with a population-based survey. Scand J Public Health. 2007;35(5):497–502. https://doi.org/10.1080/14034940701271882.
Stapelfeldt CM, Jensen C, Andersen NT, Fleten N, Nielsen CV. Validation of sick leave measures: self-reported sick leave and sickness benefit data from a Danish national register compared to multiple workplace-registered sick leave spells in a Danish municipality. BMC Public Health. 2012;12:661-2458-12-661. https://doi.org/10.1186/1471-2458-12-661.
The Ministry of Employment. Bekendtgørelse om fleksjob (in Danish) (Act on wage subsidised employment). 2017. https://www.retsinformation.dk/pdfPrint.aspx?id=186386. Accessed 14 April 2020.
The Ministry of Employment. Evaluering af reform af førtidspension og fleksjob: hovedrapport (in Danish) (Evaluation of the reform of disability pension and wage subsidised employment). 2018. https://bm.dk/media/6576/hovedrapport_foep_fleks-pdf.pdf. Accessed 14 April 2020.
The Ministry of Employment. Bekendtgørelse om overgang til efterløn samt beregning og udbetaling af efterløn (in Danish) (Act on early retirement pension). 2018. https://www.retsinformation.dk/pdfPrint.aspx?id=205646. Accessed 14 April 2020.
de Boer AG, Torp S, Popa A, Horsboel T, Zadnik V, Rottenberg Y, et al. Long-term work retention after treatment for cancer: a systematic review and meta-analysis. J Cancer Surviv. 2020;14:135–50. https://doi.org/10.1007/s11764-020-00862-2.
Arndt V, Koch-Gallenkamp L, Bertram H, Eberle A, Holleczek B, Pritzkuleit R, et al. Return to work after cancer. A multi-regional population-based study from Germany. Acta Oncol. 2019;58(5):811–8. https://doi.org/10.1080/0284186X.2018.1557341.
Duijts SF, van Egmond MP, Spelten E, van Muijen P, Anema JR, van der Beek AJ. Physical and psychosocial problems in cancer survivors beyond return to work: a systematic review. Psychooncology. 2014;23(5):481–92. https://doi.org/10.1002/pon.3467.
Fitch MI, Nicoll I. Returning to work after cancer: survivors’, caregivers’, and employers’ perspectives. Psychooncology. 2019;28(4):792–8. https://doi.org/10.1002/pon.5021.
Dorland HF, Abma FI, Roelen CAM, Smink JG, Ranchor AV, Bultmann U. Factors influencing work functioning after cancer diagnosis: a focus group study with cancer survivors and occupational health professionals. Support Care Cancer. 2016;24(1):261–6. https://doi.org/10.1007/s00520-015-2764-z.
Grunfeld EA, Cooper AF. A longitudinal qualitative study of the experience of working following treatment for gynaecological cancer. Psychooncology. 2012;21(1):82–9. https://doi.org/10.1002/pon.1874.
Acknowledgements
The authors would like to acknowledge Anja Krøyer for thorough data management.
Funding
The study was supported by funding from The Mermaid Project (Mermaid3), The Danish Health Foundation (16-B-0039) and the Danish Cancer Society (R134-A8448-15-S42).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 22 kb)
Rights and permissions
About this article
Cite this article
Horsbøl, T.A., Dalton, S.O., Ammitzbøll, G. et al. Gynaecological cancer leads to long-term sick leave and permanently reduced working ability years after diagnosis. J Cancer Surviv 14, 867–877 (2020). https://doi.org/10.1007/s11764-020-00899-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-020-00899-3