Abstract
Purpose
This study aims to examine literature on effectiveness of low-level laser therapy (LLLT) in reducing limb volume and pain in adults with breast cancer-related lymphedema (BCRL).
Methods
PubMed, PEDro, CINAHL, and Cochrane databases were searched using (lymphedema OR edema OR swelling) AND (breast cancer OR mastectomy) AND (laser OR low-level laser therapy OR LLLT OR cold laser). Intervention studies or meta-analyses reporting LLLT for BCRL were included in the search. Pooled effect sizes (ES) and 95 % confidence intervals (CI) were calculated for volume and pain. No limitations were placed on length of follow-up, publication year, or language. Final search was conducted on October 16, 2014.
Results
Nine studies met criteria for inclusion. Within-group pooled ES for volume (six studies) was −0.52 (−0.78, −0.25), representing a 75.7-ml reduction in limb volume after LLLT. Between-group pooled ES for volume (four studies) was −0.62 (−0.97, −0.28), representing a 90.9-ml greater reduction in volume with treatment including LLLT versus not including LLLT. Within-group pooled ES for pain reduction (three studies) was −0.62 (−1.06, −0.19), pain reduction of 13.5 mm (0–100 mm VAS). Between-group pooled ES for pain reduction (two studies) was non-significant at −1.21 (−4.51, 2.10).
Conclusion
Moderate-strength evidence supports LLLT in the management of BCRL, with clinically relevant within-group reductions in volume and pain immediately after conclusion of LLLT treatments. Greater reductions in volume were found with the use of LLLT than in treatments without it.
Implications for Cancer Survivors
LLLT confers clinically meaningful reductions in arm volume and pain in women with BCRL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rationale and background
Breast cancer treatments may damage lymph vessels and nodes, resulting in impaired lymph transport capacity and accumulation of protein-rich interstitial fluid in the torso or upper extremity (UE). Up to one in five women will develop UE lymphedema after breast cancer treatment [1]. Women with breast cancer-related lymphedema (BCRL) experience more pain, poorer UE mobility, poorer quality of life, and greater restrictions in activity than women without BCRL [2–5]. Other complications of chronic BCRL include cellulitis or lymphangitis, axillary vein thrombosis, and lymphangiosarcoma [6]. The current standard of care for BCRL is complete decongestive therapy (CDT), consisting of compressive bandaging, exercise, manual lymphatic drainage (MLD), and compression garments [7]. Although often effective in combination, the effectiveness of MLD independent of the other treatments has been called into question. In a 2013 systematic review and meta-analysis, Huang et al. [8] reported variable results across studies; when data were pooled, no statistically significant benefit in volume reduction from MLD alone was found. These comprehensive treatments are time consuming, labor intensive, and costly [9]. Therefore, evaluation of effective, inexpensive, and easily applied alternatives is warranted. Low-level laser therapy (LLLT) as an alternative for treatment of BCRL has been reported in the literature, but there are relatively few studies and no meta-analyses of study findings.
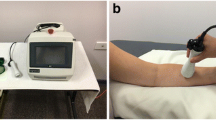
Light Amplification by Stimulated Emission of Radiation (laser) emits concentrated light as a narrow beam. The light goes through optical amplification based on stimulated emission of electromagnetic radiation in the visible to infrared range of wavelengths (670–950 nm) [10, 11]. High power, or “hot lasers,” work by thermal mechanisms and can destroy tissues, making them suitable for surgery but not rehabilitation. Conversely, low power “cold lasers,” typically between 5 and 500 mW, work by non-thermal mechanisms (photochemical reactions) and can be used to deliver energy to tissues for a wide variety of rehabilitation purposes [11]. Cold laser, known as low-level laser therapy, can be applied either by handheld units (contact or non-contact devices) using spot application to specific anatomical surfaces or by scanning units in which LLLT is applied over a larger region [11].
Non-thermal effects of LLLT include stimulation of adenosine triphosphate production, promotion of ribonucleic acid and collagen production, modulation of inflammatory cytokines, inhibition of bacterial growth, promotion of vasodilatation and endothelial regeneration, stimulation of fibroblast activity, alteration of nerve conduction velocity, and promotion of neural regeneration [11]. The proposed mechanisms involve cellular-level changes in response to photon absorption, including alteration of membrane and organelle function and promotion of other reactions that initiate complex sequences of cellular response to aid tissue healing. In early studies on wound healing in mice, Lievens reported acceleration of both vein and lymph vessel regeneration with laser application [12, 13]. More recently, LLLT was found to decrease the expression of pro-fibrotic transforming growth factor and type I collagen deposition in the rat tibialis anterior muscle after muscle lesion, suggesting that LLLT may be helpful in preventing tissue fibrosis [14]. This suggests that LLLT may provide benefit to patients with lymphedema by increasing lymphatic flow through encouragement of lymphangiogenesis, stimulation of lymphatic motoricity, and prevention of tissue fibrosis that could potentially further disrupt lymphatic function.
Systematic reviews evaluating effectiveness of LLLT for BCRL have provided moderate support for its use [15–18]. However, the authors reported heterogeneity in patient baseline characteristics, study designs, treatment regimens and modes of LLLT delivery, and in follow-up times. None has included meta-analyses. Therefore, the magnitude of the effect and relative benefit of LLLT in the treatment of BCRL remains unclear. Since 2012, one additional randomized controlled trial (RCT) has been published and is not included in previous systematic reviews [19].
Objectives
The purpose of this systematic review and meta-analysis is to examine and synthesize the most current literature and address two foreground questions: (1) In adults with BCRL, is LLLT effective in reducing pain and volume? (2) Is LLLT more effective than other interventions that do not include LLLT? Our hypotheses are that treatment with LLLT (1) is effective in reducing pain and limb swelling in patients with BCRL and (2) is more effective than treatments that do not include LLLT.
Methods
Protocol and registration
We did not register the protocol for this review.
Information sources
Two authors (LCL and BS) conducted independent systematic electronic searches of PubMed, Physiotherapy Evidence Database (PEDro), Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Cochrane Library.
Search
Search terms used in PubMed and CINAHL were (lymphedema OR edema OR swelling) AND (breast cancer OR mastectomy) AND (laser OR low-level laser therapy OR LLLT OR cold laser), a combination of MeSH terms and keywords. Recursive searches of relevant articles were also performed. Search terms for PEDro and Cochrane databases were lymphedema AND laser. Search included all available years up through October 16, 2014.
Eligibility criteria
Studies were eligible if they were an intervention study or meta-analysis investigating the use of LLLT alone or in combination with other treatments for BCRL, and they reported on upper extremity swelling and/or pain. If additional studies were identified in existing meta-analyses, the individual studies were evaluated for eligibility and included as individual studies. Studies were excluded if the study population included patients with primary lymphedema or lymphedema/edema secondary to pathology other than breast cancer treatment. Case studies and case reports were excluded from analysis. No limitations were placed on length of follow-up, publication year, or language.
Study selection
Study selection began with independent review of all titles and abstracts identified through initial database searches by two authors (LCL and BS). After identification of relevant studies, duplicates were removed, and recursive search was performed. Remaining records were screened for eligibility, and those meeting study inclusion and exclusion criteria were evaluated further for final inclusion in this systematic review and quantitative synthesis for meta-analysis.
Data abstraction
The authors extracted means and standard deviations for swelling and pain from individual studies when reported. If means and standard deviations were not reported, effect sizes, test statistics, and/or p values were extracted when provided. When data from multiple time points were reported in any one study, data from the follow-up time most similar to those from other studies were selected. When data were reported qualitatively or where data were not sufficient for calculation of effect sizes, the corresponding author of the study was contacted.
Summary measures and synthesis of results
Individual study effect sizes and 95 % confidence intervals (CI) were calculated for pre- to post-intervention changes to determine within-group effects and post-intervention group differences to determine between-groups effects.
The calculated individual study effect sizes were then weighted by their inverse variance. The Q heterogeneity statistic was calculated to determine the most appropriate model for pooling data (random effects or fixed effect model), with p ≤ 0.05 indicating significant heterogeneity necessitating use of the random effects model. For each analysis, the pooled one- or two-group effect size and 95 % CI were then calculated. Data were synthesized and analyzed using Microsoft® Excel® for Mac 2011, Version 14.2.5 statistical software package.
To convert effect sizes back into clinical units, pooled effect sizes were multiplied by the standard deviation of an individual study (pre-test standard deviation for within-group effects sizes and pooled standard deviation for between-groups effect sizes). The result was reported in the measurement units of that study.
Risk of bias in and across studies
The PEDro scale developed by the Australian Physiotherapy Evidence Database (http://www.pedro.org.au) was used to rate the quality of each study and addressed study bias. PEDro scores were compared to those reported in previous systematic reviews when available [15, 16]. Use of funnel plots and/or statistical tests for publication bias (i.e., Eggers or Begg’s test) was planned.
Results
Study selection
The searches in PubMed and CINAHL were done using the terms (lymphedema OR edema OR swelling) AND (breast cancer OR mastectomy) AND (laser OR low-level laser therapy OR LLLT OR cold laser). This yielded 41 studies in PubMed and 12 studies in CINAHL. Using the terms (lymphedema AND laser) yielded ten studies in the PEDro Database and one study in the Cochrane Database. This search identified a total of 64 records as of October 16, 2014 (Fig. 1). To ensure that all relevant studies were identified, we then conducted a second search in PubMed using only the terms lymphedema AND laser. While this search yielded 83 studies, no new studies were found, and there were fewer total relevant studies, so the original PubMed search terms were retained.
Independent review of titles and abstracts plus recursive search of 64 studies was conducted by two authors (LCL and BS). Twenty-seven studies remained after exclusion by non-relevance. One additional study was included through recursive search. Removal of duplicates resulted in 14 studies. One article presented preliminary data from Piller and Thelander [20], which was subsequently reported as follow-up in 1998 [21]. The 1995 report was irretrievable and excluded. Of the remaining 13 studies, four were systematic reviews [15–18] that contained no new records and in which meta-analyses were not conducted; these were therefore excluded. Nine studies remained and were included in this review.
PEDro scores (Table 1) and levels of evidence (Table 2) were assigned independently by two of the authors (LCL and BS). A summary of included studies is presented in Table 2 and the results in Tables 3 and 4. Laser treatment parameters are summarized in Table 5. All studies included measurement of upper extremity total limb volume using either water displacement (volumetry) or circumferential assessment (either with a tape measure or infrared perometry). Three studies [19, 21, 22] also used bioimpedance to assess resistance to electric current as a surrogate measure of interstitial fluid volume. However, only total limb volume measures are included in the current meta-analyses for limb volume changes. Of the five studies that included independent measures of pain, they used either a visual analogue scale or numeric pain rating scale. These pain measures are similar in construct and are appropriate to be combined in pooled analysis.
Summaries of individual studies
Carati et al. 2003
Carati et al. [22] conducted a two-component crossover study. The first was a double-blinded randomized sham (placebo) controlled crossover trial of a nine-session cycle of LLLT (n = 26) versus sham LLLT treatment (n = 27). After one cycle of LLLT, no significant differences in volume were found and no significant differences between groups. The second component of the trial was designed to allow comparison of two cycles of LLLT to one cycle. After completion of the crossover phase, 11 participants from the original sham laser group (unblinded) received a second nine-session cycle of LLLT treatments, and the data were pooled, bringing the number of participants receiving two cycles of active LLLT to 37. No statistically significant reductions from baseline were found in mean affected limb volume after two cycles of LLLT immediately post-treatment (p = 0.442), at 1 month post-treatment (p = 0.119), or at 3 months post-treatment (p = 0.061), although volume was decreased. Compared to the sham group, however, the two-cycle LLLT group demonstrated a significantly greater reduction in mean limb volume at 3 months post-treatment (89.7 ± 46-ml reduction vs. 32.1 ± 3.4-ml increase; p = 0.017). At 2 to 3 months following the second block of LLLT, 31 % of participants had a clinically significant reduction (>200 ml) in affected limb volume, compared to 4 % in the sham group (p = 0.01). Pain was not reported as an independent outcome.
Dirican et al. 2011
This single-group pre-test/post-test study [23] investigated the effect of LLLT on 17 women with BCRL. All patients used compression garments or bandaging, and two used a pneumatic pump during the course of the study intervention. The LLLT protocol was modeled on the protocol used by Carati et al. [22] without the crossover component and with no control group. The authors concluded that LLLT improved volume and pain when used as an adjunct to conventional treatments. All participants experienced a decrease in affected UE circumference as compared to the unaffected UE with a mean decrease of 54 % (±27 %) after initial block of treatment and 73 % (±24 %) after both blocks. Fourteen of 17 participants reported pain decrease of >40 % with a mean of 63 %. Three participants reported no improvement.
Kaviani et al. 2006
Kaviani et al. [24] conducted a small (n = 11) double-blinded, RCT comparing 2 cycles of LLLT to 2 cycles of sham laser in patients with a ≥3-month history of unilateral post-mastectomy lymphedema. Only four patients in each group completed both cycles. Each cycle consisted of three treatments per week, with an 8-week hiatus between cycles. The authors reported that the total reduction in limb circumference was greater in the laser group than in the placebo group at all assessment points, except at week 22 (8 weeks post-intervention), suggestive of transient improvement in limb volume. Pain score reduction was greater in the LLLT group, except at weeks 3 and 9. The authors report that in spite of favorable trends in volume and pain reduction, there was a lack of significance in these changes (statistics not reported).
Kozanoglu et al. 2009
In a RCT of 50 women with BCRL, Kozanoglu and colleagues [25] compared 12 LLLT sessions to 20 sessions of intermittent pneumatic compression (IC). Statistically significant improvement was noted in limb circumference differences compared to baseline in both groups immediately after treatment (p < 0.001), at 3 months (p < 0.001), and at 6 months (IC group p < 0.01; LLLT group p < 0.05). Only the LLLT group maintained significant improvement at 12-month follow-up (p < 0.01). Improvement was greater in the LLLT group compared to the IC group immediately post-treatment (p = 0.04) and at 12-month follow-up (p = 0.02). Statistically significant improvement was seen in VAS scores from baseline to immediately after treatment (p < 0.01) and at 3-month (p < 0.01), 6-month (p < 0.01), and 12-month (p < 0.01) follow-up in the LLLT group and only immediately post-treatment (p < 0.01) in IC group. No significant differences in pain scores were found between groups at any time point.
Lau and Cheing 2009
In 21 women with BCRL, Lau and Cheing [26] investigated the effect of LLLT compared to a waitlist control group in a RCT. In the laser group (n = 11), there was a 16 % average reduction in arm volume immediately after treatment (84.2 ± 8.5 %, p < 0.0001) and 28 % average reduction at 4 weeks post-treatment (71.9 ± 6.3 %, p < 0.0001). In the control group, there was an average 6 % increase in arm volume by 4 weeks post-treatment (106.0 ± 4.3 %, p < 0.0001). Although the difference between groups at the 4-week post-intervention follow-up (p = 0.044) did not reach Bonferroni-corrected statistical significance (set at <0.017), the authors suggest that LLLT may be useful in conjunction with other therapies to accelerate the benefits of treatment and reduce the need for expensive and labor-intensive treatments.
Maiya et al. 2008
In this randomized trial of women with breast cancer-related lymphedema, Maiya et al. [6] investigated the immediate effects of a 10-day course of LLLT plus UE exercise (n =10) compared to UE exercise and use of compression garment (n = 10). Significantly greater reductions in arm circumference were seen in the LLLT group compared to the no-LLLT group for both arm (p = 0.021) and forearm (p = 0.05) circumference measurements at the conclusion of the intervention. The pain scores in the LLLT group (1.5 ± 0.51) and control group (4.8 ± 1.50) were significantly different at the conclusion of the intervention (p = 0.001).
Omar et al. 2011
Omar et al. [27] conducted a RCT comparing LLLT (n = 25) to sham laser (n = 25). Of the 58 women initially randomized, eight were lost to follow-up (four women in each group): in the LLLT group, one withdrew for cellulitis and three for non-adherence; in the sham group, two withdrew for cellulitis and two for non-adherence. Average duration of lymphedema was 13.98 months (±2 months). Limb circumference was significantly decreased in the LLLT group compared to baseline at each time point (p < 0.05). There were significant (p < 0.05) within-group decreases in limb circumference for the sham group as well, with the exception of week 4. Differences between groups, with greater reductions in the LLLT than in the sham group, were statistically significant (p < 0.01) at weeks 8, 12, and 16. The authors concluded that LLLT may be effective in reducing arm circumference in persons with BCRL, with results lasting up to 16 weeks.
Piller and Thelander 1998
Piller and Thelander [21] conducted a small pre-test/post-test within-group study with 11 participants at enrollment who had BCRL for between 3 and 10 years. Ten women completed 16 sessions of LLLT. Results were reported for regional circumference differences between limbs, for volume calculated from circumference, and for bioimpedance. Overall reductions in circumference were noted in the proximal and distal upper arm, the elbow, and the wrist over the 10-week series. No change was noted in the upper forearm, and an increase in circumference was noted at the lower forearm over the treatment period. Limb volume, calculated from circumference, revealed an average decrease of 100 ml over the 10-week treatment period. Increased volume was noted in the early post-treatment stage (+300 ml), which was decreased by 6 months (−397 ml) and 36 months (−288 ml) from baseline. Reduction in limb volume appeared to be maintained in the seven remaining participants, with a volume reduction of the affected arm reaching 29 % over a 2.5-year follow-up. Correlation between duration of treatment and volume difference was reported as the measure of association. Measures of variability were not reported.
Ridner et al. 2013
Ridner et al. [19] conducted a RCT in which 46 women with unilateral BCRL were randomized into one of three treatment arms: (1) LLLT + compression bandaging, (2) manual lymphatic drainage (MLD) + compression bandaging, or (3) combined MLD/LLLT + compression bandaging. For the LLLT group, the median duration of lymphedema was 27 months (IQR: 6, 58). Medians, interquartile range, and effect sizes for limb volume for each group were reported. All three groups demonstrated clinically and statistically significant volume reductions (p < 0.001), but no statistically significant between-groups differences were found (circumference p = 0.422). The largest effect sizes reported were for circumference differences for the two LLLT groups. The authors suggest that LLLT followed by compression bandaging may be as effective at reducing volume and less burdensome relative to MLD or combined MLD/LLLT followed by compression bandaging. However, since each group received compression bandaging after treatment, the beneficial effect of compression bandaging itself cannot be discounted. Assessment of UE pain/ache was included as part of the Lymphedema Symptom Intensity and Distress Scale-Arm (LSIDS-A). Effect sizes for UE ache comparing baseline to immediately following the final treatment were 0.24 for the MLD group, −0.31 for the LLLT group, and −0.07 for the MLD + LLLT group. While between-groups comparisons specific to UE pain/ache were not done, the differences among groups for the total LSIDS-A scores were not significantly different.
Study characteristics and results across studies
All studies included a measure of upper extremity volume, but only five included independent measures of pain. Effect sizes for individual studies were calculated, where authors presented sufficient data specifically reflecting the results of LLLT within a single treatment cohort or between treatment groups (Table 3). If studies did not report effect sizes or provide data to calculate them, attempts were made to contact study investigators to obtain data. If data were not available, the studies were not included in meta-analysis for that outcome. Effect sizes were calculated for one assessment period only (for outcomes assessed between 0 and 4 weeks of conclusion of the intervention). An overview of study parameters and conclusions for all nine studies is presented in Table 4.
Synthesis of results
Limb volume
The within-group pooled effect size for changes in UE volume post-LLLT treatment was calculated using data from six studies (Fig. 2) [18, 24–26]. Statistical heterogeneity, as represented by a Q-statistic of 2.77 (p = 0.73), was not statistically significant. Cohen’s d within-group pooled effect size, calculated using the fixed effect model, was statistically significant for a moderate reduction in volume post-treatment (d = −0.52, 95 % CI = −0.78, −0.25). When converted back to clinical units, this effect size equates to a reduction in arm volume of 75.7 ml.
The between-groups pooled effect size for differences in volume between groups, after treatment, was calculated using data from four studies (Fig. 3) [6, 25, 26]. Statistical heterogeneity was non-significant, Q = 2.71 (p = 0.44), and a moderate, statistically significant pooled effect size was calculated using the fixed effect model (d = −0.62; CI = −0.97, −0.28). When converted back to clinical units, this effect size is equivalent to a 90.9-ml greater reduction in arm volume with treatment including LLLT than with treatment not including LLLT.
Pain
Three studies reporting pain outcome data measured by the visual analog scale (VAS) were included in within-group meta-analysis [18, 24, 25]. The outcomes reported were statistically homogeneous, Q = 1.4 (p = 0.49). Meta-analysis using a fixed effect model revealed a statistically significant, moderate pooled effect size of LLLT on pain reduction (d = −0.62; CI = −1.06, −0.19; Fig. 4). This represents a clinical reduction in pain of 13.5 mm on the 0–100 mm VAS.
Data for pain outcomes immediately post-treatment were extracted from two studies [6, 25] and combined to calculate the comparative benefit of LLLT on pain reduction through between-groups pooled effect size statistical analysis. The data were significantly heterogeneous (Q-statistic of 22.60, p = <0.001). Calculation of between-groups, pooled effect size of LLLT on pain reduction using the random effects model revealed a large pooled effect size (d = −1.21) but a wide confidence interval crossing zero (95 % CI = −4.51, 2.10), thus no statistically significant difference in amount of pain reduction after LLLT as compared to other treatments (Fig. 5). The effect size was converted into clinical units to reveal a 21.1-mm larger reduction in pain on the VAS with treatment including LLLT than with treatment not including LLLT.
Harm
Six of the nine studies reported on adverse events or discussed harm [6, 21–24, 27]. Dirican et al. [23] reported development of cellulitis in one participant in the LLLT group. Omar et al. [27] reported cellulitis in one LLLT participant and two participants in the sham laser group. Piller reported a severe injury-related arm infection (unrelated to the study) in one participant who had been enrolled but did not continue the intervention [21]. All other studies reported no adverse events to participants or did not report on harm.
Risk of bias in and between studies
The PEDro scale was used to evaluate study quality (Table 1). Scores varied from a minimum of 4 to a maximum of 8. The two single-group studies were at greater risk for bias due to the nature of the study design (lack of experimental controls). Evaluating publication bias for this meta-analysis was not possible due to the low number of studies included in meta-analysis.
Discussion
Summary of evidence
This systematic review and meta-analysis examined current evidence of the effects of LLLT on swelling and pain in women with BCRL. Nine studies of level of evidence from 2 to 4 were eligible for inclusion. The results support our hypothesis that the use of LLLT alone or combined with other treatments decreases swelling and pain in women with BCRL. Additionally, LLLT is more effective in decreasing swelling, but not pain, when compared to treatments that do not include LLLT.
Although the minimal clinically important difference (MCID) in limb volume reduction following treatment for BCRL has not been established, a reduction of 76 ml following LLLT may represent a clinically significant improvement in swelling as it may impact diagnosis and treatment decisions. Conversion of the between-groups pooled effect size for swelling revealed a 91-ml greater reduction in arm volume with treatment including LLLT than with treatment not including LLLT. Limb volume reductions in women with BCRL have been associated with improvements in mobility and quality of life. It may also be reasonable to expect that decreases in arm swelling may lead to attendant changes in skin quality or texture (e.g., fibrosis) or in pain severity. Treatments that contribute to meaningful reductions in swelling warrant consideration as a viable treatment option in the management of BCRL.
Treatment with LLLT resulted in reduction of pain in women with BCRL. Converting this single-group pooled effect size to clinical units resulted in an average reduction of 13.5 mm on the 0–100 mm VAS for pain. This exceeds the MCID of 9–11 mm for the VAS [28]. While the between-groups pooled effect size for pain reduction yielded the largest effect size (−1.21), of potential clinical importance, the difference between groups did not reach statistical significance (95 % CI = −4.51, 2.10). Only two studies provided pain data for this between-groups effect size.
While there was improvement in pain in those who received treatment with and without LLLT, one could speculate that the decrease in pain was a result of the decrease in volume of the affected limb or because of improved mobility of the affected limb. However, as many practicing clinicians may experience, there is an entire spectrum of pain syndromes that may arise as the result of breast cancer treatment. Other potential causes of pain in breast cancer survivors include cervical radiculopathy, brachial plexopathy, mono-neuropathies, chemotherapy-induced peripheral neuropathy, rotator cuff tendonitis, shoulder adhesive capsulitis, axillary web syndrome, post-mastectomy pain syndrome, post-surgical pain and edema, and bone metastases [29]. Treatments for these conditions are often addressed simultaneously with the treatment of lymphedema. In future studies, it may be beneficial to further investigate the complaint of pain in relation to intervention.
Regarding harm, while there were no apparent differences in adverse treatment-related events in LLLT versus control groups across studies, important contraindications and precautions for LLLT should be considered when using this modality. The total incidence of cellulitis reported in the included studies was two per group [23, 27]. Women with UE lymphedema after breast cancer treatment are at greater risk for developing cellulitis than women without lymphedema, likely due to stagnation of proteins and fluid in the edematous limb [30, 31]. Cellulitis is an acute infection of the skin and subcutaneous tissues characterized by erythema, pain, warmth, and swelling. Through medical record review of patients seen at the Thailand Lymphedema Day Care Center, Teerachaisakul et al. [30] identified 1456 patients diagnosed with lymphedema. Of these, 179 were determined to have had cellulitis for which several associated independent risk factors were identified: percent difference in limb circumference, primary lymphedema diagnosis, food-induced complication experience, and elevated systolic blood pressure. Interestingly, skin injury was not included in the list of potential risk factors. In the chronic wounds of 25 patients with primary lymphedema, methicillin-resistant Staphylococcus aureus was found in 35 % of the cases [32]. Meticulous skin care in patients with chronic lymphedema, to prevent opportunistic infections from microorganisms on the skin, is important in the prevention of cellulitis. Though LLLT does not appear to increase the risk for cellulitis, patients with skin breakdown or signs and symptoms of cellulitis should be referred for appropriate medical management.
Particularly relevant to patients with BCRL is the potential for malignancy. Because laser has been shown to increase blood flow and cellular energy production [11], it has been theorized that laser could have a carcinogenic influence on tissues [16]. According to a 2009 review [33], no evidence has demonstrated in vivo harm from laser therapy regarding increases in cancer or cancer cell activity. Similarly, in vitro studies showed no adverse effects, with some studies reporting increased phagocytic and chemotactic activity of leukocytes while noting no acceleration of tumor cell reproduction [33]. None of the studies included in this review evaluated the effect of LLLT on cancer recurrence or metastasis, which would require longer-term follow-up and much larger sample sizes.
Primary evidence regarding the effect of LLLT consists of seven small level 2 to 3 RCTs of variable methodological rigor and two single-group pre-test/post-test studies of lower quality (level 4). Individual study quality for the RCTs was evaluated using the PEDro scale. Scores ranged from 4 to 8 (out of 10) for the seven two-group studies. Those studies with PEDro scores <5 were downgraded from a level of evidence 2 to a level of evidence 3. All of the RCTs reported to have randomly allocated participants to groups. However, the study by Kozanoglu [25] reported that patients were randomized, blindly, “by consecutive alternate allocation according to the admittance to our clinic”. Quasi-randomized allocation strategies, such as alternation, do not satisfy this PEDro item criterion. Baseline characteristics are reported, however, and no statistically significant differences in important characteristics were seen. Maiya et al. [6] reported block randomization of their 20 participants (ten per group), but it was unclear how this was done. The authors did not report demographic baseline characteristics other than generally in the abstract. All other two-group studies demonstrated baseline comparability between groups. Few studies reported on concealment of allocation, and thus most were scored low on that item. Non-concealed allocation, non-random allocation, and baseline group differences may introduce a source of bias, threatening the internal validity of the study and increasing the risk for confounding factors to obscure the relationship between the treatment and the outcome. In these studies, this was less of a problem than lack of blinding. Lack of blinding of participants and/or assessors is another source of potential bias. Blinding minimizes differential treatment of the groups throughout the study and the potential for differential assessment of outcomes, minimizing bias and improving study validity. Participants were blinded in only the three RCTs that utilized sham laser as the control [22, 24, 27]. Assessors were blinded in three studies [24, 26, 27].
While statistical heterogeneity was only demonstrated for one of our analyses, there is qualitative heterogeneity across the nine studies in study design, types of control groups, and in protocols for LLLT. Control groups in the two-group studies included sham laser in three studies [22, 24, 27], intermittent compression in one [25], waitlist in one [26], compression garment in one [6], and MLD or MLD/LLLT in one [19]. Two studies had no comparison group [21, 23]. LLLT treatment parameters also varied widely among studies. Frequency and number of LLLT sessions ranged from ten sessions on consecutive days to 36 sessions provided three times per week for 12 weeks. Three of the studies provided LLLT in two distinct 3-week, nine-session treatment cycles with an 8-week hiatus between cycles [22–24]. Seven of the nine studies used direct contact or non-contact spot application handheld units. The most common laser wavelength applied was ~904 nm, included in seven of nine of the studies (Table 5). Laser application duration ranged from 17 to 34 min per session. Laser application ranged from 5 to 17 standardized locations, and all protocols included treatment to the axilla. Is it unknown if the frequency and timing of visits, number of minutes per session, or total “dose” of laser applied is the important variable. Participants in the Maiya [6] study had a total of 340 min of LLLT over 10 days, while participants in the Lau et al. [26] and Kozanoglu et al. [25] studies each had 240 min of LLLT over a 4-week period, a considerably lower “dose” with greater temporal spread. Future studies could examine dose more specifically. The parameters most commonly used among these studies included ≥17-min treatment sessions of 904-nm LLLT, three times per week for 3 to 4 weeks with a dosage of 1.5 J/cm2 applied to the axillary region. These parameters are in accordance with those that have been reported in pre-clinical research to a have bio-stimulatory effect [34].
Differences in study heterogeneity and participant characteristics may account for the differences seen among individual study effect sizes. This becomes important to consider when determining generalizability of individual study or aggregate results to clinical practice. All studies included adult women who met study-defined criteria for diagnosis of lymphedema (>200-ml interlimb difference, >2-cm difference between limbs at multiple measurement locations, or % difference between limbs). Although the Maiya et al. study enrolled women between 3 and 6 weeks post-surgery, the remaining studies included women with lymphedema of at least 2 months in duration and most greater than 3 months.
Sample sizes of the studies included in this review were varied and small, ranging from 8 to 64. Total sample size across all studies was 289. However, study heterogeneity and/or lack of data necessary for calculation of individual study effect sizes limited the ability to pool all studies for both outcomes. Therefore, sample sizes for the meta-analyses remained modest. Pooling data from three studies for the within-group effect size for pain yielded a sample size of 44. Pooling two studies for between-groups differences in pain yielded a sample size of 67 (33 in LLLT and 34 in control groups). The latter analysis may still be underpowered to detect between-groups differences in pain, which did not reach statistical significance. Pooled sample sizes for volume were larger. For the within-group analysis of volume changes, pooling data from six studies yielded a sample size of 115. For the between-groups analysis of volume, pooling results from four studies resulted in a sample size of 138 (69 in LLLT and 69 in control groups).
Statistical reporting varied among studies, adding to the challenge of pooling data. Between-groups statistical comparisons were not reported, and no measure of variability appeared in Kaviani et al., precluding it from inclusion in the between-groups meta-analysis. While the Carati et al. study was a RCT, only within-group effect sizes could be included in this meta-analysis since p values were only reported for the 3-month follow-up between-groups comparison. Of the single-group studies, Piller did not include measures of variability and was thus not included in meta-analysis of within-group effects. No studies explicitly stated that intention to treat analysis was performed; however, the Maiya et al. and Lau et al. studies had no dropouts, and all participants completed the study.
An additional threat to validity may include publication bias, in which studies with favorable outcomes are more often published than those with negative outcomes. This may have biased our meta-analytic results toward favoring LLLT; however, statistical tests for publication bias (i.e., Eggers test) could not be reliably utilized since so few studies were included in the meta-analysis. While all but one of the individual studies reported clear benefit of LLLT for within-group comparisons for volume, comparison between groups was more balanced with four studies favoring LLLT (n = 184) and three not (n = 75) (Table 4), and in spite of the authors’ conclusions, the individual study effect sizes that were calculated for volume within-group meta-analysis were not statistically significant. The within-group volume effect size only reached statistical significance once pooled. This may reflect inadequate power in the individual studies. For the between-groups comparisons for volume, half of the studies favored LLLT and half did not. Once pooled, the between-groups volume difference did reach statistical significance.
The best study design for establishing a causal relationship between an intervention and outcome is the RCT. A meta-analysis of high-quality RCTs provides the highest level of evidence, but unfortunately, there are limited numbers of methodologically rigorous studies on LLLT on the treatment of lymphedema. Enhanced rigor can be achieved through consistent blinding of participants and assessors when possible and true and concealed random allocation to ensure that valid conclusions can be drawn from the results. The current standard of care for BCRL is CDT, which has been shown to be effective in volume reduction as a multimodal treatment [7], and comparison of LLLT or LLLT plus CDT compared to CDT alone is warranted.
In determining the strength of evidence, it is important to consider risk of study bias, consistency in effect sizes among studies, directness of comparisons, and the precision and magnitude of the effect sizes for the outcomes considered important [35]. Risk of bias was formally addressed by evaluating study design and methodology with the PEDro rating scale and Oxford Centre for Evidence-Based Medicine Levels of Evidence [36]. While the two single-group studies were at greater risk for bias, the remaining RCTs had greater internal controls for study bias. However, blinding of investigators and participants in these studies was variable. Consistency, or similarity in direction and range of effect sizes, was high in this meta-analysis. While not all individual study effect sizes were statistically significant, they were consistently in the same direction.
Due to the comprehensive nature of BCRL management, and variability in study methodology, this meta-analysis was unable to fully parse out the effects of LLLT alone on limb volume and pain. Only two of the RCTs compared LLLT alone against a placebo treatment [22, 24] and one to a waitlist control [26]. For the others, the number and type of co-interventions varied. Stout et al. [9] demonstrated that the use of a compression garment alone is effective at reducing limb volume in women with early volume changes after breast cancer surgery. If, however, the control group interventions were effective themselves in reducing volume or pain, this may result in an underestimate of the effect of LLLT on these outcomes. Within the RCTs that utilized co-interventions, the co-interventions were the same across treatment groups, allowing LLLT to be compared directly to alternative treatments. For example, Omar [27] compared LLLT, exercise, education, and compression garments to a control group of sham laser, exercise, education, and compression garments, allowing direct comparison of active to sham LLLT. With regard to pain, there was little, if any, information provided in the studies about co-interventions, so interpretation of effects of LLLT on pain requires caution.
The precision around the effect size estimates for volume was such that conclusions could be drawn about the benefit of treatment. This was not the case for the between-groups comparisons for pain for which the confidence interval was wide, and finally, the magnitude of the effect size should be considered. Effect sizes of 0.2 are considered small, 0.5 are considered medium, and 0.8 are considered large [37]. The magnitudes for the pooled effect sizes were moderate for between- and within-group comparisons for volume and the within-group comparisons for pain.
Conclusions
Therefore, the results of this systematic review and meta-analysis provide moderate evidence in support of the use of LLLT in reducing limb volume in the management of BCRL. While there are a limited number of studies, with small sample sizes, the results of pooled analyses support statistically significant and clinically meaningful reductions in limb volume immediately upon conclusion of treatments that included LLLT compared to those that did not include LLLT. While there is evidence of pain reduction with the use of LLLT, there is insufficient evidence that treatments that utilize LLLT provide additional benefit beyond treatments that do not include LLLT. However, in evaluating the applicability of this evidence to clinical practice, a number of factors should be taken into account. This includes the validity and quality of the individual studies included in the review and the quality and generalizability of the review itself.
References
DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013;14(6):500–15.
Smoot B, Wong J, Cooper B, Wanek L, Topp K, Byl N, et al. Upper extremity impairments in women with or without lymphedema following breast cancer treatment. J Cancer Surviv. 2010;4(2):167–78.
Dawes DJ, Meterissian S, Goldberg M, Mayo NE. Impact of lymphoedema on arm function and health-related quality of life in women following breast cancer surgery. J Rehabil Med. 2008;40(8):651–8.
Hayes SC, Johansson K, Stout NL, Prosnitz R, Armer JM, Gabram S, et al. Upper-body morbidity after breast cancer: incidence and evidence for evaluation, prevention, and management within a prospective surveillance model of care. Cancer. 2012;118(8 Suppl):2237–49.
Ridner SH. Quality of life and a symptom cluster associated with breast cancer treatment-related lymphedema. Support Care Cancer. 2005;13(11):904–11.
Maiya A, Olivia E, Dibya A. Effect of low energy laser therapy in the management of post-mastectomy lymphoedema. Physiother Sing. 2008;11:2–5.
Hwang JM, Hwang JH, Kim TW, Lee SY, Chang HJ, Chu IH. Long-term effects of complex decongestive therapy in breast cancer patients with arm lymphedema after axillary dissection. Ann Rehabil Med. 2013;37:690–7.
Huang TW, Tseng SH, Lin CC, Bai CH, Chen CS, Hung CS, et al. Effects of manual lymphatic drainage on breast cancer-related lymphedema: a systematic review and meta-analysis of randomized controlled trials. World J Surg Oncol. 2013;11:15.
Stout NL, Pfalzer LA, Springer B, Levy E, McGarvey CL, Danoff JV, et al. Breast cancer-related lymphedema: comparing direct costs of a prospective surveillance model and a traditional model of care. Phys Ther. 2012;92(1):152–63.
Thiel H. Low power laser therapy—an introduction and a review of some biological effects. J Can Chiropr Assoc. 1986;30(3):133–8.
Cameron M. Electromagnetic radiation: lasers and light. In: Cameron MH, editor. Physical agents in rehabilitation: from research to practice. 3rd ed. St. Louis: Saunders; 2009.
Lievens P. The influence of laser-irradiation on the motricity of the lymphatical system and on the wound healing process. In: Proceedings International Congress on Laser in Medicine and Surgery, Bologna, June 26–28, 1985. Monduzzi. 1985:171–4.
Lievens P. The effect of a combined HeNe and IR laser treatment on the regeneration of the lymphatic system during the process of wound healing. Lasers Med Sci. 1991;6(2):193–9.
Assis L, Moretti AI, Abrahao TB, de Souza HP, Hamblin MR, Parizotto NA. Low-level laser therapy (808nm) contributes to muscle regeneration and prevents fibrosis in rat tibialis anterior muscle after cryolesion. Lasers Med Sci. 2013;28(3):947–55.
Omar MT, Shaheen AA, Zafar H. A systematic review of the effect of low-level laser therapy in the management of breast cancer-related lymphedema. Support Care Cancer. 2012;20(11):2977–84.
Lima ME, Lima J, de Andrade M, Bergmann A. Low-level laser therapy in secondary lymphedema after breast cancer: systematic review. Lasers Med Sci. 2014;29:1289–95.
Moseley AL, Carati CJ, Piller NB. A systematic review of common conservative therapies for arm lymphoedema secondary to breast cancer treatment. Ann Oncol. 2007;18(4):639–46.
Flórez-García MT, Valverde-Carrillo MD. Effectiveness of nonpharmacological interventions in the management of lymphedema postmastectomy. Rehabilitacion. 2007;41(3):126–34.
Ridner SH, Poage-Hooper E, Kanar C, Doesram JK, Bond SM, Dietrich MS. A pilot randomized trial evaluating low-level laser therapy as an alternative treatment to manual lymphatic drainage for breast cancer-related lymphedema. Oncol Nurs Forum. 2013;40:383–93.
Piller N, Thelander A. Treating chronic postmastectomy lymphedema with low level laser therapy: a cost effective strategy to reduce severity and improve quality of survival. Laser Ther. 1995;7(23):163–8.
Piller NB, Thelander A. Treatment of chronic postmastectomy lymphedema with low level laser therapy: a 2.5 year follow-up. Lymphology. 1998;31(2):74–86.
Carati CJ, Anderson SN, Gannon BJ, Piller NB. Treatment of postmastectomy lymphedema with low-level laser therapy: a double blind, placebo-controlled trial. Cancer. 2003;98(6):1114–22.
Dirican A, Andacoglu O, Johnson R, McGuire K, Mager L, Soran A. The short-term effects of low-level laser therapy in the management of breast-cancer-related lymphedema. Support Care Cancer. 2011;19(5):685–90.
Kaviani A, Fateh M, Yousefi Nooraie R, Alinagi-zadeh MR, Ataie-Fashtami L. Low-level laser therapy in management of postmastectomy lymphedema. Lasers Med Sci. 2006;21(2):90–4.
Kozanoglu E, Basaran S, Paydas S, Sarpel T. Efficacy of pneumatic compression and low-level laser therapy in the treatment of postmastectomy lymphoedema: a randomized controlled trial. Clin Rehabil. 2009;23(2):117–24.
Lau RW, Cheing GL. Managing postmastectomy lymphedema with low-level laser therapy. Photomed Laser Surg. 2009;27(5):763–9.
Omar M, Abd-El-Gayed Ebid A, El Morsy A. Treatment of post-mastectomy lymphedema with laser therapy: double blind placebo control randomized study. J Surg Res. 2011;165(1):82–90.
Bird SB, Dickson EW. Clinically significant changes in pain along the visual analog scale. Ann Emerg Med. 2001;38(6):639–43.
Stubblefield MD, Keole N. Upper body pain and functional disorders in patients with breast cancer. PM R. 2014;6(2):170–83.
Teerachaisakul M, Ekataksin W, Durongwatana S, Taneepanichskul S. Risk factors for cellulitis in patients with lymphedema: a case-controlled study. Lymphology. 2013;46(3):150–6.
de Godoy JMP, da Silva SH. Prevalence of cellulitis and erysipelas in post-mastectomy patients after breast cancer. Arch Med Sci. 2007;3:249–51.
Daróczy J. Antiseptic efficacy of local disinfecting povidone iodine (Betadine) therapy in chronic wounds of lymphedematous patients. Dermatology. 2002;204:75–8.
Tilley S. Use of laser therapy in the management of lymphoedema. J Lymphoedema. 2009;4(1):39–43.
Hawkins D, Abrahamse H. Effect of multiple exposures of low-level laser therapy on the cellular responses of wounded human skin fibroblasts. Photomed Laser Surg. 2006;24(6):705–14.
Owens DK, Lohr KN, Atkins D, et al. Grading the strength of a body of evidence when comparing medical interventions. In: Agency for healthcare research and quality. Methods guide for comparative effectiveness reviews [posted July 2009]. Rockville, MD. Available at: http://effectivehealthcare.ahrq.gov/healthInfo.cfm?infotype=rr&ProcessID=60.
OCEBM Levels of Evidence Working Group*. The Oxford levels of evidence 2. Oxford Centre for Evidence-Based Medicine. http://www.cebm.net/index.aspx?o=5653. *OCEBM Levels of Evidence Working Group=Jeremy Howick, Iain Chalmers (James Lind Library), Paul Glasziou, Trish Greenhalgh, Carl Heneghan, Alessandro Liberati, Ivan Moschetti, Bob Phillips, Hazel Thornton, Olive Goddard and Mary Hodgkinson.
Cohen J. Statistical power analysis. Curr Dir Psychol Sci. 1992;1(3):98–101.
Acknowledgments
The authors wish to thank Felicia F. Ferlin, PT, DPT, and Victoria Deguzman, PT, DPT, for their review and critique of this manuscript. Dr. Smoot is partially supported by the Building Interdisciplinary Research Careers in Women’s Health (BIRCWH) K12, Grant Number K12HD052163 NICHD/NIH, and by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number KL2TR000143.
Conflict of interest
The authors declare no financial conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix A
Appendix B
Rights and permissions
About this article
Cite this article
Smoot, B., Chiavola-Larson, L., Lee, J. et al. Effect of low-level laser therapy on pain and swelling in women with breast cancer-related lymphedema: a systematic review and meta-analysis. J Cancer Surviv 9, 287–304 (2015). https://doi.org/10.1007/s11764-014-0411-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-014-0411-1