Abstract
Objective
Lobe-specific nodal dissection (LND) is increasingly used for non-small cell lung cancer (NSCLC) in Japan; however, its treatment validity remains unclarified. Since 2013, LND has been used as a standard procedure for clinical stage-I (c-stage-I) NSCLC at our institution. We aimed to evaluate its validity using intraoperative frozen section analysis (FSA) for c-stage-I NSCLC.
Methods
The participants comprised patients with NSCLC who underwent LND between 2013 and 2016 (n = 307) or systematic nodal dissection (SND) between 2002 and 2013 (n = 367) for c-stage-I disease. FSA was routinely performed in LND to examine at least three stations. Outcomes were compared between the LND and SND groups. Patients in whom LND was converted to SND due to metastasis on FSA of the sampled lymph node were still categorized into the LND group, i.e., intention-to-treat analysis. The prognostic impact was compared using propensity score matching.
Results
The rate of conversion from LND to SND was 10.4%. Of the patients converted to SND, 12.5% had metastases outside the LND area. False-negative N2 results were detected in only 0.7% of the LND group patients after FSA. After matching, each group had 220 patients. There were no significant between-group differences in the lymph-node recurrence rate (7% vs. 6%), 5-year recurrence-free survival (80.1% vs. 79.0%), and overall survival (90.4% vs. 90.3%).
Conclusions
LND with intraoperative FSA is a valid modality that could serve as a standard surgical procedure for c-stage-I NSCLC. Intraoperative FSA may lower the residual lymph-node metastasis risk in LND.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Complete resection with lobectomy and systematic nodal dissection (SND) is the current standard surgical treatment for non-small cell lung cancer (NSCLC). However, Japanese retrospective studies [1,2,3] have proposed lobe-specific nodal dissection (LND) for early-stage NSCLC to address the limitations of SND. LND is a procedure with selective omission of mediastinal lymph-node dissection depending on the primary tumor location. LND for clinical stage-I (c-stage-I) NSCLC was originally proposed in 2006 [4] without a significant difference in the postoperative prognosis between LND and SND but significantly lower morbidity with LND. Subsequent studies found no significant difference in overall survival (OS) between SND and LND [5,6,7,8] and that LND was less invasive [5, 6, 8]. A recent study reported that LND led to better OS in stage I and II NSCLC patients than SND [9]. Therefore, LND has become the standard procedure for NSCLC treatment in Japan [10].
These studies had several limitations. First, there was no established strategy or eligibility criteria, as patients who were initially planned for LND but converted to SND when lymph-node metastasis (LNM) was detected during surgery were inconsistently excluded or included in the SND group. Therefore, it is possible that the SND group included a greater number of advanced-stage patients, and these studies reported favorable outcomes for LND. In addition, although intraoperative frozen section analysis (FSA) was initially performed routinely [4], subsequent studies performed intraoperative FSA only when LNMs were suspected to be positive macroscopically [5, 6], and most studies did not mention FSA. In our institution, LND was initially performed depending on patient-related risk factors, and the rate of mediastinal node recurrence was significantly higher in patients undergoing LND than in those undergoing SND [6]. Therefore, when LND became a standard procedure for c-stage-I NSCLC in 2013, we decided to include routine intraoperative FSA. When the sampled lymph node showed metastasis, patients who initially planned for LND were converted to SND to minimize the risk of residual pathological N2 (pN2) disease outside the LND area. However, the effects of intraoperative FSA on preventing intraoperative oversight of N2 and local recurrence, prognosis improvement, patient conversion rate from LND to SND, and residual rate of pN2 outside the LND remain unclear.
Second, most studies did not include preoperative radiological evaluation using thin-section computed tomography (TSCT) to determine the rate of ground-glass opacities (GGO) or positron emission tomography (PET) to quantify the maximum standardized uptake value (SUVmax) of the primary tumor, both key indicators of tumor invasiveness.
Thus, this study aimed to assess and compare the validity of LND with intraoperative FSA and SND for c-stage-I NSCLC patients undergoing curative lobectomy with radiological evaluation using both PET and CT. The prognostic impact and surgical outcomes were compared between the two modalities using the propensity score (PS) matching method. Moreover, the patients who underwent conversion from LND to SND were categorized into the LND group in the intention-to-treat (ITT) analysis to avoid biasing the results against SND.
Methods
Study design and patient enrollment
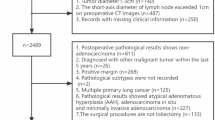
This retrospective study evaluated 2669 consecutive patients who were diagnosed with NSCLC (TNM classification, 7th edition) and underwent pulmonary resection (September 2002–December 2016) in our institution. Among them, 1,192 patients underwent complete resection with lobectomy and lymph-node dissection for c-stage-I (i.e., tumor diameter ≤ 5 cm and clinical N0). Patients who received induction therapy, those with residual tumor at the resection margin, those with pleural dissemination including malignant effusion, and those who underwent pneumonectomy or bilobectomy were excluded.
Before January 2013, SND was performed as a standard procedure for c-stage-I NSCLC, and LND was only performed in patients with one or more risk factors such as advanced age or the presence of diabetes, respiratory dysfunction, or cardio-cerebrovascular disease requiring treatment and were judged at the surgical conference of our institution to be at risk for SND or those with a wide GGO area [6]. However, since February 2013, LND has become a standard procedure for c-stage-I NSCLC. To perform LND while minimizing the risk of pN2 disease outside the LND area, patients with primary tumors of the middle lobe, left lingular, and bilateral superior segment of the lower lobe were excluded because of the high frequency of both superior mediastinal and subcarinal node metastases [1,2,3, 11,12,13]. We also excluded LND patients with risk factors, as they are generally ineligible for lymph-node dissection [6].
Finally, 307 patients who underwent LND with routine intraoperative FSA between February 2013 and December 2016 (LND group) and 367 patients who underwent SND between September 2002 and January 2013 (SND group) were enrolled. The SND group was set as the historical control. The eligible primary tumors of the SND group were comparable with those of the LND group (Supplemental Fig. 1).
All enrolled patients underwent preoperative staging with TSCT (1–2-mm section thickness). The primary tumor was evaluated as part-solid (i.e., consolidation/tumor ratio < 1.0 on TSCT) or solid tumor according to differences in postoperative prognosis [14]. Additional staging procedures included bronchoscopy, PET, and head magnetic resonance imaging. LNM was defined as an enlarged lymph node sized ≥ 1 cm in the short axis on CT and/or hypermetabolism on PET.
Follow-up, definition of recurrence, and evaluation of recurrence were performed as described previously [15]. Morbidity was defined as a ≥ grade II postoperative complication according to the Clavien–Dindo classification [16].
This study was approved by the Institutional Review Board of the Shizuoka Cancer Center (approval number: J2019-181). The need for written informed consent was waived owing to the retrospective nature of the study.
Surgical procedure
Lobectomy was performed with hilar and mediastinal lymph-node dissection based on the International Association for the Study of Lung Cancer node map [17]. SND was performed as previously described [9]. For right-sided tumors, mediastinal fat tissues, including stations 2R, 4R, 7, 8, and 9, were resected. For left-sided tumors, mediastinal fat tissues, including stations 4L, 5, 6, 7, 8, and 9, were resected. For the upper lobe, stations 8 and 9 were not routinely dissected according to the general clinical procedure in Japan [2, 3, 12].
LND was performed based on lobe-specific LNM patterns and a previously described procedure [9]. For upper lobe tumors, superior mediastinal and/or aortic nodes (stations 2R and 4R for right-sided tumors and stations 4L, 5, and 6 for left-sided tumors) were dissected, whereas inferior mediastinal nodes (stations 7, 8, and 9) were not. When the tumor was located in the lower lobe, inferior mediastinal nodes (stations 7, 8, and 9) were dissected, and the superior mediastinal and/or aortic nodes were preserved.
Since February 2013, LND was routinely performed for intraoperative FSA. We examined at least three stations, including one station of lobe-specific mediastinal nodes (station 4R for right upper lobe tumors, station 5 for left upper lobe tumors, and station 7 for lower lobe tumors) and two stations for N1 nodes (stations 11 and 12). Representative lymph nodes, which were the largest nodes in each station or those suspected of being positive macroscopically, were examined. When the sampled lymph nodes showed metastasis, patients were immediately converted to SND.
Statistical analyses
Associations between variables were analyzed using Fisher’s exact test or the Mann–Whitney U test. The patients who were initially planned for LND but converted to SND when LNM was detected were included in the LND group for the ITT analysis (LND (ITT) group). The LND group, which excluded patients who were converted to SND, was also investigated for the on-treatment analysis (LND (on-treatment) group).
OS was measured from the date of surgery to the date of death due to any cause. Recurrence-free survival (RFS) was measured from the date of surgery to the date of first occurrence of the event (local and/or distant recurrence or death). The OS and RFS rates were estimated using the Kaplan–Meier method and compared using the log-rank test. Independent risk and prognostic factors were identified using multivariable analysis with a Cox proportional hazards model.
PS matching analysis was used to adjust for potential confounders. PS was calculated using logistic regression based on age, sex, smoking history, location of the primary tumor, maximum tumor size, carcinoembryonic antigen, HRCT findings of the primary tumor, SUVmax of the primary tumor (cutoff, 2.5) [18,19,20,21], and histology. PS matching was performed in a 1:1 ratio using the nearest-neighbor method (caliper = 0.20).
All statistical analyses were performed using EZR (version 1.40; Saitama Medical Center, Jichi Medical University, Saitama, Japan) [22], a modified version of R commander with a user interface designed to add statistical functions frequently used in biostatistics (The R Foundation for Statistical Computing, Vienna, Austria). Differences were considered significant at p < 0.05.
Results
Characteristics of the study cohort
The characteristics of the total cohort are shown in Table 1. Of the 674 patients studied, 62 (9.2%) had pN2 disease, and the proportion was higher in the SND than in the LND group but without significant differences (11% vs. 7%; p = 0.061). The rate of pN2 outside the LND area was 1.4% (5/367) in the SND group (1.3% in upper lobe tumors and 1.4% in lower lobe tumors) and 1.3% (4/307) in the LND group (0.9% in upper lobe tumors and 2.2% in lower lobe tumors). The characteristics of the patients with pN2 outside lobe-specific nodal dissection area are shown in Supplemental Table 1.
The nodal status in the clinical (cN), intraoperative (sN), and pathological (pN) stages of the LND group is shown in Fig. 1. Overall, 32 patients (10.4%) had sN1–2 disease, and all of them were converted to SND. Among them, four patients (12.5% in the SND-converted group) had pN2 outside the LND area, where additional dissection was performed. False-negative N2 results (cN0, sN0, and pN2) were detected in 0.7% (2/275) patients.
The median follow-up time for the censored patients was 87 months (range, 12–190) and 58 months (range, 6–87) in the SND and LND groups, respectively. The RFS and OS curves are shown in Fig. 2a, b. The 5-year RFS and OS rates were 77.3% and 88.0% in the SND group and 79.0% and 90.2% in the LND (ITT) group, respectively, with no significant between-group differences (p = 0.81 and 0.60, respectively). Conversely, the 5-year RFS rate of the LND (on-treatment) group was 84.5%, significantly better than that of the SND group (p = 0.043). Among the 403 patients with solid tumors on HRCT, there were no significant differences between SND and LND (ITT) groups in the 5-year RFS (73.6% vs. 72.0%) and OS (86.2% vs. 87.8%).
Kaplan–Meier survival curves. a Recurrence-free survival (RFS) and b overall survival (OS) in the LND (on-treatment, i.e., exclude the patients converted to SND), LND (intention-to-treat), and SND groups before propensity score matching; and c RFS and d OS in the LND (intention-to-treat) and SND groups after propensity score matching
Multivariable analyses of RFS and OS in the total cohort are shown in Supplemental Table 2. Solid-predominant tumors and high SUVmax were identified as independent prognostic factors for RFS. LND was not a poor prognostic factor for either RFS (hazard ratio [HR] = 0.86, 95% confidence interval [CI] 0.60–1.23) or OS (HR = 1.03, 95% CI 0.63–1.68).
PS-matched cohort
Patient characteristics after PS matching are shown in Table 1. In total, more than 88% of patients in each group had solid-predominant tumors, and more than 60% of patients had solid tumors. All patients underwent PET, and the median SUVmax was 5.1 in the SND group and 4.7 in the LND group. The density plot before and after propensity matching in each group is described in Supplemental Fig. 2.
The RFS and OS curves are shown in Fig. 2c, d. The 5-year RFS and OS rates were 79.0% and 90.3% in the SND group and 80.1% and 90.4% in the LND group, respectively, with no significant between-group differences (p = 0.84 and 0.81, respectively).
Postoperative outcomes
The postoperative outcomes are shown in Supplemental Table 3. Before matching, the SND group had significantly higher morbidity than the LND group (SND 23% vs. LND 16%; p = 0.025); however, after matching, this difference became insignificant (SND 22% vs. LND 16%; p = 0.11). No patient died within 30 days postoperatively. The median operative time and blood loss were significantly increased in the SND group (all p < 0.0001) before and after PS matching. There were no significant differences in recurrence and lymph-node recurrence (SND 6% vs. LND 7%).
Discussion
Although LND can achieve a similar postoperative prognosis to SND [5,6,7,8], its validity as a treatment strategy for stage-I NSCLC remains unclarified. This study revealed that LND with intraoperative FSA is a valid modality for c-stage-I NSCLC and can be a standard surgical procedure for this malignancy. Intraoperative FSA allowed the conversion to SND when LNM was detected and minimized the risk of residual LNM.
To our knowledge, this was the largest study to compare LND and SND and address the two main limitations of previous studies regarding handling the conversion from LND to SND and preoperative radiological evaluation. Here, the patients who underwent conversion from planned LND to SND were included in the LND group and evaluated as the ITT group to avoid biased results against SND. Previous studies excluded patients who were converted from planned LND to SND or categorized these patients in the SND group, thus biasing the results in favor of LND. We demonstrated that the LND (on-treatment) group, which excluded patients who converted to SND, had a significantly better prognosis than the SND group.
We investigated the preoperative radiological evaluation with the consolidation/tumor ratio on TSCT and SUVmax, important indicators of tumor invasiveness, on PET [23, 24]. Our results confirmed that these two factors were independent prognostic factors for RFS. After matching, all patients underwent PET, and the median SUVmax was around 5.0. Moreover, 88% of the patients in both groups had solid-predominant tumors on TSCT. These patients are likely to have occult pN2 [21, 24], and suitable patient selection for comparison between LND and SND was possible.
This study was also the first to investigate the value of routine intraoperative FSA on LND. Intraoperative FSA was performed to detect LNM that was unsuspected on preoperative evaluation and to prevent residual LNM by converting from LND to SND. Although intraoperative FSA was routinely performed in a previous study on LND [4], the conversion rate from LND to SND and residual rate of pN2 outside LND have never been reported.
The false-negative N2 rate was only 0.7% (2/275 patients) after routine FSA, which was lower than our previous finding of 4.9% (11/223 patients) when FSA was performed only for lymph nodes suspected to be positive macroscopically for metastases (pre-2013). Although intraoperative FSA did not eliminate false-negative results, it significantly decreased the rate of nodal upstaging after surgery and more accurately diagnosed unsuspected LNM during surgery than analyses of only macroscopically suspected lymph nodes. Here, intraoperative FSA findings supported the conversion to SND in 10.4% of patients in the LND group, and 12.5% of patients converted to SND had metastases in the additional resected mediastinal nodes. Residual LNM leads to local recurrence, which leads to poor prognosis because a radical cure is difficult, even if recurrence only occurs in the lymph node and local treatment is performed [15, 25].
We previously reported that recurrence of mediastinal node metastasis is significantly greater in patients undergoing LND without routine intraoperative FSA than in those undergoing SND [6]. However, here, we found no significant difference in lymph-node recurrence between the SND and LND groups. This finding supports the efficacy of FSA in LND for preventing local recurrence.
Previous studies enrolled different populations, including patients with risk for pN2 outside the LND area. For example, these studies enrolled both stage-I patients and those at stages II–III; most studies also excluded patients with middle-lobe tumors at risk of metastasis outside the LND area but included, for example, the superior segment of both lower lobes and the lingular segment [4,5,6,7,8,9]. Recent studies reported a rate of pN2 disease outside the LND area in SND of approximately 3% in the total cohort. The rates were also higher in lower lobe tumors than in upper lobe tumors (e.g., 5.8% vs 1.3% in c-stage-I adenocarcinoma [26] and 5.5% vs 1.6% in c-stage-I–II adenocarcinoma [9]). Here, the rate of pN2 outside the LND area was 1.4% in the SND group and 1.3% in the LND group, and those in both the upper and lower lobe tumors were approximately 1%, with minimal difference. The low frequency of pN2 outside the LND area could be attributed to the inclusion of patients who had c-stage-I disease only and the exclusion of patients whose primary tumors were located in the bilateral superior segment of the lower lobe, in contrast to other studies [2, 3, 11].
To be established as a standard surgical procedure, LND should be less invasive than SND. Here, we demonstrated that LND was less invasive based on decreased operative time and blood loss. A low operative time indicates a less invasive surgery and is the most important factor in reducing the medical cost of surgery for lung cancer [27].
This study had some limitations. First, it was performed at a single institution, and the number of patients was limited, especially after PS matching. Moreover, the compared two groups differed in the time period of surgery. The clinical circumstances and post-recurrence treatment differed across the different periods. A prospective randomized controlled study is underway in Japan (JCOG1413), which may provide additional insight [28]. Second, intraoperative FSA and pathological evaluation were not standardized, and these methods were associated with the risk of false-negative findings. Previous studies have shown that most patients with pN2 disease outside the LND area also have lobe-specific mediastinal LNM [3], and there was no skip metastasis (without pN1) to pN2 disease outside the LND area, at least in c-stage-IA patients [29]. Moreover, no patients in the SND group had pN2 disease only outside the LND area. Although our findings support that intraoperative FSA may be an appropriate procedure, its usefulness in LND should be investigated by prospective or PS-matched studies using nationwide data.
Overall, based on our eligibility criteria, LND is a valid treatment strategy for c-stage-I NSCLC, with acceptable prognostic outcomes and less invasiveness than SND. Thus, LND could become a standard surgical procedure. Furthermore, routine intraoperative FSA of the lymph nodes can decrease the risk of residual LNM from LND. Therefore, intraoperative FSA should be performed in LND.
References
Okada M, Tsubota N, Yoshimura M, Miyamoto Y. Proposal for reasonable mediastinal lymphadenectomy in bronchogenic carcinomas: role of subcarinal nodes in selective dissection. J Thorac Cardiovasc Surg. 1998;116:949–53. https://doi.org/10.1016/S0022-5223(98)70045-5.
Asamura H, Nakayama H, Kondo H, Tsuchiya R, Naruke T. Lobe-specific extent of systematic lymph node dissection for non-small cell lung carcinomas according to a retrospective study of metastasis and prognosis. J Thorac Cardiovasc Surg. 1999;117:1102–11. https://doi.org/10.1016/s0022-5223(99)70246-1.
Watanabe S, Asamura H, Suzuki K, Tsuchiya R. The new strategy of selective nodal dissection for lung cancer based on segment-specific patterns of nodal spread. Interact Cardiovasc Thorac Surg. 2005;4:106–9. https://doi.org/10.1510/icvts.2004.098814.
Okada M, Sakamoto T, Yuki T, Mimura T, Miyoshi K, Tsubota N. Selective mediastinal lymphadenectomy for clinico-surgical stage I non-small cell lung cancer. Ann Thorac Surg. 2006;81:1028–32. https://doi.org/10.1016/j.athoracsur.2005.09.078.
Ishiguro F, Matsuo K, Fukui T, Mori S, Hatooka S, Mitsudomi T. Effect of selective lymph node dissection based on patterns of lobe-specific lymph node metastases on patient outcome in patients with resectable non-small cell lung cancer: a large-scale retrospective cohort study applying a propensity score. J Thorac Cardiovasc Surg. 2010;139:1001–6. https://doi.org/10.1016/j.jtcvs.2009.07.024.
Maniwa T, Okumura T, Isaka M, Nakagawa K, Ohde Y, Kondo H. Recurrence of mediastinal node cancer after lobe-specific systematic nodal dissection for non-small-cell lung cancer. Eur J Cardiothorac Surg. 2013;44:e59-64. https://doi.org/10.1093/ejcts/ezt195.
Adachi H, Sakamaki K, Nishii T, Yamamoto T, Nagashima T, Ishikawa Y, et al. Lobe-specific lymph node dissection as a standard procedure in surgery for non-small cell lung cancer: a propensity score matching study. J Thorac Oncol. 2017;12:85–93. https://doi.org/10.1016/j.jtho.2016.08.127.
Zhao Y, Mao Y, He J, Gao S, Zhang Z, Ding N, et al. Lobe-specific lymph node dissection in clinical stage IA solid-dominant non-small-cell lung cancer: a propensity score matching study. Clin Lung Cancer. 2021;22:e201–10. https://doi.org/10.1016/j.cllc.2020.09.012.
Hishida T, Miyaoka E, Yokoi K, Tsuboi M, Asamura H, Kiura K, et al. Lobe-specific nodal dissection for clinical stage I and II NSCLC: Japanese multi-institutional retrospective study using a propensity score analysis. J Thorac Oncol. 2016;11:1529–37. https://doi.org/10.1016/j.jtho.2016.05.014.
Endo S, Ikeda N, Kondo T, Nakajima J, Kondo H, Yokoi K, et al. Model of lung cancer surgery risk derived from a Japanese nationwide web-based database of 78 594 patients during 2014–2015. Eur J Cardiothorac Surg. 2017;52:1182–9. https://doi.org/10.1093/ejcts/ezx190.
Watanabe S, Suzuki K, Asamura H. Superior and basal segment lung cancers in the lower lobe have different lymph node metastatic pathways and prognosis. Ann Thorac Surg. 2008;85:1026–31. https://doi.org/10.1016/j.athoracsur.2007.10.076.
Aokage K, Yoshida J, Ishii G, Hishida T, Nishimura M, Nagai K. Subcarinal lymph node in upper lobe non-small cell lung cancer patients: is selective lymph node dissection valid? Lung Cancer. 2010;70:163–7. https://doi.org/10.1016/j.lungcan.2010.02.009.
Sakao Y, Okumura S, Mingyon M, Uehara H, Ishikawa Y, Nakagawa K. The impact of superior mediastinal lymph node metastases on prognosis in non-small cell lung cancer located in the right middle lobe. J Thorac Oncol. 2011;6:494–9. https://doi.org/10.1097/JTO.0b013e31820b8891.
Hattori A, Matsunaga T, Takamochi K, Oh S, Suzuki K. Neither maximum tumor size nor solid component size is prognostic in part-solid lung cancer: impact of tumor size should be applied exclusively to solid lung cancer. Ann Thorac Surg. 2016;102:407–15. https://doi.org/10.1016/j.athoracsur.2016.02.074.
Isaka M, Kojima H, Takahashi S, Omae K, Ohde Y. Risk factors for local recurrence after lobectomy and lymph node dissection in patients with non-small cell lung cancer: implications for adjuvant therapy. Lung Cancer. 2018;115:28–33. https://doi.org/10.1016/j.lungcan.2017.11.014.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Rusch VW, Asamura H, Watanabe H, Giroux DJ, Rami-Porta R, Goldstraw P, et al. The IASLC lung cancer staging project: a proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol. 2009;4:568–77. https://doi.org/10.1097/JTO.0b013e3181a0d82e.
Kim HR, Kim DJ, Lee WW, Jheon S, Sung SW. The significance of maximum standardized uptake values in patients with stage I pulmonary adenocarcinoma. Eur J Cardiothorac Surg. 2009;35:712–6. https://doi.org/10.1016/j.ejcts.2008.12.030.
Okada M, Nakayama H, Okumura S, Daisaki H, Adachi S, Yoshimura M, et al. Multicenter analysis of high-resolution computed tomography and positron emission tomography/computed tomography findings to choose therapeutic strategies for clinical stage IA lung adenocarcinoma. J Thorac Cardiovasc Surg. 2011;141:1384–91. https://doi.org/10.1016/j.jtcvs.2011.02.007.
Lin Y, Lin WY, Kao CH, Yen KY, Chen SW, Yeh JJ. Prognostic value of preoperative metabolic tumor volumes on PET-CT in predicting disease-free survival of patients with stage I non-small cell lung cancer. Anticancer Res. 2012;32:5087–91.
Lin JT, Yang XN, Zhong WZ, Liao RQ, Dong S, Nie Q, et al. Association of maximum standardized uptake value with occult mediastinal lymph node metastases in cN0 non-small cell lung cancer. Eur J Cardiothorac Surg. 2016;50:914–9. https://doi.org/10.1093/ejcts/ezw109.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8. https://doi.org/10.1038/bmt.2012.244.
Liu J, Dong M, Sun X, Li W, Xing L, Yu J. Prognostic value of 18F-FDG PET/CT in surgical non-small cell lung cancer: A meta-analysis. PLoS ONE. 2016;11: e0146195. https://doi.org/10.1371/journal.pone.0146195.
Ito H, Suzuki K, Mizutani T, Aokage K, Wakabayashi M, Fukuda H, et al. Long-term survival outcome after lobectomy in patients with clinical T1 N0 lung cancer. J Thorac Cardiovasc Surg. 2020. https://doi.org/10.1016/j.jtcvs.2019.12.072.
Terada Y, Isaka M, Harada H, Konno H, Kojima H, Mizuno T, et al. Radiotherapy for local recurrence of non-small-cell lung cancer after lobectomy and lymph node dissection-can local recurrence be radically cured by radiation? Jpn J Clin Oncol. 2020;50:425–33. https://doi.org/10.1093/jjco/hyz188.
Haruki T, Aokage K, Miyoshi T, Hishida T, Ishii G, Yoshida J, et al. Mediastinal nodal involvement in patients with clinical stage I non-small-cell lung cancer: possibility of rational lymph node dissection. J Thorac Oncol. 2015;10:930–6. https://doi.org/10.1097/JTO.0000000000000546.
Khullar OV, Fernandez FG, Perez S, Knechtle W, Pickens A, Sancheti MS, et al. Time is money: hospital costs associated with video-assisted thoracoscopic surgery lobectomies. Ann Thorac Surg. 2016;102:940–7. https://doi.org/10.1016/j.athoracsur.2016.03.024.
Hishida T, Saji H, Watanabe SI, Asamura H, Aokage K, Mizutani T, et al. A randomized Phase III trial of lobe-specific vs systematic nodal dissection for clinical Stage I-II non-small cell lung cancer (JCOG1413). Jpn J Clin Oncol. 2018;48:190–4. https://doi.org/10.1093/jjco/hyx170.
Abughararah TZ, Jeong YH, Alabbood F, Chong Y, Yun JK, Lee GD, et al. Lobe-specific lymph node dissection in stage IA non-small-cell lung cancer: a retrospective cohort study. Eur J Cardiothorac Surg. 2021;59:783–90. https://doi.org/10.1093/ejcts/ezaa369.
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Isaka, M., Kojima, H., Imai, T. et al. Lobe-specific nodal dissection with intraoperative frozen section analysis for clinical stage-I non-small cell lung cancer: a validation study by propensity score matching. Gen Thorac Cardiovasc Surg 70, 977–984 (2022). https://doi.org/10.1007/s11748-022-01827-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-022-01827-1