Abstract
Hypoxia during one-lung ventilation is a significant problem in descending aortic surgery via left thoracotomy. Veno-arterio-pulmonary-arterial extracorporeal membrane oxygenation (VAPa-ECMO), which consists of veno-arterial extracorporeal membrane oxygenation (VA-ECMO) and an additional arterial branch to perfuse a pulmonary artery (Pa), is useful.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Descending aortic aneurysm surgery via left thoracotomy is an invasive and high-risk operation and still a challenging operation among cardiovascular surgery. Depending on a location of an aortic aneurysm, a method of extracorporeal circulation changes; for example, partial extracorporeal circulation including cardiopulmonary bypass, left heart bypass, and ultra-low hypothermic circulation arrest [1]. However, in any partial extracorporeal circulation, left thoracotomy and right one-lung ventilation are essential for descending aortic aneurysm surgery. Hypoxia, due to right-side pulmonary hemorrhage, atelectasis, and pneumothorax, can be life-threatening. We experienced a case of hypoxia during descending aortic replacement with partial extracorporeal circulation. Therefore, veno-arterio-pulmonary-arterial extracorporeal membrane oxygenation (VAPa-ECMO) was established by adding a pulmonary-arterial perfusion line to send oxygenated blood for a main pulmonary artery, onto veno-arterial extracorporeal membrane oxygenation (VA-ECMO) using a femoral artery and a femoral vein, and we safely replaced descending aortic aneurysm, withdrew from cardiopulmonary bypass, and performed a hemostatic operation.
Case report
A 70-year-old man had undergone an urgent ascending aortic replacement for acute type A aortic dissection 10 years ago. The descending aorta gradually enlarged to 65 mm, and he underwent descending aortic replacement under partial cardiopulmonary bypass.
His preoperative respiratory function data were not poor. The lung capacity was 3230 ml and the percent predicted forced expiratory volume in 1 s was 76.4%. He used to smoke, but quit smoking 30 years before surgery. We were not concerned about his respiratory status before operation.
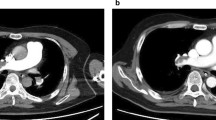
A left-sided double-lumen tube could not be inserted into the left main bronchus because of the stenosis in the left main bronchus due to compression of the aneurysm (Fig. 1). A normal intubation tube was inserted into the trachea, and a blocker was then inserted into the left main bronchus.
The patient was placed in a right lateral decubitus position, and a left inguinal incision was made to secure femoral artery and vein. We performed a left fourth intercostal thoracotomy. Right one-lung ventilation was started, but oxygenation became poor. Therefore, we divided the arterial line of extracorporeal membrane oxygenation (ECMO) into two lines to prepare VAPa-ECMO.
After heparin was administered, 24Fr cannula was inserted into the right atrium from the left femoral vein as a venous line. An artificial graft was anastomosed to the left femoral artery, and 22Fr cannula was inserted into the main pulmonary artery (Fig. 2). Veno-pulmonary-arterial extracorporeal membrane oxygenation (VPa-ECMO) was started with clamping of the femoral arterial line. The flow was started at 2.5 l/min. Thereafter, right one-lung ventilation was performed. It was confirmed that arterial blood oxygen saturation was 100%.
Schema of VAPa-ECMO circuit. A 24Fr cannula was inserted into the right atrium from the left femoral vein as a venous line. An artificial graft was anastomosed to the left femoral artery, and a 22Fr cannula was inserted into the main pulmonary artery. When VAPa-ECMO was started, the total pump flow was increased and blood flow was adjusted by a half clamp in the pulmonary artery line to maintain the lower limb blood pressure and arterial blood oxygen saturation of the upper body. Suction lines consisting of two roller pumps and a cardiotomy reservoir are added. VAPa-ECMO; veno-arterio-pulmonary-arterial extracorporeal membrane oxygenation
After dissection of aortic arch and descending aorta, the aorta was clamped and femoral arterial line was opened. VAPa-ECMO was started. Because lower limb blood pressure decreased, the total pump flow was increased to 5 l/min, and blood flow was adjusted by a half clamp in the pulmonary artery line to maintain the lower limb blood pressure and arterial blood oxygen saturation of the upper body. Subsequently, the descending aorta was clamped and descending aortic replacement was performed.
After the aorta was unclamped, the perfusion to the femoral artery was terminated, and the perfusion to the main pulmonary artery continued at the flow rate of 2.5 l/min. This means conversion from VAPa-ECMO to VPa-ECMO. Protamine was administered and hemostasis was performed while collapsing the left lung. After hemostasis was completed, both lungs were ventilated, systemic oxygenation recovered, and VPa-ECMO was then terminated.
The respirator was withdrawn on the 3rd day after the operation, and the postoperative course was good without organ damage.
Discussion
Left thoracotomy and right one-lung ventilation are essential for descending aortic surgery. The incidence of hypoxemia in one-lung ventilation is reported as 3% [2]. In this case, the preoperative respiratory function was not poor and there was no obesity, but the left main bronchus was narrowed by the aortic aneurysm. It was difficult to insert a double-lumen left bronchial tube. Complex procedure to secure airway might cause bronchial edema and increased secretion, and hypoxemia occurred during right one-lung ventilation in the operation. Veno-venous extracorporeal membrane oxygenation (VV-ECMO) seemed to be one of the solutions in this situation, but we could not access the juggler veins because of right lateral position. Therefore, we planned to add the arterial line to the main pulmonary artery and perform VPa-ECMO, instead of VV-ECMO. The function of VPa-ECMO is almost same as VV-ECMO and more efficient, because short-circuit phenomenon would unlikely occur in VPa-ECMO than in VV-ECMO.
Since we shared the venous cannula and divided the arterial line, we could switch the extracorporeal circulation between VPa-ECMO and VAPa-ECMO instantly.
Surgery using VAPa-ECMO has two advantages. The first point is the stability of oxygenation. With VAPa-ECMO, distal perfusion can be maintained, and at the same time, oxygenation of upper body can be efficiently maintained by sending oxygenated blood directly to a pulmonary artery regardless of the patient’s lung condition. In addition, cannulation to the main pulmonary artery is simple and easy in left thoracotomy, and it is free from short-circuit phenomenon [3].
The second point is that it works advantageously to maintain oxygenation even without axillary arterial perfusion during hemostasis under the one-lung ventilation if the heparin-free circuit is used.
When the arterial line is divided to a pulmonary artery and a femoral artery, blood flow is imbalanced due to a difference in vascular resistance. We increased the flow rate of the centrifugal pump and created a stenosis in the arterial line of the pulmonary artery. During VAPa-ECMO, we adjusted the flow and the stenosis to maintain the blood pressure of the lower body and oxygenation of the upper body.
Conclusion
VAPa-ECMO improves the safety of descending aortic surgery via left thoracotomy for patients in whom hypoxia occurs with right one-lung ventilation.
References
Suga K, Kobayashi Y, Ochiai R. Impact of left heart bypass on arterial oxygenation during one-lung ventilation for thoracic aortic surgery. J Cardiothorac Vasc Anesth. 2017;31:1197–202.
Weksler B. During one-lung ventilation, KISS-keep it simple surgeons. J Thorac Cardiovasc Surg. 2017;154:367–8.
Palmér O, Palmér K, Hultman J, Broman M. Cannula design and recirculation during venovenous extracorporeal membrane oxygenation. ASAIO J. 2016;62:737–42.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Minami, T., Uchida, K., Yasuda, S. et al. Veno-arterio-pulmonary-arterial extracorporeal membrane oxygenation in descending aortic surgery. Gen Thorac Cardiovasc Surg 69, 727–730 (2021). https://doi.org/10.1007/s11748-020-01518-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-020-01518-9