Abstract
Objective
We evaluated beating heart thoracic aortic surgery (BHTAS) using selective myocardial perfusion (SMP) in patients with aortic anomalies with complex surgical needs.
Methods
Between 2012 and 2018, 27 infants with aortic anomalies underwent BHTAS using SMP.
Results
Median body weight was 3.5 kg (range 2.6–5.2). In total, 15 cases of aortic coarctation, 7 cases of hypoplastic left heart syndrome, and 5 cases of interrupted aortic arch were included. An extended aortic arch anastomosis maneuver was used in 7 cases and aortic arch reconstruction compensated with an autologous pericardium patch was used in 6 cases. A Norwood-type procedure was used in 11 cases. The median Aristotle comprehensive score was 13.9 (7.0–20.0). BHTAS cases were not inferior in postoperative CK-MB/CK ratio (12.4 ± 2.8 in BHTAS vs 13.9 ± 3.6 in CTAS, p = 0.09), and there were no instances of myocardial ischemia. Two late deaths occurred due to shunt obstruction (n = 1) and valve malfunction (n = 1). Freedom from aortic reintervention was not inferior to conventional thoracic aortic surgery. BHTAS cases exhibited shorter cardiac arrest time than that of conventional thoracic aortic surgery in similar surgical procedures [CoA/VSD cases: 48.0 ± 8.0 min in the BHTAS cases and 65.7 ± 10.8 min in the CTAS cases (p = 0.0122), simple CoA/re-CoA cases: 0 min in the BHTAS cases and 20.1 ± 3.6 min in the CTAS cases].
Conclusions
BHTAS reduced cardioplegic arrest time while maintaining postoperative CK-MB/CK ratio, mid-term death, and aortic reintervention rates.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Congenital aortic or aortic arch anomalies generally require surgical repair during the neonatal period or early infancy. At times, complicated procedures are necessary for treating patients with thoracic aortic anomalies and/or intracardiac anomalies. Use of Norwood-type procedures or aortic arch repair of a beating heart was first reported more than a decade ago [1, 2]. For some complex cases, we began to perform beating heart thoracic aortic surgery (BHTAS) using selective cerebral perfusion (SCP) and selective myocardial perfusion (SMP) starting in 2012. Herein we report short- to mid-term outcomes of patients who underwent BHTAS using SCP and SMP.
Materials and methods
Study patients
Between January 2012 and December 2018, 62 consecutive patients with congenital aortic or aortic arch obstructions underwent thoracic aortic surgery at Okinawa Prefectural Nanbu Medical Center and Children’s Medical Center. The patients were identified from medical records for inclusion in the study. Two low birth weight infants underwent thoracic aortic surgery using systemic circulatory arrest. One patient was excluded because of the lack of some intraoperative parameter data. In total, 27 patients underwent BHTAS using SMP, and the other 32 patients underwent conventional thoracic aortic surgery (CTAS) using ordinary cardioplegic arrest. The selection is based on a difference of era or surgeon’s preference. This single-center retrospective study was approved by the Okinawa Prefectural Nanbu Medical Center and Children’s Medical Center Research Integrity and Compliance Committee. The requirement of written informed consent was waived.
Surgical procedure
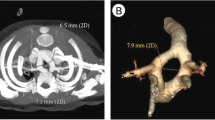
We directly inserted an arterial cannula with a small metal tip into the innominate artery (INNA) via midline sternotomy or through an expanded polytetrafluoroethylene (ePTFE; Gore & Assoc., Flagstaff, AZ) graft. Next, we initiated bicaval venous drainage and cardiopulmonary bypass (CPB). An intracardiac vent was inserted through the right upper pulmonary vein, in cases with biventricular cardiac anatomy. If necessary, another arterial cannula was placed in the descending aorta (DAo), just above the diaphragm, in cases requiring a complicated aortic arch reconstruction maneuver. A cardioplegic spike was placed in the proximal ascending aorta (AAo) and connected to the side arm of the arterial circuit using extension tube with a one-way valve (Supplementary Material Section S1A, B; Fig. 1a). After clamping the neck vessels, DAo and AAo, SCP and SMP were established (Fig. 1b; Video 1).
Intraoperative depiction of beating heart thoracic aortic surgery. In cases with ordinary-sized AAo (a, b) and hypoplastic AAo (c–e). AAo ascending aorta, CP cardioplegic, DAo descending aorta, ePTFE expanded polytetrafluoroethylene, MPA main pulmonary artery, RV right ventricle, SMP selective myocardial perfusion
In cases with hypoplastic AAo, a small selective cardioplegic tip (DLP distal perfusion model 33,000, arteriotomy cannula, Medtronic, Minneapolis, MN) was inserted from transected AAo (Fig. 1c–e; Video 2). During SMP, we maintained an esophageal temperature (as a surrogate of myocardial temperature) of approximately 30 °C to keep each patient’s heart beating. During BHTAS, myocardial hue, heart rate, and ST-T changes on electrocardiography were observed and recorded. Although none of the patients exhibited myocardial ischemia in this series, we were prepared to switch to cardioplegic arrest if any of the above changes were observed.
During BHTAS, we took care so as not to compress the myocardium. For patients with normal cardiac anatomy, we clamped DAo using a Cooley-Derra vessel clamp from the right side of the AAo (Fig. 1b, d, white arrows) so as not to compress the myocardium. If the proximal AAo needed to be incised, this was to be performed under cardioplegic arrest. Other more complex intracardiac procedures were also to be performed under cardioplegic arrest.
Statistical analysis
Descriptive statistics are presented as frequencies and percentages for categorical variables. Continuous variables are expressed as means and standard deviations, or as median values and ranges. Between-group comparisons were made using Student’s t test (for continuous data) and the Mann–Whitney U test (for ordinal data). Other characteristics were compared using the Chi-squared test. Kaplan–Meier curves were generated to reflect time to adverse event-free survival and overall survival. All statistical calculations were performed using JMP Pro Version 14 software (SAS Institute Inc., Cary, NC).
Results
The characteristics of the 27 study patients are presented in Table 1. The median body weight at the time of surgery was 3.5 kg (range 2.6–5.2). The most common aortic morphology was aortic coarctation (CoA), including re-CoA; there were 15 cases (56%). There were seven cases (26%) of hypoplastic left heart syndrome.
The surgical procedures are presented in Table 2. Aortic arch repair, using an extended aortic arch anastomosis (EAAA), was done in seven cases (26%), and aortic arch reconstruction compensated with an autologous pericardium patch was used in six cases (22%). Norwood-type procedures were used in 11 cases (41%). VSD closure alone or no additional procedure was used in eight cases (30%). Three patients additionally underwent an arterial switch operation with intraventricular rerouting, and another three cases also received atrioventricular valvuloplasty. Consequently, the Aristotle basic scores and comprehensive scores were 10.9 (6.0–14.5) and 13.9 (7.0–20.0), respectively [3]. In addition, a pulmonary blood flow source combined with Norwood-type procedure and Blalock–Taussig shunt was used in five cases, right ventricle–pulmonary artery shunt in four cases, and bidirectional Glenn in two cases.
The aim of the BHTAS maneuver was to save cardioplegic arrest time. The reasonable adaptations of the BHTAS approach included complicated aortic arch reconstruction (aortic arch reconstruction procedure compensated with autologous pericardium or Norwood-type procedure, n = 17, 63%), additional complicated procedures (n = 4, 15%), unusual aortic arch repair maneuver (simple but not familiar aortic arch repair other than EAAA procedure, n = 3, 12%), and combined palliative operations (n = 3, 11%). The adaptation range of BHTAS expanded year by year (Supplementary Material Section S2).
Detailed intraoperative data are presented in Table 3. Arterial perfusion was carried out using INNA alone in 11 cases (41%), and combined DAo perfusion was used in 16 cases. We applied the lower body circulatory arrest maneuver to 11 cases, and the median lower body circulatory arrest time was 14 min. Mean intraoperative minimum esophageal temperature was higher for the BHTAS cases (29.2 ± 1.8 °C), compared with that of the CTAS cases (26.9 ± 1.9 °C). There was no significant difference between the groups in mean intraoperative minimum rectal temperature and minimum regional cerebral oxygen saturation levels [4].
Median CBP time was 215 min (range 45–316), and cardiac arrest time was 42.5 min (range 0–156). Eight patients (30%) tolerated the entire operation without cardiac arrest. When comparing similar surgical procedures like CoA/VSD or simple CoA repair between BHTAS and CTAS cases, their cardiac arrest time in BHTAS was shorter than that in CTAS cases. We compared 4 BHTAS cases with 10 CTAS cases among the CoA/VSD cases. The mean CPB time was 182.0 ± 45.2 min in the BHTAS cases and 132.0 ± 36.6 min in the CTAS cases, respectively. In contrast, the mean cardiac arrest time was 48.0 ± 8.0 min in the BHTAS cases and 65.7 ± 10.8 min in the CTAS cases, respectively (p = 0.0122). In addition, we compared three BHTAS cases with eight CTAS cases among the simple CoA/re-CoA cases. The mean CPB time was 97.0 ± 16.1 min in the BHTAS cases and 70.0 ± 17.9 min in the CTAS cases, respectively. In contrast, the mean cardiac arrest time was 0 min in the BHTAS cases and 20.1 ± 3.6 min in the CTAS cases, respectively. From these results, it can be suggested that BHTAS technique could contribute to reduce cardiac arrest time. In CPB time, it is difficult to compare BHTAS cases with CTAS cases. But, it may cost a few minutes of CPB time to establish BHTAS circuit.
No patient in BHTAS cases developed clinical symptoms of myocardial ischemia. Temporal measurements of CK, CK-MB, and the CK-MB/CK ratio are presented in Supplementary Material Section S3. Immediately after commencing CPB, there were no significant differences between the groups in any of these measures. The CK-MB/CK ratio exhibited no significant differences between the groups in the immediate postoperative period (12.4 ± 2.8 in BHTAS vs 13.9 ± 3.6 in CTAS, p = 0.09).
There were no instances of early mortality. One case of mediastinitis was observed. Scheduled delayed sternal closure was performed in eight cases, with no case of unscheduled delayed sternal closure. The median follow-up period was 40.1 months (4.6–75.3), and there were two late deaths. One patient died because of complications from a mechanical prosthetic valve malfunction at 25.6 months after the initial operation. Another patient died of cerebral hemorrhage during emergent extracorporeal membrane oxygenation because of severe desaturation due to his right ventricle–pulmonary artery shunt obstruction at 6.2 months after the initial operation.
The estimated freedom from death rates were 95.8% at 1 year, 91.0% at 3 years, and 91.0% at 5 years (Fig. 2a). In the BHTAS cases, there were two aortic reintervention cases. Two patients underwent percutaneous transluminal angioplasty for re-CoA, one at 6.7 months and one at 10.1 months after their initial operations. There were four aortic reintervention cases in the CTAS cases. Two patients underwent surgical repair for re-CoA at 4.6 months and 4.1 months, respectively, after the initial operation. One patient underwent surgical repair for AAo stenosis at 11.9 months after the initial operation. Another patient underwent percutaneous transluminal angioplasty for re-CoA at 11.1 months after initial operation. The estimated freedom from aortic reintervention rates were 91.1% at 1 year, 91.1% at 3 years, and 91.1% at 5 years in BHTAS cases and 86.1% at 1 year, 86.1% at 3 years, and 86.1% at 5 years in CTAS cases, respectively, (p = 0.561) (Fig. 2b). No patient showedclinical symptoms of neurological abnormalities. Furthermore, none of the patients experienced coagulopathies or bleeding complications.
Discussion
There are some reports that described the use of a Norwood-type procedure on a beating heart, and evidence exists to suggest that the beating heart procedure improved postoperative hemodynamics and hospital mortality [5, 6]. However, previously reported maneuvers did not use SMP. Turek et al. reported use of a Norwood-type procedure with SMP, and their survival, postoperative cardiac function, and lactate levels emerged as non-inferior to the standard technique [7]. Although there is a report of surgical repair using SMP for CoA and IAA, the authors did not compare their method with the conventional procedure [8]. There is a report that BHTAS was less superior in total inotropic, amount of pleural effusion, and length of intensive care unit and hospital stay, to conventional procedure [9]. There are some reports of excellent surgical results achieved using BHTAS with SMP for Norwood-type and CoA repairs [10,11,12]. However, once again, BHTAS was not compared with the conventional procedure.
Rüffer et al. reported BHTAS with SMP using an additional roller pump [13]. They found that postoperative troponin T and CK-MB were significantly lower in the BHTAS cases than in the CTAS cases. Our arterial circuit was a one pump system that used the side arm of the arterial circuit. Although we adapted this maneuver for more cases than Rüffer’s group, there were no intraoperative complications in our series. Although our BHTAS cases included more patients considered “complicated cases” (the median Aristotle comprehensive score was 13.9 for BHTAS vs 8.3 for CTAS), the BHTAS cases were not inferior in the CK-MB/CK ratio. Although the postoperative status was not significantly different between BHTAS and CTAS groups, considering that the Aristotle score was significantly higher in BHTAS group, BHTAS had superiority over CTAS.
Further, there were similar results in aortic reintervention in our study. Patients in both the BHTAS and CTAS cases seem to have received aortic surgeries of similar quality. In BHTAS cases, there were two late deaths: one valve malfunction patient and one right ventricle–pulmonary artery shunt obstruction patient. The causes of their death were not related to re-CoA and/or cardiac function. Therefore, differences between BHTAS and CTAS maneuver appear to be unrelated to the cause of death.
In 8 out of 27 BHTAS cases (30%), surgery was completed without cardioplegic arrest. For patients who underwent the EAAA procedure or a Norwood-type procedure with a relatively large AAo, we could have completed surgery with a beating heart. In case of Norwood-type procedure with hypoplastic AAo, we have sutured the proximal AAo under cardioplegic arrest. Intraventricular procedures have been also performed under cardioplegic arrest. From the results of similar surgical procedures, we concluded that the BHTAS technique could contribute to reduce the cardiac arrest time. Regarding the CPB time, it is difficult to compare the BHTAS cases with the CTAS cases but establishing a BHTAS circuit may have cost us a few minutes of CPB time.
This study had some limitations. Because our cohort was a mixture of biventricular patients/single right ventricular patients, with/without intracardiac procedure, and patients with various preoperative conditions, it is difficult to evaluate postoperative cardiac function. The BHTAS cases included some patients with single right ventricle and/or complex heart disease. Even in the patients with simple CoA or CoA/VSD, we used the BHTAS technique for more complex cases.
Hence, we substituted CK-MB and the CK-MB/CK ratio for changes in cardiac ischemia during the acute postoperative phase. We routinely measure CK and CK-MB just after initiating CPB and during the immediate postoperative period. However, fewer than half of patients had CK-MB measured on POD1 and POD2. Therefore, we had little CK-MB data, with the exception of measures obtained just after CPB initiation and during the early postoperative period. Further, we did not measure troponin T and/or troponin I, because there were no patients with suspected postoperative ischemic myocardial changes at that time.
In conclusion, BHTAS using SCP and SMP was associated with excellent surgical outcomes. BHTAS appeared to reduce the cardioplegic arrest time without complications. Considering that the Aristotle score was significantly higher in BHTAS group, the BHTAS cases showed no postoperative adverse effects on the CK-MB/CK ratio, mid-term death rate, or aortic reintervention rate.
References
Király L, Prodán Z. Continuous systemic perfusion via collaterals at moderate hypothermia in aortic arch repairs in neonates. Croat Med J. 2002;43:656–9.
Ishino K, Kawada M, Irie H, Kino K, Sano S. Single-stage repair of aortic coarctation with ventricular septal defect using isolated cerebral and myocardial perfusion. Eur J Cardiothorac Surg. 2000;17:538–42.
Lacour-Gayet F, Clarke D, Jacobs J, Comas J, Daebritz S, Daenen W, et al. The Aristotle score: a complexity-adjusted method to evaluate surgical results. Eur J Cardiothorac Surg. 2004;25:911–24.
Cho AR, Kwon JY, Kim C, Hong JM, Kang C. Effect of sensor location on regional cerebral oxygen saturation measured by INVOS 5100 in on-pump cardiac surgery. J Anesth. 2017;31:178–84.
Asfour B, Fink C, Sinzobahamvya N, Wetter J, Urban AE, Photiadis J. Modified children's II operation on the beating heart allows growth potential. Ann Thorac Surg. 2005;80:e14–e1616.
Photiadis J, Asfour B, Sinzobahamvya N, Fink C, Schindler E, Brecher AM, et al. Improved hemodynamics and outcome after modified Norwood operation on the beating heart. Ann Thorac Surg. 2006;81:976–81.
Turek JW, Hanfland RA, Davenport TL, Torres JE, Duffey DA, Patel SS, et al. Norwood reconstruction using continuous coronary perfusion: a safe and translatable technique. Ann Thorac Surg. 2013;96:219–23.
Lim HG, Kim WH, Jang WS, Lim C, Kwak JG, Lee C, et al. One-stage total repair of aortic arch anomaly using regional perfusion. Eur J Cardiothorac Surg. 2007;31:242–8.
Lim HG, Kim WH, Park CS, Chung ES, Lee CH, Lee JR, et al. Usefulness of regional cerebral perfusion combined with coronary perfusion during one-stage total repair of aortic arch anomaly. Ann Thorac Surg. 2010;90:50–7.
De Rita F, Lucchese G, Barozzi L, Menon T, Faggian G, Mazzucco A, et al. Selective cerebro-myocardial perfusion in complex congenital aortic arch pathology: a novel technique. Artif Organs. 2011;35:1029–35.
Hoxha S, Abbasciano RG, Sandrini C, Rossetti L, Menon T, Barozzi L, et al. Selective cerebro‐myocardial perfusion in complex neonatal aortic arch pathology: midterm results. Artif Organs. 2018;42:457–63.
Gil-Jaurena JM, González-López MT, Pita A, Pérez-Caballero R, Herviás M, Blanco D. Beating-heart aortic arch surgery in neonates and infants. Interact Cardiovasc Thorac Surg. 2018;27:586–90.
Rüffer A, Klopsch C, Münch F, Gottschalk U, Mir TS, Weil J, et al. Aortic arch repair: let it beat! Thorac Cardiovasc Surg. 2012;60:189–94.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

11748_2020_1304_MOESM1_ESM.jpg
Supplementary material section S1. Beating heart thoracic aortic surgery circuit. Schema of arterial circuit (A) and actual arterial circuit (B). A cardioplegic spike or tip was placed at the proximal ascending aorta and connected to the side arm of the arterial circuit using an extension tube with a one-way valve. CP = cardioplegic; DAo = descending aorta; ePTFE = expanded polytetrafluoroethylene; SCP = selective cerebral perfusion; SMP = selective myocardial perfusion (JPG 84 kb)

11748_2020_1304_MOESM2_ESM.jpg
Supplementary material section S2. Cases of BHTAS and CTAS. Number of patients. BHTAS = beating heart thoracic aortic surgery; CTAS = conventional thoracic aortic surgery (JPG 83 kb)

11748_2020_1304_MOESM3_ESM.jpg
Supplementary material section S3. Temporal measurements of CK and CK-MB. *1: Just after cardiopulmonary bypass initiation. *2: Just after cardiac surgery. *3: Postoperative day 1. *4: Postoperative day 2. CK = creatine kinase; CK-MB = creatine kinase MB isoenzyme (JPG 39 kb)
11748_2020_1304_MOESM4_ESM.mpg
Supplementary Video 1. BHTAS using ordinary cardioplegic spike. AAo = ascending aorta; ASO = arterial switch operation; BHTAS = beating heart thoracic aortic surgery; CP = cardioplegic; DAo = descending aorta; EAAA = extended aortic arch anastomosis; IVR = intraventricular rerouting (MPG 70902 kb)
11748_2020_1304_MOESM5_ESM.mpg
Video 2. BHTAS for hypoplastic aorta. AAo = ascending aorta; BHTAS = beating heart thoracic aortic surgery; CP = cardioplegic; HLHS = hypoplastic left heart syndrome; INNA = innominate artery (MPG 107664 kb)
Rights and permissions
About this article
Cite this article
Fuchigami, T., Nishioka, M., Tamashiro, Y. et al. Beating heart thoracic aortic surgery under selective myocardial perfusion for patients with congenital aortic anomalies. Gen Thorac Cardiovasc Surg 68, 956–961 (2020). https://doi.org/10.1007/s11748-020-01304-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-020-01304-7