Abstract
Background
Extended arch repair for acute type A aortic dissection remains controversial. Our strategy for acute type A aortic dissection was primary entry resection and tear-oriented ascending/hemiarch replacement for patients with the intimal tear in the ascending aorta or is not found in the ascending/aortic arch. Extended total/partial arch replacement was performed for patients with the tear located in the aortic arch. Here, we investigated the validity of our strategy from the viewpoints of long-term survival and reoperation.
Patients and methods
Between 2003 and 2014, 267 acute type A aortic dissection patients (mean age; 65.2 ± 12.9 years, 134 men and 133 women) underwent emergent surgical repair. Ascending/hemiarch replacements were performed in 225 patients (ascending/hemiarch group) and total/partial arch replacements in 42 patients (arch group). Early and late outcomes of both groups were compared.
Results
The hospital mortality rates in the ascending/hemiarch and the arch groups were 4.4 and 9.5 %, respectively (p = 0.25). For ascending/hemiarch and arch groups, the actuarial survival rates were 80.7 vs. 84.3 % after 5 years, and 66.4 vs. 74.6 %, respectively, after 10 years (p = 0.94). For ascending/hemiarch and arch groups, reoperation-free survival rates were 72.1 vs. 77.1 % after 5 years, and 62.0 vs. 67.1 %, respectively, after 10 years (p = 0.85).
Conclusions
We observed no significant differences in the actuarial survival or reoperation-free survival rates between the groups. These findings suggest that tear-oriented ascending/hemiarch replacement for acute type A aortic dissection does not increase the risk of long-term mortality or reoperation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute type A aortic dissection (ATAAD) is a lethal condition that is associated with a high risk of mortality. Although operative mortality has improved, patients remain at high potential risk of reoperation and vascular-related complications in the long-term period [1–3]. Although several studies reported that extended arch repair decreases the risk of reoperation in the long term [4–7], the procedure may increase operative morbidity or mortality. In addition, it remains equivocal whether extended arch repair can reduce the risk of long-term death. Because the preservation of life should be prioritized in such life-threatening conditions, we limited ascending/hemiarch replacement to patients for whom the entry site was located in the ascending aorta or those in whom the entry is not found in the ascending or aortic arch. For patients whose entry extended to or was located in the aortic arch, we performed total/partial arch replacement. The aim of this study was to determine whether our strategy for ATAAD influences long-term outcomes.
Patients and methods
The institutional review board approved this retrospective observational study, and the approval included a waiver of informed consent. Between 2004 and 2014, 267 patients with AAAD (mean age, 65 ± 12 years old; 134 men and 133 women) underwent surgical repair at Jichi Medical University Hospital. Ascending/hemiarch replacement was performed in 225 patients (ascending/hemiarch group, 84.3 %), and total/partial arch replacement was performed in 42 patients (arch group, 15.7 %). Emergency operations were performed within 48 h of onset for all patients.
Retrosternal chest pain and back pain were the common presenting symptoms. Computed tomography scanning and echocardiography were the common modalities of definitive diagnosis. Angiography was not routinely performed. When the diagnosis of AAAD was confirmed by CT scan and echocardiography, the patient was transferred to the operating room as soon as possible.
Surgical techniques
Surgery was performed with standard cardiopulmonary bypass under hypothermic circulatory arrest (bladder temperature of 26–28 °C). During circulatory arrest, either antegrade selective cerebral perfusion or retrograde cerebral perfusion was performed for brain protection. The distal anastomosis site depended on the site of intimal tear. Ascending/hemiarch aortic replacement was performed in patients with the intimal tear localized in the ascending aorta or in the lesser curvature of the transverse aortic arch. When the intimal tear extended close to the orifice of the arch vessels, total arch replacement was performed. When the intimal tear could not be identified in the ascending or aortic arch (so called “DeBakey IIIb retrograde dissection”), we simply replaced the ascending aorta. Both proximal and distal anastomosis were performed with reinforcing by double felt strips for reapproximation of the dissected aortic layers (adventia inversion technique was not used). Gelatin–resorcinol–formaldehyde (GRF) glue was not used to avoid the risk of aortic wall necrosis. Elephant trunk technique or open stent grafting for total arch replacement was not used in most cases. When the intimal tear extended to the sinus of Valsalva or we observed root dilatation associated with annulo-aortic ectasis, aortic root replacement was performed.
Follow-up
Outcome data were obtained through patient follow-up. We either examined patients at our outpatient clinic or contacted them by letter or telephone. The follow-up rate was 98 % (6 patients were lost to follow-up) with a mean duration of 57 ± 32 months (1–130 months).
Statistical analysis
Continuous variables were compared using unpaired two-tailed t-test and were expressed as the mean ± SD. Categorical variables were presented as counts, and differences between groups were assessed by Fisher’s exact test. Overall survival was defined as the time from surgery to death from any cause. Time-related survival was estimated using the Kaplan–Meier method and compared by log-rank test. Statistical analysis was performed with Stat View 5.0 (Abacus Concepts Inc., Berkeley, CA). P values <0.05 were considered statistically significant.
Results
The characteristics of the two groups are listed in Table 1. Compared with ascending/hemiarch replacement, arch replacement was performed in significantly younger patients who were more likely to be men (p < 0.01). Furthermore, arch replacement was performed more often in patients with maintenance hemodialysis (p = 0.03). There were no other differences in any of the preoperative variables evaluated. Risk analysis based upon Japan score indicates no difference between the two groups (Table 1). Operative data indicated that there were no significance differences in concomitant procedures. Cardiopulmonary bypass and operation times were significantly longer in the arch replacement group (p < 0.01; Table 2).
In-hospital mortality and morbidity
Hospital mortality and morbidity are described in Table 3. The overall hospital mortality was 5.2 % (14 patients). The hospital mortality rate was 4.4 % (10 of 225 patients) in the ascending/hemiarch group. Causes of death were the following: cerebral ischemia (n = 4 patients), pneumonia (n = 2), heart failure (n = 1), postoperative reperfusion injury (n = 1), rupture of residual false lumen (n = 1), and hepatic failure (n = 1). The hospital mortality rate in the arch group was 9.5 % (4 of 42 patients). The causes of death were the following: cerebral ischemia (n = 2), heart failure (1 patient), and multiple organ failure (1 patient). There were no statistical differences in hospital mortality between the two groups (p = 0.25).
Several morbidities occurred during the postoperative period. However, there were no significant differences in morbidities between the two groups. The duration of hospital stay was 26 ± 20 days in the ascending/hemiarch group and 29 ± 17 days in the arch group (p = 0.28). The patency rate of the distal false lumen and diameter of the downstream aorta 2–3 weeks after surgery was similar between the two groups (Table 3).
Actuarial and reoperation-free survival
After discharge from the hospital, thirty-three of the ascending/hemiarch patients (15.3 %) and 4 of the Arch patients (10.5 %) died. There were no significant differences in the late mortality rate (p = 0.47). The causes of deaths are described in Table 4. Aorta-related deaths occurred in 2.3 % (5 of 215 patients) in the ascending/hemiarch group and 2.6 % (1 of 38 patients) in the arch group. Aorta-related deaths in the ascending/hemiarch group included rupture of the residual false lumen (n = 1), aortic dissection (n = 1), consumption coagulopathy (n = 1), postoperative pneumonia after repeat surgery (n = 1), and postoperative cerebral hemorrhage after repeat surgery (n = 1). In the arch group, one patient died of rupture of anastomotic pseudoaneurysm. Aorta-related death rates indicated no significant difference between the groups (p > 0.99).
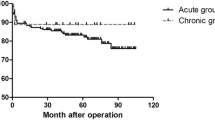
The actuarial survival rates including hospital death were 80.7 ± 3.0 % at 5 years and 66.4 ± 6.3 % at 10 years in the ascending/hemiarch group. In the arch group, the rates were 84.3 ± 6.0 % at 5 years and 74.6 ± 8.3 % at 10 years (p = 0.94). Log-rank survival analysis indicated no significance difference in actuarial survival rates between the groups (p = 0.94). The actuarial survival curves for the two groups are shown in Fig. 1.
Reoperations were performed for the dilated downstream aorta in 21 patients after discharge from the hospital (19 patients in the ascending/hemiarch group and 2 patients in the arch group; Table 4). In the ascending/hemiarch group, reoperations included 9 descending aorta replacements, 2 thoracoabdominal replacements, 2 total arch replacements, one arch/descending aorta replacement, and 5 endovascular surgeries. In the arch group, reoperations included one descending aorta replacement and one endovascular surgery for descending aorta. Actuarial reoperation-free survival rates at 5 and 10 years were 72.1 % ± 3.4 % and 62.0 ± 5.7 %, respectively, in the ascending/hemiarch group, and 77.1 % ± 7.3 % and 67.1 ± 9.2 %, respectively, in the arch group (p = 0.85). The actuarial reoperation-free survival curves are shown in Fig. 2.
Discussion
Despite recent advances in cardiac surgery, ATAAD remains associated with high mortality and morbidity during short- and long-term follow-up. Early surgical mortality rates are estimated to range from 4.7 to 16.9 % [1, 2, 4–9, 11, 12], with 5-year survival rates of 73–89 % [6, 9, 11]. In the present series, the in-hospital mortality rate was 5.2 %, and the actuarial survival rate was approximately 80 % at 5 years, both rates were comparable to those of previous reports. The principal finding of this study was that both ascending/hemiarch replacement and arch replacement for AADA were associated with similarly low hospital mortality rates, and the incidences of late death and long-term aortic events of limited ascending/hemiarch replacement were similarly low when compared with extensive aortic arch replacements.
Patients with ATAAD are at risk of cardiac tamponade, rupture, aortic regurgitation, and malperfusion. In such life-threatening conditions, the first priority should be the patient’s life and use of less invasive surgeries. To achieve this aim, some groups advocated a conservative tear-oriented conservative approach [8–10]. They reported that tear-oriented conservative ascending/hemiarch replacement with resection of the intimal tear did not increase the risk of reoperation and would not compromise late results. While the inherent pathological characteristics of the dissection process affected the entire length of the aorta in most patients with ATAAD, other groups have advocated the aggressive strategy of complete replacement of the ascending aorta and aortic arch (extensive aortic repair) [4–7]. Those groups recommended extensive aortic arch repair because of its capability of reducing the risk of distal dissection, promoting the occlusion and thrombosis of the false lumen, and achieving a favorable long-term prognosis; however, some reports suggest that extensive arch repair is associated with greater morbidity and mortality than is ascending/hemiarch replacement [6, 13, 14]. Although Omura et al. recently reported that extensive arch replacement reduced distal aortic events without compromising early results [11], it remains controversial whether surgeons should perform extended arch replacement to improve long-term outcomes or use a conservative strategy with ascending/hemiarch replacement to palliate the life-threatening condition. The present study indicated that ascending/hemiarch replacement did not compromise the actuarial survival rate and aorta event-free survival rates compared with arch replacement. Although operative mortality and morbidity rates of the arch replacement were not inferior to those of the ascending/hemiarch replacement, extensive arch replacement was associated with longer cardiopulmonary bypass time and operation time, both of which are considered potential risks of operative mortality and morbidity [12].
Yan et al. performed a meta-analysis using pooled data regarding the surgical strategy for ATAAD and evaluated the less aggressive proximal aortic repair versus extensive aortic repair [13]. They concluded that less aggressive proximal repair had lower operative mortality than did extensive repair, but was also associated with increased incidence rate of late aortic re-intervention; however, prognostic results, including long-term mortality, were similar for both. These results suggest that re-intervention has been performed safely, on an elective basis. In fact, recent studies reported that redo aortic surgery for proximal/distal dilatation was achieved with low operative risk when the procedures were carried out an on elective basis [14, 15]. They recommended the ascending/hemiarch replacement for initial surgical strategy and the untreated aortic arch should be electively performed in the chronic period, if necessary [14, 15]. However, patients with Malfan syndrome are more prone to develop late complications, and this condition has been reported as a risk factor that affects long-term results [8, 9, 15]. As Shiono et al. mentioned, [9] extensive surgical strategy might be necessary for this patient cohort.
In this study, patency rate of downstream false lumen was higher than previous reports [2, 16]. We did not use the additional procedures such as elephant trunk technique, open stent grafting, or surgical adhesives including GRF-glue for re-approximation of dissected aorta. These factors may partially explain higher patency rate of false lumen. For remodeling to the false lumen, open stent grafting may effective. Uchida mentioned in the review article that employing the graft diameter of 90 % of total aortic diameter and the limited distal landing zone up to the T4 vertebral level prevent new intimal tear and spinal cord injury effectively [16]. A commercially available open stent graft has been introduced recently, and this may encourage the long-term surgical outcomes of ATAAD.
Our study has several limitations. First, it was a non-randomized and retrospective study. Second, the small sample size and relatively short-term follow-up are clear limitations. Third, this study encompasses data over a time line of 10 years. During this time, variability in factors, such as surgical technique and perioperative management, can influence outcomes.
Conclusions
We observed no significant differences in the actuarial survival and reoperation-free survival rates between the tear-oriented ascending/hemiarch and extensive aortic arch replacements. Tear-oriented ascending/hemiarch replacement did not increase the risk of long-term mortality or reoperation. To reduce the operative mortality without compromising late outcomes among patients with ATAAD, our tear-oriented conservative strategy might be appropriate.
References
Kimura N, Itoh S, Yuri K, Adachi K, Matsumoto H, Yamaguchi A, et al. Reoperation for enlargement of the distal aorta after initial surgery for acute type A aortic dissection. J Thorac Cardiovasc Surg. 2015;149:S91–8.
Kimura N, Tanaka M, Kawahito K, Yamaguchi A, Ino T, Adachi H. Influence of patent false lumen on long-term outcome after surgery for acute type A aortic dissection. J Thorac Cardiovasc Surg. 2008;136:1160–6.
Zierer A, Voeller RK, Hill KE, Kouchoukos NT, Damiano Jr RJ, Moon MR. Aortic enlargement and late reoperation after repair of acute type A aortic dissection. Ann Thorac Surg. 2007;84:479–86 (discussion 486–7).
Uchida N, Shibamura H, Katayama A, Shimada N, Sutoh M, Ishihara H. Operative strategy for acute type a aortic dissection: ascending aortic or hemiarch versus total arch replacement with frozen elephant trunk. Ann Thorac Surg. 2009;87:773–7.
Takahara Y, Sudo Y, Mogi K, Nakayama M, Sakurai M. Total aortic arch grafting for acute type A dissection: analysis of residual false lumen. Ann Thorac Surg. 2002;73:450–4.
Kazui T, Washiyama N, Muhammad BA, Terada H, Yamashita K, Takinami M, et al. Extended total arch replacement for acute type a aortic dissection: experience with seventy patients. J Thorac Cardiovasc Surg. 2000;119:558–65.
Urbanski PP, Siebel A, Zacher M, Hacker RW. Is extended aortic replacement in acute type A dissection justifiable? Ann Thorac Surg. 2003;75:525–9.
Westaby S, Saito S, Katsumata T. Acute type A dissection: conservative methods provide consistently low mortality. Ann Thorac Surg. 2002;73:707–13.
Shiono M, Hata M, Sezai A, Niino T, Yagi S, Negishi N. Validity of a limited ascending and hemiarch replacement for acute type A aortic dissection. Ann Thorac Surg. 2006;82:1665–9.
Tanaka M, Kimura N, Yamaguchi A, Adachi H. In-hospital and long-term results of surgery for acute type A aortic dissection: 243 consecutive patients. Ann Thorac Cardiovasc Surg. 2012;18:18–23.
Omura A, Miyahara S, Yamanaka K, Sakamoto T, Matsumori M, Okada K, et al. Early and late outcomes of repaired acute DeBakey type I aortic dissection after graft replacement. J Thorac Cardiovasc Surg. 2015;151:341–8.
Conzelmann LO, Weigang E, Mehlhorn U, Abugameh A, Hoffman I, Blettner M, et al. Mortality in patients with acute aortic dissection type A: analysis of pre- and intraoperative risk factors from the German Registry for Acute Aortic Dissection Type A (GERAADA). Eur J Cardiothorac Surg. 2016;49:e44–52.
Yan Y, Xu L, Zhang H, Xu ZY, Ding XY, Wang SW, et al. Proximal aortic repair versus extensive aortic repair in the treatment of acute type A aortic dissection: a meta-analysis. Eur J Cardiothorac Surg. 2015;. doi:10.1093/ejcts/ezv351.
Rylski B, Beyersdorf F, Kari FA, Schlosser J, Blanke P, Siepe M. Acute type A aortic dissection extending beyond ascending aorta: Limited or extensive distal repair. J Thorac Cardiovasc Surg. 2014;148:949–54 (discussion 954).
Luciani N, De Geest R, Lauria G, Farina P, Luciani M, Glieca F, et al. Late reoperations after acute aortic dissection repair: single-center experience. Asian Cardiovasc Thorac Ann. 2015;23:787–94.
Uchida N. Open stent grafting for complex diseases of the thoracic aorta: clinical utility. Gen Thorac Cardiovasc Surg. 2013;61:118–26.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kei Aizawa and other coauthors have no conflict of interest.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Rights and permissions
About this article
Cite this article
Aizawa, K., Kawahito, K. & Misawa, Y. Long-term outcomes of tear-oriented ascending/hemiarch replacements for acute type A aortic dissection. Gen Thorac Cardiovasc Surg 64, 403–408 (2016). https://doi.org/10.1007/s11748-016-0648-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-016-0648-x