Abstract
Lipid emulsions for parenteral nutrition are used to provide calories and essential fatty acids for patients. They have been associated with hypertriglyceridemia, hypercholesterolemia, and metabolic stress, which may promote the development of endothelial dysfunction in patients. The aim of the present study was to determine whether five different industrial lipid emulsions may affect the endothelial function of coronary arteries. Porcine coronary artery rings were incubated with lipid emulsions 0.5, 1, or 2% (v/v) for 30 min before the determination of vascular reactivity in organ chambers and the level of oxidative stress using electron paramagnetic resonance. Incubation of coronary artery rings with either Lipidem®, Medialipid® containing long- and medium-chain triacylglycerols (LCT/MCT), or SMOFlipid® containing LCT, MCT, omega-9, and -3, significantly reduced the bradykinin-induced endothelium-dependent relaxation, affecting both the nitric oxide (NO) and endothelium-dependent hyperpolarization (EDH) components, whereas, Intralipid® containing LCT (soybean oil) and ClinOleic® containing LCT (soybean and olive oil) did not have such an effect. The endothelial dysfunction induced by Lipidem® was significantly improved by indomethacin, a cyclooxygenase (COX) inhibitor, inhibitors of oxidative stress (N-acetylcysteine, superoxide dismutase, catalase) and transition metal chelating agents (neocuproine, tetrathiomolybdate, deferoxamine and l-histidine). Lipidem® significantly increased the arterial level of oxidative stress. The present findings indicate that lipid emulsions containing LCT/MCT induce endothelial dysfunction in coronary artery rings by blunting both NO- and EDH-mediated relaxations. The Lipidem®-induced endothelial dysfunction is associated with increased vascular oxidative stress and the formation of COX-derived vasoconstrictor prostanoids.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lipid emulsions are commonly used to provide a nutritional source of calories and to prevent essential fatty acid deficiency in critically ill patients [1–3]. Their benefits include the reduction of the potential side effects of high glucose perfusion, an essential fatty acids supply, and an improved nitrogen balance [4]. Several studies have reported that infusion of lipid emulsions is related to hypertriglyceridemia [5], hypercholesterolemia, and metabolic stress, leading to acute elevation of the free fatty acid (FFA) level, which may promote the development of endothelial dysfunction by decreasing nitric oxide (NO) formation [6–9]. Furthermore, ex vivo studies have reported that some individual fatty acids, such as lauric acid and stearic acid, attenuate the endothelium-dependent relaxation induced by acetylcholine in rabbit aorta rings at physiological concentrations [10].
Formulations of clinically used lipid emulsions have different proportions of fatty acids, and, their biological properties may vary depending on their composition. The first generation lipid emulsion Intralipid® containing a large amount of long-chain triacylglycerols (LCT) from soybean oil including the n-6 polyunsaturated fatty acid (PUFA) linoleic acid (18:2n-6) and a relatively low amount of α-linolenic acid (18:3n-3) [11, 12]. Linoleic acid is readily converted to arachidonic acid (20:4n-6) and subsequently metabolized via the cyclooxygenase (COX) and lipo-oxygenase (LOX) pathways to pro-inflammatory mediators, such as prostaglandins, thromboxanes, and leukotrienes [13]. The second generation lipid emulsions with a lower PUFA content have been developed by partially replacing the LCT-containing soybean oil by various oils such as the medium chain triacylglycerols (MCT)-containing coconut oil (Medialipid®), LCT-containing olive oil (ClinOleic®), LCT/MCT-containing fish oil (Lipidem®), or, as a third-generation of lipid emulsions, LCT/MCT-containing olive and fish oils, rich sources of long-chain n-3 PUFAs (SMOFlipid®) [14].
Omega-3 long-chain PUFAs, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which can compete with arachidonic acid for the production of less inflammatory eicosanoids, are absent in vegetable oils [15]. A recent study has indicated the ability of both EPA, DHA, and, in particular, the EPA:DHA 6:1 ratio to induce endothelium-dependent relaxations of porcine coronary artery rings, and to increase the endothelial formation of NO subsequent to the redox-sensitive activation of the phosphoinositide 3-kinase/Akt pathways leading to the phosphorylation of eNOS at the activation site Ser1177 [16].
Therefore, the aim of the present study was to determine the effect of five different industrial lipid emulsions on the endothelial function of isolated porcine coronary arteries. The endothelial function was assessed in response to bradykinin, a potent inducer of endothelium-dependent relaxations of human and porcine coronary arteries involving both NO and endothelium-dependent hyperpolarization (EDH) [17].
Materials and Methods
Lipid Emulsions and Reagents
The following lipid emulsions (20%) were tested: Intralipid®, Lipidem®, Medialipid®, ClinOleic®, and SMOFlipid®. The composition of the lipid emulsions in terms of sources of oil and major fatty acids are presented in Tables 1 and 2, respectively. Medialipid® and Lipidem® were obtained from B. Braun (Boulogne Billancourt, France), Intralipid® and SMOFlipid® from Fresenius-Kabi (Sèvres, France), and ClinOleic® from Baxter (Maurepas, France). All reagents were obtained from Sigma-Aldrich (Saint-Quentin Fallavier, France), except U46619 (9,11-dideoxy-9α-methanoepoxy prostaglandin F2α) from Cayman Chemical (Ann Arbor, MI, USA), apamin (APA) and charybdotoxin (CTX) from Latoxan (Valence, France), and the SOD mimetic MnTMPyP from Enzo Life Sciences (Lausen, Switzerland).
Vascular Reactivity Studies
Vascular reactivity studies were performed using porcine coronary artery rings as previously described [18, 19]. Pig hearts were collected from the local slaughterhouse (COPVIAL, Holtzheim, France). Briefly, the left circumflex coronary arteries were excised, carefully cleaned of connective tissue in Krebs bicarbonate solution and cut into rings (3–4 mm length). In some preparations, the endothelium was mechanically removed by rubbing the intimal surface of rings with a pair of forceps. Rings with or without endothelium were suspended in organ chambers containing oxygenated (95% O2; 5% CO2) Krebs bicarbonate solution (mM: NaCl 119, KCl 4.7, KH2PO4 1.18, MgSO4 1.18, CaCl2 1.25, NaHCO3 25, and d-glucose 11, pH 7.4, 37 °C) for the determination of changes in isometric tension. The coronary artery rings were stretched to 5 g of tension and then allowed to equilibrate for 60 min. After the equilibration period, the rings were exposed to a Krebs bicarbonate solution containing a high concentration of potassium (80 mM) until reproducible contractile responses were obtained. After a 30 min washout period, the rings were contracted with the thromboxane mimetic U46619 (1–60 nM) to about 80% of the maximal contraction before addition of bradykinin (BK, 0.3 µM) to check the presence of a functional endothelium. After washout and a 30 min equilibration period, the rings were again contracted with U46619 to a plateau level before the construction of concentration-relaxation response curve to either BK or the NO donor sodium nitroprusside (SNP). The endothelium-dependent relaxation was determined in response to BK (0.1 nM to 1 µM) and the endothelium-independent relaxation in response to SNP (0.1 nM to 1 µM).
To assess the effect of lipid emulsions on the endothelial function, coronary artery rings were incubated for 30 min either with Intralipid®, Medialipid®, Lipidem® ClinOleic® , or SMOFlipid® diluted in Krebs solution to a final concentration of 0.5, 1 or 2% (v/v) before the addition of U46619 and the subsequent construction of a concentration-relaxation curve to bradykinin. Relaxations are expressed as a percentage of the sub-maximal contraction to U46619.
The bradykinin-induced endothelium-dependent relaxation in the porcine coronary artery is mediated by both NO and EDH responses [20, 21]. In some experiments, rings were incubated with Lipidem® in the presence of different pharmacological modulators for 30 min before contraction with U46619. The NO-mediated component of the relaxation was determined in the presence of the non-selective COX inhibitor indomethacin (10 µM) and the Ca2+-dependent K+ channels inhibitors charybdotoxin (CTX, 100 nM) plus apamin (APA, 100 nM) to inhibit the formation of prostanoids and the endothelium-derived hyperpolarization (EDH)-mediated response, respectively. The EDH-mediated component of the relaxation was determined in the presence of indomethacin (10 µM) and the non-selective NO synthase inhibitor NG-nitro-l-arginine (L-NA, 300 µM) to avoid the participation of vasoactive prostanoids and NO, respectively.
To examine the role of oxidative stress in the vascular dysfunction, rings were incubated for 30 min with a ROS modulator, such as N-acetylcysteine (NAC, 100 µM), MnTMPyP (membrane permeant superoxide dismutase mimetic, 100 µM), superoxide dismutase (SOD, 500 U/mL), polyethyleneglycol-catalase (PEG-catalase, membrane permeant catalase, 500 U/mL), catalase (500 U/mL), the copper chelators neocuproine (10 µM), bathocuproine (10 µM), and tetrathiomolybdate (TTM, 10 µM), the iron chelator deferoxamine (50 µM) and the zinc chelator l-histidine (50 µM), in combination with a lipid emulsion.
Electron Paramagnetic Resonance (EPR)
Porcine coronary artery rings were incubated in Krebs-Hepes solution with a lipid emulsion 1% v/v for 30 min. To measure superoxide anions (O2 .-) production, rings were allowed to equilibrate in deferoxamine-chelated Krebs-Hepes solution containing 1 hydroxy-3 methoxycarbonyl 2,2,5,5-tetramethylpyrrolidin (CMH, Noxygen, Germany; 500 mM), deferoxamine (25 mM), and DETC (5 mM) under constant temperature (37 °C) for 1 h. The reaction was stopped by freezing the samples in liquid nitrogen, and then samples were analyzed by EPR spectroscopy. Superoxide anions cannot be directly measured by ESR due to their short half-life. Therefore, the CMH spin-trapping reagent has been used. It reacts with O2 .- to generate the stable CMN radical, which gives a characteristic triplet signal ESR spectra, with an amplitude directly proportional to the quantity of CMN present in the sample. The quantification of the signal is based on the mean of the height (amplitude) of the three signals. Values are expressed in signal amplitude (amplitude, arbitrary units) and expressed as arbitrary units per milligram weight of dried tissue (A/Wd).
Statistical Analysis
All values are expressed as the mean ± SEM of n different experiments. Statistical analysis was performed using one-way and two-way analysis of variance test (ANOVA), followed by Bonferroni’s post hoc test as appropriate using GraphPad Prism software (version 5.04 for Windows, GraphPad software, Inc., San Diego, CA, USA). A P value < 0.05 was considered to be statistically significant.
Results
Lipid Emulsions Affect Endothelial Relaxation
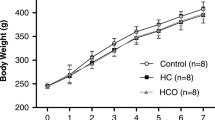
The bradykinin-induced relaxations in coronary artery rings with endothelium were significantly reduced in rings pre-incubated with either Lipidem®, Medialipid®, or SMOFlipid® and only minimally affected in those incubated with Intralipid® or ClinOleic® (Fig. 1). The relaxation induced by 30 nM of bradykinin was 90.7 ± 3.1 and 54.5 ± 6.6% in the control rings and the Lipidem® 1%-treated rings, respectively (P < 0.05; Fig. 1a).
Effect of lipid emulsions on the vascular reactivity to bradykinin (a, c) and sodium nitroprusside (b) in porcine coronary artery rings with or without endothelium. Coronary artery rings were incubated with either Intralipid®, Medialipid®, ClinOleic®, Lipidem®, or SMOFlipid® for 30 min before contraction with U46619, an analogue of thromboxane A2, and subsequent relaxation to bradykinin (BK) or sodium nitroprusside (SNP). Effect of 1% Lipidem® on the concentration-contraction curve to serotonin (5-HT) (d) and to U46619 (e) in endothelium-intact and -denuded coronary artery rings. Rings were exposed to 1% Lipidem® for 30 min before the construction of a concentration-contraction curve. Results are shown as mean ± SEM of 7–9 different experiments. *P < 0.05 versus control rings
In contrast, the different lipid emulsions affected minimally the SNP-induced concentration-dependent relaxation curve in rings without endothelium (Fig. 1b). Amongst the lipid emulsions, Lipidem® induced the most pronounced impairment of the bradykinin-induced relaxation at 1%, therefore all further experiments were performed with Lipidem®. Both 1 and 2%, but not 0.5% of Lipidem® significantly reduced the bradykinin-induced relaxation (Fig. 1c). In contrast, 1% Lipidem® did not significantly affect the serotonin (5-HT)-induced contraction in rings either with or without endothelium (Fig. 1d). The effect of 1% Lipidem® on U46619-induced contractions in both intact and endothelium denuded coronary artery rings is shown in Fig. 1e. Lipidem® did not affect contractions to U46619 up to 10 nM and increased slightly but significantly those to higher concentrations in rings with endothelium (Fig. 1e). In contrast, Lipidem® did not affect contractions to U46619 in rings without endothelium (Fig. 1e).
Lipid Emulsions Affect Both the NO and the EDH Component of the Endothelium-Dependent Relaxation
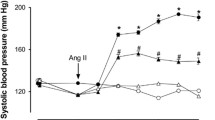
Incubation of coronary artery rings with endothelium with 1% Lipidem® for 30 min significantly reduced the bradykinin-induced endothelium-dependent relaxations, affecting both the NO-mediated component, assessed in the presence of the combination of indomethacin plus CTX and APA (65.4 ± 9.0 vs. 93.2 ± 2.2% in Lipidem®-treated rings and control rings, respectively; Fig. 2a), and the EDH-mediated component assessed in the presence of indomethacin plus L-NA (38.7 ± 8.2 vs. 87.1 ± 2.6% in Lipidem®-treated rings and control rings, respectively; Fig. 2b). In the presence of the COX inhibitor indomethacin, relaxations to bradykinin were significantly improved in rings incubated with 1% Lipidem® (Fig. 2c).
Characterization of the Lipidem®-induced endothelial dysfunction in coronary artery rings. Coronary artery rings with endothelium were incubated with Lipidem® 1% (v/v) for 30 min before the addition of U46619. NO-mediated relaxations were determined in the presence of indomethacin (10 µM) and charybdotoxin plus apamin (both at 100 nM) to avoid the participation of vasoactive prostanoids and EDH, respectively (a). EDH-mediated relaxations were assessed in the presence of indomethacin (10 µM) and NG-nitro-l-arginine (300 µM) to rule out the formation of vasoactive prostanoids and NO, respectively (b). The role of cyclooxygenase-derived vasoactive prostanoids was determined in the presence of indomethacin (10 µM) (c). Results are shown as mean ± SEM of 5–7 different experiments. *P < 0.05 versus control, # P < 0.05 versus Lipidem® 1%
Role of Oxidative Stress in the Lipidem®-Induced Endothelial Dysfunction
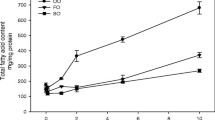
Since lipid emulsions such as Lipofundin (MCT/LCT®) have been shown to increase the vascular formation of ROS [19], the contribution of oxidative stress in the endothelial dysfunction induced by Lipidem® was evaluated. Therefore, the bradykinin response was assessed in the presence of different antioxidants or metal chelators. The Lipidem®-induced endothelial dysfunction was markedly improved in the presence either of NAC, SOD, MnTMPyP, catalase, or PEG-catalase (Fig. 3). It was also significantly improved in the presence of the membrane-permeable copper chelators neocuproine, bathocuproine, and tetrathiomolybdate, the membrane-permeable iron chelator deferoxamine, and the zinc chelator l-histidine (Fig. 4). In addition, the possibility that lipid emulsions affect the vascular level of oxidative stress and in particular superoxide anions was assessed using electron paramagnetic resonance. The lipid emulsions, Lipidem® and Medialipid® increased the formation of superoxide anions in intact coronary arteries, whereas no such effect was observed with Intralipid®, SMOFLipid® , and ClinOleic® (Fig. 5).
Role of oxidative stress in the endothelial dysfunction induced by Lipidem®. Coronary artery rings with endothelium were incubated with Lipidem® and an antioxidant N-acetylcysteine (NAC, 100 µM; a), native superoxide dismutase (SOD, 500 U/mL or a membrane-permeant SOD mimetic MnTMPyP, 100 µM; b), native catalase (CAT, 500 U/mL or a membrane-permeant catalase PEG-CAT, 500 U/mL; c) for 30 min before addition of U46619. The results are expressed as mean ± SEM of 5–7 different experiments. # P < 0.05 versus Lipidem® 1%
Role of transition metals in the endothelial dysfunction induced by Lipidem®. Coronary artery rings with endothelium were incubated with Lipidem® and either with the copper chelating agents: neocuproine (10 µM), bathocuproine (10 µM), or tetrathiomolybdate (TTM, 10 µM; a), the zinc chelator l-histidine (50 µM), or the iron chelator deferoxamine (50 µM; b) for 30 min before addition of U46619. The results are expressed as mean ± SEM of 7–9 different experiments. *P < 0.05 versus Lipidem® 1%
Discussion
The present study has investigated the effect of different lipid emulsion formulations on both the vascular and the endothelial function. Both the MCT and LCT-containing lipid emulsions such as Lipidem®, Medialipid®, and SMOFlipid® significantly blunted the bradykinin-induced endothelium-dependent relaxation in coronary artery rings. In contrast, lipid emulsions containing either only LCT from soybean (Intralipid®) or a mixture of LCT from soybean and olive oil (ClinOleic®) affected minimally relaxations to bradykinin. Moreover, since the lipid emulsions affecting the endothelial function did not affect the relaxation to the NO donor sodium nitroprusside, they predominantly target the endothelial function rather than that of the vascular smooth muscle. Lipidem® was selected for further characterization of the endothelial dysfunction since this lipid emulsion induced the greatest impairment of the endothelial function compared to the other four. These experiments have characterized the mechanism underlying the Lipidem®-induced blunted endothelial relaxation, and determined the role of oxidative stress using various pharmacological tools, and electron paramagnetic resonance.
The present findings indicate that the Lipidem®-induced endothelial dysfunction affected both the NO and the EDH components of the relaxation, and that the EDH component is affected to a greater extent than the NO component in coronary artery rings. In addition, Lipidem® increased the contractile response to U46619 to some extent but not that to 5-HT. Such a difference might be due to the involvement of different signal transduction mechanisms in response to the activation of thromboxane prostanoid receptors and 5-HT receptors.
The fact that indomethacin improved endothelium-dependent relaxations to bradykinin in Lipidem®-treated coronary artery rings suggests the involvement of vasoconstrictor prostanoids. The COX pathway has been shown to play an important role in modulating the endothelial function under both physiological and pathological conditions [24]. The COX-1 isoform is constitutively expressed in human endothelial cells, whereas endothelial COX-2 is induced mainly during the inflammatory response [25]. COX catalyzes the synthesis of prostaglandin H2 (PGH2), which is the precursor of both vasorelaxant prostanoids, such as prostacyclin (PGI2), and vasoconstrictor prostanoids, such as thromboxane A2 (TXA2) [26]. A high content of n-6 PUFAs, such as linoleic acid, in lipid emulsions has been related to a major production of pro-inflammatory mediators derived from arachidonic acid, including prostaglandin F2 alpha (PGF2 alpha) and TXA2 through the COX pathway [27], and leukotrienes through the lipo-oxygenase pathway [28, 29], resulting in an increased risk of lipid peroxidation, endothelial dysfunction and related vascular injury [7, 30–32]. In the present study, an increased availability of arachidonic acid might have stimulated the COX-dependent production of vasoconstrictors PGH2 and TXA2, and hence, to increase vascular tone. Linoleic acid is the most abundant fatty acid present both in Lipidem® and Medialipid®, supporting the view that Lipidem® might induce endothelial dysfunction by activating arachidonic acid metabolism through a COX-dependent pathway. These findings are in good agreement with previous ones indicating that COX inhibition protected the endothelium-dependent vasodilatation against elevated circulating fatty acid levels in humans [33], and also improved the endothelium-dependent relaxation of microvessels in a hypercholesterolemic porcine model of chronic ischemia [34].
Previous studies have reported that lipid emulsions are able to increase the level of circulating triacylglycerols and the vascular formation of ROS promoting endothelial dysfunction [35–38]. Consistent with these previous studies, the antioxidant vitamin C partly restored the blunted acetylcholine-induced relaxation induced by free fatty acids, and triacylglycerol attenuated NO formation associated with oxidative stress [39, 40]. The present findings indicate that Lipidem® and Medialipid® (1%) increased ROS production, whereas SMOFLipid®, Intralipid®, and ClinOleic® had little effect. In addition, different antioxidants (N-acetylcysteine, superoxide dismutase and catalase) improved the Lipidem®-induced endothelial dysfunction indicating the involvement of both superoxide anions and hydrogen peroxide. Since an improved relaxation was also observed in the presence of a chelator either of copper, zinc, or iron, transition metals may possibly contribute to the formation of ROS through the Fenton Haber–Weiss reaction [41]. However, their source remains to be clarified and might include besides the cellular pools possibly also the low level in the physiological salt solution and/or the lipid emulsion. The l-arginine-NO pathway is well-known to be influenced by oxidative stress since superoxide anions can react with NO to form the free radical peroxynitrite [42]. An impaired endothelial function might contribute to explain the transiently increased mean aortic blood pressure and systemic vascular resistance in conscious dogs following parenteral administration of Medialipid®, but not Intralipid®, [43]. Medialipid® also enhanced the pro-inflammatory and oxidative/nitrosative markers including COX-2, NO, O2 .-, and pIkB in the aorta and heart associated with an exacerbation of the peritonitis-induced vascular dysfunction in a rat model of septic shock [44]. Similarly, Lipofundin® containing LCT/MCT and Intralipid® inhibited acetylcholine-induced NO-mediated relaxations in the rat aorta [45]. Altogether, these findings suggest that although the American Society of Parenteral and Enteral Nutrition identified MCT containing oils as a potentially beneficial additive to lipid emulsions [46], further studies are required to better assess the effect of MCT, LCT, and a mixture of LCT/MCT on the pivotal protective effect on the endothelium on the vascular system. The different effect of lipid emulsions on the endothelial function in the present study might be due to differences in fatty acid composition such as an increased content of medium-chain fatty acids and a reduced content of long-chain fatty acids.
In conclusion, the present findings indicate that lipid emulsions containing medium chain triacylglycerols including Lipidem® and Medialipid® significantly blunt the bradykinin-induced endothelium-dependent relaxation in porcine coronary artery rings, and that this effect is due, at least in part, to an increased vascular level of oxidative stress, which promotes endothelial dysfunction by decreasing both the NO and the EDH components.
Abbreviations
- DHA:
-
Docosahexaenoic acid (22:6n-3)
- EDH:
-
Endothelium-dependent hyperpolarization
- EPA:
-
Eicosapentaenoic acid (20:5n-3)
- KCN:
-
Potassium cyanide
- LCT:
-
Long chain triacylglycerols
- MCT:
-
Medium chain triacylglycerols
- MnTMPyP:
-
Mn(III) Tetrakis(1-methyl-4 pyridyl) porphyrin
- NAC:
-
N-acetylcysteine
- NO:
-
Nitric oxide
- PUFA:
-
Polyunsaturated fatty acid
- ROS:
-
Reactive oxygen species
- VAS-2870:
-
3-Benzyl-7-(2-benzoxazolyl) thio-1,2,3-triazolo (4,5-d) pyrimidine
References
Chan S, McCowen KC, Bistrian B (1998) Medium-chain triglyceride and n-3 polyunsaturated fatty acid-containing emulsions in intravenous nutrition. Curr Opin Clin Nutr Metab Care 1:163–169
Ziegler TR (2009) Parenteral nutrition in the critically ill patient. N Engl J Med 361:1088–1097
Boisramé-Helms J, Toti F, Hasselmann M, Meziani F (2015) Lipid emulsions for parenteral nutrition in critical illness. Prog Lip Res 60:1–16
Tilley SL, Coffman TM, Koller BH (2001) Mixed messages: modulation of inflammation and immune responses by prostaglandins and thromboxanes. J Clin Invest 108:15–23
Markowitz S, Neal JM (2009) Immediate lipid emulsion therapy in the successful treatment of bupivacaine systemic toxicity. Reg Anesth Pain Med 34:276
Steinberg HO, Tarshoby M, Monestel R, Hook G, Cronin J, Johnson A, Bayazeed B, Baron AD (1997) Elevated circulating free fatty acid levels impair endothelium-dependent vasodilation. J Clin Invest 100:1230–1239
Gosmanov AR, Smiley DD, Peng L, Siquiera J, Robalino G, Newton C, Umpierrez GE (2012) Vascular effects of intravenous intralipid and dextrose infusions in obese subjects. Metab Clin Exp 61:1370–1376
De Kreutzenberg SV, Crepaldi C, Marchetto S, Calo L, Tiengo A, Del Prato S, Avogaro A (2000) Plasma free fatty acids and endothelium-dependent vasodilation: effect of chain-length and cyclooxygenase inhibition. J Clin Endocrinol Metab 85:793–798
Steer P, Basu S, Lithell H, Vessby B, Berne C, Lind L (2003) Acute elevations of medium- and long-chain fatty acid have different impacts on endothelium-dependent vasodilation in humans. Lipids 38:15–19
Edirisinghe I, McCormick Hallam K, Kappagoda CT (2006) Effect of fatty acids on endothelium-dependent relaxation in the rabbit aorta. Clin Sci 111:145–151
Carpentier YA, Simoens C, Siderova V, el Nakadi I, Vanweyenberg V, Eggerickx D, Deckelbaum RJ (1997) Recent developments in lipid emulsions: relevance to intensive care. Clin Nutr 13:73S–78S
Waitzberg DL, Torrinhas RS, Jacintho TM (2006) New parenteral lipid emulsions for clinical use. J Parenter Enteral Nutr 30:351–367
Liang B, Wang S, Ye YJ, Yang XD, Wang YL, Qu J, Xie QW, Yin MJ (2008) Impact of postoperative omega-3 fatty acid-supplemented parenteral nutrition on clinical outcomes and immunomodulations in colorectal cancer patients. World J Gastroenterol 14:2434–2439
Calder PC (2009) Hot topics in parenteral nutrition. Rationale for using new lipid emulsions in parenteral nutrition and a review of the trials performed in adults. Proc Nutr Soc 68:252–260
Mayer K, Grimm H, Grimminger F, Seeger W (2002) Parenteral nutrition with n-3 lipids in sepsis. Br J Nutr 87:S69–S75
Zgheel F, Alhosin M, Rashid S, Burban M, Auger C, Schini-Kerth VB (2014) Redox-sensitive induction of Src/PI3-kinase/Akt and MAPKs pathways activate eNOS in response to EPA:DHA 6:1. PLoS One 18:105102
Nakashima M, Mombouli JV, Taylor AA, Vanhoutte PM (1993) Endothelium-dependent hyperpolarization caused by bradykinin in human coronary arteries. J Clin Invest 92:2867–2871
Auger C, Kim J-H, Trinh S, Chataigneau T, Popken AM, Schini-Kerth VB (2011) Fruit juice-induced endothelium-dependent relaxations in isolated porcine coronary arteries: evaluation of different fruit juices and purees and optimization of a red fruit juice blend. Food Funct 2:245–250
Anselm E, Chataigneau M, Ndiaye M, Chataigneau T, Schini-Kerth VB (2007) Grape juice causes endothelium-dependent relaxation via a redox-sensitive Src- and Akt-dependent activation of eNOS. Cardiovasc Res 73:404–413
Rivilla F, Vallejo S, Peiro C, Sanchez-Ferrer CF (2012) Characterization of endothelium-dependent relaxations in the mesenteric vasculature: a comparative study with potential pathophysiological relevance. J Pediatr Surg 47:2044–2049
Heaps CL, Robles JC, Sarin V, Mattox ML, Parker JL (2014) Exercise training-induced adaptations in mediators of sustained endothelium-dependent coronary artery relaxation in a porcine model of ischemic heart disease. Microcirculation 21:388–400
Félétou M, Huang Y, Vanhoutte PM (2010) Vasoconstrictor prostanoids. Pflüg Arch-Eur. J Physiol 459:941–950
Feletou M, Huang Y, Vanhoutte PM (2011) Endothelium-mediated control of vascular tone: COX-1 and COX-2 products. Br J Pharmacol 164:894–912
Ricciotti E, FitzGerald GA (2011) Prostaglandins and inflammation. Arterioscler Thromb Vasc Biol 31:986–1000
Caughey GE, Cleland LG, Penglis PS, Gamble JR, James MJ (2001) Roles of cyclooxygenase (COX)-1 and COX-2 in prostanoid production by human endothelial cells: selective up-regulation of prostacyclin synthesis by COX-2. J Immunol 167:2831–2838
Morin C, Sirois M, Echave V, Rizcallah E, Rousseau E (2009) Relaxing effects of 17(18)-EpETE on arterial and airway smooth muscles in human lung. Am J Physiol Lung Cell Mol Physiol 296:L130–L139
Adkins Y, Kelley DS (2010) Mechanisms underlying the cardioprotective effects of omega-3 polyunsaturated fatty acids. J Nutr Biochem 21:781–792
de Kreutzenberg SV, Puato M, Kiwanuka E, Del Prato S, Pauletto P, Pasini L, Tiengo A, Avogaro A (2003) Elevated non-esterified fatty acids impair nitric oxide independent vasodilation, in humans: evidence for a role of inwardly rectifying potassium channels. Atherosclerosis 169:147–153
Krohn K, Koletzko B (2006) Parenteral lipid emulsions in paediatrics. Curr Opin Clin Nutr Metab Care 9:319–323
Umpierrez GE, Smiley D, Robalino G, Peng L, Kitabchi AE, Khan B, Le A, Quyyumi A, Brown V, Phillips LS (2009) Intravenous intralipid-induced blood pressure elevation and endothelial dysfunction in obese African-Americans with type 2 diabetes. J Clin Endocrinol Metab 94:609–614
Steer P, Millgard J, Basu S, Lithell H, Vessby B, Berne C, Lind L (2003) Vitamin C, diclophenac, and l-arginine protect endothelium-dependent vasodilation against elevated circulating fatty acid levels in humans. Atherosclerosis 168:65–72
Chu LM, Robich MP, Bianchi C, Feng J, Liu Y, Xu SH, Burgess T, Sellke FW (2012) Effects of cyclooxygenase inhibition on cardiovascular function in a hypercholesterolemic swine model of chronic ischemia. Am J Physiol Heart Circ Physiol 302:479–488
Inoguchi T, Li P, Umeda F, Yu HY, Kakimoto M, Imamura M, Aoki T, Etoh T, Hashimoto T, Naruse M, Sano H, Utsumi H, Nawata H (2000) High glucose level and free fatty acid stimulate reactive oxygen species production through protein kinase C–dependent activation of NAD(P)H oxidase in cultured vascular cells. Diabetes 49:1939–1945
Li JM, Shah AM (2004) Endothelial cell superoxide generation: regulation and relevance for cardiovascular pathophysiology. Am J Physiol Regul Integr Comp Physiol 287:R1014–R1030
Chinen I, Shimabukuro M, Yamakawa K, Higa N, Matsuzaki T, Noguchi K, Ueda S, Sakanashi M, Takasu N (2007) Vascular lipotoxicity: endothelial dysfunction via fatty-acid-induced reactive oxygen species overproduction in obese Zucker diabetic fatty rats. Endocrinology 148:160–165
Batchuluun B, Inoguchi T, Sonoda N, Sasaki S, Inoue T, Fujimura Y, Miura D, Takayanagi R (2014) Metformin and liraglutide ameliorate high glucose-induced oxidative stress via inhibition of PKC-NAD(P)H oxidase pathway in human aortic endothelial cells. Atherosclerosis 232:156–164
Osanai H, Okumura K, Hayakawa M, Harada M, Numaguchi Y, Mokuno S, Murase K, Matsui H, Toki Y, Ito T, Hayakawa T (2000) Ascorbic acid improves postischemic vasodilatation impaired by infusion of soybean oil into canine iliac artery. J Cardiovas Pharmacol 36:687–692
Ilan E, Tirosh O, Madar Z (2005) Triacylglycerol-mediated oxidative stress inhibits nitric oxide production in rat isolated hepatocytes. J Nutr 135:2090–2095
Gutteridge JM, Halliwell B (2010) Antioxidants: molecules, medicines, and myths. Biochem Biophys Res Commun 393:561–564
Beckman JS, Koppenol WH (1996) Nitric oxide, superoxide, and peroxynitrite: the good, the bad, and ugly. Am J Physiol 271:C1424–C1437
Van de Velde M, Wouters PF, Rolf N, Van Aken H, Vandermeersch E (1998) Comparative hemodynamic effects of three different parenterally administered lipid emulsions in conscious dogs. Crit Care Med 26:132–137
Boisrame-Helms J, Said A, Burban M, Delabranche X, Stiel L, Zobairi F, Hasselmann M, Schini-Kerth V, Toti F, Meziani F (2014) Medium-chain triglyceride supplementation exacerbates peritonitis-induced septic shock in rats: role on cell membrane remodeling. Shock 42:548–553
Ok SH, Lee SH, Yu J, Park J, Shin IW, Lee Y, Cho H, Choi MJ, Baik J, Hong JM, Han JY, Lee HK, Chung YK, Sohn JT (2015) Lipid emulsion attenuates acetylcholine-induced relaxation in isolated rat aorta. Bio Med Res Int 2015:871545
Vanek VW, Seidner DL, Allen P, Bistrian B, Collier S, Gura K, Miles JM, Valentine CJ, Kochevar M (2012) Clinical role for alternative intravenous fat emulsions. Nutrition in clinical practice. Am Soc Parenter Enteral Nutr 27:150–192
Leaf A, Weber PC (1988) Cardiovascular effects of n-3 fatty acids. N Engl J Med 318:549–557
Granato D, Blum S, Rössle C, Le Boucher J, Malnoë A, Dutot G (2000) Effects of parenteral lipid emulsions with different fatty acid composition on immune cell functions in vitro. J Parenter Enteral Nutr 24:113–118
Wanten GJ, Calder PC (2007) Immune modulation by parenteral lipid emulsions. Am J Clin Nutr 85:1171–1184
Grimm H, Mertes N, Goeters C, Schlotzer E, Mayer K, Grimminger F, Fürst P (2006) Improved fatty acid and leukotriene pattern with a novel lipid emulsion in surgical patients. Eur J Nutr 45:55–60
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
About this article
Cite this article
Amissi, S., Boisramé-Helms, J., Burban, M. et al. Lipid Emulsions Containing Medium Chain Triacylglycerols Blunt Bradykinin-Induced Endothelium-Dependent Relaxation in Porcine Coronary Artery Rings. Lipids 52, 235–243 (2017). https://doi.org/10.1007/s11745-016-4225-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11745-016-4225-y