Abstract
The effect of hypercholesterolemia induced immune response and inflammation on progression of atherosclerosis in ApoB tm25gy LDLr tm1Her mice, expressing only ApoB100 and deficient in the low density lipoprotein (LDL) receptor, thus closely resembling human cholesterol transport is not well defined. Atherosclerosis was induced by a high cholesterol diet and its progression was studied at 8, 14 and 20 weeks. Antibody response was determined by ELISA. Lymphocytes in spleen and aortic expression of inflammatory markers were studied by flow cytometry, and immunohistochemistry respectively. A rapid increase in plasma LDL levels in the first 8 weeks was followed by the exponential development of atherosclerosis between 8 and 14 weeks. Progression of the disease was accompanied by an accumulation of macrophages and increased expression of IL17 and IFN-γ in the aorta. Hypercholesterolemia resulted in increased immune response to modified lipids and aortic inflammation, with an expansion of Th17 cells in the spleen. Progression of atherosclerosis showed a positive correlation (r = 0.84, P < 0.001) with Th17 cells and a negative correlation with Treg cells (r = 0.83, P < 0.001). IgM antibodies to Ox-LDL and Th17 cells in spleen showed greatest association with disease development. Our results suggest that anti Ox-LDL IgM antibodies, Th17 cells could be developed as a potential marker to study disease progression and to study the effect of therapeutic regulation of inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atherosclerosis is a complex chronic inflammatory disease of the large and medium sized arteries. Apart from lipid accumulation, inflammation and immune response play a major role in the initiation and progression of the disease [1, 2]. Despite the widespread occurrence of the disease, our understanding of chronological changes in cellular and biochemical components of lesions is still incomplete, primarily due to the slow progression and complex pathophysiology of the disease, confounded by the unavailability of plaque material from human samples for systematic studies [3].
Animal models have provided valuable information on the sequential events and the mechanisms responsible for initiation and maturation of atherosclerotic lesions [3–6]. Apolipoprotein E deficient (ApoE−/−) and LDL receptor deficient (LDL-R−/−) mice are two hypercholesterolemic models used extensively in atherosclerosis research [7, 8]. The uptake of VLDL, LDL, and chylomicrons is disrupted in ApoE−/− deficient mice resulting in greater proportion of these cholesterol in the plasma and development of spontaneous atherosclerosis even in normal diet [9]. Inactivation of LDL-R results in moderate elevation of plasma cholesterol levels and mild atherosclerosis in mice [10, 11]. In contrast, individuals with familial hypercholesterolemia, caused by mutations in the LDL-R gene have 2–6 times higher LDL levels in plasma and higher predisposition for coronary artery disease [12]. This difference is due to the presence of two forms of Apolipoprotein B (ApoB100 and ApoB48) in mice while only ApoB100 is present in humans. Mice deficient in ApoB mRNA editing synthesize exclusively ApoB100 and have markedly elevated LDL cholesterol in the absence of LDL-R. These mice develop widespread atherosclerosis and are reported to mimic human atherosclerosis more closely than other models [13, 14]. While ApoE−/− and LDL-R−/− mice have been extensively studied with regard to lipoprotein metabolism and development of atherosclerosis, its progression over time and its relation to adaptive immunity remains to be defined in ApoB tm2Sgy/Ldlr tm1Her/J mice [15, 16]. Moreover, the hypercholesterolemia induced immune response was found to be intrinsically different in ApoE−/− and LDL-R−/− mice, reiterating the importance of investigating the role of hypercholesterolemia in disease progression in this animal model [17].
Arterial inflammation mediated by immune response to self antigens like modified lipids and heat shock proteins is known to initiate the development of atherosclerosis [18]. Activated helper T cells secreting interferon-γ are abundantly present in mouse and human lesions while the role of Th2 and Th17 still remains controversial [18–21]. Other effector cells of the immune system. like the B lymphocytes, monocytes mast cells also contribute to the development of the lesion [22]. In contrast regulatory T cells have been shown to have an atheroprotective effect [23]. A better understanding of the influence of hypercholesterolemia on the immune system and the progression of atherosclerosis could provide novel insights into the spectrum of the disease and its mechanism in mice. In addition, we also wanted to determine if changes in peripheral immune markers could be correlated to disease progression. In this study we studied the correlation of aortic lesions with the peripheral immune response to oxidized lipoprotein and lymphocyte population in the spleen and expression of inflammatory markers in the lesion.
Methods
Animals
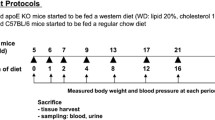
Mice with C57BL/6 background and deficient in LDL-R and ApoB48 (Apobtm25gy LDLr tm1Her) were used for the experiment (Jackson Laboratory, USA). This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA), Ministry of Environment, Government of India and confirms to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication, 8th Edition, 2011). The protocol was approved by the Institutional Animal Ethics Committee of the Thrombosis Research Institute (Registration Number: 1261/c/09/CPCSEA).
Induction of Atherosclerosis in Apob tm25gy LDLr tm1Her Mice
Apob tm2Sgy/Ldlr tm1Her/J mice were kept under standard laboratory conditions and fed a normal chow diet (Nutrilab, India) or a high-fat diet (Harlan, TD 96121 Indianapolis, USA). Food and water were administered ad libitum. Atherosclerosis was induced in 40 (20 M and 20 F) experimental animals (5–6 weeks old) by feeding diet rich in fat (21 % anhydrous milk fat and 1.25 % cholesterol). At each time point 8–10 mice were sacrificed humanely using an overdose of isoflurane inhalant anesthetic (15 %) as per American Veterinary Medical Association guidelines [24]. The mouse was exsanguinated using a 23 gauge needle through the apex of the ventricle. The spleen was collected under sterile conditions in Hanks' balanced salt solution (HBSS). The heart was dissected out and collected in either optimal cutting temperature (OCT) medium (Tissue Tek, Leica, Germany) and neutral buffered phenol (NBF). Using microdissection scissors, fat around the ascending aorta was removed. The aortic arch was carefully dissected and collected in RNAlater and frozen at −80 °C for RNA extraction. Aortic root Sections (10 μm) were cut from the hearts embedded in an OCT medium under frozen conditions using a cryotome (Leica CM 1900 UV Cryotome) and from NBF after embedding in paraffin blocks. Samples were collected after 0.8, 14 and 20 weeks. Cells were isolated from the spleen by passing through a sterile cell strainer, washed twice with HBSS and stored in liquid nitrogen at a concentration of 1 × 107 cells/mL.
Atherosclerotic Lesion Assessment and Immunohistochemical Analysis
Quantification of atherosclerotic lesions was carried out as per the protocol approved by the Animal Models of Diabetic Complications Consortium (http://www.diacomp.org) and as previously described by Daugherty et al. [25]. For lesion analysis in each mouse, five Sections 80 μm apart were stained with Elastica van Geison (EVG) and Oil Red O (ORO) to quantify the percentage of lesion area and lipid in the aortic sinus. Plaque necrosis was quantified by measuring the size of the hematoxylin and eosin-negative acellular area, as described previously [26]. Total area and area covered with Lesion were calculated using Image-Pro Plus software (Media Cybernetics, Bethesda, MD, USA). Fluorescent labeled antibodies were used to quantify specific antigens and cytokines in the aortic sinus. Frozen sections were permeabilized using 0.2 % of triton ×100 for 30 min, fixed with ice-cold acetone, blocked with 5 % serum and incubated with primary antibodies followed by appropriate secondary antibody and were mounted with Vectashield. Images were captured using a Leica DMI 4000 B Confocal microscope and the analysis was done using Image-Pro plus software (Media Cybernetics, Bethesda, USA). Antibody staining including CD4 for T cells CD68 for macrophages and tumor necrosis factor α (TNF-α) for inflammatory marker were carried out in frozen aortic sinus sections as described earlier [27].
Cytokine Quantification in the Aorta by Real-Time PCR Analysis
Quantitative RT-PCR was carried out for different groups of genes that are involved with inflammation and immune regulation. Total RNA was extracted from the ascending part of the mice aorta using TRIzol® Reagent (Invitrogen, Carlsbad, USA). RT-PCR was performed with two-step Express SYBR superscript RT-PCR kit (Invitrogen, Carlsbad, California, USA) using the ABI PRISM 7500 sequence detection system (Applied Biosystems, 7500 real time PCR system) according to the manufacturers protocol and the amplification was carried out at 95 °C for 5 min, 95 °C for 45 s, and 60 °C for 1 min for each step for 40 cycles in triplicate. Gene levels were normalized to that of glyceraldehyde3-phosphate dehydrogenase (GAPDH). The sequence of primers used are given below:
- TGF-β1-F:
-
TTGCTTCAGCTCCACAGAGA
- TGF-β1-R:
-
TGGTTGTAGAGGGCAAGGAC
- IFN-γ-F:
-
ATGAACGCTACACACTGCATC
- IFN-γ-R:
-
CCATCCTTTTGCCAGTTCCTC
- IL17- F:
-
TTTAACTCCCTTGGCGCAAAA
- IL17-R:
-
CTTTCCCTCCGCATTGACAC
- IL10-F:
-
GTGGCAGTGAAGACCATGAAGTTG
- IL10-R:
-
GAACTCCGGGATAGGGAGTCAT
- GAPDH-F:
-
AACTTTGGCATTGTGGAAGG
- GAPDH-R:
-
ACACATTGGGGGTAGGAACA
Flow Cytometry
Cells from the spleen of mice were isolated after different time periods. For intracellular cytokine staining, cells were activated for 4 h with phorbol myristate acetate (PMA-10 ng/mL) and ionomycin (1 µg/mL) in the presence of protein transport inhibitor brefeldin (100 ng/mL).Flow cytometry analyses were performed by FACS Canto II using FACS DIVA software (Becton–Dickinson, New Jersey, USA) and FLOWJO software (Tree star Ltd, Oregon, USA). The antibodies used were as follows: Fluorescein isothiocyanate (FITC)-conjugated CD4 (clone RM4-5), allophycocyanin (APC)-anti CD25 (clone PC61.5), phycoerythrin (PE)-anti-fork head box p3 (Foxp3) (clone NRRF-30), PE- IFN-γ (clone XMG1.2) all from e-Biosciences San Diego, CA, USA. APC-Cy™ 7 IL-17A (clone TC11-18H10, BD pharmingen, San Jose, USA) and isotype-matched control antibodies. Intracellular staining for cytokines and Foxp3 was performed using the intracellular staining kit (eBiosciences San Diego, CA, USA) according to the manufacturer’s instructions. Surface staining was performed according to standard procedures at a density of 1 × 105 cells/100 µL, and volumes scaled up accordingly.
Cell Proliferation Assays
Cell culture experiments were performed in Rosewell Park Memorial Institute (RPMI) 1640 medium (Bio Whittaker, Walkersville, MD, USA) supplemented with 10 % fetal bovine serum, 2 mM glutamine, 10 mM HEPES (4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid), sodium pyruvate, and antibiotics. Cells from individual spleens were passed through a sterile cell strainer (100 µm, SPL Life sciences, Gyeonggi-do, Korea), red blood cells were lysed with ammonium chloride, washed twice in HBSS and plated in 96-well culture dishes at a concentration of 5 × 105 cells/mL in RPMI medium. Cells were stimulated with 10 µg/mL of native or copper oxidized LDL or concanavalin A (ConA; Merck, New Jersey, USA). The cell proliferation assay was carried out on spleen cells of mice at different time points by using Roche cell proliferation BrdU assay kit by strictly following the manufacturers’ guidelines. This technique is based on the incorporation of pyrimidine analogue BrdU instead of thymidine into the DNA of proliferating cells. Cultured spleen cells were labeled with 10 µl BrdU reagent for the last 18 h of culture. The cells were fixed, and the DNA was denatured by adding fixing and denaturation solution. (FixDenat), followed by anti-BrdU-POD antibody which binds to the BrdU incorporated into the newly synthesized cellular DNA. The immune complexes are detected by the subsequent substrate reaction using tetra methyl benzidine and absorbance was recorded by an ELISA reader.
Lipid Profile
Blood was collected from the retro orbital venous plexus under 3 % isoflurane inhalant anesthesia in oxygen as per American Veterinary Medical Association guidelines. Lipid profile of plasma triglycerides, total cholesterol and low density lipoprotein was carried out by using Siemens Dimension® Xpand® plus following the manufacturer’s instructions. Plasma was diluted 10 times to get the lipid values within the range. Final concentration in plasma was calculated by taking the dilution factor into account.
ELISA Protocol
Antigen specific ELISA was carried out for native LDL and Ox-LDL on plasma samples at different stages of disease development. LDL (Sigma chemicals, St. Louis, USA) was oxidized overnight with CuSO4 (5 µM), as described earlier [28] and plates were coated with 10 µg/mL Cu-oxidized LDL or native LDL as capture antigen. Sera were diluted 1:100, incubated on coated plates for 2 h at 4 °C, washed, and detected with horseradish peroxidase (HRP)-labeled anti-mouse IgG or IgM (Sigma chemicals, St. Louis, USA) as secondary antibodies [29].
Statistical Analysis
Graph Pad PRISM for Windows version 5.01 (GraphPad software inc. 2007) was used for statistical analysis. Data are expressed as means ± SEM. Non-parametric Spearman correlation analysis was used to test correlation between lipid levels in plasma, lesion area and immune response. Continuous data were log transformed for analysis. Nonparametric ANOVA and the Kruskal–Wallis test were used for the comparison of multiple groups and the Mann–Whitney test was used for comparison of continuous data between two groups. A P value <0.05 was considered significant.
Results
Plaque Progression in Apob tm2Sgy Ldlr tm1Her/J Mice
Progression of atherosclerosis was studied at 8, 14 and 20 weeks. The percentage of lesion covering the aortic sinus was 16.7 ± 2.8 after 8 weeks, which increased to 50.5 ± 5.3 by 14 weeks and 58.9 ± 1.5 by 20 weeks. The atherosclerotic lesion developed slowly in the first 8 weeks but progressed exponentially between 8 and 14 weeks, beyond which the progression slowed down. The increase in aortic lesion was significant between 8 and 14 weeks (P = 0.004) and between 8 and 20 weeks (P = 0.009) but not between 14 and 20 weeks (Fig. 1a, b). Plaque morphology showed changes at 14 and 20 weeks with the appearance of necrotic area (Fig. 1c). Lipid accumulation in the plaque continued to increase significantly with plaque progression. At 8 weeks 8.8 ± 2.3 % of the plaque showed positive staining for lipids (ORO), which increased to 21.7 ± 1.4 %, P = 0.03 and 39.5 ± 6.8 %, P = 0.015 at week 14 and 20, respectively (Fig. 1d, e).
Plaque Progression in Apob tm2Sgy Ldlr tm1Her/J Mice. a Representative photomicrographs of EVG stained plaque area aortic sinus of 0, 8 14 and 20 weeks old ApoB tm25gy LDLrtm1Her mice. Scale bar represents 200 µm. b Quantitative analysis of percentage plaque area in total surface area of the aortic sinus (n = 6 animals per group). c Quantitative analysis of necrotic acellular area in the total surface area of the aortic sinus (n = 6 animals per group). d Representative photomicrographs of oil red O (ORO) stained plaque area aortic sinus of 0, 8 14 and 20 weeks old ApoB tm25gy LDLr tm1Her mice (n = 6 animals per group). Scale bar represents 200 µm. e Quantitative analysis of percentage lipid deposition in total lesion area of aortic sinus (n = 6 animals per group)
Plasma Lipid Concentration and its Correlation with Plaque Growth and Plaque Lipid Content
Total cholesterol, (275.0 ± 10.8 to 665.8 ± 46.7) and LDL (118.2 ± 6.22 to 393.8 ± 22.0) levels showed a rapid increase in the first 8 weeks followed by a moderate increase in the next 6 weeks to a final concentration of 843.5 ± 18.2 and 562.4 ± 40.3, respectively, at 20 weeks (Fig. 2a). We observed an increase in triglyceride levels by 14 weeks which stabilized by 20 weeks while HDL levels were only moderately elevated over time. While plasma lipid levels rapidly increased in the initial phase of 8 weeks, its effect in exponential development of atherosclerotic lesion was observed between 8 and 20 weeks (Fig. 2b, c). Plasma LDL levels showed a significant association (r = 0.86, P < 0.001) with plaque growth and plaque lipid deposition (r = 0.83, P = 0.001) as quantified by oil red O staining (Fig. 2d).
Plasma lipid concentrations and their correlation with plaque growth and plaque lipid accumulation. a Increase in lipid concentration in plasma. b and c Increase in total cholesterol (TC) and low density lipoprotein (LDL) with plaque growth and lipid deposition in plaque. d Correlation of LDL levels in the plasma with increase in lesion and lipid accumulation in aortic sinus (n = 8 animals per group)
Antibody Response and Splenocyte Proliferation to Oxidized LDL
To study the correlation between immune response to modified lipids and progression of atherosclerosis, we assessed the antibody levels to LDL in the serum of mice at different time points of disease development. Hypercholesterolemia induced IgM antibody response to both native LDL and Ox-LDL. While IgM antibody levels to native LDL peaked at 14 weeks and did not show further increase, antibody levels to Ox-LDL significantly increased (P = 0.004) until 20 weeks (Fig. 3a). The levels of IgG antibodies to LDL were very low in the serum, however the antibodies specific for Ox-LDL increased over time and peaked at 14 weeks, followed by a decrease at 20 weeks (Fig. 3b). Splenocyte proliferation to LDL increased slowly over time and was significantly higher at 20 weeks (8.7 ± 1.2 vs 4.1 ± 0.62, P = 0.046) compared to 14 weeks, while Ox-LDL specific proliferation was significantly higher (P < 0.01) at 14 weeks compared to other time point (Fig. 3c). Response to Concanavalin A (Con A) remained comparable between the groups. In corroboration with proliferation the concentration of IFN-γ was higher in the culture supernatant of Ox-LDL stimulated splenocytes at 14 weeks and reduced by 20 weeks (P < 0.001) (Fig. 3d).
Antibody response and Splenocyte proliferation to oxidized LDL. a IgM antibody levels in serum to Oxidized LDL (Ox-LDL) and native LDL as determined by ELISA at 1:100 dilution of serum (n = 8 animals per group). b IgG antibody levels in serum to Oxidized LDL (Ox-LDL) and native LDL as determined by ELISA at 1:100 dilution of serum (n = 8 animals per group). c Splenocyte stimulation to Ox-LDL and native LDL as determined by bromo deoxyuridine (Brdu) proliferation assay (n = 6 animals per group). d Concentration of IFN-γ in the supernatant of splenocytes stimulated with Ox-LDL (n = 6 animals per group)
Changes in T Cell Population in the Spleen
Since hypercholesterolemia and atherosclerosis can influence the peripheral lymphocyte population, we enumerated the T cell subpopulation in the spleen of mice at different time points of disease progression. The percentage of interferon-γ positive CD4 + cells in the spleen did not change significantly during the early stages of the disease, however they were significantly higher (P = 0.045) after 14 weeks compared to week 8 (Fig. 4a, b). Interestingly the IL17 positive cells increased significantly over time (0.9 ± 0.1 to 5. 8 ± 1.2, P = 0.014 from 0 to 20 week) (Fig. 4a, c). In contrast, CD4+ CD25+ Foxp3+ cells decreased with severe hypercholesterolemia (0.3 ± 0.04 to 0.06 ± 0.03, P = 0.025) at 0 and 20 weeks, respectively (Fig. 4a, d). Since age related changes in the proportion of different T cell subsets have been documented, we compared the T cell subpopulation in age and gender matched mice with and without diet-induced atherosclerosis. The proportion of CD4 T cells were comparable between the two groups of mice until 14 weeks, however their numbers in diseased mice increased at 20 weeks (38.8 ± 1.5 vs 27.2 ± 0.66, P = 0.045). The IFN-γ positive CD4 cells showed an increase in hypercholesterolemic mice at 14 (2.9 ± 0.3 vs 1.5 ± 0.2) and 20 weeks (2.9 ± 0.3 vs 1.5 ± 0.2). Treg cells as enumerated by CD4+ CD25+ Foxp3+ was significantly lower (0.20 ± 0.02 vs 0.04 ± 0.014, P = 0.015), while IL17 secreting T cells were significantly higher (0.4 ± 0.04 vs 5. 8 ± 1.2, P = 0.028) at 20 weeks in hypercholesterolemic mice compared to normal mice (Fig. 4e–h).
Changes in T cell population in the spleen in correlation with plaque progression. a The percentages of Th1, Th17, and Treg cells in splenocytes of ApoB tm25gy LDLr tm1Her mice were detected by flow cytometry. Splenocytes from atherosclerotic mice were stimulated with phorbol myristic acetate PMA (10 ng/mL), ionomycin (1 μg/mL), and protein transport blocking reagent-brefeldin A (100 ng/mL), incubated at 37 °C, 5 % CO2 for 4 h, and then assayed for assessment of the number of CD4+IFN-γ+(Th1), CD4+IL-17+ (Th17), and CD4+CD25+Foxp3+ (Treg) T cells by flow cytometry. b–d Quantitative representation of changes in Th1, Th17, and Treg cells in spleen of ApoB tm25gy LDLr tm1Her mice after high fat diet feed for 8, 14, and 20 wk (n = 6 mice per group). e–h Comparison of CD4, CD4+CD25+Foxp3+ (Treg) CD4+IL-17+ (Th17) and CD4+IFN-γ+(Th1), between normal chow diet and high fat diet fed mice at same age) (n = 6 animals per group)
Accumulation of Pro Inflammatory Markers in the Plaque
Macrophages as enumerated by CD68 antibodies increased significantly with plaque progression in the aortic sinus (P < 0.01). The percentage of plaque positive for macrophage staining showed a rapid increase from week 8 (0.05 ± 0.01) to week 14 (0.31 ± 0.07, P = 0.03) and week 20 (0.44 ± 0.11 %, P = 0.02) (Fig. 5a). The percentage of pro-inflammatory marker TNF-α in the plaque was very low (0.02 ± 0.01) at 8 weeks thereafter increased significantly (0.57 ± 0.14, P = 0.03) and remained at high levels till week 20 (Fig. 5b). CD4 + cells in the sinus remained high at 8–14 weeks and showed a small reduction at 20 weeks (0.57 ± 0.07, P = 0.02 compared to week 8) (Fig. 5c). To understand the relationship between Th1, Th17 and Treg cells in the plaque, we studied the expression of IFN-γ, IL17 and TGF-β in the plaque with progression of disease. The RT PCR results were normalized to GAPDH and compared with 0 week aorta as control (Fig. 5d). The changes in expression were also compared with an earlier time point to understand their relative increase or decrease in expression. The expression of IFN-γ was found to increase significantly from 0 to 8 weeks (threefold) and 14 weeks (sixfold) but was not found to increase further. The IL17 expression was found to peak at 14 weeks (fourfold) beyond which there was a decline in expression. In contrast the TGF-β levels showed an increase at week 20. Expression of both IL17 and IFN-γ were highest at 14 weeks. The ratio between IL17 and TGF-β expression was 1.4 at 8 weeks, 2.6 at week 14 and reduced to 0.83 % at week 20, while that between IFN-γ and TGF-β was 3.3 at week 8, 4.0 at week 14 and remained high at 3.7 at week 20 (Fig. 5d).
Accumulation of pro-inflammatory markers in the plaque. Representative photomicrographs showing immunofluorescence staining of aortic sinus sections of mice at 8, 14 and 20 weeks following a high fat diet feed. Left panel represents a bright field image while the right panel represents immunofluorescent staining. a CD68 (red) and its quantitative analysis (n = 6 per group). b TNF-α (red) and its quantitative analysis (n = 6 per group). c CD4 (red) and its quantitative analysis (n = 6 per group). d Relative mRNA levels of IL17, IFN-γ, TGF- and IL10 in the ascending aorta at 8, 14 and 20 week time point compared with week 0 quantified by RT-PCR and normalized to GAPDH
Correlation of Hypercholesterolemia and Disease Progression with Immune Response
Finally we studied the correlation between increased plasma LDL levels with changes in peripheral T cells, immune response to modified LDL and plaque inflammation and the relationship between the changes in circulating cells and immune response with plaque progression. Increase in plasma LDL concentration showed a strong positive correlation with antibody response to Ox-LDL, (r = 0.81, P = 0.003 for IgM and r = 0.77, P = 0.007 for IgG) and Th17 cells in spleen (r = 0.61, P = 0.02). LDL concentrations showed a negative correlation (r = −0.63, P = 0.015) with Treg cells in spleen, while no correlation could be observed with Th1 cells in spleen and splenocyte proliferative response to Ox-LDL. Hypercholesterolemia was found to increase plaque inflammation as seen by the strong positive correlation between plasma LDL increase and TNF- and IFN- positive areas in lesion (r = 0.79, P = 0.004 and r = 0.65, P = 0.014, respectively). We then analyzed the effect of these changes in the immune response on plaque progression. Antibody response and T cell proliferative response to Ox-LDL showed a positive correlation with plaque progression (r = 0.89, P < 0.001 for IgM and r = 0.66, P = 0.001 for IgG and r = 0.63, P = 0.012 for splenocyte proliferation to Ox-LDL). Splenic Th17 cells showed a strong positive correlation with plaque growth (r = 0.84, P < 0.001) while negative correlation was observed with Treg cells (r = −0.83, P < 0.001). Surprisingly the correlation between Th1 cells and plaque progression was not significant (Table 1).
Discussion
In this study we investigated the development of atherosclerosis in ApoB tm25gy LDLrtm1Her mice and correlated the progression of disease with hyperlipidemia, adaptive immune response and changes in lymphocyte population in the spleen. These results provide an insight into the interplay of immune response to modified lipids, changes in circulating lymphocytes and the development of atherosclerotic lesions in a mice model closely resembling humans with respect to cholesterol transport.
As reported earlier, lipid levels in the plasma increased in animals fed on high cholesterol diet which was followed by an increase in the aortic lesion. A rapid phase of lesion growth was accompanied by an accumulation of macrophages, increased expression of IL17 and IFN-γ in the plaque and an increase in adaptive immune response to Ox-LDL. The expression of inflammatory markers and adaptive immune response reduced at later phase of plaque development with a moderate increase in aortic expression of TGF-β and IL10. Although IFN-γ expression was high in the plaque, it did not reflect as increased number of Th1 cells in the spleen, but IL17/Th17 cells increased in the spleen with plaque growth with a concomitant decrease in Treg cells. Significant positive correlation was observed between Th17 cells and the Th17/Treg ratio in the spleen and plaque progression.
Hypercholesterolemia has profound effects on the immune response and host defense against pathogens [30, 31]. Although atherosclerosis is a T-helper1 (Th1) mediated inflammatory disease, severe hypercholesterolemia was associated with a decreased Th1 response and increased levels of Th2 response to modified LDL in ApoE−/− mice [32–34]. LDL accumulation and oxidation is known to activate endothelial cells, macrophages and T cells. Ox-LDL has been identified as one of the most important auto antigens and the major cause of inflammation and immune response in atherosclerosis [35–38]. Antigen presenting cells take up modified LDL and ApoB peptides and present them to naive T cells in spleen or lymph nodes differentiating them to effector T cells which migrate to the arterial intima. Resident macrophages and dendritic cells in the intima can amplify the effector T cell activation and expression of pro-inflammatory molecules which promote disease progression [39]. Therefore, we studied adaptive immune response to Ox-LDL during the progression of disease in mice.
Hypercholesterolemia was found to augment the antibody response to Ox-LDL as seen by the increase in both IgG and IgM antibodies in the serum. This enhanced immune response to Ox-LDL showed a positive correlation with plaque progression in the aortic sinus of mice. Increase in LDL cholesterol resulted in an amplification of CD4 cells secreting IL17 and reduction of regulatory T cells in the spleen but showed no correlation with IFN-γ secreting CD4 cells. Hypercholesterolemia induced Th17 cells showed a strong positive correlation with progression of atherosclerosis while a negative correlation was observed with CD4+ CD25+ Foxp3+ Treg cells in the spleen. These changes were specific for hypercholesterolemic mice as age-matched mice fed with normal chow diet did not show any increase in Th17 cells. Studies in ApoE−/− mice have shown a positive correlation between Th1, Th17 and CD4 cells expressing both IL17 and IFN-γ with disease development and progression [40]. Surprisingly we did not observe a significant association of Th1 cells secreting IFN-γ in the spleen with progression of atherosclerosis. These results are in contrast to previous evidence which has shown that atherosclerosis aggravated by Th1 cells and IFN-γ which contribute to lesion development by enhancing inflammatory cell recruitment and secretion of pro-inflammatory cytokines [41, 42]. Recently Th17 cells were shown to have a pro-atherogenic role, and it was reported that T cells infiltrating human coronary artery produce both IL17 and IFN-γ and act synergistically to induce a pro-inflammatory response [43, 44]. Increased Th17 cells and recombinant IL17 were reported to be associated with the magnitude of atherosclerotic plaque in ApoE−/− mice which was inhibited by neutralizing anti-IL17 antibody, suggesting a direct role of IL17 in disease progression [45]. Although several studies implicate IL17 producing T cells as pro-atherogenic, the role of Th17 cells or IL17 in atherogenesis are inconsistent [46]. Plaque burden was not altered by the deletion of IL17 gene and deletion of suppressor of cytokine signaling 3 (Socs3) which indirectly increases IL17 production was atheroprotective [47, 48]. In a recent study using a biobank of human samples both Th17 and Treg cells were not detected in human aorta across the spectrum of the disease [49].
We observed an increase in the expression of IL17 and IFN-γ in the aorta through the development of lesions until 14 weeks, during the growth phase of the plaque. In the next 6 weeks, the increase in volume of the plaque slowed down and was associated with a decrease in IL17 and IFN-γ expression with a moderate increase in TGF-β expression. Our results are in agreement with earlier studies in LDL-R−/− mice which showed that severe hypercholesterolemia induced an accumulation of Treg in the atherosclerotic aorta [50]. We also observed a positive correlation between higher LDL levels and plaque inflammation as observed by increased TNF-α and IFN-γ positive areas in the aortic sinus.
Thus in ApoB tm25gy LDLr tm1Her mice increase in plasma LDL levels is accompanied by high anti-Ox-LDL antibodies in serum, increased proliferation of Ox-LDL specific T cells, an increase in the proportion of TH17 cells in the spleen and expression IL17, IFN-γ and TNF-α in the plaque resulting in a rapid increase in the progression of lesions. From 14-20 weeks slowing of plaque growth was accompanied by a reduction in antibodies and T cell response to Ox-LDL and Th1 cells in spleen. Anti Ox-LDL IgM antibodies, Th17 cells and the ratio of Th17/Treg cells in the spleen emerged as markers which showed the greatest association with disease development.
Our results suggest that the nature of immune response and the immune system mediated pathogenesis of atherosclerosis may be different in ApoB tm2Sgy/Ldlr tm1Her/J mice compared to ApoE−/− and LDL-R−/− mice. Earlier studies with these models have shown Th1 dominance in the disease process, while our study reveals a stronger role for Th17 cells during the disease progression. The proportion of IL17/Th17 cells and the imbalance between these cells and Treg cells in peripheral lymphoid organs seem to play a role in pathogenesis in these animals. Th17/Treg functional imbalance has been reported in patients with acute coronary syndrome [44]. These results also suggest that this ratio could be developed as a potential marker to study disease progression and to study the effect of therapeutic regulation of inflammation.
Although the strain of mice used in this study closely mimics human disease, it does not represent human atherosclerosis. The animals in our study exhibited severe hypercholesterolemia which is unlikely to occur in humans. The results of this study therefore can only be considered as a model to assess the effect of hypercholesterolemia regulation of the immune system. A limitation of this study is that it is a small preliminary investigation and further elaborate studies with more time points for a longer duration in order to confirm our preliminary results.
Abbreviations
- Apo B:
-
Apolipoprotein B
- Apo E:
-
Apolipoprotein E
- Con A:
-
Concanavalin A
- EVG:
-
Elastica van Gieson
- GAPDH:
-
Glyceraldehyde-3 phosphate dehydrogenase
- HDL:
-
High-density lipoprotein
- HFD:
-
High fat diet
- HBSS:
-
Hanks' balanced salt solution
- IL-17:
-
Interleukin-17
- IL-10:
-
Interleukin-10
- IFN-γ:
-
Interferon-γ
- LDL:
-
Low-density lipoprotein
- LDL-R:
-
Low-density lipoprotein receptor
- NBF:
-
Neutral buffered phenol
- Ox-LDL:
-
Oxidized low-density lipoprotein
- ORO:
-
Oil red O
- PMA:
-
Phorbol myristate acetate
- RT-PCR:
-
Real-time polymerase chain reaction
- RPMI:
-
Rosewell Park Memorial Institute
- TC:
-
Total cholesterol
- Th1:
-
T-helper 1
- TGF-β:
-
Transforming growth factor
- TNF-α:
-
Tumor necrosis factor α
References
Hansson GK (2005) Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med 352:1685–1695
Hansson GK (2009) Atherosclerosis–an immune disease: The Anitschkov Lecture 2007. Atherosclerosis 202:2–10
Daugherty A, Rateri DL (2005) Development of experimental designs for atherosclerosis studies in mice. Methods 36:129–138
Daugherty A (2002) Mouse models of atherosclerosis. Am J Med Sci 323:3–10
Getz GS, Reardon CA (2012) Animal models of atherosclerosis. Arterioscler Thromb Vasc Biol 32:1104–1115
Mukhopadhyay R (2013) Mouse models of atherosclerosis: explaining critical roles of lipid metabolism and inflammation. J Appl Genet 54:185–192
Ishibashi S, Brown MS, Goldstein JL, Gerard RD, Hammer RE, Herz J (1993) Hypercholesterolemia in low density lipoprotein receptor knockout mice and its reversal by adenovirus-mediated gene delivery. J Clin Invest 92:883–893
Zhang SH, Reddick RL, Piedrahita JA, Maeda N (1992) Spontaneous hypercholesterolemia and arterial lesions in mice lacking apolipoprotein E. Science 258:468–471
Nakashima Y, Plump AS, Raines EW, Breslow JL, Ross R (1994) ApoE-deficient mice develop lesions of all phases of atherosclerosis throughout the arterial tree. Arterioscler Thromb 14:133–140
Linton MF, Farese RV Jr, Chiesa G, Grass DS, Chin P, Hammer RE, Hobbs HH, Young SG (1993) Transgenic mice expressing high plasma concentrations of human apolipoprotein B100 and lipoprotein(a). J Clin Invest 92:3029–3037
Callow MJ, Stoltzfus LJ, Lawn RM, Rubin EM (1994) Expression of human apolipoprotein B and assembly of lipoprotein(a) in transgenic mice. Proc Natl Acad Sci USA 91:2130–2134
Soutar AK, Naoumova RP (2007) Mechanisms of disease: genetic causes of familial hypercholesterolemia. Nat Clin Pract Cardiovasc Med 4:214–225
Powell-Braxton L, Veniant M, Latvala RD, Hirano KI, Won WB, Ross J, Dybdal N, Zlot CH, Young SG, Davidson NO (1998) A mouse model of human familial hypercholesterolemia: markedly elevated low density lipoprotein cholesterol levels and severe atherosclerosis on a low-fat chow diet. Nat Med 4:934–938
Veniant MM, Pierotti V, Newland D, Cham CM, Sanan DA, Walzem RL, Young SG (1997) Susceptibility to atherosclerosis in mice expressing exclusively apolipoprotein B48 or apolipoprotein B100. J Clin Invest 100:180–188
Ma Y, Wang W, Zhang J, Lu Y, Wu W, Yan H, Wang Y (2012) Hyperlipidemia and atherosclerotic lesion development in Ldlr-deficient mice on a long-term high-fat diet. PLoS One 7:e35835
Reddick RL, Zhang SH, Maeda N (1994) Atherosclerosis in mice lacking apo E. Evaluation of lesional development and progression. Arterioscler Thromb 14:141–147
Martens GW, Vallerskog T, Kornfeld H (2012) Hypercholesterolemic LDL receptor-deficient mice mount a neutrophilic response to tuberculosis despite the timely expression of protective immunity. J Leukoc Biol 91:849–857
Lichtman AH, Binder CJ, Tsimikas S, Witztum JL (2013) Adaptive immunity in atherogenesis: new insights and therapeutic approaches. J Clin Invest 123:27–36
Andersson J, Libby P, Hansson GK (2010) Adaptive immunity and atherosclerosis. Clin Immunol 134:33–46
Hermansson A, Ketelhuth DF, Strodthoff D, Wurm M, Hansson EM, Nicoletti A, Paulsson-Berne G, Hansson GK (2010) Inhibition of T cell response to native low-density lipoprotein reduces atherosclerosis. J Exp Med 207:1081–1093
Lahoute C, Herbin O, Mallat Z, Tedgui A (2011) Adaptive immunity in atherosclerosis: mechanisms and future therapeutic targets. Nat Rev Cardiol 8:348–358
Hansson GK, Hermansson A (2011) The immune system in atherosclerosis. Nat Immunol 12:204–212
Mallat Z, Gojova A, Brun V, Esposito B, Fournier N, Cottrez F, Tedgui A, Groux H (2003) Induction of a regulatory T cell type 1 response reduces the development of atherosclerosis in apolipoprotein E-knockout mice. Circulation 108:1232–1237
Steven Leary WU, Raymond A, Cartner S, Corey D, Grandin T, Greenacre C, McCrackin MA, Meyer R, Miller D, Shearer J,Yanong R, AVMA Guidelines for the Euthanasia of Animals. https://www.avma.org/issues/animal_welfare/euthanasia.pdf
Daugherty A, Whitman SC (2003) Quantification of atherosclerosis in mice. Methods Mol Biol 209:293–309
Feng B, Zhang D, Kuriakose G, Devlin CM, Kockx M, Tabas I (2003) Niemann-Pick C heterozygosity confers resistance to lesional necrosis and macrophage apoptosis in murine atherosclerosis. Proc Natl Acad Sci 100:10423–10428
Mundkur L, Mukhopadhyay R, Samson S, Varma M, Kale D, Chen D, Shivaprasad S, Sivanandan H, Soman V, Lu X, Kakkar VV (2013) Mucosal Tolerance to a Combination of ApoB and HSP60 Peptides Controls Plaque Progression and Stabilizes Vulnerable Plaque in Apob(tm2Sgy)Ldlr(tm1Her)/J Mice. PLoS One 8:e58364
Lopes-Virella MF, Koskinen S, Mironova M, Horne D, Klein R, Chassereau C, Enockson C, Virella G (2000) The preparation of copper-oxidized LDL for the measurement of oxidized LDL antibodies by EIA. Atherosclerosis 152:107–115
Dimayuga PC, Zhao X, Yano J, Chyu KY (2006) Changes in immune responses to oxidized LDL epitopes during aging in hypercholesterolemic apoE(−/−) mice. Am J Physiol Regul Integr Comp Physiol 291:R1644–R1650
Lei L, Li H, Yan F, Xiao Y (2013) Hyperlipidemia Impaired Innate Immune Response to Periodontal Pathogen Porphyromonas gingivalis in Apolipoprotein E Knockout Mice. PLoS One 8:e71849
Martens GW, Arikan MC, Lee J, Ren F, Vallerskog T, Kornfeld H (2008) Hypercholesterolemia impairs immunity to tuberculosis. Infect Immun 76:3464–3472
Robertson AK, Zhou X, Strandvik B, Hansson GK (2004) Severe hypercholesterolaemia leads to strong Th2 responses to an exogenous antigen. Scand J Immunol 59:285–293
Zhou X, Johnston TP, Johansson D, Parini P, Funa K, Svensson J, Hansson GK (2009) Hypercholesterolemia leads to elevated TGF-beta1 activity and T helper 3-dependent autoimmune responses in atherosclerotic mice. Atherosclerosis 204:381–387
Zhou X, Paulsson G, Stemme S, Hansson GK (1998) Hypercholesterolemia is associated with a T helper (Th)1/Th2 switch of the autoimmune response in atherosclerotic apo E-knockout mice. J Clin Invest 101:1717–1725
Hansson GK (2001) Immune mechanisms in atherosclerosis. Arterioscler Thromb Vasc Biol 21:1876–1890
Steinberg D, Parthasarathy S, Carew TE, Khoo JC, Witztum JL (1989) Beyond cholesterol. Modifications of low-density lipoprotein that increase its atherogenicity. N Engl J Med 320:915–924
Binder CJ, Chang MK, Shaw PX, Miller YI, Hartvigsen K, Dewan A, Witztum JL (2002) Innate and acquired immunity in atherogenesis. Nat Med 8:1218–1226
Hansson GK (2002) Vaccination against atherosclerosis: science or fiction? Circulation 106:1599–1601
Stemme S, Faber B, Holm J, Wiklund O, Witztum JL, Hansson GK (1995) T lymphocytes from human atherosclerotic plaques recognize oxidized low density lipoprotein. Proc Natl Acad Sci USA 92:3893–3897
Gao Q, Jiang Y, Ma T, Zhu F, Gao F, Zhang P, Guo C, Wang Q, Wang X, Ma C, Zhang Y, Chen W, Zhang L (2010) A critical function of Th17 proinflammatory cells in the development of atherosclerotic plaque in mice. J Immunol 185:5820–5827
Koga M, Kai H, Yasukawa H, Yamamoto T, Kawai Y, Kato S, Kusaba K, Kai M, Egashira K, Kataoka Y, Imaizumi T (2007) Inhibition of progression and stabilization of plaques by postnatal interferon-gamma function blocking in ApoE-knockout mice. Circ Res 101:348–356
Methe H, Brunner S, Wiegand D, Nabauer M, Koglin J, Edelman ER (2005) Enhanced T-helper-1 lymphocyte activation patterns in acute coronary syndromes. J Am Coll Cardiol 45:1939–1945
Eid RE, Rao DA, Zhou J, Lo SF, Ranjbaran H, Gallo A, Sokol SI, Pfau S, Pober JS, Tellides G (2009) Interleukin-17 and interferon-gamma are produced concomitantly by human coronary artery-infiltrating T cells and act synergistically on vascular smooth muscle cells. Circulation 119:1424–1432
Cheng X, Yu X, Ding YJ, Fu QQ, Xie JJ, Tang TT, Yao R, Chen Y, Liao YH (2008) The Th17/Treg imbalance in patients with acute coronary syndrome. Clin Immunol 127:89–97
Gao Q, Jiang Y, Ma T, Zhu F, Gao F, Zhang P, Guo C, Wang Q, Wang X, Ma C, Zhang Y, Chen W, Zhang L (2010) A critical function of Th17 proinflammatory cells in the development of atherosclerotic plaque in mice. J Immunol 185:5820–5827
Taleb S, Tedgui A, Mallat Z (2015) IL-17 and Th17 cells in atherosclerosis: subtle and contextual roles. Arterioscler Thromb Vasc Biol 35:258–264
Taleb S, Romain M, Ramkhelawon B, Uyttenhove C, Pasterkamp G, Herbin O, Esposito B, Perez N, Yasukawa H, Van Snick J, Yoshimura A, Tedgui A, Mallat Z (2009) Loss of SOCS3 expression in T cells reveals a regulatory role for interleukin-17 in atherosclerosis. J Exp Med 206:2067–2077
Erbel C, Chen L, Bea F, Wangler S, Celik S, Lasitschka F, Wang Y, Bockler D, Katus HA, Dengler TJ (2009) Inhibition of IL-17A attenuates atherosclerotic lesion development in apoE-deficient mice. J Immunol 183:8167–8175
van Dijk RA, Duinisveld AJF, Schaapherder AF, Mulder-Stapel A, Hamming JF, Kuiper J, de Boer OJ, van der Wal AC, Kolodgie FD, Virmani R, Lindeman JHN (2015) A Change in Inflammatory Footprint Precedes Plaque Instability: a systematic evaluation of cellular aspects of the adaptive immune response in human atherosclerosis. J Am Heart Assoc 4
Maganto-Garcia E, Tarrio ML, Grabie N, Bu DX, Lichtman AH (2011) Dynamic changes in regulatory T cells are linked to levels of diet-induced hypercholesterolemia. Circulation 124:185–195
Acknowledgments
We gratefully acknowledge the support of the trustees of Thrombosis Research Institute, London and Bangalore and the Tata Social Welfare Trust, India (TSWT/IG/SNB/JP/Sdm). The study was supported by Department of Biotechnology, Ministry of Science and Technology, Government of India (BT/01/CDE/08/07) and Garry Weston foundation UK.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
About this article
Cite this article
Rao, L.N., Ponnusamy, T., Philip, S. et al. Hypercholesterolemia Induced Immune Response and Inflammation on Progression of Atherosclerosis in Apob tm2Sgy Ldlr tm1Her/J Mice. Lipids 50, 785–797 (2015). https://doi.org/10.1007/s11745-015-4046-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11745-015-4046-4