Abstract
EDs restricted visitors during the COVID-19 pandemic on the assumption that the risks of disease spread outweighed the psychological benefits of liberal visitation. But data suggest that beyond providing emotional support, family and caregivers can clarify history, improve patient monitoring, and advocate for patients—actions that can improve quality of care. Our objective was to assess whether removing visitors from the bedside contributed to errors in emergency care. We reviewed a database of medical errors covering visits from 11/15/17 to 7/30/22 at an urban, tertiary-care, academic ED for five types of error amenable to visitor intervention: inadequate history gathering, inadequate monitoring, falls, giving a medication to which a patient is allergic, and inappropriate medication dosing. These records were reviewed by two investigators to determine the likelihood visitor presence could have prevented the error. For those errors judged susceptible to visitor intercession, the number in each category was compared for the period before and after strict restrictions took effect. Our review found 27/781 (3.5%) errors in the pre-pandemic period and 27/568 (4.8%) errors in the pandemic period fell into one of these five categories (p = 0.29). Visitors prevented harm from reaching the patient in three of 27 pre-pandemic errors (11.1%), compared to 0 out of 27 peri-pandemic errors (p = 0.23). On review by two attendings, 17/24 (70.8%) errors that reached the patient in the pre-pandemic period were judged amenable to visitor intervention, compared to 25/27 (92.6%) in the pandemic period (p = 0.09). There were no statistically significant differences in the categories of error between the two groups; monitoring errors came the closest: 1/17 (5.9%) pre-COVID errors amenable to visitor intervention in these categories were monitoring related, whereas 7/25 (28.0%) post-COVID errors were (p = 0.16). While this study did not demonstrate a statistically significant difference in error between lenient and restrictive visitation eras, we did find multiple cases in the pre-COVID era in which family presence prevented error, and qualitative review of post-COVID errors suggested many could have been prevented by family presence. Larger trials are needed to determine how frequent and consequential such errors are and how to balance the public health imperative of curbing disease spread with the harm caused by restricting visitation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past few decades, many providers and patient advocates have pushed for increased or unrestricted family visitation, particularly in the intensive care setting, arguing that restrictions were “neither compassionate, caring, or necessary” [1]. These liberalizing efforts focused on the ICU both because hospitals had for decades restricted visitation in that setting and because family presence during critical illness was theorized to be particularly vital to patient wellbeing. Subsequent research found liberalizing visiting hours in the ICU setting were associated with lower rates of delirium, reduced patient anxiety, improved family satisfaction, and better cardiovascular outcomes [2,3,4,5]. To date, comparatively little research has been conducted into the effect of visitation restrictions in the emergency department setting.
The trend toward more open visitation came to an abrupt halt with the rise of the COVID-19 pandemic in early 2020. Almost overnight, hospitals that once regularly welcomed family and caregivers to the bedside effectively barred their doors to visitors, at times even when patients were taking their last breaths [6, 7]. Given both the initial dearth of personal protective equipment and the high case rates in early waves, hospital leaders deemed such restrictions necessary to preserve the health care system’s capacity to care for sick patients. Yet some restrictions lingered far past the acute crisis, and while the psychological harm caused by such policies was plain, there has been little research into the effect they may have had on error. Visitors in the ED can potentially guard against error by clarifying a patient’s history, serve as an additional set of eyes to monitor sick patients, prevent the administration of inappropriate medications, and advocate for their loved one to get appropriate medications that might otherwise be overlooked. Prior studies have not directly addressed the potential impact of visitation restrictions on medical error.
The objective of this study was to determine whether restrictive policies implemented during the pandemic led to an increase in categories of medical errors particularly amenable to family and caregiver intercession.
Methods
Study setting
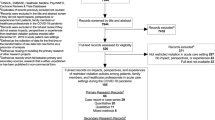
We conducted a retrospective, observational, cohort study of consecutive patients presenting from November 15, 2017 to July 30, 2022 at an urban, tertiary-care, academic emergency department with an annual census of 53,000 visits. Visitation restrictions were implemented at the study emergency department on or around March 15, 2020, which was taken as the dividing line between pre-COVID and peri-COVID visitation eras. In the first 3 months of the pandemic all visitors were banned, while for the remainder of the peri-pandemic period, visitors were only allowed on a case-by-case basis at the discretion of the emergency providers. Institutional review board (IRB) exemption as a quality improvement initiative was received prior to initiation of the study.
Study design
Investigators reviewed a database consisting of patient visits that had taken place in that period, been referred to the department’s Quality Assurance (QA) Committee, and then judged by the committee to have potentially contained a medical error. The QA Committee comprises 20 attending physicians and nurses tasked by the department with reviewing cases for error and providing feedback to involved providers and the department at large. Each member undergoes training in quality improvement methodology prior to joining the committee. Error is determined by consensus of the members. This study included cases that the committee determined had “definitely” occurred as well as those that “probably” or “possibly” occurred. The committee reviews all cases of death within 24 h, returns within 72 h leading to admission, ICU transfers within 24 h of admission, as well as cases flagged by a clinician or which resulted in a formal patient complaint.
Prior to the data analysis, the study authors agreed on a set of five error types that they considered most amenable to visitor intercession. These were (1) inadequate history gathering, (2) inadequate monitoring, (3) falls, (4) giving a medication to which a patient is allergic, and (5) inappropriate medication dosing. One of the study authors then reviewed this database of medical errors for these five types of error. Rates of such errors were compared before and after the implementation of pandemic visitation restrictions. Errors in one of these five categories were then reviewed by two of the investigators to determine the likelihood visitor presence could have prevented the error. For instance, if there was a medication error for a drug the patient did not take at home, this was judged not susceptible to visitor intercession, whereas a patient not receiving their home insulin would be judged potentially amenable to visitor intercession. For the five categories together, the number of errors affecting the patient that were judged susceptible to visitor intercession was compared for the period before and after strict restrictions took effect, which was the primary outcome of the study. Secondary outcomes included difference in the number of errors prevented from reaching the patient by visitor intercession and differences in errors judged amenable to visitor intercession within each of the five categories individually.
Primary data analysis
All p values are from a two-sample test of proportions, with two-sided 95% confidence intervals, testing the null hypothesis that there were no differences between the two groups. The results are reported as percentages. When appropriate, “p” values sensitivities, specificities, and positive and negative predictive values are reported along with 95% confidence intervals (CI) around the point estimate.
Results
Of 781 errors in the pre-pandemic period and 568 errors in the post-pandemic period, 27 (3.5%) pre-pandemic and 27 (4.8%) peri-pandemic errors fell into one of these five categories (p = 0.29). Visitors prevented harm from reaching the patient in three of the pre-pandemic errors out of 27 (11.1%), compared to zero out of 27 (0%) in the peri-pandemic period (p = 0.23). On review by two ED attendings, 17/24 (70.8%) errors that reached the patient in the pre-pandemic period were judged amenable to family intervention, compared to 25/27 (92.6%) in the peri-pandemic period (p = 0.09). There were no statistically significant differences in the categories of error between the two groups; monitoring errors came the closest: 1/17 (5.9%) pre-COVID errors affecting the patient were monitoring related, whereas 7/25 (28.0%) post-COVID errors were (p = 0.16). We did not find statistical significance for our primary or secondary outcomes (see Table 1).
Four cases were also chosen to illustrate qualitatively the effect family or caregiver presence can have on error in the emergency setting. They include errors in history-taking, dispensing of medications, and monitoring. Three cases are from the pandemic visitation period; one is from the pre-pandemic visitation period (see Fig. 1).
Discussion
Although this pilot study did not show a statistically significant difference in errors for the categories assessed between the pre-pandemic and peri-pandemic periods studied, it did show a trend towards statistical significance. Furthermore, a review of these errors uncovered multiple instances in which visitor presence prevented or may have prevented harm. There was an increased number of monitoring errors in the pandemic era, but perhaps partly due to the size of the study, we did not demonstrate statistical significance. This raises the possibility that if family or caregiver presence does reduce error, maximizing family presence as an additional avenue for patient care monitoring could be particularly useful. If so, family and caregiver presence would likely be most valuable when the health care system is overwhelmed, and when the risk of negligent care, as seen in some of the clinical vignettes, may be higher. In that case, hospital policies that bar visitors at times of crowding might deprive patients of an additional layer of protection precisely when they need it most.
New York City hospitals in COVID’s first wave had multiple patients on BiPAP who were found dead after they took off their masks to go to the bathroom and collapsed [8]. A recent lawsuit about a 23-year-old patient who died while in the ED after a fentanyl overdose treated with naloxone alleges the patient was ignored by staff for 7 h even as the fentanyl toxicity recurred, leading to respiratory arrest. Family members were not allowed into the emergency department due to COVID restrictions [9]. It is easy to see in such cases how family or caregiver presence could have saved lives. Furthermore, an association between visitation restriction implemented during the pandemic and the incidence of delirium in emergency medicine admissions was noted in a single-center, retrospective study in Japan [10].
It is important to note that visitation may cause harm in some instances, such as if a family member or caregiver is disruptive. One pre-pandemic study found increased feelings of burnout among ICU providers after a more lenient visitation policy was adopted, though clinicians generally maintained favorable opinions of that policy [10].
The public health benefits of family visitation in a pandemic must also be balanced against the harm these policies are already known to cause patients and families. Pandemic-era polices led patients to avoid emergency departments due to fear of being cut off from their loved ones and this, in turn, may have delayed critical end-of-life care decisions [11, 12]. These policies added a trauma of separation to illness and death during the pandemic [13,14,15].
Attempting to prove causality between family and caregiver presence and error is an inherently fraught endeavor for a number of reasons. Near misses involving families and caregivers may go unreported. We do not systematically record the presence or absence of family. In addition, it is difficult to assess whether family or caregiver presence would have changed an outcome simply because it could have. It is clear, however, that families and caregivers can play a vital role in preventing medical errors, even if we cannot conclude the magnitude of their impact from this study. Better assessing the effect of visitor restrictions on error will be vital to implementing appropriate visitation policies both presently and during future pandemics.
Limitations
This study suffers from several important limitations, foremost among them the inability to control for the markedly changed care environment engendered by the pandemic beyond the different visitation policy. The statistically significant change in overall error rates between the two periods raises questions about whether other factors—such as a difference in the patient population, non-visitation systems changes, or changed attitudes toward error—might independently have affected error rates for the five categories studied. It is worth noting that a prior study in the same department, which included only those errors deemed to have “definitely” or “probably” occurred, did not find a statistically significant change in errors between April-June of 2020 and the corresponding months in 2018 and 2019 [16]. While not the focus of this study, it does appear that the “possibly” error category, which accounts for only four of the pre-COVID and three of the COVID era errors here, makes up much of the difference in overall error rates reported above.
While the QA Committee’s process of reviewing errors remained broadly unchanged in both periods, it certainly did not capture every error that occurred (falls, for instances, were rarely reviewed as errors in this database unless they resulted in an actionable adverse event such as a laceration requiring sutures). It is also possible that the attitude toward reporting or adjudicating error may have differed during the peri-pandemic period.
Initial assignment of errors into one of the five categories was also performed by a single reviewer—independent review by another clinician at that stage might have included cases missed by the initial assessment. In addition, the reviewer was not blinded to whether the errors were pre- or peri-pandemic at the time the data were reviewed. The determination of whether an error was amenable to family intervention was made jointly by the two reviewers, rather than separately with a subsequent review of discrepancies. Charts were reviewed to assess for signs of family presence, but even in the pre-pandemic period, the documentation of visitor presence was unreliable enough that except in circumstances when visitors interceded, it was difficult to determine whether or when they were at bedside.
Furthermore, we believe this study was likely underpowered to show statistical significance. Lastly, this was a single-center study, which limits its generalizability.
Conclusion
While this pilot did not demonstrate a statistically significant difference in error between lenient and restrictive visitation eras, we did find multiple cases in the pre-COVID era in which family presence prevented error, and qualitative review of post-COVID errors suggested several could have been prevented by family presence. Further research is needed to determine how frequent and consequential such errors are and how to balance the public health imperative of curbing disease spread with the harm caused by restricting visitation.
Data availability
De-identified data is available upon request.
References
Berwick DM, Kotagal M (2004) Restricted visiting hours in ICUs: time to change. JAMA 292(6):736–737. https://doi.org/10.1001/jama.292.6.736
Rosa RG, Tonietto TF, Tonietto TF et al (2017) Effectiveness and safety of an extended ICU visitation model for delirium prevention: a before and after study. Crit Care Med 45(10):1660–1667. https://doi.org/10.1097/ccm.0000000000002588
Eghbali-Babadi M, Shokrollahi N, Mehrabi T (2017) Effect of family-patient communication on the incidence of delirium in hospitalized patients in cardiovascular surgery ICU. Iran J Nurs Midwifery Res 22(4):327–331. https://doi.org/10.4103/1735-9066.212985
Nassar AP, Junior APN, Junior APN et al (2018) Flexible versus restrictive visiting policies in icus: a systematic review and meta-analysis. Crit Care Med 46(7):1175–1180. https://doi.org/10.1097/ccm.0000000000003155
Fumagalli S, Fumagalli S, Boncinelli L et al (2006) Reduced cardiocirculatory complications with unrestrictive visiting policy in an intensive care unit results from a pilot. Randomized Trial Circulation 113(7):946–952. https://doi.org/10.1161/circulationaha.105.572537
Lo AX, Wedel LK, Liu SW et al (2022) COVID-19 hospital and emergency department visitor policies in the United States: impact on persons with cognitive or physical impairment or receiving end-of-life care. J Am Coll Emerg Physicians Open. https://doi.org/10.1002/emp2.12622
Weiner HS, Firn J, Hogikyan ND et al (2020) Hospital visitation policies during the SARS-CoV-2 pandemic. Am J Infect Control 49(4):516–520
Rosenthal B, Goldstein J, Otterman S, Fink S. Why surviving the virus might come down to which hospital admits you. The new york times. https://www.nytimes.com/2020/07/01/nyregion/Coronavirus-hospitals.html. Published 1 July 2020. Accessed on 4 Feb 2023
Santiago E. Resuscitated after overdose, man, 23, dies in yale ER hallway: lawsuit. Patch. https://patch.com/connecticut/newhaven/resuscitated-after-overdose-man-23-dies-yale-er-hallway-lawsuit. Published 19 Aug 2022. Accessed 4 Feb 2023
Giannini A, Miccinesi G, Prandi E, Buzzoni C, Borreani C, Borreani C (2013) Partial liberalization of visiting policies and ICU staff: a before-and-after study. Intensive Care Med 39(12):2180–2187. https://doi.org/10.1007/s00134-013-3087-5
Gettler E, Stern R, Ni B et al (2022) Avoidance of emergency care in the Southeastern United States during the COVID-19 pandemic. Open Forum Infect Dis. https://doi.org/10.1093/ofid/ofac161. (Published online 8 April 2022)
Azad TD, Al-Kawaz MN, Al-Kawaz M, Turnbull AE, Rivera-Lara L (2021) Coronavirus disease 2019 policy restricting family presence may have delayed end-of-life decisions for critically ill patients. Crit Care Med. https://doi.org/10.1097/ccm.0000000000005044
Iness AN, Abaricia JO, Sawadogo W et al (2022) The effect of hospital visitor policies on patients, their visitors, and healthcare providers during the COVID-19 pandemic: a systematic review. Am J Med. https://doi.org/10.1016/j.amjmed.2022.04.005. (Published online 1 April 2022)
Zapata, Jr. V. Texts from my Father, in Elmhurst Hospital. The New Yorker. https://www.newyorker.com/magazine/2020/04/13/texts-from-my-father-in-elmhurst-hospital. Published 13 April 2020. Accessed on 7 Jan 2023
Shah J. A comedian watched her mom die from COVID on an iPad. Her live tweets will break you. Los Angeles Times. https://www.latimes.com/lifestyle/story/2020-06-18/comedian-laurie-kilmarten-live-tweets-her-mothers-death. Published 18 June 2020. Accessed on 7 Jan 2023
Grossman ES, Hoffmann B, Tibbles C et al (2022) Do error rates change in the emergency department when patient volume decreases: the effect of COVID-19 on ED error. Intern Emerg Med 17(5):1547–1550. https://doi.org/10.1007/s11739-022-03020-x
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
CMM, REW and SAG are responsible for study concept and design, drafting of the manuscript, and critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
CMM reports no conflicts of interest; REW reports no conflicts of interest; SAG reports no conflicts of interest.
Human and animal rights and Informed consent
This study followed institutional and national guidelines; institutional review board (IRB) exemption as a quality improvement initiative was received prior to initiation of the study, deeming informed consent unnecessary.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marks, C.M., Wolfe, R.E. & Grossman, S.A. The effect of visitation restrictions on ED error. Intern Emerg Med 19, 1425–1430 (2024). https://doi.org/10.1007/s11739-024-03537-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-024-03537-3