Abstract
Acute-on-chronic liver failure (ACLF) implies high short-term mortality rates and usually requires intensive care unit (ICU) admission. Proper prognosis for these patients is crucial for early referral for liver transplantation. The superiority of CLIF-C ACLF score in Asian patients with ACLF admitted to an ICU remains inconclusive when compared to other scoring systems. The purpose of the study is (i) to compare the predictive performance of original MELD, MELD-Lactate, CLIF-C ACLF, CLIF-C ACLF-Lactate, and APACHE-II scores for short-term mortality assessment. (ii) to build and validate a novel scoring system and to compare its predictive performance to that of the original five scores. Two hundred sixty-five consecutive cirrhotic patients with ACLF who were admitted to our ICU were enrolled. The prognostic values for mortality were assessed by ROC analysis. A novel model was developed and internally validated using fivefold cross-validation. Alcohol abuse was identified as the primary etiology of cirrhosis. The AUROC of the five prognostic scores were not significantly superior to each other in predicting 1-month and 3-month mortality. The newly developed prognostic model, incorporating age, alveolar–arterial gradient (A-a gradient), BUN, total bilirubin level, INR, and HE grades, exhibited significantly improved performance in predicting 1-month and 3-month mortality with AUROC of 0.863 and 0.829, respectively, as compared to the original five prognostic scores. The novel ACLF model seems to be superior to the original five scores in predicting short-term mortality in ACLF patients admitted to an ICU. Further rigorous validation is required.
Graphical abstract

“Created with BioRender.com”.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Patients with liver cirrhosis are at increased risk of acute decompensation, which may lead to organ failure(s) and the development of acute-on-chronic liver failure (ACLF) [1,2,3,4,5]. The high mortality rate associated with the syndrome often necessitates ICU admission [3, 5, 6]. Therefore, expertise in both hepatology and critical care is crucial in the intensive care management of these patients for optimizing recovery outcomes. However, some patients are at a heightened risk of rapid clinical deterioration, necessitating urgent liver transplantation (LT) [6, 7]. Due to the short transplantation window, a rapid decision-making process is necessary [6, 7].
Two important issues for a successful bridging to LT are accurate prognostication and prioritization of ACLF patients awaiting LT [6]. Therefore, it is essential to develop an accurate prognostic score to estimate the outcomes in ACLF patients and help guide clinicians in determining the appropriate treatment options according to the predicted outcomes [8].
Despite the development of several prognostic scoring systems for evaluating outcomes and organ dysfunction in ICU patients [9, 10], accurately predicting short- and long-term mortality remains a significant challenge [11]. The European Association for the Study of the Liver-Chronic Liver Failure (EASL-CLIF) Consortium developed the CLIF Consortium ACLF score (CLIF-C ACLFs) by simplifying the original CLIF-Sequential Organ Failure Assessment (SOFA) score based on CLIF-C organ failure (OF) scores, which demonstrated higher prognostic accuracy than the CLIF-SOFA, the Model for End-Stage Liver Disease (MELD), MELD-Na, and Child–Pugh (CP) scores [12] for ACLF patients. It was also externally validated in ACLF patients hospitalized in a single ICU [12]. The CLIF-C ACLF-D score was derived from the Predicting Acute-on-Chronic Liver Failure (PREDICT) study [13]. The newly devised score predicts the likelihood of ACLF occurrence in individuals with acute decompensation within 3 months of hospitalization. The score demonstrates comparable precision and reduced variance in comparison to alternative scores, as evidenced by the validation set [13].
Several generations of the acute physiology and chronic health evaluation (APACHE) system have been devised, establishing a reliable ICU prognostic tool. The system gauges the severity of illness and general health of adult critically ill patients [14,15,16]. The APACHE model demonstrated exceptional predictive precision in adjusting for mortality risk in the ICU [17]. The Child–Turcotte–Pugh (CTP) score and the MELD score are frequently employed prognostic tools in patients with liver cirrhosis. They have been utilized as key determinants in allocating donor livers in the United States since February 2002 [18,19,20]. Furthermore, several scoring systems have been developed to predict mortality in ACLF, including the MELD-Lactate score [21], and the CLIF ACLF-Lactate score [11].
However, limited research has been conducted to compare ICU prognostic scores with liver failure scores in individuals with ACLF. The optimal prognostic scoring system for predicting overall mortality in ICU-admitted ACLF patients remains uncertain. In addition, it is intriguing whether a new model could be created to outperform the pre-existing prognostic scores. Therefore, our primary objective was to compare the prognostic capabilities of the original MELD, MELD-Lactate, CLIF-C ACLF, CLIF ACLF-Lactate, and APACHE-II scores for predicting short-term mortality, specifically 1-month and 3-month mortality in ACLF patients. Second, a novel predicting scoring system was developed and tested for its superiority over the original five scoring systems in predicting short-term mortality among ACLF patients admitted to the ICU.
Methods
ACLF diagnosis and grading
ACLF diagnosis was established according to the diagnostic criteria specified by the EASL-CLIF Consortium. The EASL-CLIF Consortium criteria were used to assess the severity of ACLF [1, 12]. ACLF grade 1 is defined by either (a) the presence of a single organ failure (e.g., hepatic, coagulation, circulatory, or pulmonary) accompanied by a serum creatinine level of 1.5–1.9 mg/dL and/or West-Haven grade 1 or 2 hepatic encephalopathy; or (b) single renal failure (creatinine level ≥ 2.0 mg/dL) in the absence of other organ failure; or (c) single brain failure with a serum creatinine level of 1.5–1.9 mg/dL. ACLF 2 was characterized by two organ failures, while ACLF 3 was characterized by the presence of three or more organ failures.
Patient selection
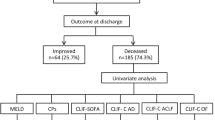
This study included cirrhotic patients with acute decompensation (AD) admitted to the hepato-gastroenterology ICU of our hospital between November 2013 and December 2019, meeting the inclusion criteria. Patients who were under age 18 years old, had pre-existing hepatocellular carcinoma or other cancers with/without liver metastasis, were pregnant, had undergone orthotopic liver transplantation before or during ICU admission, or follow-up, had ACLF score of 0, could not be classified into ACLF grades 1/2/3, and did not have available serum lactate levels within 24 h of ICU admission were excluded from the analysis. The study design and patient selection flow chart are presented in Fig. 1.
Definition of liver cirrhosis and its acute decompensation
Liver cirrhosis was diagnosed through histopathological confirmation or a composite of compatible clinical features, laboratory tests, endoscopic findings, as well as radiological imaging [11, 22,23,24]. Acute decompensation of cirrhosis is associated with severe and life-threatening complications, such as variceal bleeding, refractory ascites, sepsis, hepatic encephalopathy, or spontaneous bacterial peritonitis [22, 23].
Data source and collection
Data were collected retrospectively from the medical records of patients admitted to the hepato-gastroenterology ICU at Chang-Gung Memorial Hospital, Linkou medical center. This included patient demographics, etiology of cirrhosis, laboratory test results, vital signs, Glasgow coma scale score, urine output, oxygenation support, mechanical ventilator settings, and survival interval. Data were collected within 24 h of ICU admission and scored using appropriate formulas.
Primary, secondary outcomes, and scheduled follow-up periods
The primary outcomes were mortalities at 1 month and 3 months. Secondary outcomes were in-hospital, 6-month, and 12-month mortality. Survival of patients after discharge was confirmed through telephone interviews and/or analysis of medical records. Each patient was followed until the date of death or February 28th, 2022, whichever came first. Because patients who underwent liver transplantation during the study were excluded from the analysis, a completing risk analysis was not performed.
Calculation of prognostic scores
Prognostic scores were calculated using their respective formulas proposed in previous studies. The MELD score was 11.2 × ln [international normalized ratio (INR)] + 9.57 × ln (creatinine, mg/ dL) + 3.78 × ln (bilirubin, mg/dL) + 6.43), with a lower bound of 1 for all three variables and an upper bound of 4 for serum creatinine [25]. MELD-Lactate = 0.251 + 5.5257 × sqrt(lactate) + 0.338 × MELD [21]. The CLIF-C ACLF score = 10 × [0.33 × CLIF-OFs + 0.04 × Age + 0.63 × ln (WBC count) – 2] [12]. The lactate-adjusted CLIF-C ACLF (CLIF-C ACLF-Lactate score) = CLIF-C ACLFs + 8 × ln (lactate) – 7 [26]. The APACHE-II score was calculated according to the study by Knaus WA, et al [27].
Statistical analysis
Continuous variables were presented as mean ± SD or median and interquartile range (IQR 25–75 percentile) depending on their distribution, and comparisons were made using the Independent Student t test for normal distributions and the Mann–Whitney U test for non-normal distributions. Categorical variables were presented as frequencies and percentages, and their comparison was performed using the Chi-square test. Fisher’s exact test was used in cases where more than 20% of the statistic cells had an expected frequency of less than 5. The novel model’s predictive ability was assessed by determining the area under the receiver operating characteristic curve (AUROC) and compared with MELD, MELD-Lactate, CLIF-C ACLF, CLIF-C ACLF Lactate, and APACHE-II scores. A competing risk analysis was not performed as the number of patients who received liver transplantation during follow-up was too small and had been excluded from the analysis. The predictive performance of each score to predict mortality was compared using the Delong test. Statistical analyses were performed using IBM SPSS Statistics 26 (SPSS Inc., Chicago, IL, USA) and a p value < 0.05 was considered significant.
Novel prognostic model building
Using the current dataset, mortality at different time points (i.e., 1 month, 3 months, etc.) was the dependent variable (Supplementary Table 1). The initial model considered several independent variables, including patients’ demographics, etiology of cirrhosis, hemograms, serum biochemistry tests, vital signs (body temperature, blood pressure, respiratory rate, and heart rate), oxygenation support, mechanical ventilator setting, Glasgow coma scale (GCS) score, and urine output. Variables with p < 0.20 in the univariate analysis were entered in a multivariate logistic regression analysis [28] to identify independent predictors associated with the primary and secondary outcomes and to select variables that could predict mortality at different time points with an AUROC > 0.8 [21]. As shown in Supplementary Table 1, Model 1, 2, and 3 were, thus, obtained and were further evaluated by their performance [29]. Finally, Model 3 was found to have the highest AUROC across different time points and was, therefore, chosen as our new prediction model (Supplementary Table 1).
Model validation
For model validation, internal validation by fivefold cross-validation was performed. This method divides the dataset into 5 subsets of 80/20 splits (folds) where each 80%-fold is used as the training set for the remaining 20%. Summary statistics for this procedure include the AUROC, Brier scores, and accuracy at intervals. As revealed in Supplementary Table 2, the new model had a good performance of AUC, Brier scores, and accuracy on the train and test set across different time points.
Results
Patients’ baseline characteristics
A total of 265 cirrhotic patients with ACLF were enrolled from November 2013 to December 2019 and followed until February 2022 (Fig. 1). Table 1 displays the baseline characteristics of the 265 patients. The overall mean age was 55.2 ± 13.3 years old. Two hundred five patients (77.4%) were male. The main etiology of cirrhosis in all patients was alcohol abuse (152 patients, 57.4%). The second most common etiology was hepatitis B virus infection (56 patients, 21.1%), followed by hepatitis C virus infection (37 patients, 14.0%) and other etiologies including non-alcoholic steatohepatitis (NASH) and autoimmune hepatitis. In addition, upper gastrointestinal bleeding (131 patients; 49.4%) accounted for the major indication for ICU admission. The mean follow-up period was 1.6 years. The 1-month mortality rate was 35.8% (95/265). The in-hospital mortality rate was 45.7% (121/265). The 3-month mortality rate was 50.2% (133/265). The 6-month mortality rate was 59.2% (157/265). The 1-year mortality rate was 65.3% (173/265). The overall mortality rate was 72.4% (192/265).
For survivor patients, the main indication for ICU admission was upper GI bleeding (53 patients, 72.6%), while the main indication for ICU admission was sepsis (98 patients, 51.0%) in non-survivor patients.
In the non-survivor group, A-a gradient, respiratory rate, white cell count, INR, serum bilirubin, serum blood urea nitrogen, serum creatinine, serum glucose, and serum lactate were significantly higher than in the survivor group. Conversely, arterial pH, body temperature, and serum albumin were significantly higher in the survivor group than in the non-survivor group. The non-survivor group had significantly higher proportions of patients with PaO2/FiO2≦200 and grade III/IV hepatic encephalopathy compared to the survivor group. In contrast, the survivor group had a significantly higher proportion of patients without hepatic encephalopathy compared to the non-survivor group. Non-survivors had a higher frequency of ACLF grade 3 classification for severity assessment.
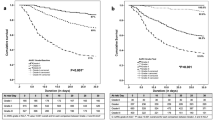
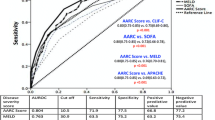
Comparison of the predictive strength of the original five prognostic scores for the primary outcomes
The AUROCs of the original five prognostic scores (MELD, MELD-Lactate, CLIF-C ACLF, CLIF ACLF-Lactate, APACHE-II) were compared concurrently to predict the primary outcomes. As shown in Table 2 and Fig. 2a, the AUROC (95% confidence intervals) of the five prognostic scores for 1-month mortality prediction was 0.818 (0.763–0.872), 0.783 (0.727–0.839), 0.787 (0.728–0.846), 0.793 (0.736–0.849), and 0.764 (0.705–0.823) respectively. The AUROC analysis did not demonstrate significant superiority of any of the five prognostic scores over the others in predicting 1-month or 3-month mortality (Table 3 and Fig. 2b).
Comparison of the predictive strength of the original five prognostic scores for the secondary outcomes
The AUROCs of the original five prognostic scores were simultaneously compared to predict secondary outcomes. Likewise, these five prognostic scores were still not significantly superior to each other in the in-hospital, 6-month, and 1-year mortality (Supplementary Fig. 1 and Supplementary Table 3).
Novel model building and validation
Since the original five prognostic models were not superior to each other, a novel model was built and validated, which was mentioned in the patient and method section (see Supplementary Table 1 and Supplementary 2).
The formulas of the novel model to predict the primary outcomes are:
-
(1)
One-month mortality = – 6.741+0.035 (age) + 0.002 (A-a gradient) + 0.009 (BUN) + 0.07 (total bilirubin) + 1.015 (INR) + βn (HE GRADE n), [1≦n≦4, n = 1, βn = 0.871; n = 2, βn = 0.913; n = 3, βn = 0.77; n = 4, βn = 1.516].
-
(2)
Three-month mortality = – 5.588 + 0.032 (age) + 0.002 (A-a gradient) + 0.012 (BUN) + 0.038 (total bilirubin) + 1.069 (INR) + βn (HE GRADE n), [1≦n≦4, n = 1, βn = 0.638; n = 2, βn = 0.631; n = 3, βn = 0.764; n = 4, βn = 0.681]
The formulas for predicting in-hospital, 6-month, and 1-year mortality as the secondary outcomes are presented in Supplementary Table 4.
Comparison of the predictive strength of the original five prognostic scores with the novel model for the primary and secondary outcomes
First, the AUROCs of the original five prognostic scores were compared with the new model concurrently to predict the primary outcomes. Table 2 and Fig. 2a demonstrate that the new model had a higher AUROC (95% confidence intervals) of 0.863 (0.818–0.907) for predicting 1-month mortality, as compared to the original five prognostic scores. The yellow-colored marks in Table 2 indicate significant difference in comparison between the models. Furthermore, the AUROC (95% confidence intervals) of the new model in predicting 3-month mortality was 0.829 (0.780–0.879), which was also superior to all the original five prognostic scores (Table 3 yellow-color marks and Fig. 2b).
The new model’s cut-off value for predicting 1-month mortality was – 1.0398, with mortality rates of 7.8% and 62.5% below and above this value, respectively. Similarly, the cut-off value for predicting 3-month mortality was 0.02, with corresponding mortality rates of 25.2% and 81.4% below and above this threshold, respectively.
Second, the predicting strength of the new model was also significantly superior to the original five prognostic scores in predicting in-hospital, 6-month, and 1-year mortalities (Supplementary Table 3 and Supplementary Fig. 2).
Subgroup sensitivity analysis was also conducted. The analysis included 131 patients who were admitted to ICU due to UGI bleeding and 114 patients who were admitted to ICU due to sepsis. The AUROC of the 1-month mortality prediction was 0.866 in the UGI bleeding subgroup and 0.800 in the sepsis subgroup.
Discussion
Prior research has shown the reliability and superiority of the CLIF-C ACLF score as an alternative prognostic scoring system for ACLF patients [30,31,32,33]. However, the superiority of the CLIF-C ACLF score compared to other prognostic scores in ICU-admitted ACLF patients remains uncertain. In our dataset, the AUROCs of the original five prognostic scores (MELD, MELD-Lactate, CLIF-C ACLF, CLIF ACLF-Lactate, APACHE-II) were compared concurrently to predict the primary and secondary outcomes. The results demonstrated that the five prognostic scores were not significantly superior to each other. Therefore, a novel predicting scoring model was built, internally validated, and tested whether it was superior to the original five prognostic scores in predicting the short-term mortality of ACLF patients who were admitted to the ICU. In summary, the new model outperformed the five prognostic scores in predicting mortality at various time points. Although this novel model may require further external validation, it remains a potentially excellent tool for assessing the short-term outcomes in ICU-admitted ACLF patients.
In this novel model, independent variables consist of age, A-a gradient, BUN, total bilirubin level, INR, and HE grades. These variables have been shown to be associated with the mortality of ACLF patients in several studies. First, age, serum total bilirubin level, INR, and HE grades are also included in the CLIF-C ACLF score [12]. Clinicians should be especially alert to the rapid progression and higher mortality rate of HE in ACLF patients [34, 35]. In addition, an elevated alveolar–arterial gradient (A-a) gradient can also be observed in patients with cirrhosis and/or portal hypertension who have developed hepatopulmonary syndrome. [36, 37]. Furthermore, acute kidney injury is an important predictor of early mortality in patients ACLF [38]. A study has indicated that serum urea is a more accurate predictor of mortality than serum creatinine in ACLF patients with acute kidney injury [39]. In critically ill patients, an elevated BUN was associated with increased mortality independent of serum creatinine [40]. Further studies on the relationship between the variables and acute-on-chronic liver failure (ACLF) are necessary to enhance understanding and improve patient outcomes.
Accurately identifying the most effective prognostic tool for ICU-admitted ACLF patients is crucial for reducing the higher short- and long-term mortality rates associated with this patient population. Consequently, more aggressive treatment modalities, such as liver transplantation, are often considered [6, 7]. This is particularly relevant in East Asia, where HBV-related ACLF is prevalent [41, 42]. However, due to the implementation of effective anti-viral agents against HBV and HCV in recent years [41], alcohol-associated cirrhosis has contributed up to 50% of the overall cirrhosis burden in the United States and worldwide nowadays [43, 44]. It was comparable to our study population (alcoholic-related cirrhosis accounted for 57.4%). Treatment of alcoholic cirrhosis and ACLF may be an important issue in Asia and the world in the future [45,46,47]. The novel model can aid hepatologists and intensivists in predicting prognosis more accurately, enabling early identification of high-risk patients who may benefit from liver transplantation [48, 49].
However, our study has some limitations. First, the novel model has not been extensively validated. Further collaboration with other ICUs is urgently needed. Second, APACHE III and IV were not adopted for comparison due to their complexity. Third, data in this study were collected within 24 h of ICU admission, while the CANONIC study collected data between days 3 and 7 to calculate the CLIF-C ACLF score. However, collecting data on the first day of ICU admission was done to ensure consistency. Data obtained at different time points for calculating these prognostic scores may lead to different results. Fourth, MELD and MELD-Lactate, although not originally developed for ACLF patients, were included in this study due to their clinical utility in assessing the prognosis of patients with end-stage liver disease. Fifth, variables remained consistent in our novel model, whereas constants exhibited variation in predicting mortality at 1-month, in-hospital, 3-month, 6-month, and 1-year intervals. Conversely, five other prognostic scores maintained uniform variables and constants across distinct periods of mortality prediction.
Conclusion
The original five prognostic scores (MELD, MELD-Lactate, CLIF-C ACLF, CLIF ACLF-Lactate, APACHE-II) were not significantly superior to each other in predicting short-term mortality among these critically ill cirrhotic patients complicated with ACLF who were admitted to a hepatology ICU. The novel model incorporating age, A-a gradient, BUN, total bilirubin level, INR, and HE grades was significantly superior to the original five prognostic scores in predicting mortalities at different time points. This novel model may require further external validation, but remains a potentially excellent tool for assessing the short-term outcomes in ACLF patients who were admitted to the ICU.
Availability of data and materials
Data are not publicly available but may be accessed upon reasonable request, IRB approval, and data policy.
References
Moreau R, Jalan R, Gines P et al (2013) Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 144(7):1426-37.e1–9
Sarin SK, Choudhury A (2016) Acute-on-chronic liver failure: terminology, mechanisms and management. Nat Rev Gastroenterol Hepatol 13(3):131–149
Arroyo V, Moreau R, Kamath PS et al (2016) Acute-on-chronic liver failure in cirrhosis. Nat Rev Dis Primers 2:16041
Sarin SK, Choudhury A, Sharma MK et al (2019) Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific association for the study of the liver (APASL): an update. Hepatol Int 13(4):353–390
Arroyo V, Moreau R, Jalan R (2020) Acute-on-chronic liver failure. N Engl J Med 382(22):2137–2145
Karvellas CJ, Francoz C, Weiss E (2021) Liver transplantation in acute-on-chronic liver failure. Transplantation 105(7):1471–1481
Artru F, Louvet A, Ruiz I et al (2017) Liver transplantation in the most severely ill cirrhotic patients: a multicenter study in acute-on-chronic liver failure grade 3. J Hepatol 67(4):708–715
Zhang Y, Nie Y, Liu L, Zhu X (2020) Assessing the prognostic scores for the prediction of the mortality of patients with acute-on-chronic liver failure: a retrospective study. PeerJ 8:e9857
Vincent JL, Moreno R (2010) Clinical review: scoring systems in the critically ill. Crit Care 14(2):207
Keegan MT, Gajic O, Afessa B (2011) Severity of illness scoring systems in the intensive care unit. Crit Care Med 39(1):163–169
Kuo CC, Huang CH, Chang C et al (2021) Comparing CLIF-C ACLF, CLIF-C ACLF(lactate), and CLIF-C ACLF-D prognostic scores in acute-on-chronic liver failure patients by a single-center ICU experience. J Pers Med 11(2):79
Jalan R, Saliba F, Pavesi M et al (2014) Development and validation of a prognostic score to predict mortality in patients with acute-on-chronic liver failure. J Hepatol 61(5):1038–1047
Trebicka J, Fernandez J, Papp M et al (2020) The PREDICT study uncovers three clinical courses of acutely decompensated cirrhosis that have distinct pathophysiology. J Hepatol 73(4):842–854
Escarce JJ, Kelley MA (1990) Admission source to the medical intensive care unit predicts hospital death independent of APACHE II score. JAMA 264(18):2389–2394
Ho KM, Dobb GJ, Knuiman M, Finn J, Lee KY, Webb SAR (2005) A comparison of admission and worst 24-hour acute physiology and chronic health evaluation II scores in predicting hospital mortality: a retrospective cohort study. Crit Care 10(1):R4
Knaus WA, Wagner DP, Draper EA et al (1991) The APACHE III prognostic system: risk prediction of hospital mortality for critically III hospitalized adults. Chest 100(6):1619–1636
Kuzniewicz MW, Vasilevskis EE, Lane R et al (2008) Variation in ICU risk-adjusted mortality: impact of methods of assessment and potential confounders. Chest 133(6):1319–1327
Brown RS Jr, Kumar KS, Russo MW et al (2002) Model for end-stage liver disease and Child–Turcotte–Pugh score as predictors of pretransplantation disease severity, posttransplantation outcome, and resource utilization in United Network for Organ Sharing status 2A patients. Liver Transpl 8(3):278–284
Kamath PS, Kim WR, Advanced Liver Disease Study G (2007) The model for end-stage liver disease (MELD). Hepatology 45(3):797–805
Srikureja W, Kyulo NL, Runyon BA, Hu KQ (2005) MELD score is a better prognostic model than Child–Turcotte–Pugh score or discriminant function score in patients with alcoholic hepatitis. J Hepatol 42(5):700–706
Sarmast N, Ogola GO, Kouznetsova M et al (2020) Model for end-stage liver disease-lactate and prediction of inpatient mortality in patients with chronic liver disease. Hepatology 72(5):1747–1757
Nusrat S, Khan MS, Fazili J, Madhoun MF (2014) Cirrhosis and its complications: evidence based treatment. World J Gastroenterol 20(18):5442–5460
Tsochatzis EA, Bosch J, Burroughs AK (2014) Liver cirrhosis. Lancet 383(9930):1749–1761
Yeom SK, Lee CH, Cha SH, Park CM (2015) Prediction of liver cirrhosis, using diagnostic imaging tools. World J Hepatol 7(17):2069–2079
Kamath PS, Wiesner RH, Malinchoc M et al (2001) A model to predict survival in patients with end-stage liver disease. Hepatology 33(2):464–470
Drolz A, Horvatits T, Rutter K et al (2019) Lactate improves prediction of short-term mortality in critically ill patients with cirrhosis: a multinational study. Hepatology 69(1):258–269
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13(10):818–829
Maldonado G, Greenland S (1993) Simulation study of confounder-selection strategies. Am J Epidemiol 138(11):923–936
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143(1):29–36
Barosa R, Roque Ramos L, Patita M, Nunes G, Fonseca J (2017) CLIF-C ACLF score is a better mortality predictor than MELD, MELD-Na and CTP in patients with acute on chronic liver failure admitted to the ward. Rev Esp Enferm Dig 109(6):399–405
Engelmann C, Thomsen KL, Zakeri N et al (2018) Validation of CLIF-C ACLF score to define a threshold for futility of intensive care support for patients with acute-on-chronic liver failure. Crit Care. https://doi.org/10.1186/s13054-018-2156-0
Chen BH, Tseng HJ, Chen WT et al (2020) Comparing eight prognostic scores in predicting mortality of patients with acute-on-chronic liver failure who were admitted to an ICU: a single-center experience. J Clin Med 9(5):1540
Ramzan M, Iqbal A, Murtaza HG, Javed N, Rasheed G, Bano K (2020) Comparison of CLIF-C ACLF score and MELD score in predicting ICU mortality in patients with acute-on-chronic liver failure. Cureus 12(2):e7087
Cordoba J, Ventura-Cots M, Simon-Talero M et al (2014) Characteristics, risk factors, and mortality of cirrhotic patients hospitalized for hepatic encephalopathy with and without acute-on-chronic liver failure (ACLF). J Hepatol 60(2):275–281
Lee GH (2015) Hepatic encephalopathy in acute-on-chronic liver failure. Hepatol Int 9(4):520–526
Sussman NL, Kochar R, Fallon MB (2011) Pulmonary complications in cirrhosis. Curr Opin Organ Transplant 16(3):281–288
Cosarderelioglu C, Cosar AM, Gurakar M, Dagher NN, Gurakar A (2016) Hepatopulmonary syndrome and liver transplantation: a recent review of the literature. J Clin Transl Hepatol 4(1):47–53
Khatua CR, Panigrahi S, Mishra D et al (2018) Acute kidney injury at admission is a better predictor of mortality than its persistence at 48 h in patients with acute-on-chronic liver failure. J Clin Transl Hepatol 6(4):396–401
Khatua CR, Sahu SK, Meher D et al (2021) Admission serum urea is a better predictor of mortality than creatinine in patients with acute-on-chronic liver failure and acute kidney injury. J Clin Exp Hepatol 11(5):565–572
Beier K, Eppanapally S, Bazick HS et al (2011) Elevation of blood urea nitrogen is predictive of long-term mortality in critically ill patients independent of “normal” creatinine. Crit Care Med 39(2):305–313
Zhao R-H, Shi Y, Zhao H, Wu W, Sheng J-F (2018) Acute-on-chronic liver failure in chronic hepatitis B: an update. Expert Rev Gastroenterol Hepatol 12(4):341–350
Chien RN, Kao JH, Peng CY et al (2019) Taiwan consensus statement on the management of chronic hepatitis B. J Formos Med Assoc 118(1 Pt 1):7–38
Lucey MR (2019) Alcohol-associated cirrhosis. Clin Liver Dis 23(1):115–126
Axley PD, Richardson CT, Singal AK (2019) Epidemiology of alcohol consumption and societal burden of alcoholism and alcoholic liver disease. Clin Liver Dis 23(1):39–50
Katoonizadeh A, Laleman W, Verslype C et al (2010) Early features of acute-on-chronic alcoholic liver failure: a prospective cohort study. Gut 59(11):1561–1569
Gustot T, Jalan R (2019) Acute-on-chronic liver failure in patients with alcohol-related liver disease. J Hepatol 70(2):319–327
Marroni CA, Fleck AM Jr, Fernandes SA et al (2018) Liver transplantation and alcoholic liver disease: history, controversies, and considerations. World J Gastroenterol 24(26):2785–2805
Chan AC, Fan ST (2015) Criteria for liver transplantation in ACLF and outcome. Hepatol Int 9(3):355–359
Kim JE, Sinn DH, Choi GS et al (2021) Predictors and outcome of emergent Liver transplantation for patients with acute-on-chronic liver failure. Dig Liver Dis 53(8):1004–1010
Acknowledgements
Thanks for all the medical staff who provided care to the patients included in this study.
Funding
This study was supported by grants from Chang Gung Medical Research Project (Chang Gung Memorial Hospital) (CMRPG3K0401-0402, CMRPG3M1931).
Author information
Authors and Affiliations
Contributions
CHH and SHL designed the study, analyzed the results, and drafted the manuscript. WTC, MHT, WLK, YTL, SFW, and CHL contributed to the clinical portions of the study, including caring patients, data collection and literature review. CHH, LTL, and BHC designed and executed the data analysis plan. RNC supervised and provided comments on the study. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval and consent to participate
The Institutional Review Board of Linkou Chang Gung Memorial Hospital approved the study (202000112B0).
Consent for publication
This manuscript contains no individual persons’ data, so the Institutional Review Board has waived the need for informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, SH., Chen, WT., Tsai, MH. et al. A novel prognostic model to predict mortality in patients with acute-on-chronic liver failure in intensive care unit. Intern Emerg Med 19, 721–730 (2024). https://doi.org/10.1007/s11739-024-03536-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-024-03536-4