Abstract
Iron deficiency anemia (IDA) is one of the most common complications of inflammatory bowel disease (IBD). We planned a prospective study to address tolerability and efficacy of sucrosomial iron, a new oral formulation of ferric pyrophosphate, in IBD patients. Thirty patients with a confirmed diagnosis of Crohn’s Disease (CD) or ulcerative colitis (UC) and mild IDA were enrolled. Patients with severe IBD were excluded. All patients underwent 12 weeks of oral treatment with 30 mg/day of sucrosomial iron. Treatment compliance and adverse events were investigated every 4 weeks. Iron status, hematological parameters and IBD activity scores were determined at baseline and at the end of treatment, as well as serum hepcidin and non-transferrin bound iron (NTBI) levels. Twenty-four (80%) patients took more than 90% of the prescribed regimen. Forty-four adverse events (AEs) were recorded, but none of them is considered certainly or probably related to the study treatment. Interestingly, only eleven gastrointestinal events were recorded in 9 (30%) patients. At the end of treatment, all iron parameters improved significantly and Hb increased in 86% of patients (from 11.67 to 12.37 g/dl, p = 0.001). Serum hepcidin showed a significant increase in 79% of patients and became positively correlated with C-reactive protein (CRP) at the end of the study, while NTBI remained below the detection threshold after iron supplementation. The IBD activity scores improved in both CD and UC. This pilot interventional study supports the therapeutic use of sucrosomial iron in IBD and paves the way for future studies in larger or more difficult IBD populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anemia is one of the most common complications of IBD, with a prevalence varying from 6 to 74% in different case studies [1], involving up to 60% of patients at diagnosis, with differences between CD and UC reported in as much as 27% and 21%, respectively [2, 3].
Anemia in IBD is often under-diagnosed, not adequately monitored and not properly treated, but it significantly compromises patients’ qualities of life.
Iron deficiency (ID) represents the main cause of anemia in IBD patients, with a prevalence up to 90% [4]. Chronic ID in IBD is due to multiple factors: insufficient dietary intake, malabsorption, chronic inflammation, and intestinal bleeding [5, 6]. The differential diagnosis between IDA and anemia caused by chronic inflammation/disease (CDA) can, therefore, be particularly difficult in IBD as both pathogenic mechanisms often overlap in affected patients. Hepcidin, the iron regulatory hormone, is down-regulated during ID, whereas it is readily induced in inflammatory states, including active IBD [7]. Therefore, at least in principle, hepcidin may represent a useful indicator of the underlying cause of anemia.
According to the European Crohn’s and Colitis Organisation’s (ECCO) guidelines [8], oral iron (OI) is the option of choice for treating mild anemia (Hb > 11 g/dl) in IBD patients with clinically inactive disease, in the absence of intolerance to OI, whereas intravenous iron (IVI) should constitute the first line treatment in subjects with Hb < 10 g/dl, active disease, a history of intolerance to OI and in patients who need erythropoiesis-stimulating agents [9].
Although OI supplementation is usually well accepted by patients, concerns have been raised on its tolerability and efficacy [10, 11].
OI supplementation can lead to NTBI excess, with potential pro-oxidant effect of its labile form (labile plasma iron, LPI) [12]. Seemingly, Erichsen et al. demonstrate that iron sulfate increases plasma malondialdehyde, a marker of lipid peroxidation, in IBD patients with ID [13]. In this line, it has also been reported that OI can cause oxidative stress in the intestinal lumen of IBD patient [14], increasing the local production of pro-inflammatory cytokines in a dose-dependent manner and leading to adverse gastrointestinal effects like metallic taste, nausea, diarrhea, constipation, and abdominal pain that limit compliance to OI [12]. Furthermore, studies from animal models show that endoluminal iron can re-exacerbate IBD and alter the intestinal microbiota, which is known to play a key role in the pathogenesis of the disease. A possible carcinogenic activity of unabsorbed iron has also been postulated [15, 16].
Recent progress in pharmacology has now led to the development of liposomal vesicles as carriers of bioactive molecules [17]. In this context, a liposomal formulation of iron should enhance iron absorption even in a state of chronic inflammation, since it does not use the intestinal iron transporter that is inhibited by hepcidin [18], and would likely increase iron supply without generating NTBI.
Sucrosomial iron has recently become available in Europe. A recent formulation consists of a ferric pyrophosphate core protected by a phospholipid bilayer membrane, mainly sunflower lecithin, and a sucrester matrix that has a gastroprotective action. This formulation seems to have an increased bioavailability compared to ferrous sulfate, allowing lower therapeutic doses [19].
The aim of our study is, therefore, to prospectively evaluate the tolerability and efficacy of 12 weeks of sucrosomial iron in a cohort of IBD patients with mild IDA.
Materials and methods
Study population
The study was designed as an open-label, prospective, monocentric, one-arm study.
Patients were included in the study if they had inactive to moderate active IBD (UC or CD) and mild IDA. UC and CD diagnoses were based on clinical, radiological, endoscopic and histological findings [20, 21]. Mild anemia was defined according to the World Health Organization (WHO) and ECCO definitions (Hb 11.0–11.9 g/dl in females and 11.0–12.5 g/dl in males), serum iron < 50 μg/dl, vitamin B12 and folic acid within range of normal. Disease activity was determined by the Colitis Activity Index (CAI) in UC or by Crohn’s Disease Activity Index (CDAI) score in CD patients. CAI index was chosen for UC since it is not influenced by Hb for levels > 10 g/dl [22, 23].
Exclusion criteria were: CAI > 10 in UC and CDAI > 450 in CD patients; need for blood transfusion or intravenous iron according to medical judgment at screening; iron preparations or erythropoietin received within 3 months around screening; presence of hemolytic anemia, bleeding hemorrhoidal disease, menometrorrhagia. Other reasons for exclusion were: alcohol abuse; renal failure (glomerular filtration < 30 ml/min, calculated by CKD-EPI); thyroid disease, including overt hyperthyroidism or subclinical hypothyroidism); active peptic disease; liver cirrhosis; hereditary anemia; thalassemia trait; history of solid tumor except of basocellular skin carcinoma; myelodysplastic disease within 5 years of screening; pregnancy and breastfeeding.
The study was approved by the Ethics Committee of Modena (145/15) and written informed consent was obtained from all individual participants included in the study.
Treatment and evaluation
After a 15-day screening period, all enrolled patients underwent 12 weeks of oral treatment with a single capsule of Sideral Forte® (Pharmanutra Spa, Pisa, Italy; sucrosomial iron 30 mg plus vitamin C 70 mg) once daily.
Patients underwent five study visits: one screening visit and one enrollment visit within 15 days, two visits during the treatment period (at 4th and 8th week of treatment) and one final visit after 12 weeks of iron intake. At enrollment, patients were instructed on how to intake iron supplementation and how to record daily sucrosomial iron intake and gastrointestinal symptoms or AEs, if occurred, on the patient’s diary.
Compliance to treatment was determined by capsules count at the end of treatment and through patient’s diary evaluation.
Safety and tolerability were evaluated based on physical examination, vital signs measurements, and collection of gastrointestinal symptoms and AEs during study visits and through patient’s interview and patient’s diary review. The following gastrointestinal symptoms were detected: presence or worsening of epigastric pain, tenesmus, vomiting, nausea, diarrhea, constipation, night evacuations, melena, intestinal and rectal bleeding. At each study visit, gastrointestinal symptoms were collected by investigators through a patient interview and a review of the patient’s diary. Investigators filled in a specific AE report in which they recorded, for each symptom, presence, intensity (mild, moderate or severe), frequency, required treatment (if any), relationship with Sideral Forte® (certain, probable, possible, unlikely or not related) and seriousness, as per protocol and Good Clinical Practice guidelines [24]. Concomitant medications were also reviewed at each clinical visit.
Efficacy endpoints focused on changes in Hb, mean corpuscular volume (MCV), reticulocytes count, serum iron, serum ferritin, serum transferrin and transferrin saturation (TSAT). Other secondary efficacy endpoints included leukocytes count, erythrocyte sedimentation rate (ESR), CRP and changes in disease activity scores. All biochemical parameters were determined at enrollment and at final visit by automated methods at the central hospital laboratory.
Serum hepcidin and NTBI determination
Measurement of serum hepcidin and NTBI levels was also conducted as part of the efficacy analysis. Blood samples were collected in the absence of EDTA or another anticoagulant. Serum was obtained via centrifugation and stored at − 80 °C until analysis.
Serum hepcidin was determined by an ELISA assay specific for the bioactive form of the protein (DRG Diagnostics, DRG Instruments GmbH, Germany).
NTBI was determined by a fluorescence method (FeROS™ eLPI, Aferrix Ltd., Israel) which measures the iron-specific redox activity in serum in the presence of a mobilizing agent (overcoming the effects of plasma albumin, citrate and uric acid) [25].
Hepcidin assay was a quantitative method while NTBI assay provided qualitative results (positive for value > 0.2 eLPI unit, negative for value < 0.2 eLPI unit) [26, 27].
Statistical analysis
Categorical variables were described using proportion and compared by Chi square or Fisher’s exact test. Continuous variables are presented as mean ± SD (if parametric) and as median and interquartile range (IQR) if non-parametric. They were compared (when two groups were considered) using the paired or unpaired Student’s t test (or Wilcoxon rank test), when appropriate. Spearman’s rho was used to assess simple correlation between continuous variables. Robust logistic regression was used to assess the association between the chosen factors/variables and the increase of Hb after therapy. In all statistical evaluations, a p < 0.05 was taken as significant.
Statistical analysis was performed by SPSS (v.24.0, IBM Analytics, Chicago, Il, USA) and STATA (v. 14.0, College Station, TX: Stata Corp LP, USA).
Results
Characteristics of enrolled IBD patients
Patients’ characteristics are reported in Table 1. In total, 30 patients were included in the study, 17 (56.7%) with CD and 13 (43.3%) with UC. One UC patient was affected by proctitis (E1, 7.7%), 7 by left-sided UC (E2, 53.8%) and 5 by extensive UC (E3, 38.5%). 5 CD patients had terminal ileum location (L1, 29.4%), 3 colon location (L2, 17.6%), 9 ileocolon location (L3, 53%). As for CD disease behavior, 7 CD patients (41.2%) had non-stricturing non-penetrating disease (B1), 3 (17.6%) had stricturing CD (B2) while the remained 7 patients (41.2%) had penetrating CD (B3) [20, 21]. The mean age was 57 ± 18.8 years and 17 (56.7%) patients were female. All recruited patients were on treatment for IBD: 17 (56.7%) were on mesalamine, 4 (13.3%) were on mesalamine plus azathioprine/6-mercaptopurine, 2 (6.7%) patients were on biologic agents while 7 (23.3%) were both on biologics and azathioprine.
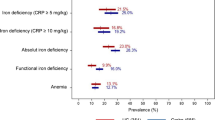
At baseline, patients were in remission or had mild disease activity, as confirmed by a CDAI between 31.8 and 206.2 for CD patients and a CAI between 0 and 7 for UC patients. The mean Hb level was 11.7 g/dl, while the mean serum iron was 42 mg/dl.
When looking at compliance to treatment, only six patients took less than 90% of the prescribed capsules (missing more than eight capsules), with a median of 78 days (IQR 8 days) of completed treatment (corresponding to 93% of capsules taken). All patients were included in the safety analysis, while one patient, who took only nine capsules, was excluded from the efficacy analysis.
AEs during 12 weeks of sucrosomial iron treatment
As to the gastrointestinal symptoms, 11 new events are recorded in 9 patients (Table 2). All were of mild severity and did not require medical treatment. None was considered certainly or probably related to the study treatment: two patients had possibly related events (one vomiting and nausea, one constipation); two had unlikely related events (one diarrhea and one epigastric pain); six gastrointestinal symptoms were considered not related: epigastric pain and intestinal bleeding (one patient), diarrhea (one patient), intestinal bleeding (two different patients) and tenesmus (one patient).
The patient diary reviews revealed that all 30 patients had mild IBD-related gastrointestinal symptoms at baseline. Of these, 8 (27%) patients showed an improvement by the end of the treatment, 17 (57%) did not present any change while 5 (17%) patients showed worsened gastrointestinal symptoms. With regard to AEs other than from gastrointestinal symptoms, 23 events are recorded in 11 patients (Table 3). All events were of mild intensity except two. One patient had an AE of moderate severity (renal colic) for which he received medical treatment at home. Another patient had one SAE during the study period: a 67-year-old man on double immunosuppression, with a CAI index of seven at screening, and previous multiple hospitalizations due to severe flare of disease, was hospitalized because of severe UC flare. For this reason, the patient ended the study prematurely, after assumption of only nine capsules and was, therefore, excluded from the efficacy analysis. This SAE was judged not related to iron supplementation and treated with fasting and IV steroids. No other patient was excluded from efficacy analysis due to changes in IBD treatment during the study period, as required by the study protocol.
Effect of sucrosomial iron in IBD patients (29 pts)
Hematological parameters
After 12 weeks of treatment with sucrosomial iron, 86% of patients had an increase in Hb. Absolute mean Hb concentration raised from 11.67 g/dl ± 0.5 to 12.38 ± 0.8 g/dl (p < 0.0001) (Fig. 1 and Table 4), with a mean increase of 0.7 g/dl (6.1%), independent of gender (p = 0.556). Moreover, 9 (31%) subjects had an Hb increment ≥ 1 g/dl. Correction of anemia was obtained in 17 (59%) patients. The increase in Hb remained statistically significant even when considering CD and UC separately: in CD patients, the mean Hb value changed from 11.58 ± 0.5 g/dl to 12.14 ± 0.7 g/dl (p < 0.001) while for UC patients Hb changed from 11.76 ± 0.5 g/dl to 12.66 ± 0.9 (p = 0.005).
Iron parameters
Serum iron levels improved after supplementation with sucrosomial iron in most patients (23%), independent of gender: the mean increase in serum iron was of 23 mg/dl, corresponding to a mean rise of 62%. Mean serum iron level raised from 41.79 ± 8.9 to 65.03 ± 34.1 mg/dl (p = 0.001) (Fig. 1 and Table 4).
Mean TSAT value raised from 10.96 ± 3.6 to 16.72 ± 10.1% (p = 0.004) (Fig. 1 and Table 4). In particular, the mean increase of TSAT was 169%.
Mean serum ferritin did not raise from baseline (45.79 ± 78.8 ng/ml) to the end of treatment (44.62 ± 70.8 ng/ml) (Table 4).
Baseline hepcidin levels are characterized by a wide variability within the study population, ranging from 0.6 ng/ml to 94.3 ng/ml (mean value of 14.09 ± 22.7) (Fig. 1). The wide variability of values remains after iron supplementation; yet, the majority of patients (79%) show significantly higher hepcidin values after treatment (mean of 19.51 ± 27.3 ng/ml, p = 0.02).
Baseline hepcidin levels are negatively correlated to baseline transferrin and positively correlated to baseline serum ferritin, regardless of the underlying IBD condition (CD or UC) or disease activity scores.
After 12 weeks of therapy, both the negative correlation between hepcidin and transferrin and the positive correlation with ferritin remain. Interestingly, after therapy, serum hepcidin becomes positively correlated with CRP.
NTBI is not detectable (concentration lower than 0.2 LPI Unit) in all patients both at baseline and after 12 weeks of therapy, suggesting that liposomal iron, unlike other oral preparations, is capable of correcting anemia without determining the formation of pro-oxidant NTBI forms.
Changes in disease activity
When looking at clinical severity of inflammatory disease in CD patients, the mean CDAI is 78.68 ± 47.2 at baseline (Fig. 1 and Table 4). Only one patient had an initial CDAI corresponding to mild disease activity (CDAI = 206), which remained in the range of mild activity even after 12 weeks of therapy (CDAI = 199), while the remaining CD patients had a CDAI lower than 150, corresponding to quiescent disease.
CDAI did not worsen but, on the contrary, significantly decreases by the end of treatment in most patients (82%), thus indicating an improvement in the clinical disease status (final CDAI = 63.6 ± 40.9, p = 0.006) (Fig. 1 and Table 4).
As to UC, all affected patients but two had a baseline CAI lower than 4, corresponding to quiescent disease: one patient had an initial CAI = 4 corresponding to mild disease activity, which became 0 after 12 weeks of therapy; another patient had an initial CAI = 7, corresponding to mild disease activity and was hospitalized after assumption of nine capsules of iron supplementation due to a severe flare of UC and, for this reason, suspended the iron supplementation intake and was excluded from the efficacy analysis.
By the end of treatment, an improvement in CAI was observed, even though statistical significance was not achieved.
Regarding the inflammatory parameters, the majority of enrolled patients (58.6%) had at baseline a serum CRP level equal or below 0.5 mg/dl, which is the cutoff used by our laboratory to define normal values, with a mean value of 0.62 mg/dl. The change in serum CRP levels observed at the end of the study is not statistically significant, while the decrease of ESR levels, which was detected in 69% of patients, is close to statistical significance (mean value changed from 31.71 to 27.43 mm/h, p = 0.076) (Table 4).
Discussion
This study is the first to assess tolerability and efficacy of sucrosomial iron (Sideral Forte®) in a challenging patient population, IBD patients with IDA.
As evidence of good tolerability, 29 patients out of 30 (96.6%) completed the study, with 80% taking all the prescribed regimen. Six patients, who took less than 10% of the prescribed therapy, report forgetfulness as the most common reason for missing the therapy. Previous data on OI supplementation with ferrous sulfate or ferric maltol report a worse compliance to treatment with AE in 1 of 4 patients and discontinuation of treatment in a one-fifth of patients [6, 10]. Such difference could be explained by the fact that sucrosomial iron, different from the other iron preparations, can be taken at any time of the day, independent of meals, and is therefore easier to manage by patients.
When considering reported AE, the majority of side effects were gastrointestinal. All AEs were of mild intensity except for two: one moderate AE (renal colic) and one serious AE (flare of UC), all judged not related to iron supplementation. Only 17% of the studied population report worsened gastrointestinal symptoms, all within the mild grade. Moreover, half of the reported events were judged unrelated to the treatment, only 7% possibly related to the supplement and none certainly or probably related to the therapy. Of note, eight patients (27%) report an improvement in overall gastrointestinal symptoms. Therefore, these data compare favorably with previous study in IBD patients with other OI supplementations [6, 10, 28].
In terms of efficacy, in our population a low dose of sucrosomial iron (30 mg/day) determines a significant increment of serum iron parameters in the majority of patients (76%). Particularly, the mean increase in TSAT, which can be considered an index of iron availability for erythropoiesis, is as much as 169%.
Consequently, Hb levels significantly increase after 12 weeks of treatment (mean increase: 0.7 g/dl), in both patients with UC and CD, regardless of gender, with correction of IDA in almost 60% of the total population.
Since the iron preparation tested in the study contains a relatively low dose of elemental iron (30 mg) compared to traditional compounds [6, 10], this is a further confirmation that its formulation allows a better absorption compared to other OIs.
Recently, a 12-week placebo-controlled trial published by Gasche et al. tested the efficacy and safety of 60 mg/day of ferric maltol in a group of IBD patients, reporting a good efficacy and a favorable safety profile. However, most of the selected patients were in disease remission with only a few CD cases having mild activity disease. Furthermore, about 25% of patients show drug-related AEs and iron therapy was consequently interrupted in 13% of cases [6, 28].
In previous studies in IBD patients treated with ferrous sulfate, the efficacy in terms of Hb increase was greater than in our study; however, this was obtained at the expense of a higher incidence of gastrointestinal side effects (at least in 25% of patients) and OI discontinuation (at least in 20%), likely due to the higher dose of OI used [11, 29].
Since previous studies about oral iron supplementation in IBD speculate a possible risk of disease exacerbation and worsening of the clinical status linked to unabsorbed iron, we assessed changes in disease activity scores. Both CDAI in CD and CAI in UC show a surprisingly downward trend, even though it reached statistical significance only for CDAI. This can be ascribed, at least in part, to the presence of hematocrit in CDAI but not in CAI calculation, which is completely independent of iron and blood counts in patients with mild anemia.
It should be noted that only three patients (two with CD, one with UC) in the whole population had a worsened disease activity score after treatment.
IDA in IBD is a composed disease model of iron deficiency and chronic inflammatory state. Hepcidin, the key regulator of iron homeostasis, increases in inflammatory states in virtue of its defensin-like properties, with consequent inhibition of both iron absorption from the intestinal lumen and release from deposits [30]. On the contrary, hepcidin is negatively regulated in iron-deficient states to ensure erythropoiesis [31]. The available literature data well emphasize the difficulty in interpreting cause and significance of hepcidin levels in IBD patients [7]. In our study, baseline serum hepcidin is characterized by a wide variability (from 0.6 to 94.3 ng/ml.) but, in spite of the obvious value dispersion, its increase from baseline to week 12 is statistically significant (p = 0.02), mirroring the observed increase in iron availability and improvement of anemic status. Also, in line with the previous literature, a direct correlation between serum hepcidin and ferritin is found both at baseline (strong correlation) and at week 12 (moderate correlation). Furthermore, hepcidin became directly related to CRP only at the end of the treatment. We hypothesize that serum hepcidin increases initially as expected in response to iron, and then, once ID is corrected, correlates with CRP, a marker of the underlying inflammatory state [32, 33].
Previous works have shown that OI can cause an elevation of NTBI levels [34, 35]. NTBI represents the circulating iron form that becomes detectable when transferrin binding capacity is overcome; NTBI, and in particular its LPI fraction, is considered a key element in inducing oxidative damage of cell membranes and other biomolecules [36]. Therefore, preventing the formation of NTBI is detrimental both in iron overload conditions and in chronic inflammatory diseases such as IBD. In fact, it has been shown that in IBD patients who take iron sulfate, ROS-mediated oxidative damage acts on a mucosa already damaged by the underlying disease, establishing a vicious circle of further mucosal damage [15].
In our study, NTBI was under the detection threshold both at baseline and at the end of treatment with sucrosomial iron, supporting that sucrosomial iron, unlike ferrous salts, does not determine the formation of free plasma iron, probably due to its pharmacokinetic characteristics.
In the sucrosomial technology, iron does not interface with the intestinal mucosa because it is released by the liposome only once it reaches the hepatocyte through the lymphatic circulation [37]. Therefore, thanks to the optimal bioavailability due to the specific mechanism of absorption, most likely free iron is not generated in the intestinal lumen, and ROS production is avoided.
The present study, with the obvious drawbacks of a single-center open-label design, provides evidence for optimal tolerability and good short-term efficacy of sucrosomial iron supplementation in both CD and UC patients with mild/moderate active disease and moderate IDA.
Due to its large prevalence among IBD patients, anemia is often underestimated and neglected despite its effects in terms of worsened quality of life, disease progression and increased social and health costs. This pilot interventional study provides positive data supporting the therapeutic use of sucrosomial iron in IBD and paves the way for future studies in larger IBD populations with more severe anemia or more active disease, also comparing sucrosomial iron to other oral or intravenous iron preparations.
References
Testa A, Rispo A, Romano M, Riegler G, Selvaggi F, Bottiglieri E, Martorano M, Rea M, Gravina A, Nardone OM, Patturelli M, Pellino G, Miranda A, Caporaso N, Castiglione F (2016) The burden of anaemia in patients with inflammatory bowel diseases. Dig Liver Dis 48:267–270. https://doi.org/10.1016/j.dld.2015.10.012
Filmann N, Rey J, Schneeweiss S, Ardizzone S, Bager P, Bergamaschi G, Koutroubakis I, Lindgren S, Morena Fde L, Moum B, Vavricka SR, Schroder O, Herrmann E, Blumenstein I (2014) Prevalence of anemia in inflammatory bowel diseases in european countries: a systematic review and individual patient data meta-analysis. Inflamm Bowel Dis 20:936–945. https://doi.org/10.1097/01.MIB.0000442728.74340.fd
Bergamaschi G, Di Sabatino A, Albertini R, Ardizzone S, Biancheri P, Bonetti E, Cassinotti A, Cazzola P, Markopoulos K, Massari A, Rosti V, Porro GB, Corazza GR (2010) Prevalence and pathogenesis of anemia in inflammatory bowel disease. Influence of anti-tumor necrosis factor-alpha treatment. Haematologica 95:199–205. https://doi.org/10.3324/haematol.2009.009985
Kulnigg S, Gasche C (2006) Systematic review: managing anaemia in Crohn’s disease. Aliment Pharmacol Ther 24:1507–1523. https://doi.org/10.1111/j.1365-2036.2006.03146.x
Zimmermann MB, Hurrell RF (2007) Nutritional iron deficiency. Lancet 370:511–520. https://doi.org/10.1016/S0140-6736(07)61235-5
Gasche C, Berstad A, Befrits R, Beglinger C, Dignass A, Erichsen K, Gomollon F, Hjortswang H, Koutroubakis I, Kulnigg S, Oldenburg B, Rampton D, Schroeder O, Stein J, Travis S, Van Assche G (2007) Guidelines on the diagnosis and management of iron deficiency and anemia in inflammatory bowel diseases. Inflamm Bowel Dis 13:1545–1553. https://doi.org/10.1002/ibd.20285
Theurl I, Schroll A, Nairz M, Seifert M, Theurl M, Sonnweber T, Kulaksiz H, Weiss G (2011) Pathways for the regulation of hepcidin expression in anemia of chronic disease and iron deficiency anemia in vivo. Haematologica 96:1761–1769. https://doi.org/10.3324/haematol.2011.048926
Dignass AU, Gasche C, Bettenworth D, Birgegard G, Danese S, Gisbert JP, Gomollon F, Iqbal T, Katsanos K, Koutroubakis I, Magro F, Savoye G, Stein J, Vavricka S, Cs European, Colitis O (2015) European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. J Crohns Colitis 9:211–222. https://doi.org/10.1093/ecco-jcc/jju009
Kaitha S, Bashir M, Ali T (2015) Iron deficiency anemia in inflammatory bowel disease. World J Gastrointest Pathophysiol 6:62–72. https://doi.org/10.4291/wjgp.v6.i3.62
Lee TW, Kolber MR, Fedorak RN, van Zanten SV (2012) Iron replacement therapy in inflammatory bowel disease patients with iron deficiency anemia: a systematic review and meta-analysis. J Crohns Colitis 6:267–275. https://doi.org/10.1016/j.crohns.2011.09.010
de Silva AD, Tsironi E, Feakins RM, Rampton DS (2005) Efficacy and tolerability of oral iron therapy in inflammatory bowel disease: a prospective, comparative trial. Aliment Pharmacol Ther 22:1097–1105. https://doi.org/10.1111/j.1365-2036.2005.02700.x
Grisham MB (1994) Oxidants and free radicals in inflammatory bowel disease. Lancet 344:859–861
Erichsen K, Ulvik RJ, Grimstad T, Berstad A, Berge RK, Hausken T (2005) Effects of ferrous sulphate and non-ionic iron-polymaltose complex on markers of oxidative tissue damage in patients with inflammatory bowel disease. Aliment Pharmacol Ther 22:831–838. https://doi.org/10.1111/j.1365-2036.2005.02652.x
Lund EK, Wharf SG, Fairweather-Tait SJ, Johnson IT (1999) Oral ferrous sulfate supplements increase the free radical-generating capacity of feces from healthy volunteers. Am J Clin Nutr 69:250–255. https://doi.org/10.1093/ajcn/69.2.250
Seril DN, Liao J, Ho KL, Warsi A, Yang CS, Yang GY (2002) Dietary iron supplementation enhances DSS-induced colitis and associated colorectal carcinoma development in mice. Dig Dis Sci 47:1266–1278
Zimmermann MB, Chassard C, Rohner F, N’Goran EK, Nindjin C, Dostal A, Utzinger J, Ghattas H, Lacroix C, Hurrell RF (2010) The effects of iron fortification on the gut microbiota in African children: a randomized controlled trial in Cote d’Ivoire. Am J Clin Nutr 92:1406–1415. https://doi.org/10.3945/ajcn.110.004564
Simao AMS, Bolean M, Cury TAC, Stabeli RG, Itri R, Ciancaglini P (2015) Liposomal systems as carriers for bioactive compounds. Biophys Rev 7:391–397. https://doi.org/10.1007/s12551-015-0180-8
Brilli E, Romano A, Fabiano A, Zambito Y, Di Raimondo F, Tarantino G (2016) Sucrosomial technology is able to promote ferric iron absorption: pre-clinical and clinical evidences. Blood 128:3618
Pisani A, Riccio E, Sabbatini M, Andreucci M, Del Rio A, Visciano B (2015) Effect of oral liposomal iron versus intravenous iron for treatment of iron deficiency anaemia in CKD patients: a randomized trial. Nephrol Dial Transplant 30:645–652. https://doi.org/10.1093/ndt/gfu357
Gomollon F, Dignass A, Annese V, Tilg H, Van Assche G, Lindsay JO, Peyrin-Biroulet L, Cullen GJ, Daperno M, Kucharzik T, Rieder F, Almer S, Armuzzi A, Harbord M, Langhorst J, Sans M, Chowers Y, Fiorino G, Juillerat P, Mantzaris GJ, Rizzello F, Vavricka S, Gionchetti P, Ecco (2017) 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: part 1: diagnosis and medical management. J Crohns Colitis 11:3–25. https://doi.org/10.1093/ecco-jcc/jjw168
Magro F, Gionchetti P, Eliakim R, Ardizzone S, Armuzzi A, Barreiro-de Acosta M, Burisch J, Gecse KB, Hart AL, Hindryckx P, Langner C, Limdi JK, Pellino G, Zagorowicz E, Raine T, Harbord M, Rieder F, Cs European, Colitis O (2017) Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J Crohns Colitis 11:649–670. https://doi.org/10.1093/ecco-jcc/jjx008
Rachmilewitz D (1989) Coated mesalazine (5-aminosalicylic acid) versus sulphasalazine in the treatment of active ulcerative colitis: a randomised trial. BMJ 298:82–86
Best WR, Becktel JM, Singleton JW, Kern F Jr (1976) Development of a Crohn’s disease activity index. National Cooperative Crohn’s Disease Study. Gastroenterology 70:439–444
Guidelines for Good Clinical Practice E6(R1), (1996) International Conference on harmonization of technical requirements
Cabantchik ZI, Breuer W, Zanninelli G, Cianciulli P (2005) LPI-labile plasma iron in iron overload. Best Pract Res Clin Haematol 18:277–287. https://doi.org/10.1016/j.beha.2004.10.003
Zipperer E, Post JG, Herkert M, Kundgen A, Fox F, Haas R, Gattermann N, Germing U (2013) Serum hepcidin measured with an improved ELISA correlates with parameters of iron metabolism in patients with myelodysplastic syndrome. Ann Hematol 92:1617–1623. https://doi.org/10.1007/s00277-013-1839-5
Zanninelli G, Breuer W, Cabantchik ZI (2009) Daily labile plasma iron as an indicator of chelator activity in Thalassaemia major patients. Br J Haematol 147:744–751. https://doi.org/10.1111/j.1365-2141.2009.07907.x
Schmidt C, Ahmad T, Tulassay Z, Baumgart DC, Bokemeyer B, Howaldt S, Stallmach A, Buning C, Group AS (2016) Ferric maltol therapy for iron deficiency anaemia in patients with inflammatory bowel disease: long-term extension data from a Phase 3 study. Aliment Pharmacol Ther 44:259–270. https://doi.org/10.1111/apt.13665
Schroder O, Mickisch O, Seidler U, de Weerth A, Dignass AU, Herfarth H, Reinshagen M, Schreiber S, Junge U, Schrott M, Stein J (2005) Intravenous iron sucrose versus oral iron supplementation for the treatment of iron deficiency anemia in patients with inflammatory bowel disease—a randomized, controlled, open-label, multicenter study. Am J Gastroenterol 100:2503–2509. https://doi.org/10.1111/j.1572-0241.2005.00250.x
Pietrangelo A, Trautwein C (2004) Mechanisms of disease: the role of hepcidin in iron homeostasis—implications for hemochromatosis and other disorders. Nat Clin Pract Gastroenterol Hepatol 1:39–45. https://doi.org/10.1038/ncpgasthep0019
Ganz T, Nemeth E (2012) Hepcidin and iron homeostasis. Biochim Biophys Acta 1823:1434–1443. https://doi.org/10.1016/j.bbamcr.2012.01.014
Bergamaschi G, Di Sabatino A, Albertini R, Costanzo F, Guerci M, Masotti M, Pasini A, Massari A, Campostrini N, Corbella M, Girelli D, Corazza GR (2013) Serum hepcidin in inflammatory bowel diseases: biological and clinical significance. Inflamm Bowel Dis 19:2166–2172. https://doi.org/10.1097/MIB.0b013e31829a6e43
Mecklenburg I, Reznik D, Fasler-Kan E, Drewe J, Beglinger C, Hruz P, Swiss IBDCSG (2014) Serum hepcidin concentrations correlate with ferritin in patients with inflammatory bowel disease. J Crohns Colitis 8:1392–1397. https://doi.org/10.1016/j.crohns.2014.04.008
Dresow B, Petersen D, Fischer R, Nielsen P (2008) Non-transferrin-bound iron in plasma following administration of oral iron drugs. Biometals 21:273–276. https://doi.org/10.1007/s10534-007-9116-5
Schumann K, Kroll S, Weiss G, Frank J, Biesalski HK, Daniel H, Friel J, Solomons NW (2005) Monitoring of hematological, inflammatory and oxidative reactions to acute oral iron exposure in human volunteers: preliminary screening for selection of potentially-responsive biomarkers. Toxicology 212:10–23. https://doi.org/10.1016/j.tox.2005.03.014
Erichsen K, Milde AM, Arslan G, Helgeland L, Gudbrandsen OA, Ulvik RJ, Berge RK, Hausken T, Berstad A (2005) Low-dose oral ferrous fumarate aggravated intestinal inflammation in rats with DSS-induced colitis. Inflamm Bowel Dis 11:744–748
Tarantino G, Brilli E, Zambito Y, Giordano G, Equitani F (2015) Sucrosomial Iron®: a new highly bioavaible oral iron supplement. Blood 126:4561
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Abbati, G., Incerti, F., Boarini, C. et al. Safety and efficacy of sucrosomial iron in inflammatory bowel disease patients with iron deficiency anemia. Intern Emerg Med 14, 423–431 (2019). https://doi.org/10.1007/s11739-018-1993-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-018-1993-9